Chapter 28:Development and Inheritance
Fertilization

Fertilization occurs when a sperm and an oocyte (egg) combine and their nuclei fuse.
This new single cell, called a zygote, contains all of the genetic material needed to form a human half from the mother and half from the father.
During the journey, fluids in the female reproductive tract prepare the sperm for fertilization through a process called capacitation, or priming.
Contact Between Sperm and Oocyte
The corona radiata is an outer layer of follicular (granulosa) cells that form around a developing oocyte in the ovary and remain with it upon ovulation.
The underlying zona pellucida (pellucid = “transparent”) is a transparent, but thick, glycoprotein membrane that surrounds the cell’s plasma membrane.
The acrosomal reaction in which the enzyme-filled “cap” of the sperm, called the acrosome, releases its stored digestive enzymes.
The mucopolysaccharides then coat the nascent zygote in an impenetrable barrier that, together with hardened zona pellucida, is called a fertilization membrane.
Embryonic Development

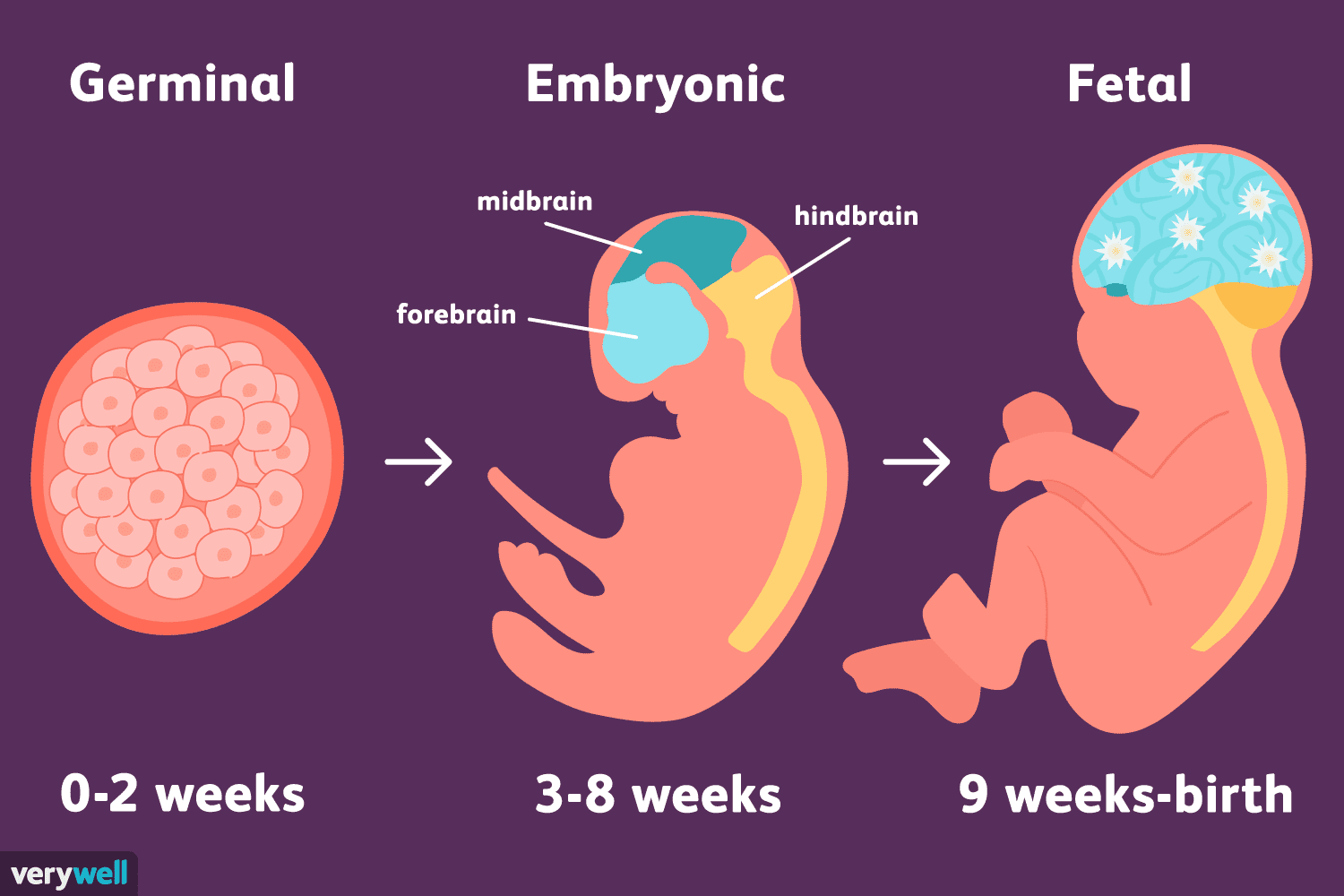
The period of time required for full development of a fetus in utero is referred to as gestation (gestare = “to carry” or “to bear”).
