12_-_Immune_systems
Lecture Notes
Immune system → system that defends the body from harm
Behavioral immune system → defensive behaviors to protect the body. Defines the immune system beyond the simple bodily systems.
Feelings of disgust towards a disfigured person
Pregnant women affinity for the smells of genetically similar males (family) because they have genetic interest of keeping her protected. They are xenophobic to foreign things because they want stability.
Innate immune system → general defense that does not target anything specific
Four major features:
Outside barrier (skin): Separate in and out.
Lysozymes (mucus, saliva, tears): Guards the openings. Enzymes that break down the cell walls of bacteria.
Phagocytes (eating cells, amoebocytes, macrophages and neutrophils in humans, haemocytes in insects)
Ex: Haemocytes and the melanization cascade: When a pathogen invades, haemocytes recognize it and initiate the melanization process. This cascade leads to oxidation of phenolic compounds, resulting in the production of melanin. Melanin ultimately helps to immobilize and kill the pathogens.
Are macrophages homologous or analogous to phagocytes? → Homologous. a. Overlap in toll receptors. b. Similar responses to the same medications
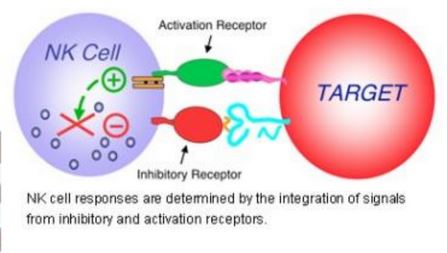
Natural killer cells → identify and eliminate tumor cells and infected cells by recognizing stressed cells.
Fluid (proteins with an affinity for pathogens, detect pathogens and poke holes in them to kill them.)
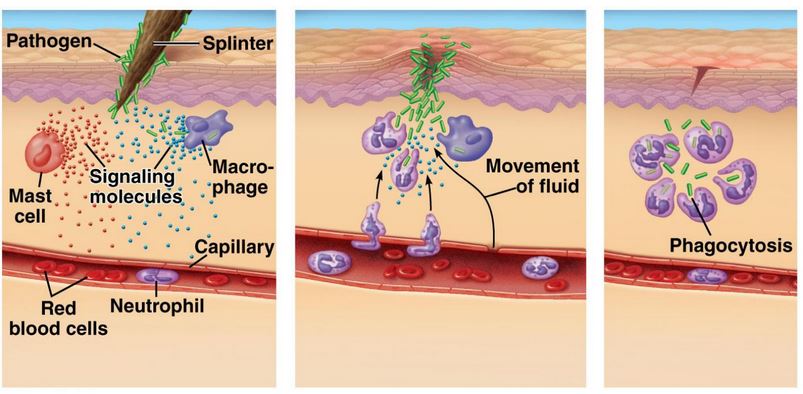
Inflammatory immune repsonse → adaptation to keep damage/infection localized
Damage happens
Mast cells release histamine
Histamines trigger phagocyte release and vasodilation for greater blood flow to the area.
Excess buildup causes swelling and inflammation
Ways to reduce inflammation: Ice and antihistamines. Allows for exposed pathogens to travel further into your body. These delay the onset of healing.
Adaptive immune system → Darwinian machine that has specific defense against particular pathogens
Why is it needed?
Human generation time is 20 years old
PROBLEM. Bacteria evolve much faster.
The adaptive immune system has this same adaptive capacity of cloning and proliferation in repsonse in variation.
It operates on the priciples of natural selection to give itself an advantage against bacteria.
Variation
Conseuqences
Hertability
SOLUTION. Throw everything at the pathogen, identify what works, and make copies of it (proliferation). Comfort is not the priority.
After proliferation, some cells further operate to kill the pathogen (effector cells), some go dormant and serve as a blueprint for the type of cells that need to be made, (memory cells).
Produce endless variation of protein receptors to throw at a pathogen, find which one works, and proliferate.
