Fluid and Electrolyte Balance in the Human Excretory System
Introduction to Excretion
Functions of the Excretory System
What is the Excretory System and what does it do?
The excretory system regulates both the water content of the body and the ion concentration in body fluids
Essentially the kidney maintains the osmolarity of the body fluids = osmoregulation
Body fluids and water content include the watery components of the body including separate compartments such as the blood plasma (begins with this), the interstitial fluid, and cerebrospinal fluid.
The kidney maintains the blood volume and interstitial fluid volume, thus it maintains blood pressure
Adequate blood volume is extremely important, if blood volume falls, then blood pressure can fall to zero. This prevents the heart from being able to pump blood through the body and you will die from low cardiac output
Interstitial fluid volume regulation is important to prevent edema (loss of blood volume when levels of fluid are too high), fluid accumulation in the lungs/heart, or dehydration (occurs when level of fluid are too low - Losing fluid in one compartment leads to compensation by pulling water from others.)
The kidney eliminates nitrogenous wastes and other wastes
During metabolism we generate excess nitrogen in the from of ammonia NH3, which needs to be excreted from the body because it is the most toxic in comparison to other nitrogenous compounds like urea and uric acid. In the body it is excreted in 4 different forms:
Ammonia*
The nitrogen in our body comes from the deamination of amino acids during protein catabolism
Aka protein in food gets broken down to amino acids which can be deaminated (or have the amino group removed) and then be metabolized to result in the accumulation of nitrogen.
Nitrogen is then removed in the form of ammonia (NH3) a highly soluble gas and strong base that pulls four protons from water to create an ammonium ion (NH4+)
Requires the most water to excrete
Requires the least energy to synthesize (make)
Urea*
humans have a relatively high concentration of urea in the blood
Uric Acid* (least toxic)
mostly insoluble, precipitates into white crystals
Requires the least amount of water to excrete
Requires the most energy to synthesize (make)
Creatinine
excreted in the urine
comes from the breakdown of creatine
*= main human nitrogenous wastes
If an organism, such as fish, lives in freshwater, it is essentially living in distilled water. This means that their bodies are always accumulating water through osmosis and it is more difficult to get rid of excess water
This means a large amount of water is excreted through their kidneys and ammonia concentrations are always low, since they are continually excreting water to avoid lysis
If an organism lives in saltwater, it is hyperosmotic to the body fluids. This means that their bodies are always losing water through osmosis and it is easier to become dehydrated.
This means that these organism do not use or use less ammonia as their nitrogenous waste because it requires a lot of water to excrete (use uric acid)
Birds and other flying animals use a lot of energy to fly and cannot carry lots of water due to it’s weight, so nitrogen is converted to uric acid instead → the white stuff in bird poop
Humans mostly use urea as the form for excreting nitrogen from the body = a happy medium
The excretory system also secretes hormones:
Erythropoietin (EPO)
Stimulates red bone marrow to produce RBCs
Renin (an enzyme)
Activates a set of hormones that regulate the salt content of body fluids
Overview of Excretion
The kidney is supplied by a big artery that carries blood at a high pressure, thus there is a high pressure, flow, and rate of blood throughout the kidney. This allows for increased fluid filtration
The kidney is comprised of units known as nephrons. Nephrons are a hollow tube made of a single layer of epithelial cells and consisting of a glomerulus and tubule. One end of the tubule is open and the other is closed
The tubule that forms during embryonic development is closed, with one end expanding to form a bulb shape
Sometime during embryonic development, the bulbous end is pushed in or invaginated
At one point the invagination forms a double walled cup with a space in the middle
Differentiation occurs and the inner wall of the cup are modified to support diffusion
This is the bowman’s capsule, which has an inner layer comprised of podocytes
Inside the bowman’s capsule is the glomerulus which is a ball of capillaries that is supplied by an afferent arteriole. Once blood is filtered from the capillaries the it exits via the efferent arteriole and through the peritubular capillary
Blood flowing through afferent arteriole is highly pressurized
Blood flowing through efferent arteriole is at a lower pressure
Both the afferent and efferent arterioles, are arterioles because they contain smooth muscle
The capillaries in the glomerulus are leaky, and leaking fluid that is then filtered through the slits between endothelial cells. The result of this filtration is water, ions, and small/medium organic molecules → this is called the filtrate
proteins DO NOT leak out
Has the same composition of plasma minus proteins
In capillaries in other areas of the body this filtrate becomes the interstitial fluid however in the nephron the filtrate passes through the bowman’s capsule and remains in the lumen of the tubule
In the tubule the filtrate is forced out of the glomerulus into the bowman’s capsule by the difference between the blood (hydrostatic) pressure and the osmotic pressure: This is known as Filtration
The outward movement of water out of the capillary
Filtrate moves along the tubule driven by the net pressure, which moves the filtrate until it reaches the end of the nephron
Along the length of the tubule, the epithelial cells will transport materials, taking in water ions and organic molecules that travel through the apical membrane (faces lumen) and out the basolateral membrane (faces away from lumen).
