Chapter 10: Euthanasia
section 10.2, sections 10.4-10.6
Passive euthanasia - withholding or withdrawing treatment, allowing a patient to die
Active euthanasia - active intervention aiming to bring about the death of a person (lethal injection) “mercy killing”
Physician-assisted suicide - doctors prescribe lethal medication for patients to take themselves
Voluntary euthanasia - consensual
Non-voluntary euthanasia - those who are unable to give consent (infants, people with severe brain damage)
“Just because some action might be morally permissible does not necessarily mean it ought to be legally permissible”
“If you think that it is the consequences, rather than the nature of actions themselves, that matter morally, then you can focus on those considerations. If, instead, you think that we should judge whether some action is right or wrong in itself for some reason, then you can focus on those considerations”
Consequentialist Considerations
Voluntariness matters morally only to the extent that it affects human happiness and welfare
Those dying may be the best people to make good decisions about things that primarily affect them.
The person who is dying is not the only one affected, so it can be argued that the effects on others are also relevant (emotions)
Individual decisions are not always wise and do not always work for the greatest benefit of the person making them
Someone who is ill or disabled may refuse life saving treatment for lack of money or lack of services available
(RULE UTILITARIANS) Considers the policies and practices that would maximize happiness
Such policies might place a substantial burden of proof on proposals that would deny a dying person’s wishes
Non-Consequentialist Considerations
Appeals to the value of personal autonomy in euthanasia decisions
Autonomy is good in of itself, carrying heavy moral weight
In many euthanasia cases however, a person’s mental competence and autonomy is compromised by either fear, lack of understanding, dependency, and/or hopelessness.
Moreover, depression from patients with terminal illnesses may increase desire for death
Autonomy - self-rule
How often are we fully clear about what we want?
Consequentialist Concerns (About Active Euthanasia v. Passive Euthanasia)
Rule utilitarian - concerned about the overall results or consequences of practices and policies
Nonconsequentialist Concerns
Lecture Notes
Euthanasia = intentional ending of a life to end suffering due to terminal illness.
Two main distinctions:
Active and passive
Voluntary and non-voluntary
Active and Passive Euthanasia
Active: Doing something to cause patient’s death
Illegal in US; considered immoral by AMA (America Medical Association)
Passive: Stopping treatment to allow patient to die
Is common and legal
Physician-assisted suicide is a different thing
Voluntary and Non-voluntary Euthanasia
Voluntary Euthanasia: Causing death with patient’s consent.
Includes advance directives. (Do Not Resuscitate)
Non-voluntary Euthanasia: Causing death of patient who is unable to consent.
Is not involuntary euthanasia.
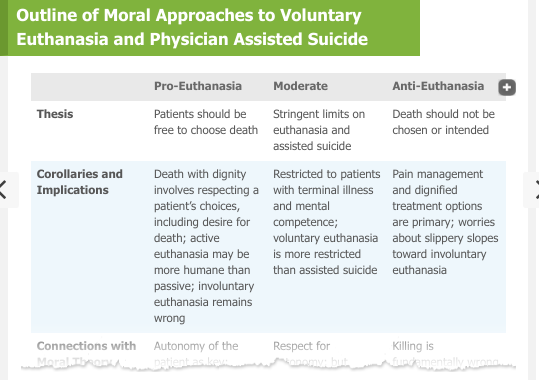
Moral Arguments about Euthanasia
Voluntariness — Patient’s right to control own life.
Utilitarian: respecting choices usually beneficial; must consider all affected.
Deontological: allowing euthanasia respects patient autonomy.
Active v. Passive Euthanasia
Act Util: euthanasia (any kind) is right if best outcome in that case.
Rule Util: active euthanasia as policy may be dangerous
Deontological: autonomy is most important
J. Gay-Williams, “Wrongfulness of Euthanasia”
Euthanasia is inherently and practically wrong.
Referring to active euthanasia only
Three arguments against (active) euthanasia
1) Euthanasia violates human nature; biology and instincts aim at living
2) Euthanasia is against patientś self-interest; death ends possibility of treatment.
3) Euthanasia may have negative practical effects on medicine; corrupts commitment to saving lives
Conclusion: (Active) euthanasia is morally wrong
Both inherently and practically.
James Rachels, “Active and Passive Euthanasia”
Active/passive distinction is morally problematic
Contradictory to only allow passive to end suffering (active also does this).
There is no moral difference between active and passive euthanasia.
Killing and letting die are the same in principle.
If patient’s life should or should not be saved, method should not matter.
Active and passive euthanasia are both actions on the part of the doctor.
Actively kills or actively withholds treatment
Doctor is no less involved in ‘passive’ euthanasia.
Conclusion: there is no moral difference between active and passive euthanasia
[Note that Rachels is not arguing for/against euthanasia; his focus is only on challenging the moral relevance of the distinction between active and passive euthanasia.]