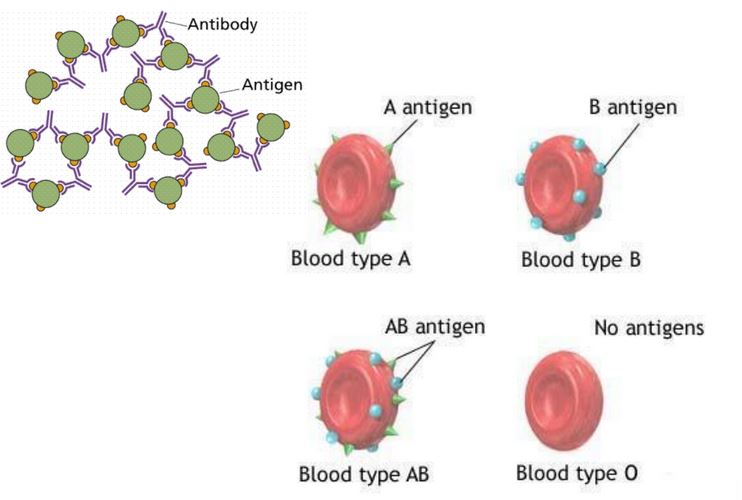
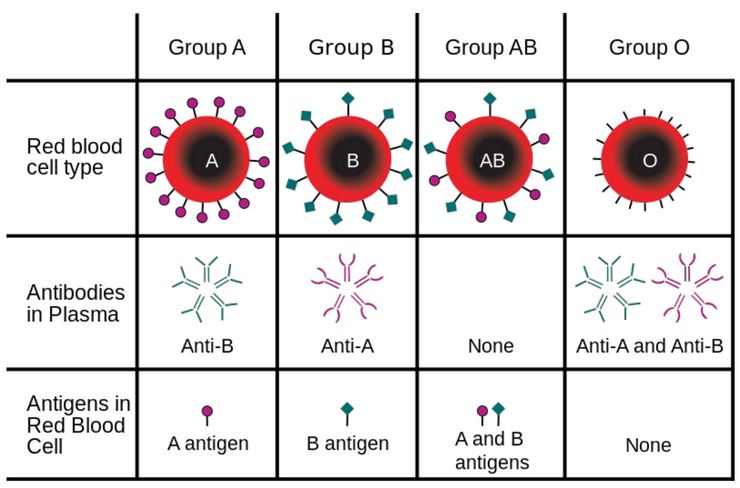
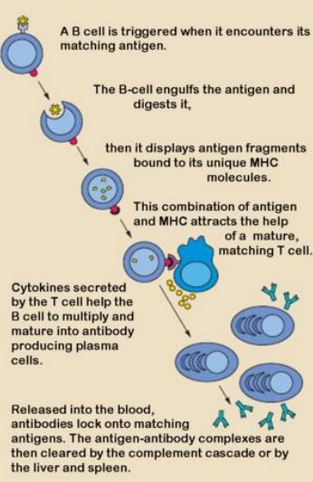
Antibodies: Proteins produced by B cells in response to specific antigens that identify and neutralize pathogens. Circulate in the blood and help mark invaders for destruction.
Antigens: Proteins that engage with immune receptors. Found on the surface of pathogens that are recognized by antibodies or T cells. Trigger an immune response by eliciting the production of antibodies or activating T cells, labeling them as foreign entities.
How does it work practically? → B side (humoral) and T side (cell-mediated)
B cells: Makes antibodies (humoral)
B cells bind with antigen and start proliferating. Makes effector cells, memory cells, and antibodies.
Anti-venom: Antibodies for snake venom
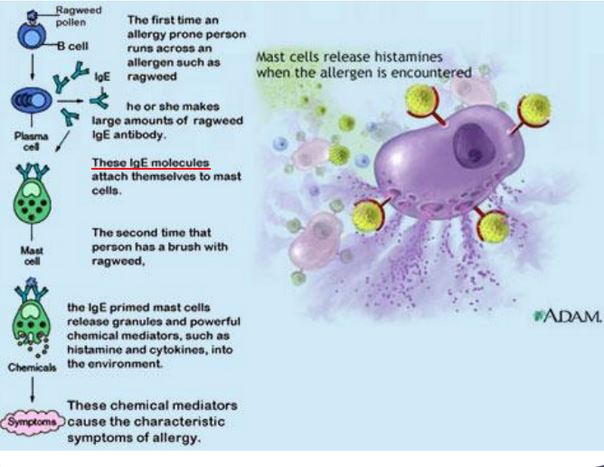
Allergies are triggered when antibodies attach to mast cells. The second time they have an interaction with the allergen, the primed mast cells release histamines.
