Respiratory System pt2
Respiration
pulmonary respiration - ventilation (breathing) and exchange of gases in the lungs
Celluloar respiration - relates to O2 utilization and CO2 production by the tissues
Function of the respiratory system
The primary function of the respiratory system is to facilitate gas exchange between the atmosphere and the body’s cells
allows for the intake of oxygen (O2) and the removal of carbon dioxide (CO2) from the bloodstream
This gas exchange occurs through two main processes:
ventilation
diffusion
Ventilation refers to the mechanical process of moving air in and out of the lungs, commonly known as breathing
Diffusion involves the random movement of molecules from an area of high concentration to an area of low concentration
Ventilation -This is the movement of respiratory gases between the atmosphere and the alveolar region of the lungs, where gas exchange occurs.
Alveolar Gas Exchange - This process involves the diffusion of respiratory gases between the alveolar region of the lungs and the blood. O2 moves from the lungs, where its pressure is higher, into the blood. Conversely, CO2 moves from the blood, where its pressure is higher, to the lungs, where it is then expelled.
Circulatory Transport - This refers to the transportation of respiratory gases in the blood from the lungs to the body’s cells.
Systemic Gas Exchange - This final step involves the diffusion of respiratory gases between the blood and the body’s cells. Here, O2 diffuses from the blood into the cells due to pressure differences, while CO2 diffuses from the cells into the venous blood.
Functions of Respiratory System:
Removes Waste Products
Acid Base Balancing
Communication
Filters Incoming Air
Warms Incoming Air
Structure of the Respiratory System
The human respiratory system consists of a series of passages that filter air and transport it into the lungs, where gas exchange takes place in tiny air sacs called alveoli
Key organs include the nose, nasal cavity, pharynx, larynx, trachea, bronchial tree, and the lungs themselves.
The upper portion of the respiratory tract comprises the nose, nasal cavity, and pharynx, while the lower respiratory zone includes the trachea, bronchi, and bronchioles
The respiratory bronchioles connect to the alveoli, where gas exchange occurs
The anatomical position of the lungs in relation to the diaphragm, the major muscle of inspiration
Both the right and left lungs are enclosed by membranes known as pleura. The visceral pleura adheres to the outer surface of the lungs, while the parietal pleura lines the thoracic walls
These two layers of pleura are separated by a thin layer of fluid that acts as a lubricant, allowing them to glide smoothly over one another
The pressure in the pleural cavity (known as intrapleural pressure) is lower than atmospheric pressure, and it decreases even further during inspiration
This pressure difference causes air to flow from the environment into the lungs
This lower intrapleural pressure is crucial because it prevents the collapse of the delicate air sacs (alveoli) within the lungs
The airways that connect to and from the lungs are categorized into two functional zones
The conducting zone - comprises all the anatomical structures—such as the trachea, bronchial tree, and bronchioles—that air travels through before reaching the respiratory zone
The respiratory zone - where gas exchange takes place, and it includes the respiratory bronchioles, alveolar ducts, and alveolar sacs
Respiratory bronchioles are part of this zone because they contain small clusters of alveoli