Materials can leak through the spaces between the epithelial cells, the can be:
Taken out of the nephron lumen and into the surrounding interstitial fluid. Then the materials can diffuse into the leaky peritubular capillary: This is known as Reabsorption
The inward movement of water into the capillaries
This is because what is in the filtrate was initially in the blood plasma and it gets put back in the blood plasma
Materials can be transported from the interstitial fluid to the nephron/tubule: This is known as Secretion
The movement of materials from the blood plasma into the tubule lumen
At the end of the tubule, urine comes out (is not modified after leaving the tubule)
So in short Excretion is:
Filtration (amount put into tubule) - Reabsorption (amount moved from tubule to blood) + Secretion (amount moved from blood to tubule) = Excretion (amount peed out)
The Human Excretory System
Humans have 2 kidneys composed of 2 different layers
Outer layer is the renal cortex
Inner layer is the renal medulla
The kidneys have a renal pelvis, or a series of tubes/funnels that collect urine from the nephron
We have two kidneys in the abdomen that process blood and make urine; if you cut a kidney in half, you’ll see repeated pointy units called renal pyramids. Within these renal pyramids are nephrons.
Nephrons are densely packed together within the renal pyramids
Nephrons means the same thing as kidney tubule
Nephrons are not short and straight, like in the simplified diagram before, they are long, bendy, and convoluted. These tubules filter out the plasma minus the proteins and modify the tubular fluid to form urine, which is then excreted.
The ureter is a big tube that propel urine to the bladder, which leads to the urethra
The Nephron
There are two types of nephrons:
Cortical Nephron: Resides in the renal cortex and has a short loop of henle (80% of nephrons)
Juxtamedullary Nephron: Extends down into the renal medulla and has a long loop of henle (20% of nephrons)
The nephron consists of the glomerulus (w/ glomerular capillaries → highest pressure capillaries in the body) that is supplied by the afferent arteriole, which delivers blood to the glomerular capillaries at a high pressure and flow rate. The afferent arteriole is a smaller vessel that stems form the big renal artery
There is 25x more blood flow through the kidney than the average of other organs
It gets a lot of blood because the kidney continually adjusts the fluid, ion, and molecular composition of the plasma → 60 time the plasma volume/day
How does the process work?
Fluid is filtered out of the bowman’s capsule and pushed along the tubule buy the net filtration pressure. The fluid then reaches the curlicued proximal tubule (near bowman’s capsule) and down a long straight branch into the medulla that then comes up again. This is the Loop of Henle composed of the descending and ascending limbs. Once fluid passes the loop of henle it arrives at the distal tubule and then empties into a straight section of the tubule collecting duct (multiple nephrons can feed into one duct) where the fluid is further modified and comes out as urine. Urine is conveyed to the bladder via the ureters
The peritubular capillaries parallel the flow of fluid traversing through the nephron and are supplied by the efferent arteriole.
The peritubular capillaries take blood from the efferent arterioles and take it to venules, larger veins, then the renal vein, which leads to the vena cava and right atrium. The blood through the peritubular capillaries can flow all the way down the loop or a short distance down the loop.
