Before
Asthma
Asthma Pathophysiology
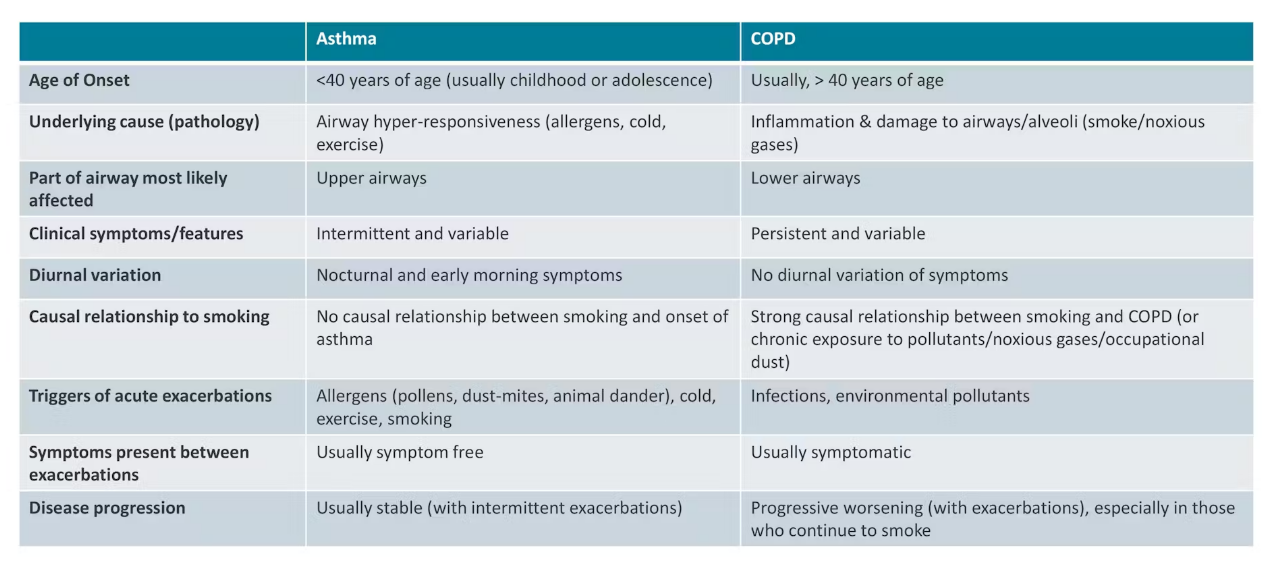
Overview of Respiratory Conditions
Focus on asthma and chronic obstructive pulmonary disease (COPD)
Presentation by Professor Anna Hutchinson, a critical care and respiratory nurse consultant
Asthma Overview
Prevalence:
Affects approximately 12% of boys and 8% of girls in childhood
In adults over 25, prevalence shifts to 12-16% in women and 8-10% in men
Pathophysiology:
Affects lower respiratory tract
Inflammation of lower airways and acute spasm of bronchial smooth muscles
Results in acute narrowing of airways
Symptoms include:
Wheezing
Shortness of breath
Coughing
Chest tightness
Decreased exercise tolerance
Fatigue
Risk Factors for Asthma
Combination of genetic predisposition and environmental exposure
Common Triggers:
Indoor/outdoor air pollution
Cigarette smoking
Household chemicals and cleaning products
Indoor pollutants (dust, molds, pet dander)
Bacterial and viral infections
Acute changes in weather, e.g., cold air, thunderstorms
Emotional changes (anger, fear)
Hormonal changes (pregnancy)
Physical exercise
Medications (e.g., aspirin, NSAIDs, and beta blockers) can worsen asthma
Thunderstorm Asthma
A unique phenomenon occurring in specific Australian states
Triggered by high pollen counts during hot, dry, and windy conditions
2016 Epidemic in Melbourne:
3,365 hospital presentations and 10 deaths within 30 hours
Development of thunderstorm asthma forecasting system for early warnings
Severity of Asthma
Ranges from mild intermittent symptoms to severe persistent inflammation
Severe cases significantly affect quality of life, exercise capacity, and social participation
Untreated episodes can be life-threatening
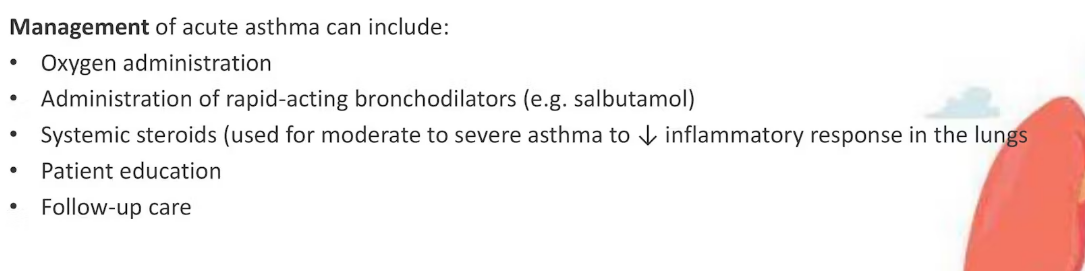
Treatment Strategies
Focus on medications to decrease airway inflammation and treat bronchospasm
Further details will be provided in the next video
Reference to additional resources available through the Victorian Health Department.
