Hepatic Dysfunction Overview
Functions of the Liver
The liver performs several vital functions:
Glucose Metabolism:
Converts glucose from meals into glycogen for storage.
In times of need, glycogen is converted back to glucose (glycogenolysis) or synthesized from amino acids (gluconeogenesis).
Ammonia Conversion:
Converts ammonia (toxic by-product) into urea for excretion.
Protein Metabolism:
Synthesizes almost all plasma proteins.
Fat Metabolism:
Breaks down fatty acids to produce energy and ketone bodies; helps in cholesterol and complex lipid synthesis.
Vitamin and Iron Storage:
Stores vitamins A, B, E, D, and iron.
Bile Formation:
Bile aids in fat digestion and is continuously produced, stored in the gallbladder.
Bilirubin Excretion:
Processes bilirubin, a waste product from the breakdown of red blood cells, and excretes it in bile.
Drug Metabolism:
Metabolizes and detoxifies drugs; important for bioavailability of medications.
Liver Disorders
Liver disorders can arise from various causes, including viruses, toxins, obesity, and metabolic conditions.
Notable diseases include cirrhosis and hepatitis.
Symptoms of Liver Dysfunction
Common signs and symptoms include:
Jaundice: Yellowing of skin and eyes due to high bilirubin levels.
Fatigue & Weakness: General lack of energy.
Malaise & Pruritus: Discomfort and itching often due to bile salt retention.
