The Visual System
The Retina
Retina: Thin light-sensitive layer of tissue lining the back of the eye. It functions as the primary sensory organ of the visual system converting light into electrical signals that are transmitted to the brain for visual perception.
Photoreceptors
Rods: Photoreceptor cells in the retina specialised for low-light (scotopic) vision. They are highly sensitive to light but do not detect colour, making them crucial for night vision.
Function: Specialised for scotopic vision (low-light conditions).
Distribution: More numerous and located primarily in the peripheral retina.
Sensitivity: Highly sensitive to light but do not detect color.
Cones: Photoreceptor cells in the retina responsible for color vision and sharp visual acuity under bright light conditions (photopic vision). There are three types of cones, each sensitive to different wavelengths (red, green, and blue).
Function: Specialised for photopic vision (bright light) and colour vision.
Distribution: Concentrated in the fovea, providing sharp central vision.
Specialised Regions of the Retina
Macula: An oval-shaped, pigmented region near the centre of the retina that surrounds the fovea. It is responsible for central vision and fine-detail perception.
Fovea: A small depression in the center of the macula with the highest density of cones and no rods. It provides the sharpest visual acuity and the most detailed colour vision.
Peripheral Retina: The area of the retina outside the macula, rich in rods but fewer cones. It is specialised for detecting motion, low-light vision, and peripheral vision.
Optic Disc: The location in the retina where the optic nerve exits the eye. It contains no photoreceptors, resulting in a blind spot in the visual field.
Pathways of Visual Processing
Retino-Geniculo-Striate Pathway
Retino-Geniculo-Striate Pathway: Main neural route for processing conscious visual information responsible for visual discrimination and perception. Also known as the primary visual pathway. (Visual information processing → Can only see with this pathway)
Retina: Visual information begins in the retina, where photoreceptors (rods and cones) detect light and initiate phototransduction.
Optic Nerve: Axons of retinal ganglion cells converge at the optic disc to form the optic nerve (Cranial Nerve II). The optic nerve carries visual signals from the retina toward the brain.
Optic Chiasm: At the optic chiasm, fibers from the nasal retina cross to the opposite side, while fibers from the temporal retina remain ipsilateral. Crossing ensures that the left visual field of both eyes is processed in the right hemisphere and vice versa.
Optic Tract: Beyond the optic chiasm, the fibers are reorganized into the optic tract. Each optic tract contains nasal fibers from the contralateral eye and temporal fibers from the ipsilateral eye.
Lateral Geniculate Nucleus (LGN): Located in the thalamus, the LGN acts as a relay station for visual signals. The LGN organizes signals spatially (retinotopic map) and segregates input from each eye.
Magnocellular Layers: Motion detection (from rods).
Parvocellular Layers: Color and detail detection (from cones).
Optic Radiations: Axons from the LGN project to the primary visual cortex (V1) via two pathways:
Meyer’s Loop: Fibers pass through the temporal lobe and carry information from the upper visual field.
Baum’s Loop: Fibers pass through the parietal lobe and carry information from the lower visual field.
Striate Cortex (V1): Located in the occipital lobe, specifically in the calcarine sulcus. The striate cortex is responsible for the initial processing of visual input, organization of input into retinotopic maps and detection of edges, orientation, motion, and color. After analysis signals are sent to higher-order visual areas (e.g., V2, V3) for further processing.
Functions:
Visual Perception: Recognizing shapes, colors, and spatial relationships.
Detail and Color Detection: Through cone-mediated input processed in the parvocellular layers.
Motion and Broad Spatial Awareness: Through rod-mediated input processed in the magnocellular layers.
Retino-Tecto-Pulvinar-Extrastriate Pathway
Retino-Tecto-Pulvinar-Extrastriate Pathway: Secondary visual processing route that bypasses the primary visual cortex (V1), facilitating non-conscious visual functions such as reflexive eye movements and attention orientation. (Spatial information processing)
Retinal Input: Visual signals begin in the retina, where photoreceptor cells (rods and cones) detect light and initiate phototransduction. Retinal ganglion cells collect the processed signals and project directly to the superior colliculus in the midbrain.
Superior Colliculus: Primary hub for visual input that detects motion, spatial orientation, and abrupt changes in the visual field (e.g., detecting a moving object) and coordinates reflexive eye and head movements via connections with motor regions and cranial nerves controlling extraocular muscles.