A developing human is referred to as an embryo during weeks 3–8, and a fetus from the ninth week of gestation until birth.
Pre-implantation Embryonic Development
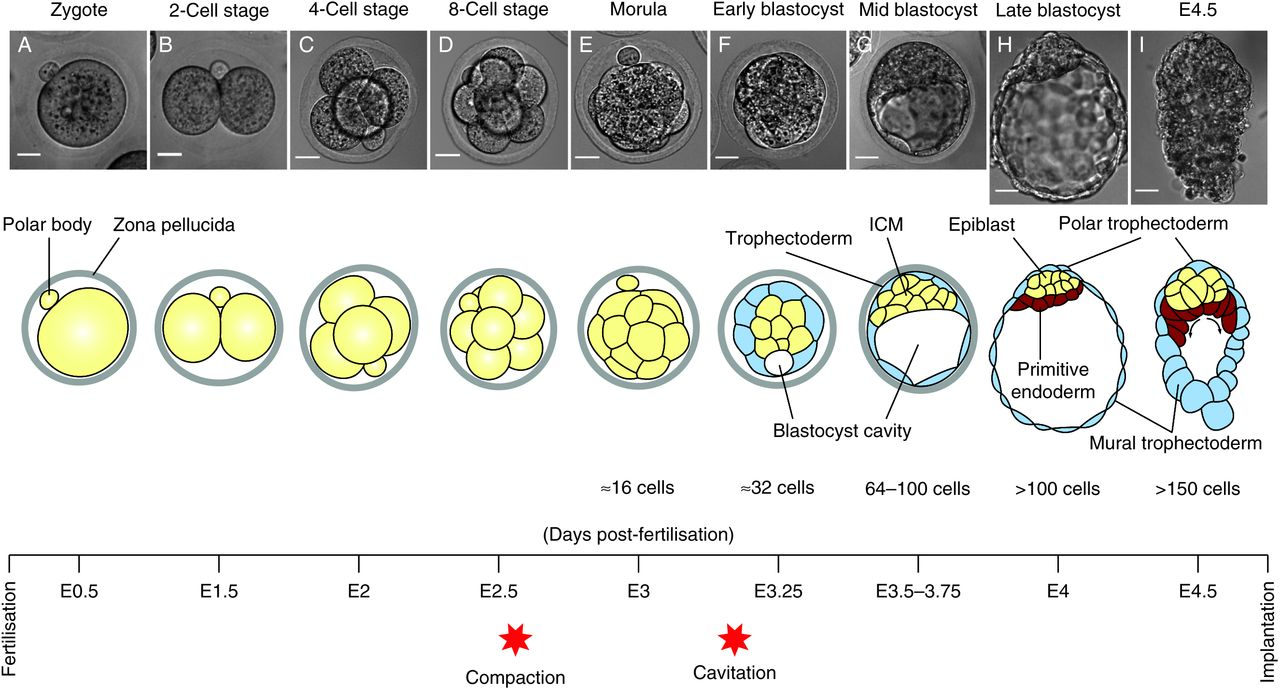
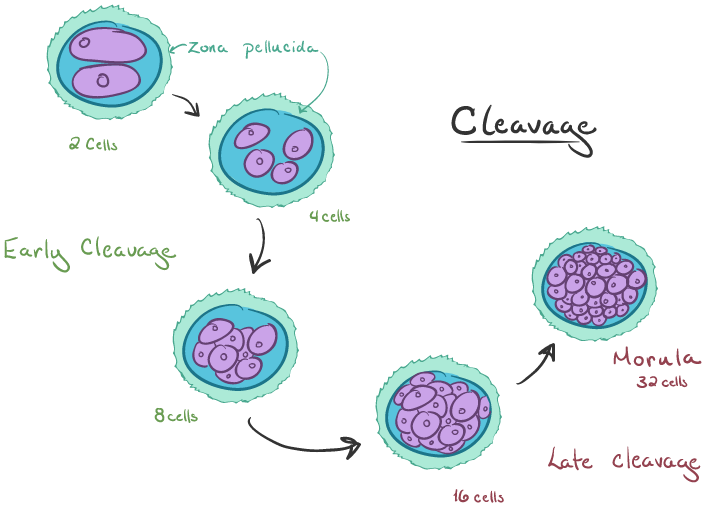
Following fertilization, the zygote and its associated membranes, together referred to as the conceptus, continue to be projected toward the uterus by peristalsis and beating cilia.
Although each cleavage results in more cells, it does not increase the total volume of the Conceptus.
Each daughter cell produced by cleavage is called a blastomere (blastos = “germ,” in the sense of a seed or sprout).
The name given to this structure is the morula (morula = “little mulberry”).