Antigens can be used to find the specific receptors to turn in off and prevent this allergen response via a shot.
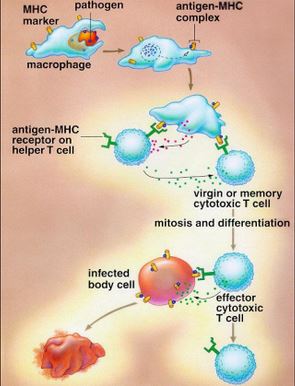
T cells: Makes cytotoxic T-cells
1. Antigen Recognition: Helper T cells are activated when their receptors (TCR) recognize specific antigens presented on MHC (Major Histocompatibility Complex) molecules.
CD8+ T cells recognize antigens presented by MHC I on all nucleated cells, responding to intracellular pathogens.
CD4+ T cells interact with antigens presented by MHC II on antigen-presenting cells (APCs) like macrophages and dendritic cells, responding to extracellular pathogens.
2. Costimulation: For a full activation, T cells require additional signals. This occurs when interactions between co-stimulatory molecules on the T cell and the APC, is provided.
3. Clonal Expansion: Once activated, the T cells undergo clonal expansion, where they proliferate and differentiate into effector and memory T cells. Effector T cells are responsible for the immediate immune response, while memory T cells remain in circulation for long-term protection against future infections.
Cytotoxic T cells (CD8+) kill infected host cells directly.
Helper T cells (CD4+) release cytokines that coordinate the immune response, enhancing the activity of B cells and other immune cells, promoting inflammation and recruiting more white blood cells to the site of infection. Also function as memory cells.
4. Memory Formation: After the elimination of the pathogen, some of the T cells remain as memory cells. These cells persist in the body for years and provide a faster and more robust response in case of re-exposure to the same pathogen.
Summary of T cells and B cells:
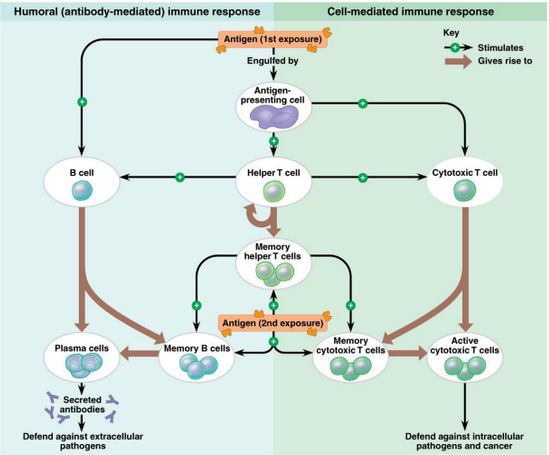
Vaccines give antigens to start the production of helper T-cells. Gives a head start in immune response.
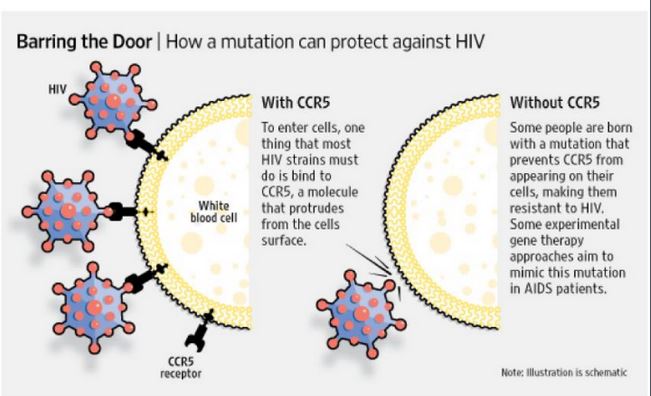
HIV → targets helper T cells via CCR5 recpetors, weakens immune systems making you more vulnerable disease.
People who are immune to HIV don’t have the CCR5 receptors, they have a different one.
This mutation is common in european populations because of the plague
The -CCR5 variant was favoured during the plague. This was determined by examining the history of neutral mutations.
Giving bone marrow of people who have this mutation can provide others with immunity for HIV.