Some of the blood coming from the first arteriole goes a looooooooongggg way before it gets to the first venule
The long straight capillaries of this network are known as the vasa recata (these parallel the loop of henle)
These receive water, irons, and organic molecules removed from the tubule (reabsorption) and supply waster products from the blood to the tubule (secretion). These are highly selective processes
Fluid Exchange Across Capillaries
Fluid gets driven out of capillaries by high blood pressure at the beginning of a vessel. This movement of fluid out of the capillaries is opposed by the inward movement of fluid caused by osmotic pressure (from the plasma proteins remaining in the blood). Thus there is a net movement out at upstream.
When BP falls at the end of a capillary, the outward movement of fluid decreases and the osmotic pressure remains the same, thus there is a net movement in at downstream
***In the kidney a back pressure is created by the net movement of fluid out of the capillary, as that fluid must displace the interstitial fluid within the bowman’s capsule. This back pressure is what moves the fluid in the nephron (kidney tubule)
The pressure in bowman’s capsule is not zero, its higher
As blood travels through the peritubular capillaries, BP will decreases. BP starts high in the glomerular capillaries and at the vasa recta BP is much much lower, and thus there is a shift towards net reabsorption (AKA movement of materials from nephron to capillaries). At the distal tubule BP is low and there is reabsorption, but it is not as high as at the vasa recta
Glomerular Filtration
The bowman’s capsule has an inner, visceral layer composed of podocytes
These podocytes form filtration slits, are motile, and respond to stimuli and hormones
These slits can widen or narrow to adjust rate of filtration
The fluid coming out of the bowman’s capsule and glomerulus complex has the SAME COMPOSITION OF BLOOD PLASMA EXCEPT IT DOES NOT HAVE THE PLASMA PROTEINS and then travels down the rest of the nephron
Net Filtration Pressure = Capillary Blood P - Osmotic P - Hydrostatic P in Lumen of Bowman’s Capsule
Tubular Transport
How does transportation and modification of fluid occur in the Nephron?
Proximal Tubule
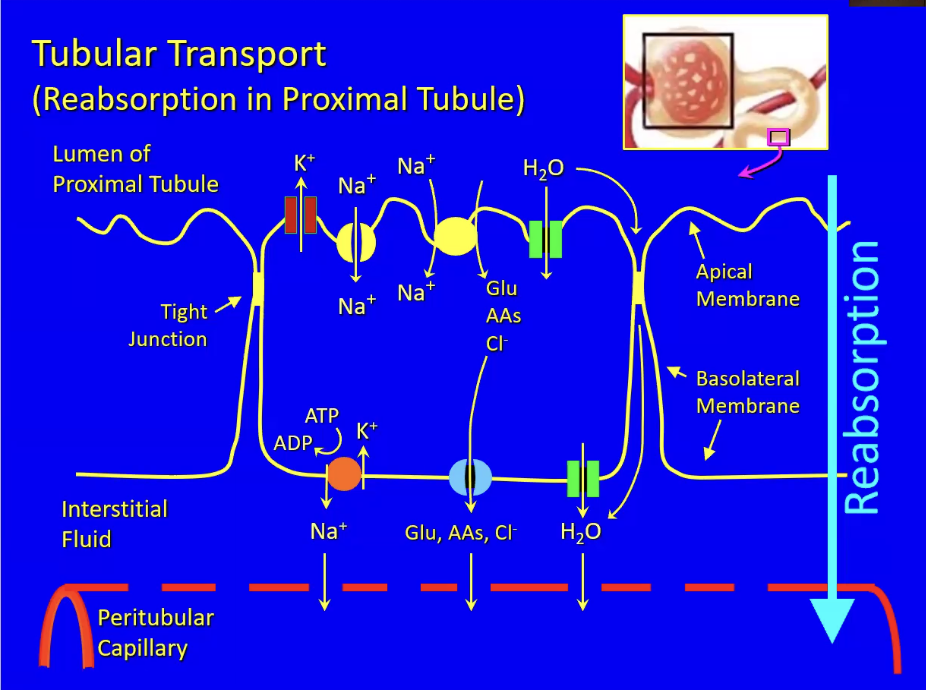
For epithelia that line a hollow organ, one side (the apical membrane that faces the lumen) performs different functions than the other (the basolateral membrane that faces the interstitial fluid → these cells are polarized
The cells adhere to one another with intercellular and tight junctions that form a belt around the cell
These tight junction limit the diffusion of materials in between cells, sealing off the extracellular space
The cells are in control of of what moves across epithelium
These cells facilitate the reabsorption of materias from the lumen to the blood and the secretion of materials from the interstitial fluid to the lumen
Materials in the interstitial fluid will diffuse into or out of the peritubular capillary down a concentration gradient.