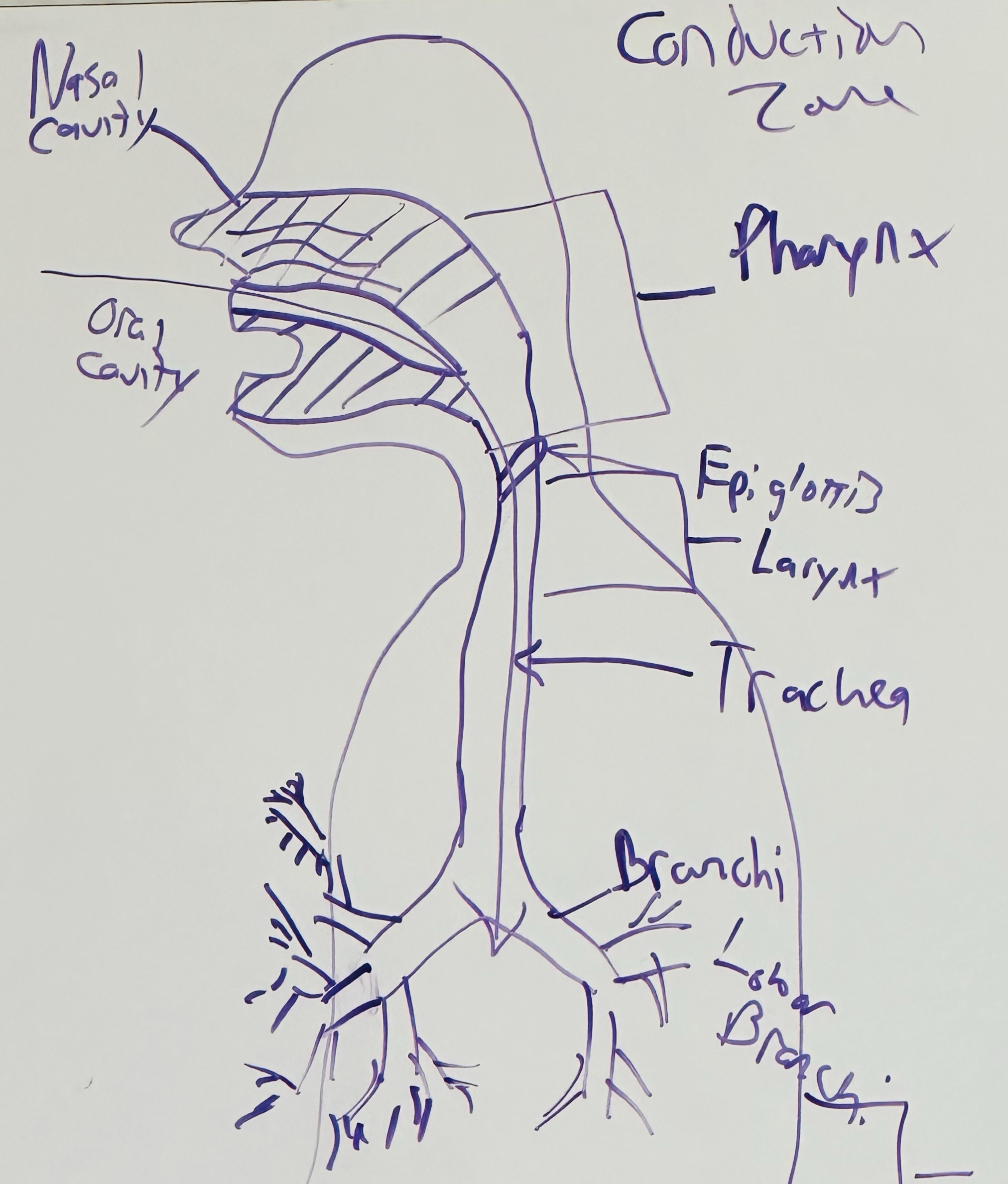
Conducting Zone
Air enters the trachea from the pharynx (throat) and receives input from both the nasal and oral cavities
At rest, breathe through the noses
During moderate to heavy exercise, the mouth becomes the primary passageway for air
For air to enter or exit the trachea, it must pass through a valve-like structure called the epiglottis, which is located between the vocal cords
The trachea then branches into two primary bronchi (right and left) that lead into each lung
The bronchial tree further divides several more times, forming smaller branches known as bronchioles
Bronchioles continue to subdivide and eventually lead to the alveolar ducts, which connect to the alveolar sacs and the respiratory zone of the lung
The conducting zone of the respiratory system serves not only as a passageway for air but also functions to filter and humidify it as it moves toward the respiratory zone
Regardless of the temperature or humidity of the environment, the air that reaches the lungs is warmed and saturated with water vapor
This process of warming and humidifying the air protects the delicate lung tissue from drying out, especially during exercise when breathing rates increase
Respiratory Zone
Gas exchange in the lungs takes place across approximately 300 million tiny alveoli
This vast number of structures provides the lungs with a large surface area for diffusion
The rate of gas diffusion is further enhanced by the fact that each alveolus is only one cell layer thick, resulting in a total blood-gas barrier that is just two cell layers thick (one from the alveolar cell and one from the capillary cell)
Avelio can cause problems like:
the surface tension from the liquid lining the alveoli creates relatively strongforces that can cause them to collapse
To fix this:
some of the alveolar cells produce and release a substance called surfactant, which reduces the surface tension in the alveoli and helps prevent their collapse
Mechanics of Breathing
Pulmonary ventilation, the movement of air from the environment into the lungs, occurs through a mechanism called bulk flow
Process involves the movement of air molecules along a passageway driven by pressure differences
During inspiration, the pressure within the lungs falls below atmospheric pressure, allowing air to flow in
Expiration takes place when the pressure inside the lungs surpasses atmospheric pressure, pushing air out
Inspiration
Inspiratory muscles are those that increase the volume of the chest, with the diaphragm being the most crucial for normal breathing
Dome-shaped muscle connects to the lower ribs and is controlled by the phrenic nerves
As the diaphragm contracts, it pushes the abdominal contents downward and lifts the ribs outward, leading to an increase in both the vertical and lateral dimensions of the thoracic cavity and the expansion of the lungs
This lung expansion lowers intrapulmonary pressure below atmospheric pressure, facilitating airflow into the lungs
While the diaphragm does most of the work for inspiration during rest, accessory muscles become engaged during exercise to support breathing
Accessory muscles include:
the external intercostals
pectoralis minor, scalene muscles
sternocleidomastoids
Expiration
During normal, quiet breathing, expiration is a passive process; no muscular effort is required for expiration to occur at rest
Because both the lungs and the chest wall are elastic, allowing them to return to their equilibrium position after expanding during inhalation
During exercise, expiration becomes an active process