The ball of now tightly bound cells starts to secrete fluid and organize themselves around a fluid-filled cavity, the blastocoel. At this developmental stage, the conceptus is referred to as a blastocyst.
The cells that form the outer shell are called trophoblasts (trophe = “to feed” or “to nourish”).
These cells will develop into the chorionic sac and the fetal portion of the placenta (the organ of nutrient, waste, and gas exchange between mother and the developing offspring).
Implantation
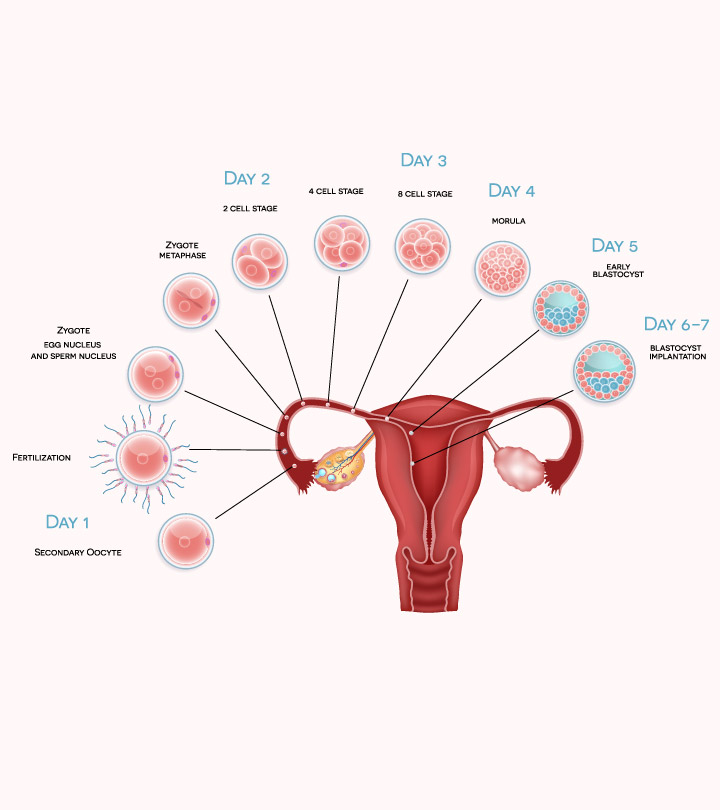
At the end of the first week, the blastocyst comes in contact with the uterine wall and adheres to it, embedding itself in the uterine lining via the trophoblast cells.