Epithelial cells have pumps, ion channels, and transporters.
ATPases
sodium-potassium pump (orange circle)
In the basolateral membrane
This drives everything in the cell as it pumps out 3 Na+ ions for ever 2 K+ ions in using 1 ATP molecule. This pump uses a lot of glucose/O2
Active transport of Na out of cells, makes intracellular sodium levels low (inside cell). This makes the inside of the cell negative and causes and inward sodium electrochemical gradient, which allows sodium ions to flow back into the cell through a passive sodium selective channel (yellow circle to the right - in apical membrane).
Sodium ions are being reabsorbed into the blood
Potassium ion channels in the aplical membrane pump K out of the cell, as the build up of it inside the cell creates an outward electrochemical gradient
This allows for secretion of K into the tubule fluid and excretion of it in the urine
Sodium dependent, secondary active transporters (yellow circle in the middle)
In apical membrane
Do not directly use ATP, but use energy stored in the inward sodium electrochemical gradient to transport molecules (glucose, amino acids, chloride) against their concentration/electrochem gradients into the cell
Facilitated diffusion, passive transporters (blue circle)
In basolateral membrane
Transport the same substances as secondary active transporters, but do so down a concentration gradient
Diffuse out of the cell into the interstitial fluid and then into the peritubular capillary,
These substances are reabsorbed into the blood)
An osmotic gradient is created by the reabsorption of solute into the blood. This causes water to diffuse from the nephron to the blood, via osmosis through 2 paths. This drives the reabsorption of water in the blood
Some water diffuses through the tight junctions
Travel though aquaporin channels
An osmotic gradient is created by the reabsorption of all the solute into the blood. This causes water to diffuse via osmosis through 2 paths. This drives the reabsorption of water in the blood
Diabeties mellitus occurs when the glucose levels in the plasma are too high which show up in the urine.
Big Picture (Tubular Transport)
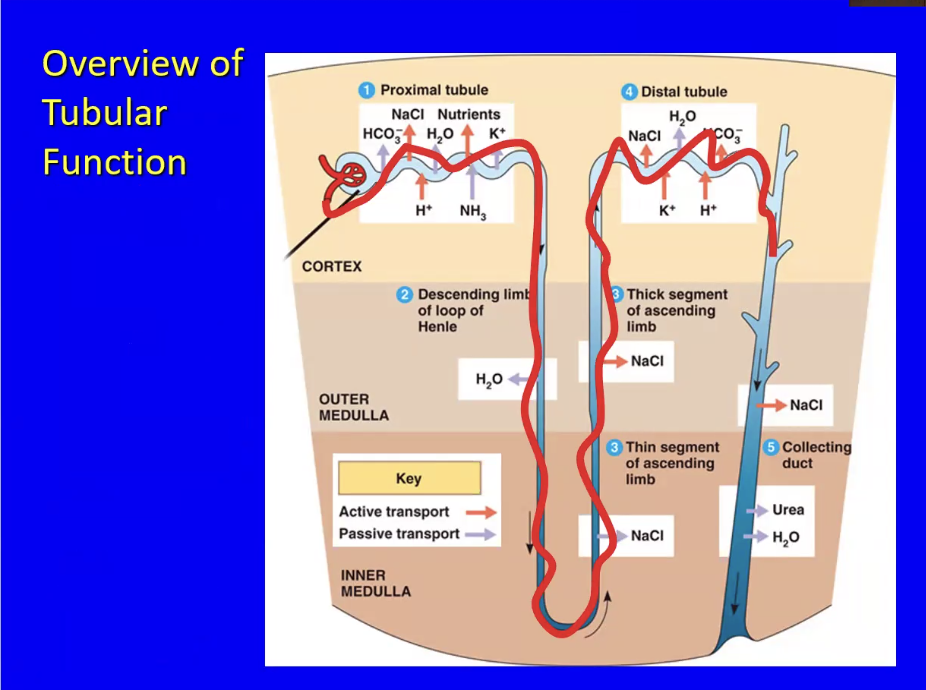
The Loop of Henle has 3 total parts
Descending limbs moves fluid down
Only facilitates reabsorption water passively
Ascending limb moves fluid up and can be broken down into upper and lower parts.