Asthma Management - Treatment
Pathophysiology of Asthma
Two key mechanisms drive the condition:
Inflammation of the Upper Respiratory Tract:
Inflammation of bronchial walls leads to acute narrowing of airways.
Chronic untreated inflammation can cause scarring and decrease lung function.
Acute Bronchospasm:
Caused by smooth muscle contraction in the bronchial tree.
Treatment Goals
Goals of asthma management:
• Prevent and Control asthma symptoms
• Maintain lung function and activity
• Prevent morbidity and mortality
Patient education focuses on:
• Avoidance of triggers
• Pharmacotherapy
• Self-management
Asthma action plans (& regular review):
• written document
• helps people with asthma to detect early warning signs/symptoms of an exacerbation
• provides instructions on how to manage exacerbations
The Asthma action plan should include three parts:
1. Maintenance therapy (when well)
2. Early exacerbation management (when not well)
3. Crisis management (If symptoms worsen - Danger Signs)
Types of Medications
Bronchodilators (Relievers)
Medications for rapid relief of asthma symptoms.
Can be used before exercise to prevent exercise-induced bronchoconstriction.
Mechanism of action: relax bronchial smooth muscle (short-acting beta-agonists (SABAs)
Main groups:
Beta-2 Agonists:
Main medications include:
Salbutamol (Ventolin)
Onset time: 2-5 minutes.
Duration of action: 4-6 hours.
Commonly used for acute asthma attacks in community settings.
Terbutaline (Bricilin).
Types:
Short-acting Beta-2 Agonists:
For immediate relief of sudden breathlessness.
Long-acting Beta-2 Agonists:
Maintains action for 12-24 hours, daily dosage for asthma control.
Common examples include Salmeterol and Formoterol.
Preventers
Aim to control asthma symptoms and prevent attacks.
Reduce inflammation, redness, and swelling in airways:
Less sensitivity and lower risk of acute bronchospasm.
Typically delivered as inhalers containing low dosages of corticosteroids routinely (daily)
Mainstay of treatment to address the root causes of asthma symptoms.
"Symptom controller" medications:
Aim: provide long-acting bronchodilation (up to 12 hours)
Mechanism of Action: relax bronchial smooth muscles (long-acting beta- agonists (LABAs))
Administered: once or twice daily
Examples: salmeterol, formoterol (both Beta2-agonists)
Combination Therapies
Used in Australia for moderate to severe asthma treatment.
Combines long-acting bronchodilators with corticosteroids in a single inhaler.
Administered: once or twice daily
Benefits include:
Long-acting reliever to decrease breakthrough symptoms.
Corticosteroid to reduce inflammation in the airways.
Regular use is effective for:
Relieving symptoms.
Stabilizing asthma.
Decreasing the risk of exacerbations.
Improving patient quality of life.
The Nurses Role In Asthma Management
Chapter 1: Introduction to Asthma Management
Overview of Nurses' Roles in Asthma Management
Nurses participate in multidisciplinary teams in primary care settings.
Roles include assessing patients and offering asthma education to improve control.
Diagnosis of Asthma
Involves history, physical examination, ruling out other diagnoses, and spirometry to document airflow limitation.
Identification of asthma triggers is key (e.g., cigarette smoke, allergies, viral infections).
Assessing Asthma Control
Many Australians live with poorly controlled asthma; frequent reliever use (e.g., Ventolin) is often mistaken for normal.
Nurses should engage patients to clarify asthma symptom control and prevention of exacerbations.
Use an evidence-based checklist for assessing control:
Do you wake at night with symptoms?
Do you have symptoms in the morning?
How soon do you need your reliever medication after waking?
How often do you need your reliever during the day?
Are your daily activities or exercise restricted by asthma?
Days off work or school due to asthma in the past couple of weeks?