Pulvinar: Acts as a relay and processing hub, receiving inputs from the superior colliculus. It filters and prioritises visual information based on saliency (importance), emphasising stimuli that demand attention or action.
Extrastriate Cortex: Includes visual areas beyond V1, such as V2, V3, and the middle temporal (MT) area, collectively engaged in advanced visual processing tasks:
V2 and V3: Early-stage processing for orientation, texture and depth.
MT: specialised for motion perception and spatial localisation.
Functions:
Visual Attention and Orientation: This pathway enables rapid, unconscious responses to visual stimuli, aiding in orienting movements and attention shifts.
Blindsight: In individuals with damage to V1, this pathway may support residual visual capabilities without conscious awareness, a phenomenon known as blindsight.
Retino-Hypothalamic Tract
Retino-Hypothalamic Tract: Specialized neural pathway that transmits light information from intrinsically photosensitive retinal ganglion cells (ipRGCs) in the retina to the suprachiasmatic nucleus (SCN) in the hypothalamus, synchronising the body’s circadian rhythms with the external light-dark cycle.
Retinal Ganglion Cells: Specialized intrinsically photosensitive retinal ganglion cells (ipRGCs) detect ambient light levels - specifically blue light.
Optic Nerve: Axons from ipRGCs travel through the optic nerve toward the brain.
Optic Chiasm: Some axons from the ipRGCs cross at the optic chiasm, ensuring that light information from both eyes reaches both sides of the SCN.
Retinohypothalamic tract: A distinct set of axons branching off from the optic nerve at the optic chiasm forms the RHT. These fibers directly project to the SCN in the anterior hypothalamus.
Superchiasmatic Nucleus: Acts as the body’s central circadian pacemaker using light information to synchronise the internal biological clock with the external light-dark cycle.
Functions:
Circadian Rhythm Regulation: The SCN coordinates daily cycles of behavior and physiology, such as sleep-wake cycles, hormone release (e.g., melatonin), and body temperature.
Light as a Zeitgeber: Light acts as a zeitgeber (time-giver), resetting the SCN and aligning the body’s internal clock with the external environment.
Melatonin Suppression: Light input via the RHT inhibits the release of melatonin from the pineal gland, promoting wakefulness. Darkness reduces input to the SCN, allowing melatonin secretion and facilitating sleep.
Dorsal and Ventral Stream
Dorsal Stream (Where Pathway): Visual processing pathway that extends from the secondary visual cortex (V1) to the posterior parietal cortex. It is responsible for processing motion, spatial relationships, and object location, enabling spatial awareness and visually guided actions.
Retino-Tecto-Pulvinar-Extrastriate Pathway: Provides significant input via the retino-tecto-pulvinar division, particularly for detecting motion and orienting to moving stimuli. (Mainly)
Retino-Geniculo-Striate Pathway: Provides motion and spatial input via the magnocellular layers of the LGN. (To lesser extend)
Ventral Stream (What Pathway): The ventral stream is a visual processing pathway that extends from the primary visual cortex (V1) to the inferotemporal cortex. It is responsible for processing object recognition, form, colour, and detail, allowing for identification of objects and faces.
Retino-Geniculo-Striate Pathway: Provides detailed form and colour input from the parvocellular layer of the LGN.
Ocular Muscles
Interocular Muscles
Radial Muscles: Smooth muscles in the iris responsible for dilating the pupil (mydriasis) to allow more light into the eye. Activated by the sympathetic nervous system.
Circular Muscles: Smooth muscles in the iris responsible for constricting the pupil (miosis) to reduce the amount of light entering the eye. Activated by the parasympathetic nervous system via the oculomotor nerve (CN III).
Ciliary Muscles: Smooth muscles located in the ciliary body, responsible for changing the shape of the lens during accommodation to focus on near or distant objects. Activated by the parasympathetic nervous system via the oculomotor nerve (CN III).