The primary muscles involved in this active expiration are located in:
the abdominal wall
the rectus abdominis and the external oblique muscles
the internal intercostal muscles assist by pulling down on the ribs
Decreasing the size of the thoracic cavity
When muscles contract, they push the diaphragm upward and pull the ribs downward and inward, resulting in a decrease in the volume of the chest cavity and facilitating expiration
Airway resistance
The pressure difference required for airflow into the lungs depends on the resistance of the airways
The relationship governing airflow through the respiratory system can be expressed by:
Airflow = (P1 - P2) / Resistance
P1 - P2 represents the pressure difference at the two ends of the airway, while resistance is the opposition to airflow posed by the airway itself
Airflow increases anytime there is a greater pressure gradient across the pulmonary system or a decrease in airway resistance
The most significant factor contributing to airway resistance is the diameter of the airway
When airways become narrowed due to conditions such as chronic obstructive pulmonary disease (COPD) or asthma, they present greater resistance to airflow compared to healthy, open airways
reduction in the radius of an airway notably increases resistance to flow
Pulmonary Ventilation
V is used to denote a volume of gas - means volume per unit of time (generally one minute).
Subscripts T, D, A, I, E are used to denote tidal (T), dead space (D), alveolar (A), inspired (I), and expired (E), respectively
Pulmonary ventilation - the movement of gas into and out of the lungs
The amount of gas ventilated per minute is the product of the frequency of breathing (f) and the amount of gas moved per breath (tidal volume, abbreviated as VT):
V = Vt x f
In a 70-kg man, the at rest is generally around 7.5 L/min, with a tidal volume of 0.5 L and a frequency of 15 breaths per minute. During very heavy to severe exercise, ventilation may reach 120 to 175 L/min, with a frequency of 40 to 50 breaths per minute and a tidal volume of approximately 3 to 3.5 L.
Note that not all of the air that passes the lips reaches the alveolar gas compartment where gas exchange occurs
Part of each breath remains in conducting airways (trachea, bronchi, etc.) and thus does not participate in gas exchange
This “unused” ventilation is called dead space ventilation (VD), and the space it occupies is known as anatomical dead space
The volume of inspired gas that reaches the respiratory zone is referred to as alveolar ventilation (V̇A)
Total minute ventilation can be subdivided into dead space ventilation and alveolar ventilation:
V = Va + Vd
It follows that alveolar ventilation (VA) can be computed as:
Va = (Vt - Vd)
Since the anatomical dead space in the lungs does not increase during exercise, any increase in VT results in an increase in VA
Therefor by increasing VT rather than increasing the frequency of breathing (fR) ensures that VD does not increase and that VA rises
Note that pulmonary ventilation is not equally distributed throughout the lung
The base (bottom) of the lung receives more ventilation than the apex (top region), particularly during quiet breathing
This changes during exercise, with the apical (top) regions of the lung receiving an increased percentage of the total ventilation
Pulmonary Volumes and Capacities
Pulmonary volumes are measured using spirometry, a technique where a subject breathes into a device that records inspired and expired gas volumes. Key terms include:
Vital Capacity (VC) - Maximum gas expired after maximum inspiration.