the epithelial cells are permeable to salt, but not to water. The bottom of the ascending limb has thin epithelial cells which transport salt passively to blood and the top part of the ascending limb has thick epithelial cells which transport salt actively to blood using Na/K pumps
Although similar, there is a difference between the process of the distal tubule and the proximal tubule
The mechanisms of secretion/reabsorption in the proximal tubule are unregulated (constitutive) due to occuring at a high rate
In the distal tubule, the fluid coming through is not very salty (because of the ascending limb’s reabsorption). Along the distal tubule, the solute concentration is adjusted by passive water reabsorption and active salt and bicarbonate reabsorption, along with active potassium and proton secretion. All of these processes are very regulated via hormones. This low-salt and high-water content fluid then dumps into the collecting duct
In the collecting duct, the high water content/low solute fluid travels downwards and towards the salty medulla. There are two situations to know
You are dehydrated and want to reabsorb water: Active transport is thus needed to take out more salt from this fluid. Furthermore, water and urea are reabsorbed. This happens because the medulla is very salty, which pulls water out of the tubular fluid.
You drank too much water and want to get rid of it: the collecting duct becomes impermeable to water, limiting reabsorption and promoting the dumping of water to prevent body fluids from becoming hypoosmotic
***Note: The medulla of the kidney contains high concentrations of salt and urea, with the highest concentrations being in the inner medulla, then the outer medulla is a little lower. The kidney does this so it can adjust its final extraction of water from the tubular fluid.
As the descending limb gives up water and enters the high-urea/salt-concentration regions of the medulla, there is a large drive of water to be reabsorbed into the vasa recta capillaries
As water is reabsorbed down the length of the proximal tubule and descending loop of henle, the tubular fluid becomes saltier and saltier, but the salt cant leave until the ascending limb, wherein salt is reabsorbed. Reabsorption of salt is passive at first due to the high concentration of salt in the tubular fluid and then active due to the higher concentration.
The thick ascending limb’s epithelial cells are thick, producing lots of ATP to fuel the sodium potassium pump, pumping salt out of the tubular fluid and into the vasa recta capillaries.
By the time the tubular fluid reaches the distal tubule, most of the salt is removed.
This mechanism is what makes the medulla so salty/hyperosmotic. The passive secretion of salt in the thin ascending limb/inner medulla and the active transport of salt out in the thick ascending limb/outer medulla creates the salty/hyperosmotic medulla.
The collecting duct traverses the salty medulla, and if the walls of the collecting duct are permeable, then water will flow out (be reabsorbed) in order to dilute the salty medulla. The vasa recta picks up this water and returns the water to the blood volume. THIS HAPPENS WHEN YOU ARE DEHYDRATED/TRYING TO CONSERVE WATER BY MINIMIZING FLUID LOSS.
IF YOU DRINK TOO MUCH WATER: the body wants to prevent your body fluid from becoming hypoosmotic. It then adjusts its water permeability of the collecting duct, making it impermeable to water, preventing the reabsorption of water and making the urine watery.
In short, the permeability of the collecting duct is adjustable, and controlled by a hormone.