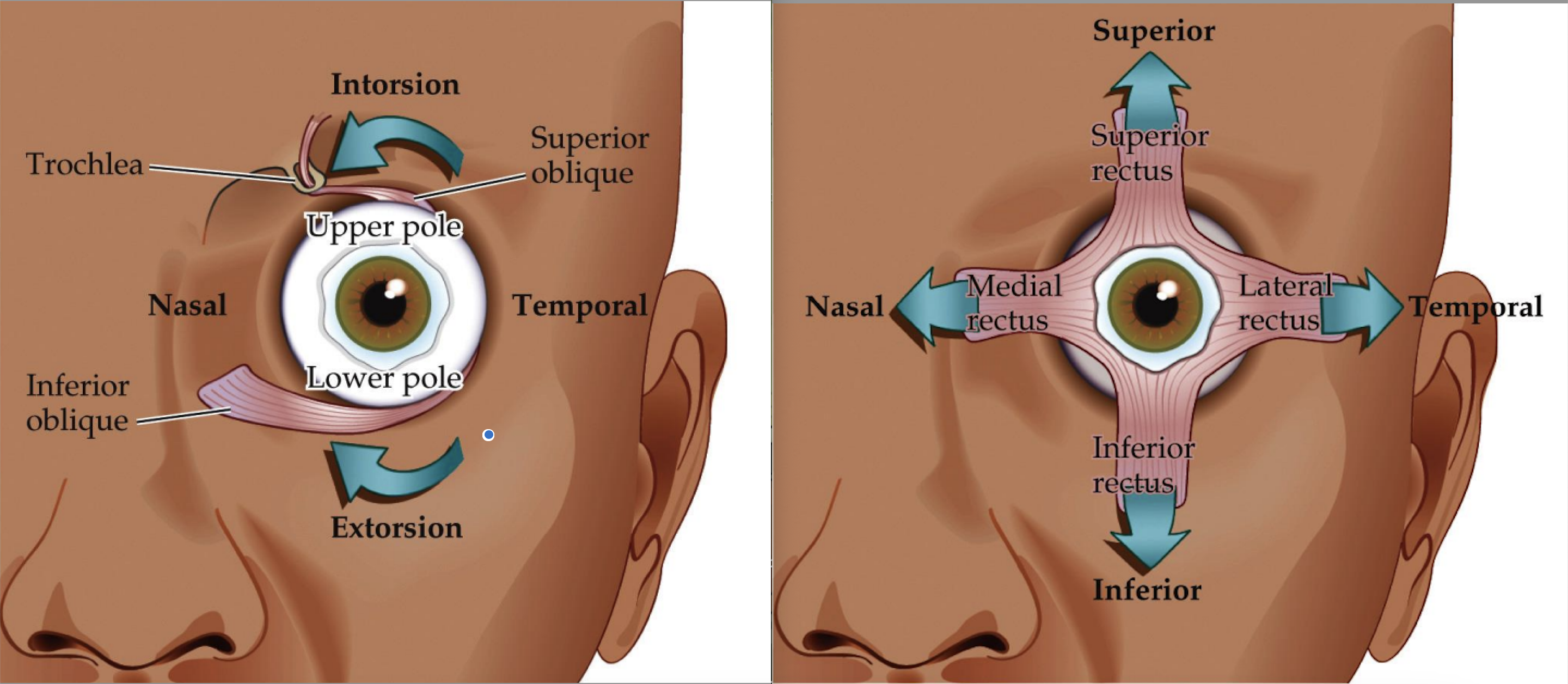
Extraocular Muscles
These muscles are part of the extraocular muscles, which include:
The four rectus muscles (lateral, medial, superior, inferior).
The two oblique muscles (superior and inferior obliques).
Primary Role: Control the direction of eye movement and ensure binocular coordination.
Muscle | Main Action | Comments | Innervation |
Lateral Rectus | Abduction (lateral) movement of the eye | Abduction = temporal | Abducens Nerve (CN VI) |
Medial Rectus | Adduction (medial) movement of the eye | Adduction = nasal | Oculomotor Nerve (CN III) |
Superior Rectus | Elevation and Intorsion (rotation of the top of the eye inwards) | Elevation increases with abduction while intorsion increases with adduction | Oculomotor Nerve (CN III) |
Inferior Rectus | Depression and Extorsion (rotation of the top of the eye outwards) | Depression increases with abduction while extorsion increases with adduction | Oculomotor Nerve (CN III) |
Inferior Oblique | Elevation and Extorsion | Elevation increases with adduction and extorsion increases with abduction | Oculomotor Nerve (CN III) |
Superior Oblique | Depression and Intorsion | Depression increases with adduction and intorsion increases with abduction | Trochlear Nerve (CN IV) |
Lesions
Sympathetic System
Normal Function: The sympathetic system controls the radial muscles of the iris (pupil dilation), eyelid elevation (via superior tarsal muscle), and blood vessel tone.