Residual Volume (RV) - Gas remaining in the lungs after maximum expiration.
Total Lung Capacity (TLC) - Total volume in the lungs after maximum inspiration.
Inspiratory Capacity - The volume of air that can be inhaled afternormal inspiration.
Expiratory Reserve Capacity - ERV The maximum volume of air that can be voluntarily exhaled
Functional Residual Capacity - Volume left in the lungs at the end of a normal breath which is notnormally part of the subdivisions
Tidal Volume - The normal to-and-fro respiratory exchange of 500 cc; vital capacity is the maximumamount of exhalable air; after a full inspiration, which added to the residual volume, is the total lung capacity
Spirometry is crucial for diagnosing lung diseases like chronic obstructive pulmonary disease (COPD)
Decreases vital capacity and airflow rates due to increased airway resistance
Forced expiratory volume (FEV1) is measured during a maximal expiration, with normal individuals showing an FEV1 to VC ratio of 80% or higher
COPD patient may have an FEV1 of only 1.0 L and a VC of 3.0 L, resulting in a much lower ratio of 33%, indicative of severe airway obstruction
Diffusion of gases
According to Dalton’s law, the total pressure of a gas mixture is equal to the sum of the pressures that each gas would exert independently
The pressure that each gas exerts independently can be calculated by multiplying the fractional composition of the gas by the absolute pressure (barometric pressure)
An example calculating the partial pressure of oxygen in air at sea level:
The barometric pressure at sea level is 760 mm Hg (recall that barometric pressure is the force exerted by the weight of the gas contained within the atmosphere)
The composition of air is generally considered to be as follows:
Oxygen - 20.93 (percentage) - 0.2093 (fraction)
Nitrogen - 79.04 (percentage) - 0.7904 (fraction)
CO2 - 0.03 (percentage) - 0.0003 (fraction)
Total = 100.00 %
Partial Pressure of O2 - PO2 = 760 × 0.2093 : PO2 = 159 mm Hg
Partial Pressure of Nitrogen - PN2 = 760 × 0.7904 : PN2 = 600 mm Hg
Since O2, CO2, and N2 make up 100% of the atmosphere
Total Barometric Pressure - P (dry atmosphere) = PO2 + PN2 + PCO2
Diffusion of gas across tissues is described by Ficks Law
Stating the rate of gas trasnfer is porportional to the tissue area, the diffusion coefficient of the gas and the difference in the partial pressure of the gas on the two sides of the tissue & is inversley proportional to the thickness
V gas = (A/T) x D x (P1 - P2)
A = Area
T = thickenss of tissue
D = Diffusion
P1 & P2 = difference in partila pressure
The rate of diffusion for gases increases with larger surface areas and higher driving pressures, while tissue thickness hinders diffusion
The lungs are particularly well-designed for gas exchange due to their large surface area and extremely thin alveolar membrane
This efficient design is crucial, especially during intense exercise when oxygen uptake and carbon dioxide output can rise 20 to 30 times compared to rest
Blood flow through the lung
The pulmonary circulation starts with the pulmonary artery, which carries mixed venous blood from the right ventricle
This blood travels through the pulmonary capillaries for gas exchange, after which the oxygenated blood is returned to the left atrium via the pulmonary vein to be distributed throughout the body
Blood flow rates in the pulmonary and systemic circulation are equal, with both ventricles delivering approximately 5 L/min in healthy adults
Pulmonary circulation operates under lower pressures compared to systemic circulation due to lower vascular resistance
During exercise, pulmonary vascular resistance decreases, leading to increased blood flow in the lungs with only slight increases in pulmonary arterial pressure
Blood flow distribution within the lungs is affected by gravity; in an upright position, flow decreases from the bottom to the top
During low-intensity exercise, blood flow to the top of the lung increases, enhancing gas exchange
Lying supine results in more uniform blood flow in the lungs, while being upside down causes increased flow to the lung apex compared to the base
Ventilation-Perfusion Relationships
normal gas exchange requires a matching of ventilation to blood flow (perfusion, Q)
In other words, an alveolus can be well ventilated, but if blood flow to the alveolus does not adequately match ventilation, gas exchange does not occur