Another way of doing this is binding an antibody at CCR5 receptors via IgG4 monoclonal antibodies directed to CCR5.
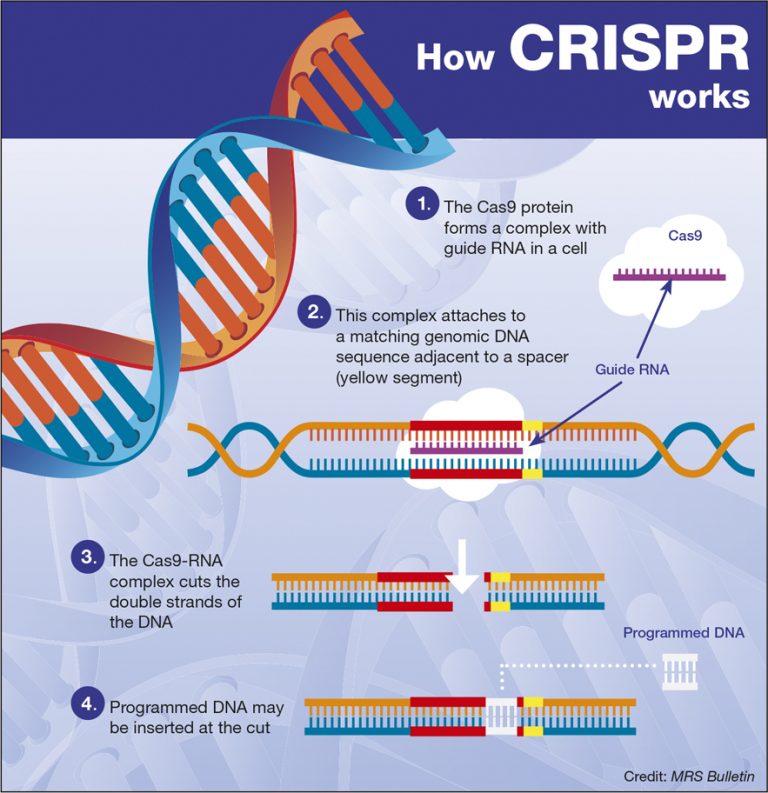
CRISPR → Genome editing technology
Adding and subtracting genes
Deactivating and reactivating genes
Functions via the bacterial immune system
Bacteria gets attacked by a virus
It makes fragmented/complementary copies of the viral DNA stored into it’s own genome
Virus shows up again, random complementary copies stick to that viral DNA.
Cas-9 cutting tool cuts where the copies stuck to to kill the virus
This serves as a method of storing information for next time.
A bad copy of a gene can be cut out and replaced via Cas-9 by inserting the undesired gene into CRISPR Cas-9.
The hole can then be filled by prepping the desired gene that overlaps with the open nucleotides.
BUG questions
How was it demonstrated that sponges have an immune system?
Demonstrated through their ability to recognize and reject cells that are not their own → Amoebocytes act like white blood cells in sponges by attacking and removing
TOLL-like receptors that allow for cell-to-cell recogniition
When cells from different sponge strains, they undergo lytic (killing) activity similar to that of higher animals
Sponges have an immune systems through the presence of immune cells.
Sponges contain cellular components similar to immune cells in more complex organisms (e.g., amoebocytes, phagocytes).
Experiments show sponges can recognize and respond to foreign materials.
What are the four main features of the innate immune system?
1. Barrier defense (skin)
2. Lysozymes (enzymes that kills cells to guard entrances to barriers)
3. Cell-mediated response (kills everything that is not wanted)
4. Fluid response → blood clotting.
Present at birth and provides immediate defense against infections.
How is it that the innate system is not adaptive within generations but can still be effective against quickly evolving agents? (think of how TOLL receptors have changed very little over time yet are still effective)
Remains effective because it targets highly conserved features of pathogens (parts essential for pathogen survival)
TOLL receptors are passed down in generations and have evolved to recognize certain molecular patterns, allowing them to recognize a wide range of attackers.
The innate immune system is not adaptive across generations, yet it effectively combats quickly evolving agents.
Conserved mechanisms and components contribute to its effectiveness.
TOLL receptors have changed very little over time, allowing the system to maintain its functionality.
This allows recognition of common patterns found in various pathogens.