When the hormone is present– the collecting duct is permeable to water
When the hormone is absent– the collecting duct is impermeable to water
The salt that the blood gains on the way down (descending limb), it loses on the way up (ascending limb). The water that the blood loses on the way down (descending limb), it gains on the way up (ascending limb)
This is known as countercurrent exchange: the exchange between 2 limbs of a vessel that are flowing in opposite directions
Regulation of Kidney Function by ADH
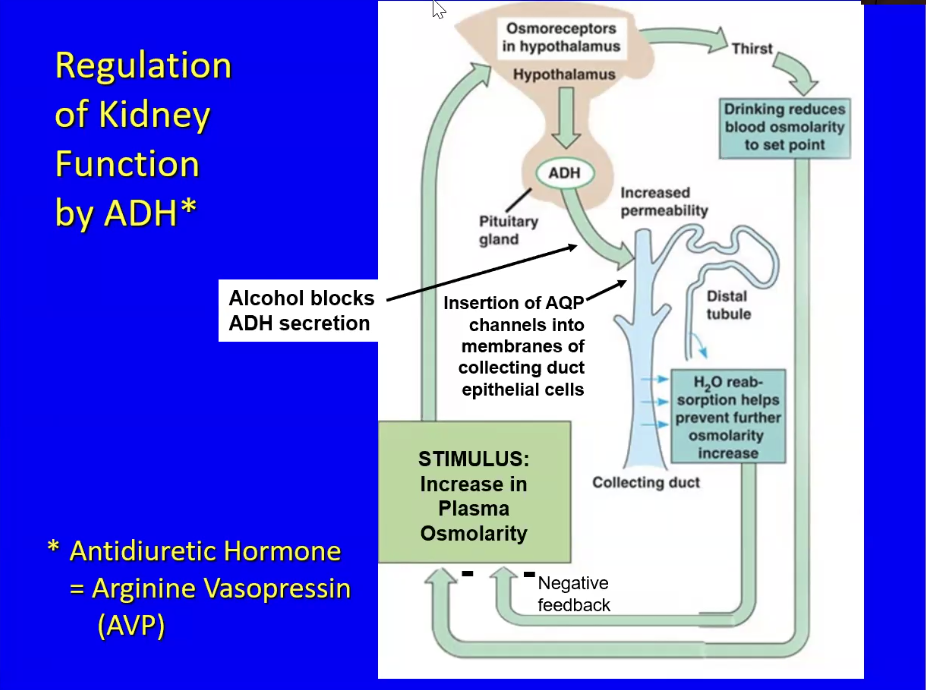
The kidney is regulated by Antidiuretic Hormone (ADH), which is also known as Arginine Vasopressin (AVP)
Diuresis refers to the production of urine, so antidiuretics = prevention of urine production
Has arginine in a key location
The picture above is an illustration of a negative feedback loop that regulates the kidney function by monitoring plasma osmolarity
An increase in plasma osmolarity (stemming from too much salt or lack of water in the blood → eating salty meals or dehydration) causes osmoreceptors in the hypothalamus to fire more nerve impulses. These impulses activate the pituitary gland to release ADH.
Alcohol blocks the secretion of ADH, which can result in increased urine output and subsequent dehydration, compounding the effects of hyperosmolarity.
The release of ADH has 3 effects
Affects collecting duct epithelial target cells
Presence of ADH causes presence of aquaporins on the apical membrane (in comparison to only the basolateral membrane). This makes both membranes permeable to water, thus stimulating the osmotic reabsorption of water. This reabsorption counteracts the initial osmolarity increase
ADH activates the hypothalamus cells that control thirst
These cells will signal thirst to the body, causing you to drink more water. When more water is drank, osmolarity is reduced down to the normal point
ADH stimulates the contraction of smooth muscle around arterioles
ADH causes arteriolar vasoconstriction all through the body, which raises blood pressure - which is where the name vasopressin comes from.
