Introduction to ME3
Skills Stations
3 rooms (45 mins each)
Skills taught:
Drugs
Assessing the sick patient
Airway
Skills Stations - Seminar
4 scenarios (-30 mins each)
Rotate through, each room will have 2 different medical emergencies
Each group has 4/5 students therefore everyone will get a practice scenario
Individual Test Moulage
Same rooms as per scenario day
Attend and have an assessment of a medical emergency
To complete this component you must:
Have demonstrated BLS competency
Attend the entire course
Complete the CANVAS assessment
Pass individual test moulage
Why do we have to do this?
GDC requirement
Resus council expectation
Public and professional expectation
Ethical duty
Might appear in an OSCE
Incidence of Medical Emergencies
Thankfully rare
Majority occur in adult patients
Paediatric medical emergencies are fast and without warning (child’s under-developed physiology coupled with small oxygen reserves)
Classification
Infants are <1 years old
Children are 1-12
Adults are 12+
What is a Medical Emergency?
Situation where a patient becomes “ill”, may become unconscious, and ultimately their life may be at risk
Can be sudden onset (CVA, cardiac arrest)
Can be slow and progressive
Team Effort
Team leader or team member
Recognise the problem and get help
Assess and monitor the “sick” patient
Get emergency drugs and equipment
Assist patients to self-medicate
Prepare emergency drugs for use
Deal with airway obstruction/choking and cardiac arrest
Liaise with paramedics
Need a leader
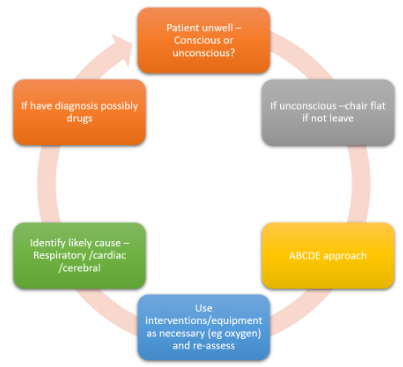
Sequence of Events in a Medical Emergency
Recognise a problem
Get help
Assess patient
Interventions as necessary - oxygen, chair position, drugs, BLS, etc
Monitor
Transfer to paramedics
Physiology of Us
Adequate oxygen entering the airway
All vital organs need oxygen
There must be sufficient oxygen entering the lungs
Upper airway must be open
Problem in unconscious patients and choking patients
Oxygen needs to be absorbed
Oxygen is absorbed into the blood via the lungs
Lower airway must be clear and open
Problem in asthma, anaphylaxis and hyperventilation
Sufficient blood volume present
Sufficient blood volume must be present in the circulation to absorb the oxygen and transport it to vital organs
Problem in anaphylaxis and faints
Pump power
The heart must be pumping properly
There must be sufficient blood pressure to circulate the blood
Problem is angina, MI, cardiac arrest, faints and anaphylaxis
The brain has overall control
The brain is the greater user of oxygen
The nervous system must be functioning properly
Problem in CVA, hypo/hyperglycaemia and seizures
Summary: Four Fundamental Things
Sufficient oxygen absorbed into the blood via the lungs
Sufficient blood present to absorb the oxygen
Sufficient pump power to circulate the oxygenated blood
A functioning nervous system to control all of the above
What Happens in a “Medical Emergency”?
There is a failure of one or more of the fundamental elements
This will progress to a failure of all of them
To treat we need to compensate for the failure, not necessarily diagnose the cause
Using a systematic assessment method will help us to find the primary element affected
Identification of the Primary Failure
Using a standardised ABCDE approach
Note down all observations
Re-assess each time an intervention is done
Re-assess each time something changes
When Someone Starts to Feel Unwell
In an emergency, stay calm
Ensure that you and your staff are safe
Look at the patient generally to see if they “look unwell”
In a conscious patient ask, “How are you?”
If they respond normally - they have a clear airway, are breathing and have brain perfusion with oxygen
ABCDE Assessment
Is the first link in the chain of survival
Treat the problems as we discover them and reassess regularly after each intervention to monitor a patient’s response to treatment
Airway Assessment and Management
Are they able to speak to you?