The process of implantation, which signals the end of the pre-embryonic stage of development.
When implantation succeeds and the blastocyst adheres to the endometrium, the superficial cells of the trophoblast fuse with each other, forming the syncytiotrophoblast, a multinucleated body that digests endometrial cells to firmly secure the blastocyst to the uterine wall.
The trophoblast secretes human chorionic gonadotropin (hCG), a hormone that directs the corpus luteum to survive, enlarge, and continue producing progesterone and estrogen to suppress menses.
In one to two percent of cases, the embryo implants either outside the uterus (an ectopic pregnancy) or in a region of uterus that can create complications for the pregnancy.
If the embryo implants in the inferior portion of the uterus, the placenta can potentially grow over the opening of the cervix, a condition called placenta previa.
Embryonic Membranes
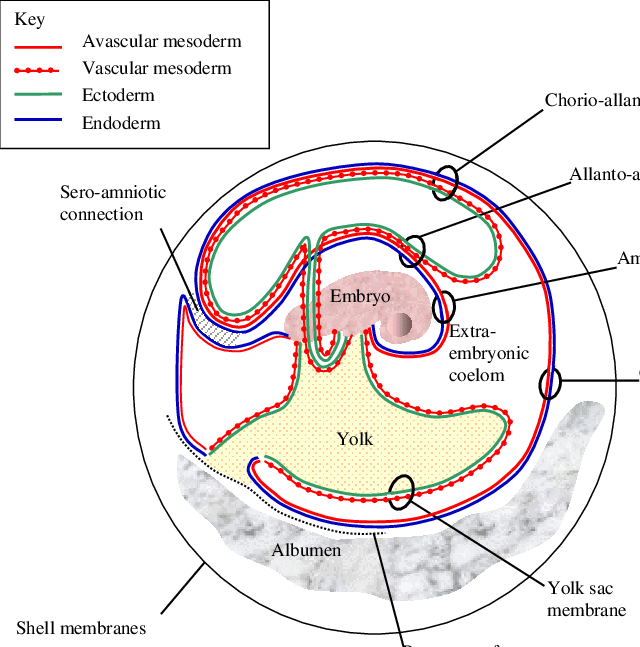
At the beginning of the second week, the cells of the inner cell mass form into a two-layered disc of embryonic cells, and a space the amniotic cavity opens up between it and the trophoblast.
Cells from the upper layer of the disc (the epiblast) extend around the amniotic cavity, creating a membranous sac that forms into the amnion by the end of the second week.
On the ventral side of the embryonic disc, opposite the amnion, cells in the lower layer of the embryonic disk (the hypoblast) extend into the blastocyst cavity and form a yolk sac.
During week 3, a finger-like outpocketing of the yolk sac develops into the allantois, a primitive excretory duct of the embryo that will become part of the urinary bladder.
The last of the extra-embryonic membranes is the chorion, which is the one membrane that surrounds all others.
Embryogenesis
As the third week of development begins, the two-layered disc of cells becomes a three-layered disc through the process of gastrulation, during which the cells transition from totipotency to multipotency.
The first layer is the endoderm, a sheet of cells that displaces the hypoblast and lies adjacent to the yolk sac.
The second layer of cells fills in as the middle layer, or mesoderm.
The cells of the epiblast that remain (not having migrated through the primitive streak) become the ectoderm.
Development of the Placenta

The placenta connects to the conceptus via the umbilical cord, which carries deoxygenated blood and wastes from the fetus through two umbilical arteries; nutrients and oxygen are carried from the mother to the fetus through the single umbilical vein.
These form the chorionic membrane, which envelops the entire conceptus as the chorion.