Abdominal Pain & Distension: Pain in the upper right quadrant due to liver enlargement or ascites.
Altered Mental Status: Changes due to hepatic encephalopathy.
Easy Bruising & Bleeding: Due to reduced clotting factors production.
Fluid Retention: Seen as edema and ascites due to hypoalbuminemia.
Assessment of Liver Health
Health history should focus on:
Exposure to Hepatotoxic Substances: Medications, alcohol use, travel history.
Physical Signs: Jaundice, muscle atrophy, spider angiomas, palmar erythema.
Labs & Diagnostics:
Liver Function Tests: ALT, AST, and GGT levels indicate liver cell damage.
Imaging: Ultrasound, CT, MRI help visualize liver structure.
Liver Biopsy: Determines extent of liver disease.
Complications of Liver Disease
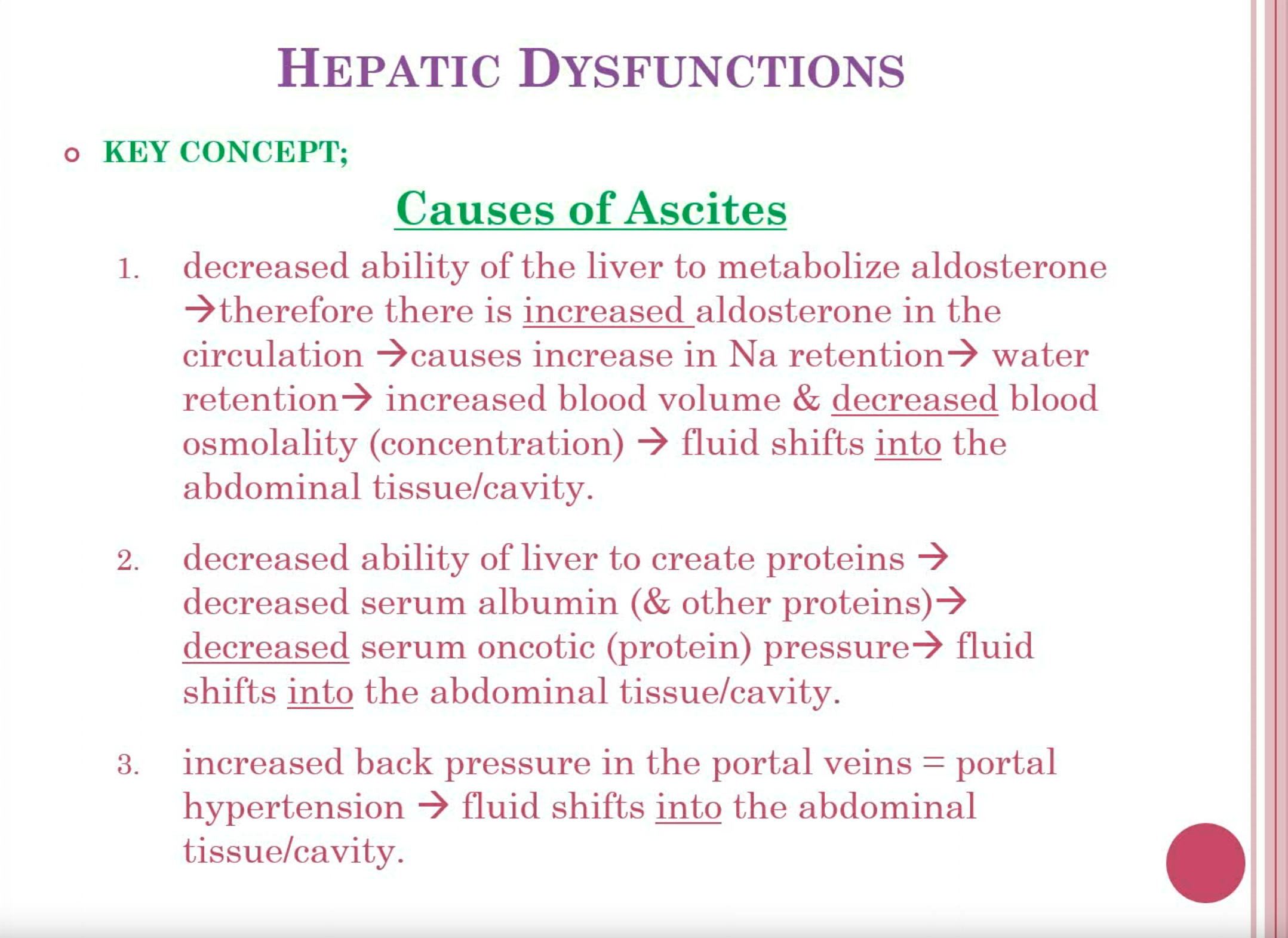
Ascites: Fluid accumulation due to portal hypertension.
DONT RESTRICT PROTEIN IN THE DIET UNTIL THE PATIENT IS CONFUSED OR HAS AN ALTERED LOC
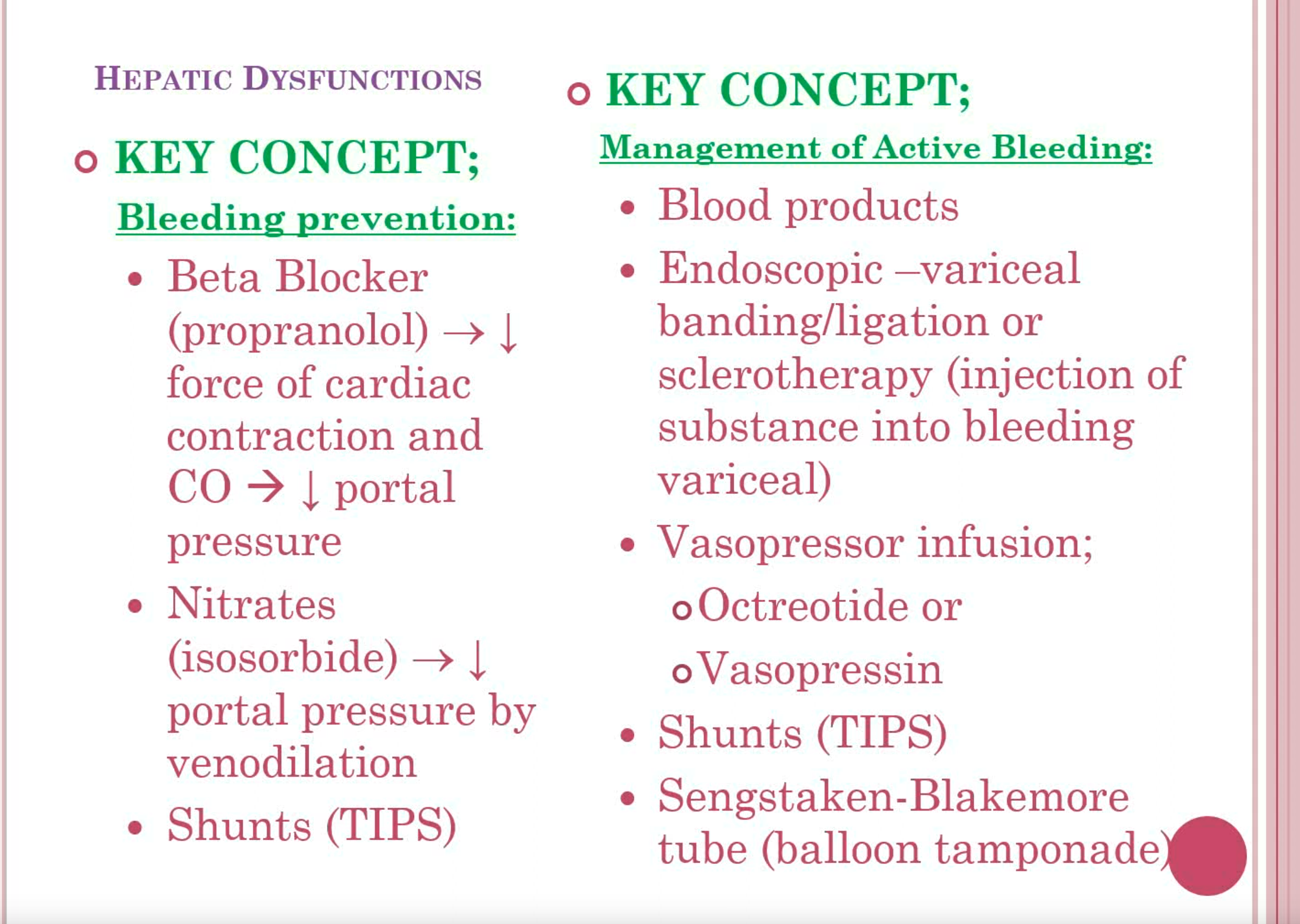
Esophageal Varices: Enlarged veins in the esophagus prone to rupture and bleed.
Varices are varicosities that develop from elevated pressure in the veins that drain into the portal system. They are prone to rupture and often are the source of massive hemorrhages from the upper GI tract and the rectum. Abnormalities in blood clotting, often seen in patients with severe liver disease, increase the likelihood of bleeding with significant blood loss. Once