Mismatching of ventilation and perfusion is responsible for most of the problems of gas exchange that occur due to lung diseases
The ideal ventilation-to-perfusion ratio (V/Q) is 1.0 or slightly greater
There is a one-to-one matching of ventilation to blood flow, which results in optimum gas exchange. However, the V/Q ratio is generally not equal to 1.0 throughout the lung, but varies depending on the section of the lung being considered
The V/Q ratio at the top and the base of the lung is calculated for resting conditions
The ventilation (at rest) in the upper region of the lung is estimated to be 0.24 L/min, whereas the blood flow is predicted to be 0.07 L/min
The V/Q ratio is 3.4 (i.e., 0.24/0.07 = 3.4)
A large V/Q ratio represents a disproportionately high ventilation relative to blood flow, which results in poor gas exchange. In contrast, the ventilation at the base of the lung is 0.82 L/min, with a blood flow of 1.29 L/min (V/Q ratio = 0.82/1.29 = 0.64)
V/Q ratio less than 1.0 means that blood flow is higher than ventilation to the region in question
Although V/Q ratios less than 1.0 are not indicative of ideal conditions for gas exchange, in most cases, V/Q ratios greater than 0.50 are adequate to meet the gas exchange demands at rest
What effect does exercise have on the V/Q ratio?
Moderate exercise improves the V/Q relationship
Heavy exercise may result in a small V/Q inequality and thus a minor impairment in gas exchange
Whether the increase in V/Q inequality is due to low ventilation or low perfusion is not clear
O2 and CO2 Transport in Blood
Oxygen (O2) and carbon dioxide (CO2) are transported in the blood primarily through two methods:
O2 binds with hemoglobin
CO2 is converted into bicarbonate (HCO3).
Hemoglobin and O2 Transport
Approximately 99% of oxygen (O2) in the blood is bound to hemoglobin
Hemoglobin - protein in red blood cells
Each hemoglobin molecule can carry four O2 molecules, forming oxyhemoglobin
The capacity to transport O2 depends on hemoglobin concentration, which is about 150 g/L for healthy males and 130 g/L for females
When fully saturated with O2, each gram of hemoglobin transports 1.34 ml of O2, allowing a healthy male to transport around 200 ml and a healthy female about 174 ml of O2 per liter of blood at sea level
Oxyhemoglobin - Heoglobin combined with O2; 1.34 ml of oxygen can combine with 1 g Hb
Deoxyhemoglobin - hemoglobin no in combination with O2
Oxygen-hemoglobin Dissociation Curve
The oxygen–hemoglobin dissociation curve illustrates the relationship between the partial pressure of O2 (PO2) and its binding to hemoglobin in blood
"Dissociate" - separation of O2 from hemoglobin, while the process of O2 binding in the lungs is termed loading, and its release at tissues is called unloading
Both loading and unloading are reversible reactions
Deoxyhemoglobin + O2 = Oxyhemoglobin
factors that determine the direction of this reaction are:
the PO2 of the blood
the affinity or bond strength between hemoglobin and O2.
A high PO2 drives the reaction to the right (i.e., loading), whereas low PO2 and a reduced affinity of hemoglobin for O2 moves the reaction to the left (i.e., unloading)
Effect of pH on O2-Hb dissociation Curve
The effect of changing blood pH on the shape of the oxygen–hemoglobin dissociation curve
A decrease in pH (increased acidity) results in a rightward shift of the curve (Bohr effect)
while an increase in pH (decreased acidity) results in a leftward shift of the curve
A decrease in blood pH (increased acidity) weakens the bond between O2 and hemoglobin, leading to a right shift in the oxyhemoglobin dissociation curve
known as the Bohr effect
This occurs during heavy exercise due to elevated hydrogen ion levels, which result in reduced hemoglobin's O2 transport capacity
Consequently, higher acidity in muscles during exercise facilitates the unloading of O2 to the tissues
Temperature effect on O2-Hb Dissociation Curve
The effect of changing blood temperature on the shape of the oxygen–hemoglobin dissociation curve
An increase in temperature results in a rightward shift in the curve
a decrease in blood temperature results in a leftward shift in the curve
Hemoglobin's affinity for O2 is inversely related to blood temperature
An increase in temperature results in a right shift of the oxyhemoglobin dissociation curve
weakening the bond between O2 and hemoglobin
which aids in O2 unloading to working muscles.