The chorionic membrane forms finger-like structures called chorionic villi that burrow into the endometrium like tree roots, making up the fetal portion of the placenta.
The placenta develops throughout the embryonic period and during the first several weeks of the fetal period; placentation is complete by weeks 14–16.
Organogenesis
Following gastrulation, rudiments of the central nervous system develop from the ectoderm in the process of neurulation.
Specialized neuroectodermal tissues along the length of the embryo thicken into the neural plate.
During the fourth week, tissues on either side of the plate fold upward into a neural fold.
The two folds converge to form the neural tube.
The tube lies atop a rod-shaped, mesoderm-derived notochord, which eventually becomes the nucleus pulposus of intervertebral discs.
Block-like structures called somites form on either side of the tube, eventually differentiating into the axial skeleton, skeletal muscle, and dermis.
The embryo, which begins as a flat sheet of cells, begins to acquire a cylindrical shape through the process of embryonic folding.
Within the first 8 weeks of gestation, a developing embryo establishes the rudimentary structures of all of its organs and tissues from the ectoderm, mesoderm, and endoderm. This process is called organogenesis.
Fetal Development
A shunt is an anatomical (or sometimes surgical) diversion that allows blood flow to bypass immature organs such as the lungs and liver until childbirth.
From the umbilical vein, the oxygenated blood flows toward the inferior vena cava, all but bypassing the immature liver, via the ductus venosus shunt.
The fetal circulation therefore bypasses the lungs by shifting some of the blood through the foramen ovale, a shunt that directly connects the right and left atria and avoids the pulmonary trunk altogether.
A shunt within the pulmonary artery, the ductus arteriosus, diverts a portion of this blood into the aorta.
The excretory system is also developing: the kidneys are well-formed, and meconium, or fetal feces, begins to accumulate in the intestines.
Sebaceous glands coat the skin with a waxy, protective substance called vernix caseosa that protects and moisturizes the skin and may provide lubrication during childbirth.
A silky hair called lanugo also covers the skin during weeks 17–20, but it is shed as the fetus continues to grow.
Maternal Changes During Pregnancy, Labor, and Birth: The 40 weeks of an average pregnancy are usually discussed in terms of three trimesters, each approximately 13 weeks.
Effects of Hormones
Weight Gain
The second and third trimesters of pregnancy are associated with dramatic changes in maternal anatomy and physiology.
The most obvious anatomical sign of pregnancy is the dramatic enlargement of the abdominal region, coupled with maternal weight gain.
Circulatory System Changes: The greater blood volume helps to manage the demands of fetal nourishment and fetal waste removal.
Respiratory System Changes: During the last several weeks of pregnancy, the pelvis becomes more elastic, and the fetus descends lower in a process called lightening.
Integumentary System Changes
The dermis stretches extensively to accommodate the growing uterus, breast tissue, and fat deposits on the thighs and hips.
Torn connective tissue beneath the dermis can cause striae (stretch marks) on the abdomen, which appear as red or purple marks during pregnancy that fade to a silvery white color in the months after childbirth.
Physiology of Labor
Childbirth, or parturition, typically occurs within a week of a woman’s due date, unless the woman is pregnant with more than one fetus, which usually causes her to go into labor early.
Some women may feel the result of the decreasing levels of progesterone in late pregnancy as weak and irregular peristaltic Braxton Hicks contractions, also called false labor.
Stages of Childbirth
Cervical Dilation
For vaginal birth to occur, the cervix must dilate fully to 10 cm in diameter wide enough to deliver the newborn’s head.
The dilation stage is the longest stage of labor and typically takes 6–12 hours.
Expulsion Stage
The expulsion stage begins when the fetal head enters the birth canal and ends with birth of the newborn.
It typically takes up to 2 hours, but it can last longer or be completed in minutes, depending in part on the orientation of the fetus.
Until recent decades, it was routine procedure for an obstetrician to numb the perineum and perform an episiotomy, an incision in the posterior vaginal wall and perineum.