Look for signs of airway obstruction or swelling
Listen for stridor/gurgling/snoring (partial airway obstructions)
Look in mouth
Opening the Airway - Infants
Aim for a neutral position
Glabella and chin are horizontally aligned
Opening the Airway - Child
Head tilt and chin lift - hand on forehead and two fingers under the mandible
Jaw thrust
Opening the Airway - Adult
Head tilt and chin lift - hand on forehead and two fingers under the mandible
Jaw thrust
Airway Adjuncts
Unconscious or low-conscious patients may need help to keep the airway open
Oropharyngeal Airways (OPAs)
Incisors to the angle of the mandible
Suitable for unconscious patients with no gag reflex
00 (babies) - 4 (adults)
Enter at 180 degrees until past the hard palate and then rotate into the correct position
In children, you can enter the correct way as they have larger soft palates than adults
Nasopharyngeal Airways (NPAs)
Tip of nose to tragus of the ear
Suitable for conscious/unconscious patients with a gag reflex
Not suitable for patients with suspected head injuries or skull fractures
Enter with the bevel facing the septum, with the tube well lubricated (ensure lube isn’t over the end of the adjunct)
Oxygen
Should always be given
15l/min
Venturi mask also called a non-rebreathe mask
If not breathing ventilate with a pocket mask or bag/valve mask 12 per min
Breathing
Recognition of breathing problems ( for no longer than 10s)
Look for respiratory distress, accessory muscles, cyanosis, respiratory rate (above 20 per min indicates a breathing problem) and chest deformity
Listen for noisy breathing and breath sounds
Feel for
Expansion, bilateral; equal
Pulse oximeter if available
Oxygen and Pulse Oximetry
Pulse oximetry: simple, non-invasive tool, provides an instant measure of the arterial blood oxygen saturation
Pulse oximeter probe is designed as a clip to be placed on the finger, having LEDs on one side and a photoreceptor on the opposite
The amount of light transmitted through the tissue is used to calculate the oxygen levels in the blood
In cardiac arrest it’s not very reliable or accurate so we will deliver 100% oxygen
Does not mean there is adequate oxygen in the tissues
Pulse oximetry results are not affected by anaemia, skin colour or jaundice
Pulse oximetry inaccuracies can be the result of:
Haemoglobins such as those present in sickle cell disease
Carbon monoxide poisoning
Nail varnish
Motion artefact
Hypotension/vasoconstriction
Bag Valve Mask
If a patient isn’t breathing on their own or has a reduced respiratory rate (<6 breaths per min)
Used on its own or with oxygen (21% oxygen in air and 85% oxygen with high flow)
2-person technique - good seal and administration of air
Gentle squeezing of the bag with each breath lasting approximately one second
Pocket Mask
Problems are airtight seal, additional oxygen and tiring
Circulation
Count the patient’s pulse - rate, rhythm, both central and peripheral (radial)
Measure capillary refill time (CRT). Apply cutaneous pressure for 5 seconds on the nailbed at heart level (or just above) with enough pressure to cause blanching. Time how long it takes for the skin to return to the colour of the surrounding skin after releasing the pressure. The normal refill time <2s. A prolonged time suggests poor peripheral perfusion.
Look for signs of cyanosis: under the tongue, at the colour of their hands and fingers: are they blue, pink, pale or mottled?
Are you able to measure blood pressure?
Treatment for Circulatory Problems
IV fluids
Chair position
Drugs
Chair Position
The instinct is to put the patient flat
Will prevent and reverse limb pooling
Will increase direct load on the heart
Will cause BP to rise
If patient is conscious then leave them alone unless fainting
If unconscious then put flat for airway control
Disability
Conscious level ACVPU
Pupils (PEARL)
Blood glucose
Make a rapid initial assessment of the patient’s consciousness level using ACVPU
Alert
Confused
Responsive to Voice
Responsive to Pain (squeeze trapezius muscle)
Unresponsive
Check blood glucose level (normal 4-6)
We can also consider signs of neurological injury:
Stroke (FAST) - call 999
PEARL
Place unconscious patients in the recovery position if their airway is not protected
Hypoxia - administer oxygen
Hypoperfusion - raise legs above the heart
Exposure
Rashes, ankle oedema, wounds
Avoid heat loss
Respect the patient’s dignity and minimise heat loss
This will allow you to see any rashes (e.g. anaphylaxis) or ankle oedema (heart failure)
Other wounds?
Review of Sequence
Transfer to Paramedics
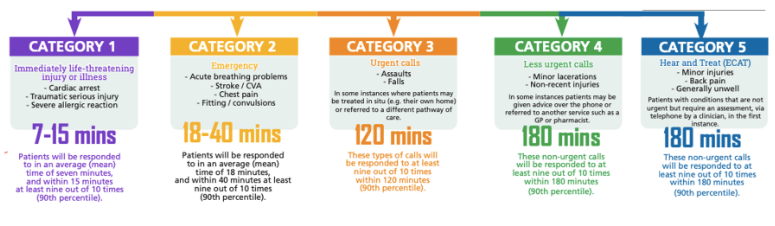
999 calls routed via a controller-specify emergency and “update” if necessary
Documentation is very helpful - record of assessments, etc
Good “handover” helps everyone
What Happens When You Phone an Ambulance?