The innate immune system can efficiently respond to diverse and rapidly changing microbial threats without needing generational adaptation.
How do we know that amoebocytes, hemocytes, and phagocytes are homologous?
They all share similar functions, and responses to threats
They typically reject each other when placed in similar environment but
Amoebocytes, hemocytes, and phagocytes share common structural and functional characteristics.
They all partake in the immune response across different organisms.
Genetic and molecular studies indicate similarities in their origins and developmental pathways.
The presence of analogous genes across species reinforces their homologous relationship.
What is a way to target the insect immune system with pesticides without harming ours?
Melanization cascade allows insects to encapsulate pathogens with melanin, killing the insect. Humans don’t have this, which is why humans are not affected by pesticides.
Develop pesticides that specifically inhibit enzymes or receptors unique to insects.
Utilize biochemical pathways that are present in insects but absent in humans and other vertebrates.
Apply compounds that disrupt insect signaling molecules without affecting similar processes in higher organisms.
Create genetically engineered biopesticides that only activate in the presence of insect-specific immune responses.
What is the difference between innate and adaptive immunity?
Innate Immunity (general):
Present at birth and provides immediate defense against infections.
Non-specific: responds to all pathogens in the same way.
Includes physical barriers (e.g., skin, mucous membranes) and immune cells (e.g., phagocytes, natural killer cells).
Does not have memory; the response is the same upon each exposure.
All animals have it
Adaptive Immunity (specific):
Develops over time and is specific to particular pathogens.
Involves the activation of lymphocytes (B cells and T cells) that respond to specific antigens.
Memory component: provides a stronger and faster response upon subsequent exposure to the same pathogen.
Typically takes longer to mount a response compar
What are the similarities of the invertebrate and vertebrate innate immune systems?
Similarities: non-specific denfenses that recognize geenral features of pathogens. Contain TOLL-like receptors. Barrier defenses. Protective enzymes (lysozymes). Amoebocytes function similarly to phagocytes in that they consume things and kill them.
These similarities suggets that the innate immune system is ancient
Both invertebrates and vertebrates possess immune systems that are present at birth and can respond immediately to infectious agents.
They rely on physical barriers (like skin and mucous membranes) to prevent pathogen entry.
Both systems utilize phagocytic cells to engulf and eliminate pathogens.
Pattern recognition receptors (PRRs) are present in both types of immune systems, allowing the recognition of common pathogen-associated molecular patterns (PAMPs).
The innate immune responses in both groups are non-specific, targeting a wide range of pathogens without adapting for specific strains or species.
Both invertebrates and vertebrates exhibit inflammatory responses as a mechanism to defend against infection and injury, involving increased blood flow and recruitment of immune cells to the site of infection.
What is inflammation? What are the steps of the inflammatory response?
Inflammation is the body's response to injury or infection, characterized by redness, swelling, heat, and pain. It is a protective mechanism that aims to eliminate the initial cause of cell injury, clear out necrotic cells and tissues, and initiate the healing process. Only vertebrates do it.
Steps of the Inflammatory Response:
Mast cells detect danger and release histamines
Histamine signal phagocytes to move towards the damage poitn
Vasodilation increases blood flow to that area
Phagocytes consume pathogens
The large amount of contents and fluids causes the inflammation.
Injury or Infection: Tissue is damaged by physical injury, pathogens, or immune responses.
Release of inflammatory mediators occurs, such as histamines, prostaglandins, and cytokines.
Vasodilation: Blood vessels dilate to increase blood flow to the injured area.
This leads to redness and heat at the site of inflammation.
Increased Permeability: Blood vessel walls become more permeable, allowing fluid, proteins, and immune cells to enter the affected tissues.
This results in swelling (edema).
Leukocyte Recruitment: White blood cells (leukocytes) are attracted to the site through chemotaxis.
Neutrophils typically arrive first, followed by monocytes that become macrophages.
Phagocytosis: Immune cells engulf and digest pathogens and debris.
This is crucial for clearing the infection and initiating tissue repair.
Resolution of Inflammation: Once the threat is eliminated, the inflammatory response subsides.
Anti-inflammatory signals are released to promote healing and return the tissue to its normal state.
How does the application of ice counteract the inflammatory response?