Decrease in temperature leads to a left shift
strengthening the bond
hindering O2 release
During exercise, the heat produced by contracting muscles promotes this right shift, facilitating O2 delivery to tissues
2-3 DPG and the O2-Hb Dissociation Curve
The concentration of 2,3 diphosphoglycerate (2-3 DPG) in red blood cells affects the oxyhemoglobin dissociation curve by reducing hemoglobin’s affinity for O2
causing a right shift
2-3 DPG levels increase during exposure to high altitude and anemia, but not significantly during exercise at sea level
The right shift during heavy exercise is attributed to acidosis and elevated blood temperature rather than changes in 2-3 DPG
O2 Transport in Muscle
Myoglobin - oxygen-binding protein primarily found in skeletal and cardiac muscle fibers, where it plays a crucial role in transporting oxygen from the muscle cell membrane to the mitochondria
Its presence is most notable in slow-twitch fibers, which have high aerobic capacity, while it is found in smaller quantities in intermediate fibers and limited amounts in fast-twitch fibers
Structurally - myoglobin resembles hemoglobin but is significantly lighter, weighing about a quarter as much
This structural difference leads to a higher affinity for oxygen in myoglobin compared to hemoglobin
As a result, myoglobin has a steeper oxygen dissociation curve at lower partial pressures of oxygen (PO2)
disengaging its oxygen even at very low PO2 levels—down to 1 or 2 mm Hg—making it particularly effective in the oxygen-poor environment of active skeletal muscle
Myoglobin O2 stores act as an "O2 reserve" during the transition from rest to exercise
Initially, there is a delay in O2 delivery to muscles when exercise begins
Myoglobin provides O2 to meet muscle demands until the cardiopulmonary system can catch up
After exercise, myoglobin O2 stores need to be replenished, contributing to the O2 debt
CO2 Transport in Blood
Carbon dioxide is transported in the blood in three forms:
Dissolved CO2 (about 10% of blood CO2 is transported this way)
CO2 bound to hemoglobin (called carbaminohemoglobin; about 20% of blood CO2 is transported via this form)
Bicarbonate (70% of CO2 found in blood is transported as bicarbonate: HCO–3)
More than 99% of oxygen (O2) in the blood is chemically bonded to hemoglobin, and its interaction is illustrated by the S-shaped O2–hemoglobin dissociation curve, which reflects how the partial pressure of O2 influences this bonding
When body temperature increases and blood pH decreases, the curve shifts to the right, indicating that hemoglobin’s affinity for oxygen is reduced
Carbon dioxide (CO2) is transported in the blood through three primary mechanisms
about 10% is dissolved directly in the plasma, approximately
20% is bound to hemoglobin as carbaminohemoglobin
majority—around 70%—is carried as bicarbonate.
In addition to hemoglobin, myoglobin is an important oxygen-binding protein found in muscle tissues
It functions as a shuttle
facilitating the movement of oxygen from the muscle cell membrane to the mitochondria, where it is utilized for respiration
Ventilation and Acid-Base Balance
Pulmonary ventilation plays a crucial role in regulating the levels of hydrogen ions (H+) in the blood through the bicarbonate (HCO3) reaction
When carbon dioxide (CO2) levels rise in the blood or body fluids, it leads to an increase in hydrogen ion concentration, resulting in a lower pH
When CO2 is removed from the system, hydrogen ion concentration decreases, causing pH levels to rise
Lung ← CO2 + H2O = H2CO3 = H+ +HCO3 → Muscle
The CO2-carbonic anhydrase reaction can be summarized as follows:
CO2 and water (H2O) combine to form carbonic acid (H2CO3), which dissociates into hydrogen ions (H+) and bicarbonate
An increase in pulmonary ventilation facilitates the exhalation of excess CO2, leading to a reduction in blood CO2 pressure (PCO2) and a subsequent increase in blood pH
On the other hand, decreased pulmonary ventilation causes CO2 to accumulate, raising hydrogen ion concentration and lowering pH
Ventilatory And Blood-Gas Responses to Exercise
Rest to Work Transitions
The transition from rest to moderate-intensity exercise, specifically below the lactate threshold, results in noticeable changes in pulmonary ventilation
Initially, there is a sharp increase in expired ventilation at the start of exercise