If plasma molarity is high, then all the watery components of the body lack water including plasma. This also means that blood volume is low, so the filling of the heart during diastole is low. Cardiac output will be low and so will blood pressure
Regulation of Kidney Function by RAA
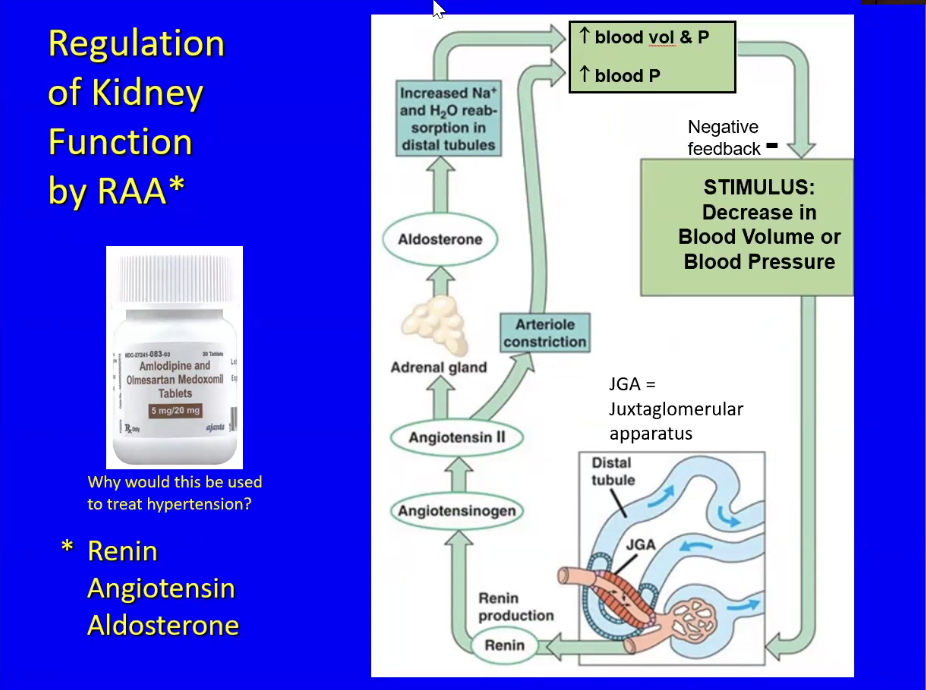
RAA = Renin Angiotensin Aldosterone
Renin → enzyme that activates the hormones below
Angiotensin → hormone
Aldosterone → hormone
In the location where the afferent arteriole supplies blood to the nephron, there is a loop of the distal tubule that passes very close to that arteriole (Juxatglomerular apparatus = JGA)
Arterioles have smooth muscle on the outside and epithelial cells on the inside
The smooth muscle at the JGA are modified to sense the flow of NaCl (from the filtrate which comes from the blood) through the distal tubule
Low blood pressure or blood volume results in less filtrate and less NaCl flow. This causes the cells to secrete Renin enzyme which will enter the blood and activate the hormone percursor angiotensinogen. Angiotensinogen will become Angiotensin II eventually
Angiotensin II has two effects
Affect on outer layer of the adrenal gland
The adrenal gland is on the outer layer of the kidney and has an outer part (adrenal cortex) and inner part. The adrenal cortex itself has 3 layer, the outer one of it contains cells with receptors for angiotensin II.
When receptors bind to angiotensin II, aldosterone is secreted.
Aldosterone is a lipophilic (not soluble in water) hormone that is synthesized from cholesterol
Is made on demand and released immediately
Aldosterone increases sodium and water reabsorption in the distal tubules. This attracts the reabsorption of chloride
This reabsorption increases the blood plasma, volume, and pressure. This means more filling during ventricle diastole. And this counteracts the initial decrease in blood pressure/volume
Stimulates the vasoconstriction of arterioles
This raises blood pressure directly without affecting blood volume, this counteracts he initial decrease in blood pressure/volume
Regulation of Kidney Function by ANH+ and Urodilatin
Is an antagonistic control system
ANH+ = Atrial Natriuretic Hormone
A hormone secreted by the atria of the heart, stimulates the excretion of sodium in the urine → this lowers blood pressure
When there is an increase in blood pressure and blood volume, the atria of the heart fill more with blood.
This overfilling of the atria, causes them to overstretch and secrete ANH+ in proportion to the amount of stretching
The release of ANH+ has 3 effects
Inhibits the release of renin from the juxtaglomerular apparatus (JGA)
remember renin’s release is the first step in RAA regulation of the kidney → so ANH+ inhibits the RAA system
Inhibits the synthesis/release of aldosterone in the adrenal cortex
This will lower BP and BV
Inhibits NaCl reabsorption (aldosterone’s effect) and ADH-stimulated water reabsorption
lowers BP and BV
Urodilation is released by the cells in the distal tubule, which respond to increased BP or BV by secreting this peptide hormone. → only has effects on the collecting duct and has the same affect as ANH+