Vasoconstriction: Ice causes blood vessels to constrict, reducing blood flow to the affected area. This limits the amount of inflammatory mediators and immune cells accessing the site, helping to minimize swelling and inflammation.
Reduced Metabolism: Cooling the tissues slows down metabolic processes, which can decrease the release of inflammatory mediators and reduce tissue damage.
Pain Relief: The cold sensation can numb the area, providing analgesic effects and reducing pain associated with inflammation.
Decreased Permeability: Ice application can decrease the permeability of blood vessel walls, which helps to reduce the escape of fluid and proteins into the surrounding tissues, thus limiting edema (swelling).
Inhibition of Inflammatory Pathways: Cold applications may also inhibit certain biochemical pathways involved in inflammation, further reducing the response.
Why is the adaptive immune system considered a Darwin Machine?
It operates under principles of Variation, Consequences, and Heritability, akin to Darwinian evolution. Here are key points on its operations:
Variation: Within the pool of B and T lymphocytes, there is a vast diversity of receptors through genetic recombination. Each receptor variant can recognize different antigens. This variation is crucial for the immune system's ability to respond to a wide range of pathogens.
Consequences: When a pathogen invades, only those lymphocytes whose receptors specifically bind to the pathogen's antigens are selected for activation and proliferation. This selective activation ensures that the immune response is tailored to effectively combat the specific threat.
Heritability: After the infection is cleared, some of the activated lymphocytes turn into memory cells. These cells persist long-term in the body, allowing for a faster and more robust response upon subsequent exposure to the same pathogen, demonstrating retention of effective adaptive strategies.
Do bacteria and archaea have adaptive immune systems?
Bacteria and archaea do have adaptive immune systems like vertebrates.
They possess a form of adaptive immunity known as CRISPR-Cas systems.
CRISPR-Cas allows them to store segments of viral DNA.
This system enables recognition and targeting of subsequent infections by the same viruses.
Provides a specific form of immunity that can improve over time.
Mechanisms and complexities differ significantly from those in higher organisms.
What is the CRISPR? How can it be useful for treating genetic disorders?
CRISPR is a revolutionary tool for editing genes, allowing scientists to modify DNA sequences. Part of bacterial immune system that can recognize bacterial sequences and store it to memory.
It utilizes a system derived from the immune mechanisms of bacteria to target and cut specific DNA sequences.
The versatility of CRISPR enables precise alterations to the genome, including gene knockouts and replacements.
This technology can be highly beneficial in treating genetic disorders by correcting mutations at their source.
Potential applications include curing hereditary diseases, altering genes associated with cancer, and developing personalized medicine.
CRISPR can also aid in research by allowing the study of genes and their functions, enhancing our understanding of various biological processes.
What is the vertebrate humoral (fluid) response? What is the cell-mediated response?
The vertebrate humoral response involves the production of antibodies by B cells in response to specific antigens. Antibodies target invaders and proliferat ewhen they find a match before the invasion can spread.
Antibodies circulate in the blood and lymph, identifying and neutralizing pathogens or marking them for destruction.
This response provides long-lasting immunity through the formation of memory B cells, which can quickly respond upon re-exposure to the same pathogen.
The cell-mediated response, on the other hand, is centered around T cells, particularly Helper T cells and Cytotoxic T cells.
Helper T cells (killer cells) activate destroy and coordinate the immune response by stimulating B cells and other immune cells.
Cytotoxic T cells directly target and destroy infected or cancerous cells.
What role does a B plasma cell play in an allergic response? (think antibodies)
B plasma cells play a crucial role in the allergic response by producing antibodies known as Immunoglobulin E (IgE) which attach to the antigen and multiply, the receptors on the B cells then shed off the cells and become antibodies.
IgE antibodies bind to allergens, which are the substances that trigger allergic reactions.
When B cells are activated by exposure to an allergen, they differentiate into plasma cells that specifically produce IgE.
The binding of IgE to allergens leads to the activation of mast cells and basophils, which release histamines and other inflammatory mediators, contributing to the symptoms of an allergic reaction.
As a result, B plasma cells are integral in mediating the immune system's response to allergens, enhancing the sensitivity to these substances upon re-exposure.
What are IgE molecules?
IgE (Immunoglobulin E) is a type of antibody.