followed by a gradual rise until a steady state is reached
During this transition, while ventilation and the partial pressures of oxygen (O2) and carbon dioxide (CO2) fluctuate, it is important to note that arterial oxygen (PO2) levels tend to decrease and arterial carbon dioxide (PCO2) levels may slightly increase
This pattern suggests that the rise in alveolar ventilation at the onset of exercise does not keep pace with the metabolic demands, highlighting a lag in the body's respiratory response relative to increased metabolic activity
Prolonged Exercise in a Hot Environment
During constant-load submaximal exercise, ventilation initially increases rapidly before gradually stabilizing at a steady-state level
with arterial PO2 and PCO2 remaining relatively constant throughout
However, in prolonged exercise under hot and humid conditions, ventilation tends to drift upward due to the rising body temperature influencing the respiratory control center
In the context of incremental exercise, ventilation (VE) exhibits a linear increase up to approximately 50% to 70% of an athlete's maximum oxygen consumption (O2 max)
Beyond these levels, ventilation escalates exponentially, a phenomenon referred to as the ventilatory threshold
It is noteworthy that exercise-induced hypoxemia affects 40% to 50% of elite endurance athletes, regardless of gender
Recent findings also highlight a physiological difference, as women possess smaller airways compared to men when lung size is accounted for, leading to an increased work of breathing during exercise
Control of Ventilation
The regulation of pulmonary ventilation is an efficient control system that maintains blood-gas and acid-base homeostasis
During exercise, pulmonary ventilation increases in proportion to exercise intensity and the need for oxygen, ensuring proper control of arterial oxygen content, carbon dioxide levels, and acid-base balance
Ventilatory Regulation at Rest
Inspiration and expiration occur through the diaphragm's contraction and relaxation during quiet breathing, with accessory muscles involved during exercise
Respiratory muscles are controlled by somatic motor neurons in the spinal cord, which are regulated by the respiratory control center in the medulla oblongata
Respiratory Control Center
The respiratory system, like the cardiovascular system, has a control mechanism to regulate breathing in accordance with the body's metabolic rate
Key components include :
the preBotzinger complex (preBotC), which acts as the primary pacemaker for inspiration,
the retrotrapezoid nucleus/parafacial respiratory group (RTN/pFRG), which controls active expiration
The Pontine respiratory center, located in the Pons, fine-tunes the rate and pattern of breathing by interacting with both the preBotC and the RTN/pFRG
Under normal conditions, breathing is primarily influenced by the preBotC, with expiration being mostly passive
During exercise, these centers work together to adjust breathing to meet increased metabolic demands, utilizing feedback from various chemoreceptors for precise regulation
Input to the Respiratory Control Center
The respiratory control center depends on input from both higher brain centers and afferent neural signals originating from various areas outside of the central nervous system
This input can be categorized into two main types:
neural
humoral
Neural input consists of signals from higher brain regions and afferent neurons that respond to stimuli other than those found in the blood
Humoral input is influenced by blood-borne substances detected by specialized chemoreceptors, which measure the strength of these stimuli and relay the necessary information to the medulla
Humoral Chemorecptor
Chemoreceptors are specialized neurons that respond to changes in the internal environment, classified into central and peripheral types
Central chemoreceptors, located in the medulla, respond to PCO2 and H+ changes in cerebrospinal fluid, increasing ventilation when these levels rise
Peripheral chemoreceptors, found in the aortic arch (aortic bodies) and carotid arteries (carotid bodies), respond to increases in arterial H+, PCO2, potassium levels, norepinephrine, decreased arterial PO2, and increased body temperature
Chemoreceptors in our body respond to changes in chemicals that affect breathing.