Afterbirth
The delivery of the placenta and associated membranes, commonly referred to as the afterbirth, marks the final stage of childbirth.
Uterine contractions continue for several hours after birth to return the uterus to its pre-pregnancy size in a process called involution, which also allows the mother’s abdominal organs to return to their pre-pregnancy locations.
Although postpartum uterine contractions limit blood loss from the detachment of the placenta, the mother does experience a postpartum vaginal discharge called lochia.
Adjustments of the Infant at Birth and Postnatal Stages
Respiratory Adjustments: Although the fetus “practices” breathing by inhaling amniotic fluid in utero, there is no air in the uterus and thus no true opportunity to breathe. (There is also no need to breathe because the placenta supplies the fetus with all the oxygenated blood it needs.)
Circulatory Adjustments: The process of clamping and cutting the umbilical cord collapses the umbilical blood vessels.
In the absence of medical assistance, this occlusion would occur naturally within 20 minutes of birth because the Wharton’s jelly within the umbilical cord would swell in response to the lower temperature outside of the mother’s body, and the blood vessels would constrict.
Thermoregulatory Adjustments
The fetus floats in warm amniotic fluid that is maintained at a temperature of approximately 98.6°F with very little fluctuation.
Birth exposes newborns to a cooler environment in which they have to regulate their own body temperature.
Newborns have a higher ratio of surface area to volume than adults.
Gastrointestinal and Urinary Adjustments
In adults, the gastrointestinal tract harbors bacterial flora—trillions of bacteria that aid in digestion, produce vitamins, and protect from the invasion or replication of pathogens.
In stark contrast, the fetal intestine is sterile.
The first consumption of breast milk or formula floods the neonatal gastrointestinal tract with beneficial bacteria that begin to establish the bacterial flora.
Lactation
Lactation is the process by which milk is synthesized and secreted from the mammary glands of the postpartum female breast in response to an infant sucking at the nipple.
The pituitary hormone prolactin is instrumental in the establishment and maintenance of breast milk supply.
In the final weeks of pregnancy, the alveoli swell with colostrum, a thick, yellowish substance that is high in protein but contains less fat and glucose than mature breast milk
The early milk, called foremilk, is watery, translucent, and rich in lactose and protein. Its purpose is to quench the infant’s thirst.
Hindmilk is delivered toward the end of a feeding. It is opaque, creamy, and rich in fat, and serves to satisfy the infant’s appetite.
Patterns of Inheritance
 Each human body cell has a full complement of DNA stored in 23 pairs of chromosomes. The pairs in a systematic arrangement called a karyotype.
Each human body cell has a full complement of DNA stored in 23 pairs of chromosomes. The pairs in a systematic arrangement called a karyotype.
Among these is one pair of chromosomes, called the sex chromosomes, that determines the sex of the individual (XX in females, XY in males).
The remaining 22 chromosome pairs are called autosomal chromosomes.
An individual’s complete genetic makeup is referred to as his or her genotype.
The characteristics that the genes express, whether they are physical, behavioral, or biochemical, are a person’s phenotype.
Because one copy of a gene, an allele, is inherited from each parent, the alleles in these complementary pairs may vary.
Although a person can have two identical alleles for a single gene (a homozygous state), it is also possible for a person to have two different alleles (a heterozygous state).
Mendel’s Theory of Inheritance
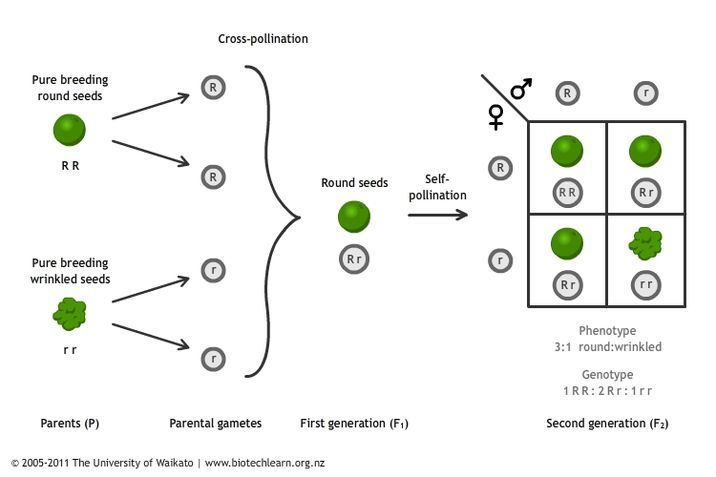
Mendel called tallness dominant because it was expressed in offspring when it was present in a purebred parent.