Bound to mast cells found in loose connective tissue which release histamines.
Mast cells cannot release histamine until IgE binds to it.
Produced by B plasma cells in response to allergens.
Plays a critical role in the immune system's allergic response.
Binds specifically to allergens, triggering allergic reactions.
Activation of mast cells and basophils occurs upon binding.
Leads to the release of histamines and inflammatory mediators.
Causes various allergic symptoms, such as itching, swelling, and difficulty breathing.
Why is it that the second exposure to an allergen, and not necessarily the first, provokes the allergic inflammatory response?
The first exposure to an allergen sensitizes the immune system. It doesn’t have a default reaction.
B cells produce IgE antibodies specific to the allergen.
IgE antibodies bind to mast cells and basophils.
Upon subsequent exposures, the allergen binds to the pre-existing IgE and memory T-cells.
This triggers mast cells and basophils to release histamines and inflammatory mediators.
The result is a rapid and amplified allergic inflammatory response, unlike the initial exposure, which may not have triggered a response yet.
The immune system thus reacts more vigorously during the second exposure due to the sensitization from the first exposure.
How does the drug work that eliminates allergic responses
Corticosteroids and anti-histamines targets the IgE antibodies, reducing their levels in the body.
By lowering IgE, the activation of mast cells and basophils is diminished.
This reduction prevents the release of histamines and other inflammatory mediators during allergen exposure.
The drug may also block the binding sites for allergens on IgE, preventing allergic reactions from occurring.
Overall, the drug aims to minimize or eliminate the symptoms of allergic responses effectively, allowing the body to tolerate allergens better without triggering inflammation.
What role does the Helper T-Cell play in eliciting immune responses? How does HIV affect this process?
Helper T cells (identification agents that determines what’s good and what’s bad) are crucial for initiating and regulating immune responses.
They activate other immune cells by releasing cytokines, enhancing the actions of B cells and cytotoxic T cells.
B cells produce antibodies against specific antigens, while cytotoxic T cells target and destroy infected cells.
HIV specifically attacks and depletes Helper T cells, weakening the immune system's ability to combat infections because ti can’t recognize what good and what;s bad.
The loss of Helper T cells hinders the activation of B cells and cytotoxic T cells, leading to increased vulnerability to opportunistic infections and diseases.
This disruption in the immune response is a hallmark of HIV infection, progressing to AIDS when Helper T cell levels become critically low.
How are some people naturally immune to HIV? How has a novel medicine used this approach?
Certain individuals have natural immunity to HIV due to genetic factors.
This immunity is often linked to mutations in the CCR5 gene, which HIV uses to enter cells.
People with the CCR5-Δ32 mutation lack functional CCR5 proteins, preventing HIV infection.
Novel medical approaches aim to mimic this natural immunity. Pro 140-IG4 a monoclonal antibody blocks tEe CCR5 receptor in helper T cells to protect them from being attacked by HIV.
Gene editing technologies like CRISPR can induce similar mutations in cells, making them resistant to HIV.
Therapies that block or alter the CCR5 receptor are under development to prevent HIV entry into host cells.
These methods utilize the principles of natural immunity to enhance treatment efficacy and potentially achieve a functional cure for HIV.
Why don’t Cytotoxic T Cells interact with cells that have MHC II (interact w CD4) rather than MHC I (interacts with CD8) compounds?
Cytotoxic T Cells do not interact with cells displaying MHC II compounds for several reasons:
MHC II Role: MHC II molecules primarily present antigens from extracellular pathogens to CD4+ T cells (Helper T cells).
Cytotoxic T Cell Function: Cytotoxic T Cells (CD8+ T cells) are designed to recognize and kill infected or cancerous cells by interacting with MHC I molecules.
Pathway Specificity: MHC I and MHC II serve different immune pathways; MHC I is crucial for presenting intracellular antigens to Cytotoxic T Cells.
Lack of Affinity: Cytotoxic T Cells lack the necessary receptors to bind to MHC II antigens, which prevents interaction.
Immune Response Coordination: This specificity is essential for coordinating an effective immune response, directing Cytotoxic T Cells specifically to infected or abnormal cells.
Activation of the cell-mediated pathway does what to the humoral pathway? What does this mean for individuals that live in a sterile environment?