When levels of carbon dioxide (PCO2) in the blood increase, minute ventilation also goes up
This increase happens because both the carotid bodies (located in the neck) and central chemoreceptors (in the brain) react to higher PCO2 levels
In healthy people breathing at sea level, changes in oxygen levels (PO2) have little effect on breathing control
When someone is at a high altitude where the air pressure is much lower, the PO2 decreases
This drop stimulates the carotid bodies, which tell the brain to increase breathing
The point where breathing starts to increase rapidly due to lower PO2 is called the hypoxic threshold, which usually occurs around 60 to 75 mm Hg of arterial PO2
The carotid bodies are mainly responsible for this response, as other chemoreceptors do not react to changes in PO2
Additionally, higher blood levels of potassium can also stimulate the carotid bodies, increasing ventilation
During exercise, potassium levels rise in the blood due to muscle activity, which may help regulate breathing during this time
Neural Input to the Respiratory Control Center
Neural input to the respiratory control center is influenced by higher brain centers and afferent pathways
The motor cortex activates skeletal muscles, increasing ventilation during exercise
Stretch receptors in the lungs contribute to the Hering-Breuer reflex, which limits lung inflation by inhibiting the inspiratory center
This reflex is more significant in infants but also plays a role in adults during high-intensity exercise
Afferent input during exercise comes from peripheral mechanoreceptors, such as muscle spindles and Golgi tendon organs, which help regulate breathing
Chemoreceptors in muscles respond to changes in potassium and H+ levels, and mechanoreceptors in the right ventricle may provide feedback to the respiratory control center regarding cardiac output during exercise
Ventilatory Control During Meoderate-Intensity Exercise
The regulation of breathing during exercise involves several key factors:
Initial Drive: The primary stimulus to increase ventilation during exercise comes from neural input (central command) from higher brain centers.
PCO2 Regulation: Arterial PCO2 is closely regulated during moderate-intensity exercise, indicating that humoral chemoreceptors and afferent neural feedback from muscles help fine-tune breathing to match metabolic demands.
Neural Contribution: During moderate-intensity exercise, 40% to 50% of the drive to breathe originates from signals sent from working muscles to the brain.
Additional Influences: In prolonged moderate-intensity exercise in hot environments, ventilation can also be influenced by rising blood temperature and increasing levels of catecholamines.
Redundant Mechanisms: The interplay between neural and chemoreceptor inputs creates redundancy in the respiratory control system, crucial for maintaining homeostasis during exercise.
Ventilatory Control During Heavy Exercise
Rise in ventilation, known as the ventilatory threshold, that occurs during incremental exercise above the lactate threshold, Key points include:
The rise in ventilation is linked to simultaneous decreases in pH and increases in blood hydrogen ion levels, which stimulate carotid bodies
Blood lactate levels are believed to be a primary stimulus for this ventilatory response
Researchers often estimate lactate threshold noninvasively through ventilatory threshold, but these do not always occur at the same work rate
Other factors influencing ventilation during high-intensity exercise include rising blood potassium levels, increasing body temperature, elevated blood catecholamines, and neural input to the respiratory control center
Motor unit recruitment during exercise intensity may also play a role in the ventilatory pattern
While blood hydrogen ions are a key mechanism for the ventilatory threshold, secondary factors also contribute to ventilation control during heavy exercise
Do lungs Adapt to Exercise Training?
The muscular-skeletal and cardiovascular systems adapt to regular endurance exercise, while the lungs do not show significant changes in structure or function in response to exercise training
This lack of adaptation is because the normal lung's capacity exceeds the oxygen and carbon dioxide transport demands during exercise in most young adults.
Highly trained elite endurance athletes may experience a failure of the pulmonary system to meet the increased oxygen transfer needs during maximal exercise, leading to hypoxemia, which can negatively impact their performance
Does the Pulmonary System Limit Maximal Exercise Performance
The pulmonary system is generally not a limiting factor for exercise performance in healthy young individuals engaging in prolonged moderate-intensity exercise, such as activities characterized by workloads at approximately 90% of their maximum capabilities
At these moderate levels, the respiratory system is typically efficient and sufficient to support physical activity
However, when the intensity of exercise surpasses 90% of maximum effort—often categorized as very heavy exercise—the dynamics shift
This fatigue can impede the efficiency of breathing, reducing the ability to take in sufficient oxygen and expel carbon dioxide, which can significantly affect overall exercise performance
Additionally, it is worth noting that some elite endurance athletes may experience incomplete pulmonary gas exchange, particularly at high exercise intensities
This phenomenon can restrict their performance by limiting the effective delivery of oxygen to the muscles and the removal of metabolic byproducts, ultimately hindering their ability to sustain peak performance levels during strenuous activities
In Class Activity
HR- 52
Total breaths - 16
Risen HR - 88