Handover
Situation - “Hi I am…from…
Background - Patient X attended and…occurred…We have given….
Assessment - I think the problem is…
Recommendation - I need you to admit the patient…Is there anything we can do while awaiting paramedics?”
Emergency Drugs
Patient may carry them (e.g. GTN, EpiPen, Salbutamol inhaler, etc)
Practice will have an emergency drugs kit
There are different routes of administration
Where do we get our Guidance From?
GDC
National INstitute for Health and Care Education
Resuscitation Council UK
Care Quality Commission
Minimum Equipment
Adhesive defibrillator pads
AED
Clear face masks for self-inflating bag (sizes 0-4)
OPA (sizes 0-4)
Oxygen cylinder (CD size)
Oxygen masks with reservoir
Oxygen tubing
Pocket mask with oxygen port
Portable suction e.g. Yankauer
Protective equipment - gloves, aprons, eye protection
Razor
Scissors
Self-inflating bag with reservoir (adult and child)
Drugs
GTN spray 400mcg per actuation
Salbutamol inhaler 100mcg actuation
Adrenaline (1:1000)
Aspirin 300mg
Glucagon injection 1mg
Oral glucose
Midazolam (buccal)10mg (conc 5mg/ml)
Oxygen (size CD) cylinder lasts approx 30 mins
Drugs and the Law
Under the Human Medicines Regulation 2012, legal status for all licensed medicines is determined by the MHRA
All medicines marketed in the UK are classified according to one of the three following categories:
POM - available only on prescription
P - available under the supervision of a pharmacist
GSL - available in general retail outlets such as supermarkets
CD - all CDs are POM but with additional restrictions in place
Misuse of Drugs Act 1971
Main purpose of the act is to prevent the misuse of controlled drugs
The only drug in our kit that is a CD is Midazolam
The law currently (Dec 2021) prevents dental therapists from administering a CD (even in the event of an emergency)
Therapists can only administer midazolam under the direct instruction of a dentist or if following a PSD
Human Medicines Regulations 2012
Permits dental hygienists and therapists to hold emergency drugs on their premises, but not to purchase the medicines directly
A dental hygienist/therapist practice needs to ensure that they hold emergency drugs on-site
Hygienist/therapist practices without an on-site dentist can obtain an emergency kit through a prescribing dentist or doctor under a PGD.
Quality Assurance Process
At least every week, check:
Expiry date for emergency medicines
Equipment and availability of oxygen
The manufacturer’s instructions must be followed about the use, storage, servicing and expiry of equipment. A planned replacement programme should be in place for disposable equipment items that have been used or that reach their expiry date
Individual Medical Emergencies
Choking
The Resuscitation Council provides us with algorithms on how to manage choking
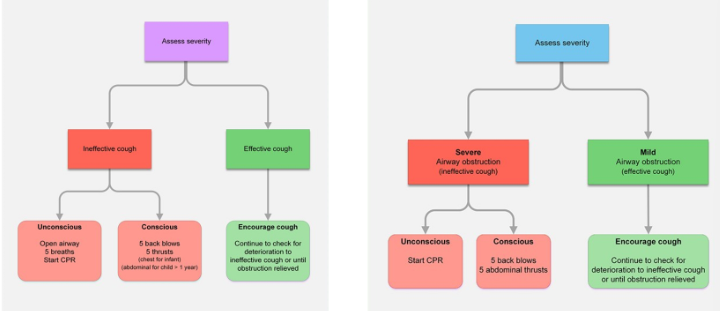
Infant Choking
Lay them face-down on the forearm with our hand supporting their mandible
Give 5 back blows
Turn over and do 5 chest thrusts with 2 index fingers
Faints/Syncope
Also called syncope, vasovagal syncope or vasovagal attack
50% will experience at least once
3% recurrent episodes