esophageal varices form, they increase in size over time and may eventually bleed.
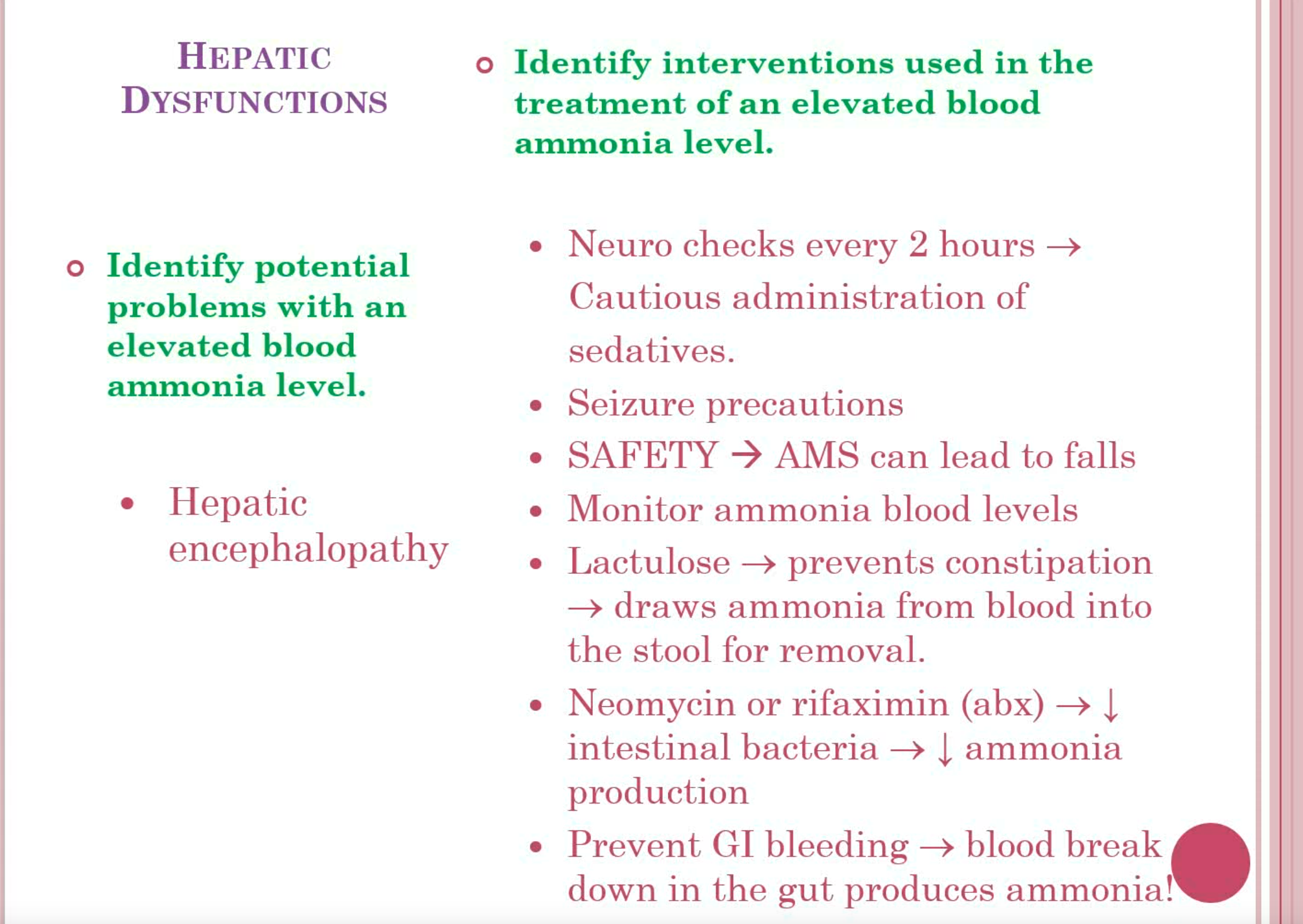
Hepatic Encephalopathy: Neurocognitive impairment caused by the accumulation of toxins like ammonia.
Portal Hypertension: Increased blood pressure in the portal venous system, leading to complications → fluid shift into the abdomen
Portal hypertension is the increased pressure throughout the portal venous system that results from obstruction of blood flow into and through the
damaged liver. Commonly associated with hepatic cirrhosis, it can also occur with noncirrhotic liver disease. Although splenomegaly may occur, the two major consequences of portal hypertension are ascites and varices
Treatment Options
Medical Management:
Dietary modifications and pharmacologic therapy for ascites and hepatic conditions.
Diuretics to manage fluid retention.
Lactulose for hepatic encephalopathy to reduce blood ammonia levels.
Surgical Interventions:
TIPS for ascites or variceal bleeding management.
An aim of a surgical shunt (TIPS )is to reduce portal venous pressure. One surgical shunting procedure is the distal splenorenal shunt, which is made between the splenic vein and the left renal vein after splenectomy
Liver transplantation is considered for irreparable liver failure.