He called dwarfism recessive because it was masked in the offspring if one of the purebred parents possessed the dominant characteristic.
Autosomal Dominant Inheritance: When the dominant allele is located on one of the 22 pairs of autosomes (non-sex chromosomes), we refer to its inheritance pattern as autosomal dominant.
Autosomal Recessive Inheritance
When a genetic disorder is inherited in an autosomal recessive pattern, the disorder corresponds to the recessive phenotype.
Carriers for an autosomal recessive disorder may never know their genotype unless they have a child with the disorder.
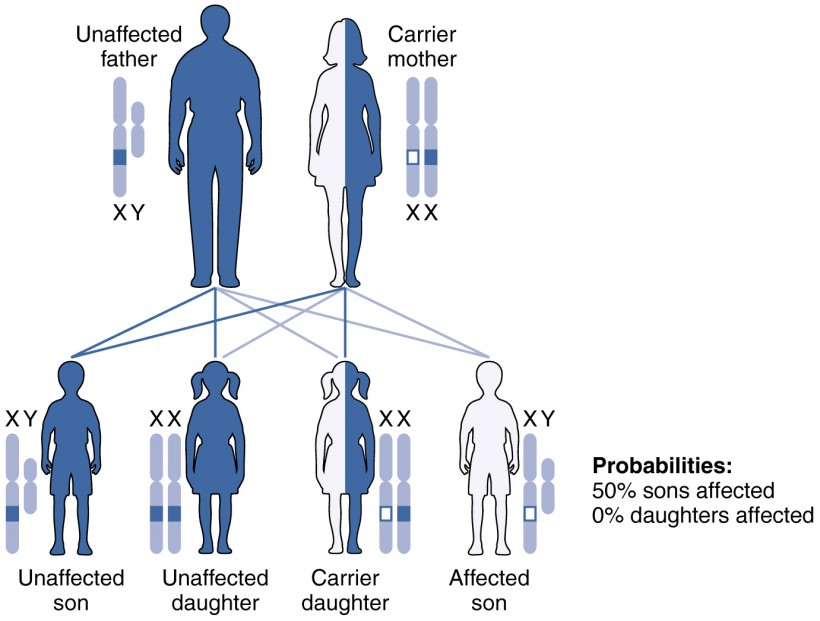
X-linked Dominant or Recessive Inheritance
An X-linked transmission pattern involves genes located on the X chromosome of the 23rd pair.
When an abnormal allele for a gene that occurs on the X chromosome is dominant over the normal allele, the pattern is described as X-linked dominant.
X-linked recessive inheritance is much more common because females can be carriers of the disease yet still have a normal phenotype.
Other Inheritance Patterns: Incomplete Dominance, Codominance, and Lethal Alleles
In incomplete dominance, the offspring express a heterozygous phenotype that is intermediate between one parent’s homozygous dominant trait and the other parent’s homozygous recessive trait.
Codominance is characterized by the equal, distinct, and simultaneous expression of both parents’ different alleles.
In recessive lethal inheritance patterns, a child who is born to two heterozygous (carrier) parents and who inherited the faulty allele from both would not survive.
Dominant lethal inheritance patterns are much more rare because neither heterozygotes nor homozygotes survive.
Mutations: A mutation is a change in the sequence of DNA nucleotides that may or may not affect a person’s phenotype.
 Knowt
Knowt