Triggers
Prolonged standing
Prolonged exposure to heat
Sudden extreme emotion
Fasting and dehydration
Stress and anxiety
Painful or unpleasant stimuli
Physiology
Trigger produces an effect on the brainstem
Increases activity of parasympathetic nervous system
Drop in heart rate and drop in BP
Decreased activity in the sympathetic nervous system
Dilation of blood vessels causing pooling in the limbs
Reduced venous return causes a further drop in BP
Cerebral hypoxia and loss of consciousness
Symptoms
Hot and sweaty
Pallor
Auditory and visual disturbances
Light-headed and dizzy
Loss of consciousness
Tonic clonic movements may occur
Management
Place patient flat with legs elevated
Give oxygen
Reassure
Slow return to upright position
Pregnant women positioned on their side
Asthma
5.2 million sufferers in the UK
1200 deaths per year
Patients usually have preventative medication and reliever medication
Physiology
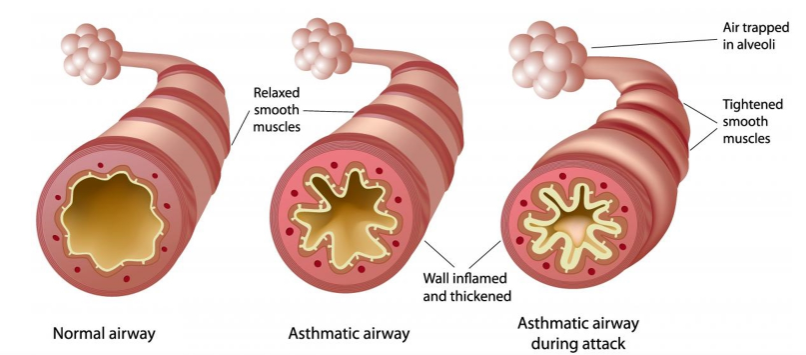
Symptoms
Difficulty breathing
Coughing
Expiratory wheeze
Progresses to use of accessory muscles
RR drops
Loss of consciousness
Avoidance
Be aware of allergens e.g. pollen
Avoid excess exertion
Reduce stress
Weather has effect
Pre-treatment use of inhaler
Treatment
Stop any treatment
Administer high-flow oxygen
Administer patients/surgery’s rescue medications (salbutamol 100mug per actuation)
2-10 puffs, each puff is to be inhaled separately, repeat every 10-20 mins
Same for adult and child
Hypoglycaemia
Low blood sugar level (outside 4-6)
Nervous tissue cannot store glucose therefore needs to access glucose in blood to function properly
If sufficient glucose available fails to function
Signs and Symptoms
Pallor, sweating, cold
Irritable, irrational, confused, aggressive
Loss of consciousness
Coma
Avoidance
Ensure all medication taken as normal
Ask patient if control levels are good
Assess blood glucose levels (monitor)
Consider timings of appointments
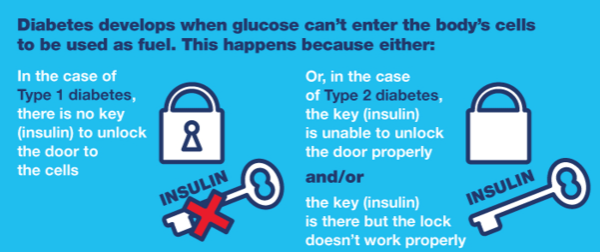
Diabetes
Type 1 - cannot produce insulin therefore must inject
Type 2 - Cells are resistant to the effects of insulin, diet or tablet-controlled
Treatment
Conscious - sugar, glucose drink, chocolate, coca cola
Unconscious - glucagon IM 0.5-1mg
The Heart
Size of a fist
Middle of the chest, a little to the left, under the sternum
Beats 100,000 times a day
Muscular organ that pumps blood around the circulatory system
Pumps 5l of blood continuously
All living tissues of the body require oxygen for life
Blood picks up oxygen as it passes through the lungs
Blood travels from the lungs to the heart before being pumped around the body, delivering oxygen as it goes
It makes its way back to the heart so that it can be returned to the lungs again
Heart Anatomy
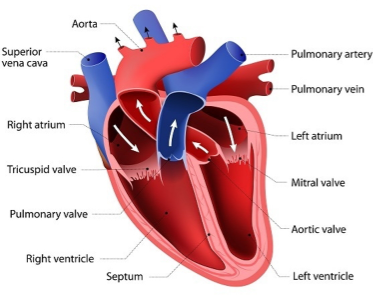
Pulmonary veins bring oxygenated blood from the lungs to the left atrium
Aorta carries oxygenated blood from the left ventricle for circulation around the body
Vena cava: carries deoxygenated blood from the body back to the right atrium of the heart
Pulmonary artery carries deoxygenated blood from the right ventricle to the lungs
Layers of the Heart Wall