Endoscopic procedures like sclerotherapy or banding for varices.
Nursing Care Considerations
Monitor I&O, daily weight, and abdominal girth for signs of ascites progression.
Educate patients on diet, medication adherence, and avoiding liver toxins like alcohol.
Provide psychological support to patients and families on the implications of liver disease and treatments.
Hepatitis Overview
Types of Viral Hepatitis: A, B, C, D, E—each with different transmission routes and implications.
Hepatitis A: Fecal-oral; often self-limiting.
Hepatitis B: Blood and sexual contact; can lead to chronic issues.
Hepatitis C: Primarily blood-borne; high risk of chronic liver disease.
Hepatitis D: Requires hepatitis B to cause infection.
Hepatitis E: Fecal-oral; similar to hepatitis A.
Preventive Measures: Vaccination, safe practices, and public health campaigns.
Cirrhosis & Liver Transplantation
Cirrhosis Definition: Replacement of liver tissue with fibrous scar tissue, disrupting function.
Management: Nutritional support, regular monitoring, medications for symptom management and hormone imbalances.
Liver Transplantation: Considered for ESLD; involves comprehensive assessment for candidacy and post-operative care to prevent complications.
Conclusion
Understanding liver functions, disorders, and management strategies is essential for providing effective nursing care in hepatic dysfunction cases.