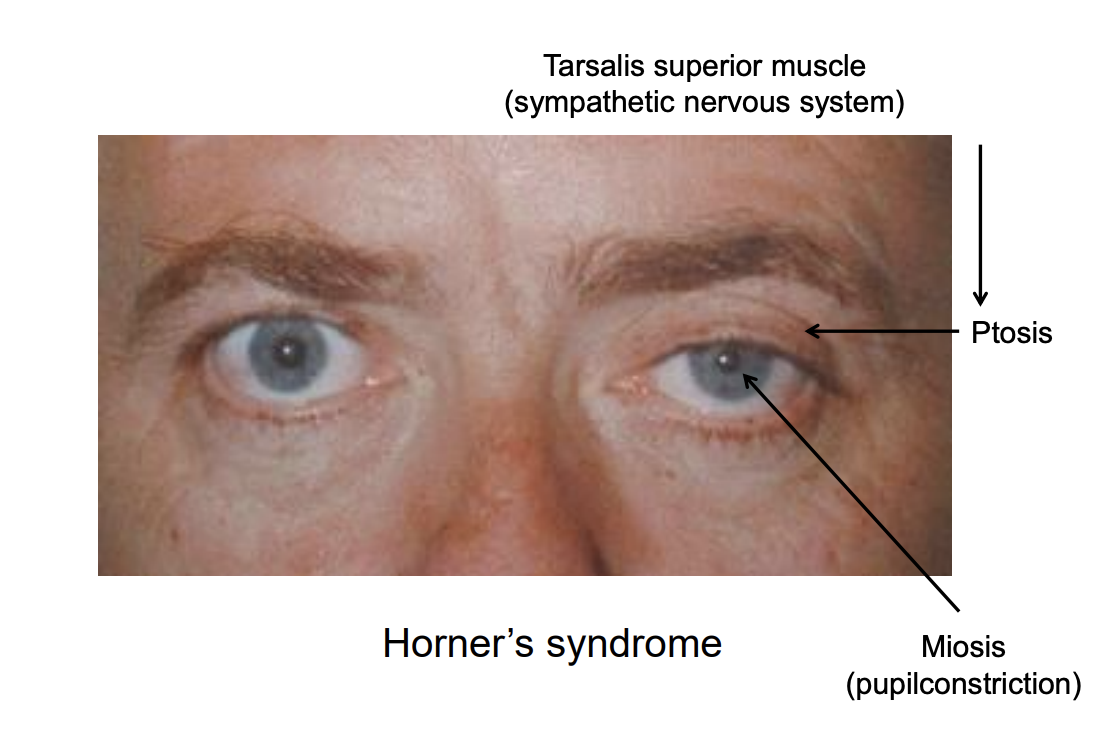
Horner’s Syndrome: Neurological condition caused by a disruption of the sympathetic nervous system pathway that supplies the eye and surrounding structures. This condition results in a characteristic triad of clinical signs: ptosis, miosis, and anhidrosis.
Ptosis: Drooping of the upper eyelid due to paralysis of the superior tarsal muscle (Müller’s muscle), which is under sympathetic control.
Miosis: Constricted pupil due to unopposed parasympathetic action on the circular muscles of the iris.
Anhidrosis: Absence of sweating on the affected side of the face due to sympathetic disruption.
Parasympathetic System
Normal Function: The parasympathetic system controls the circular muscles of the iris (pupil constriction) and ciliary muscles (lens accommodation).
Clinical Signs of Lesion: Often due to damage to the oculomotor nerve (CN III), which carries parasympathetic fibres:
Mydriasis: A dilated pupil due to unopposed sympathetic action on the radial muscles.
Loss of Accommodation: Difficulty focusing on near objects due to ciliary muscle paralysis.
Loss of Light Reflex: Affected eye does not constrict in response to light (direct reflex) or light in the contralateral eye (consensual reflex).
 Knowt
Knowt