Activation of the cell-mediated immune pathway can influence the humoral immune response.
Cell-mediated pathway strengthens immune system because it makes memory cells
A lack of pathogens results in immune responses being more frequent to less harmful things and being more severe. This is why you don’t want to avoid exposure to the environement to create those T-memory cells.
The activation of cytotoxic T cells through the cell-mediated pathway can lead to increased production of antibodies by B cells in the humoral pathway.
This interaction ensures a coordinated immune response, enhancing the body's ability to eliminate pathogens effectively.
In individuals living in a sterile environment, the lack of exposure to pathogens may result in diminished activation of the adaptive immune system, including both cell-mediated and humoral responses.
Such environments can hinder the development of memory cells and the overall robustness of the immune system, increasing susceptibility to infections when exposed to pathogens after prolonged periods of sterility.
Jeopardy and quiz questions:
Quiz questions:
How does monoclonal antibody treatment for HIV work? → It binds to the CCR5 receptor of T cells so HIV will be unable to bind to it. Some europeans have this allele which causes them to not express the CCR5 receptor
Which component of the immune system would best neutralize intracellular pathogens → Cytotoxic t cells. CD8 recognizes MHC1, CD4 recognizes MHC2
Where would you expect the highest percent of immune compilations to be reported? → New York City
Why is the respiratory system of birds more efficient to that of humans? → Air flows in one direction through the lungs. Unidirectional air flow
What is not one of the principle themes of Darwinian medicine? → Evolution of viruses. 1) Evolutionary arms races 2) Symptoms as adaptations 3) Evolutionary mismatches
It is said that the human body is mostly water, where is most of this water? → Cytoplasm
Jeopardy notes:
What changes occur form spermatids to sperm? → Not attached to other cells, exocytose the cytoplasm, condense DNA, forms acrosome
What is the purpose of a coelom → more mobility
Is countercurrent flow good or bad? → Good, more efficient becuase it maintains a concentrations gradient of oxygen between blood and air so that air is always being exchanged.
What are the respective fluids found outside blood vessels, lymph vessels, and inside lymphatic vessels? → interstitial fluids, lymphatic fluid, plasma
How do hormones affect osteoporosis and why is it more common in older females? Osteoblasts make new bones. Osteoclasts destoy bone. estrogen increases the rate at which osteoblasts work. After menopause, less estrogen leads to less dense bones.
What is meiotic drive? → evolutionary force in which chromosomes compete for access to the egg during reproduction
Which type of organism relies on direct contact with the environment for gas, nutrient, waste exchange? → unicellular organisms
Do humans or birds or birds have optimal gas exchange? → Birds because of unidirectional air flow.
How does childhood activity affect the onset of osteoporosis → Increased use, your body will develop stronger bones
Is polyspermy common? → No. The fast block and slow block prevent multiple sperm from fertilizing the egg.
What does the hypothalamus secrete? → GNRH (gonadotropin releasing hormone) which releases gonadotropin from the anterior pituitary gland which then releases LH and FSH
Why is it good to grow up with dogs? → more exposure, more developed immune system
What is a pro and con of asexual reproduction → Con: Buildup of deleterious genes, no variation. Pros: Fast, all good traits will be passed down.
What is the grandmother hypothesis? → Menopause allows grandmas to take care of children rather than making their own so that their daughter can make babies.
What does nuns disease → Nuns are more likely to get breast cancer because their hormones are imbalanced because they don’t have sex and estrogen levels are high.
What are the benefits of sexual reproduction → recombination adds variation and reduces genetic load (bad genes)
What are the two effects of progesterone? Estrogen establishes. Progesterone protects. 1. Maintains pregnancy by preventing uterine contractions, 2. promotes the thickening of the uterine lining.
How does menstruation occur? → shedding of uterine lining after no fertilization
Adaptive benefits of counter current exchange → always maintains a concentrations gradient. More exchange across the entire gill surface
What are the costs of sexual reproduction → slow, more costly, half of the population can reproduce, while the others cannot and consume resources at the same time.
Why were living creature bigger in the past? → more O2
Where does gas exchange occur in fish → gills
Does icing a body part help? → no because vasoconstriction
What is the function of the corpus luteum? → Produces estrogen and progesterone.