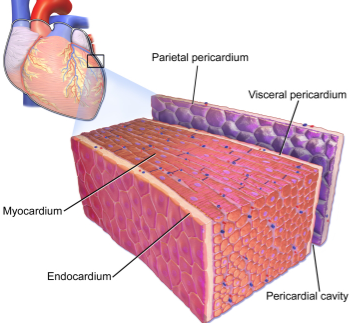
Pericardium: thin outer lining that protects and surrounds the heart
Myocardium: thick muscular tissue of heart that contracts
Endocardium: thin inner lining
The heart needs its own blood supply
Coronary arteries
Narrow if atheroma builds up inside the vessel wall
Risk and lifestyle factors
Heart Attack
MI
Supply of blood to the heart itself (via coronary arteries) is blocked by thrombus or blood clot
Obstruction of blood supply = infarction
Symptoms: chest pain, may travel to the back, arm, neck or jaw, sense of impending doom, squeezing, nausea, sweats
The longer the delay for treatment - the worse the damage
Every minute matters
Heart does not stop beating
Person usually remains conscious
Management:
ME
Administer GTN (1 dose every 5 mins, under tongue)
Call 999
Administer 300mg aspirin
GTN MOA
Rapidly absorbed through the buccal and sublingual mucosa
Peak concentration at 4 mins
Relaxes smooth muscle to produce arterial and venous dilation
Reduce venous return and improves myocardial perfusion
Reduces work of the heart and therefore oxygen demand
Side effects: headaches (due to vasodilation), palpitations and hypotension
Cardiac Arrest
Electrical malfunction of the heart
Causes arrhythmia
Without rhythm, the heart can not beat effectively
Disrupted pumping action means the heart can’t supply the body (or brain) with oxygenated blood
Rapidly leads to loss of consciousness
Death occurs without rapid treatment
Management
Can be reversible
CPR
Defibrillation
Non-shockable: asystole or pulseless electrical activity (PEA)
Shockable: ventricular fibrillation (VF) or ventricular tachycardia (VT)
Reversible Causes of Cardiac Arrest
4Hs:
Hypovolemia
Hypoxia
Hyper/hypokalemia
Hypothermia
4Ts:
Toxins
Tension pneumothorax
Thrombosis
Tamponade
Epilepsy
Generic term for a range of conditions that produce seizures
May be partial or general
Range from periods of “absence” through to tonic-clonic convulsions
Symptoms
Auditory or visual disturbances (aura)
Intense feeling of fear or happiness
Loss of consciousness
Tonic phase - all muscles contract, stiffness, air forced out of the lungs (cries)
Clonic phase independent contraction and relaxation of all muscles - uncoordinated jerky movements, bruxing, vomiting, voiding of bladder and bowels
Management
Prevent the patient from harming themselves
Avoid being harmed yourself
Oxygen
If lasts longer than 5 mins > status epilepticus > paramedics
Midazolam - buccal or nasal
Child 3-11m: 2.5mg
Child 1-4y: 5mg
Child 5-9y: 7.5mg
10+: 10mg
Anaphylaxis
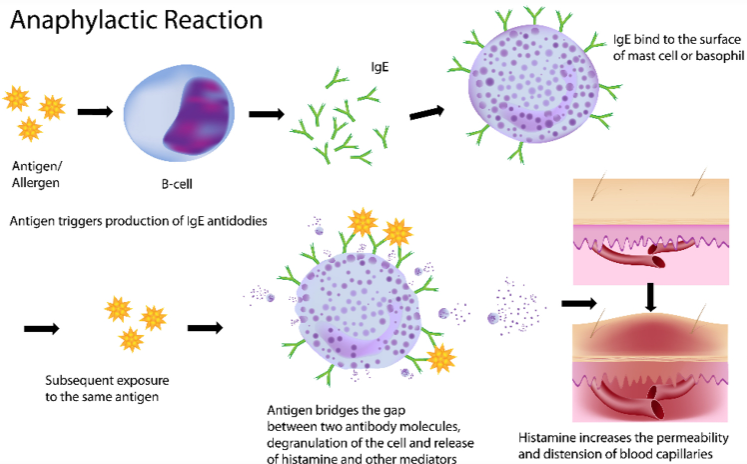
Common Allergens:
Pollen
Penicillin
NSAIDs
Shellfish (haemostats)
Latex
Peanuts
Chlorhexidine
Symptoms
Flushing
Tingling
Itching
Wheezing
Swelling
Disorientation
Light-headed/dizzy
Collapse
Treatment
Oxygen and airway support
Chair position
Adrenaline IM, second dose after 5 mins
Child <6: 0.15mg
Child 6-11: 0.3mg
12+: 0.5mg
Salbutamol if severe wheeze
Other auto-injectors: 3 MHRA approved - Epipen, Jext, Emerald
Respiratory Arrest
Causes
Airway obstruction
Decreased respiratory effort
Maintain airway
Correct ventilation rate
Check pulse every minute