Chapter 2: Written Asthma Action Plan
Importance of Asthma Action Plans
Action plans should outline key steps during flare-ups, emergency contacts, and therapy.
Emphasize the importance of seeing healthcare professionals if symptoms persist.
Proper Inhaler Use
Correct inhaler technique is crucial; many patients lack proper instruction.
Nurses should observe patients using their inhalers and correct misconceptions.
Resources available for demonstrations of proper inhaler use.
Reviewing the Asthma Action Plan
Nurses should clarify the action plan with patients and families to ensure understanding during emergencies.
Role in community settings: administer medications per action plans and assess treatment responses.
Chapter 3: Signs of Deteriorating Asthma Control
Recognizing Asthma Attacks
Typical signs: increased wheezing, cough, sudden chest tightness, and shortness of breath.
Gradual worsening of symptoms indicated by increased nighttime awakenings or frequent reliever use.
Asthma Emergencies
Define an asthma emergency: sudden severe symptoms, difficulty speaking, or cyanosis (blue lips/fingers).
Immediate action: call an ambulance if relief is not achieved with the inhaler.
Asthma First Aid Steps
Sit the person upright and keep them calm.
Administer four puffs of reliever medication (use a spacer if available).
Wait four minutes and monitor the individual closely.
If still not improving, call an ambulance and repeat salbutamol dosages (four puffs every four minutes).
Chapter 4: Conclusion
Continuous Monitoring
After four minutes, if the person is responding, reassure them while monitoring until normal breathing resumes.
If improvement occurs, follow up with a healthcare provider for check-up.
Asthma First Aid Plans for Different Ages
Review specific first aid plans for adults and children to account for differences in administration methods (e.g., spacer with or without a mask).
Nurses' Crucial Role in Acute Care
Nurses support emergency treatment, assess responses, and provide respiratory care in acute settings (ED, medical wards, ICU).
Further details on managing acute asthma exacerbations will follow.
Chronic Obstructive Pulmonary Disease
Overview of COPD Pathology
Chronic Obstructive Pulmonary Disease (COPD):
A chronic inflammatory disease that leads to obstructive airflow from the lungs.
Symptoms include:
Breathing difficulties
Chronic cough
Increased mucus production
Increased wheezing
Typically results from long-term exposure to irritating gases or particulate matter, most often from cigarette smoke.
Increased risk of developing:
Heart disease
Lung cancer
Other various conditions.
Underlying Conditions
Emphysema:
Characterized by the progressive destruction of alveoli.
Decreases the area available for gas exchange in the lungs, leading to:
Progressive shortness of breath
Decreased exercise tolerance.
Chronic Bronchitis:
Refers to chronic inflammation of the bronchial tubes' lining.
Symptoms include:
Daily cough
Daily mucus production.
Increased risk of:
Lower respiratory tract infections
Pneumonia.
Higher likelihood of requiring frequent hospitalizations for managing exacerbations.
Risk Factors and Exposures
Onset of COPD:
Gradual development over time, often due to a combination of risk factors.
Common exposures that contribute to COPD include:
Tobacco smoke exposure
Occupational exposures
Indoor air pollution
Early life factors such as:
Poor growth in utero
Prematurity
Undertreated childhood asthma.
Alpha-one antitrypsin disorder: Rare genetic condition that leads to early onset and rapid progression of COPD.
Prevalence of COPD
Global Statistics:
In 2019, COPD was the third leading cause of death worldwide.
Almost 90% of COPD deaths in individuals aged 70 and above occur in low and middle-income countries.
COPD in Australia:
Affects both men and women.
Approximately 1 in 13 Australians aged 40 and over have some form of COPD.
About half of these individuals are unaware they have the condition.
Higher prevalence in Indigenous Australians, who are 2.5 times more likely to have COPD than non-Indigenous Australians.
To improve patient outcomes, the following are essential:
Early diagnosis and treatment
Risk factor reduction
Ongoing support to slow disease progression and reduce exacerbation risks.
Diagnosis usually based on:
• History of smoking or exposure to other noxious agents
• FEV1/FVC % (forced expiratory ratio (FER) of ≤70%.
GOLD Stage
FEV₁ (% of predicted value)
Symptoms & Severity
Mild (Stage 1)
≥80%
- May have chronic cough and sputum production.
- Minimal impact on daily life.
- Often undiagnosed at this stage.Moderate (Stage 2)
50-79%
- Worsening breathlessness on exertion.
- Increased cough, sputum production, wheezing.
- May require bronchodilator therapy.Severe (Stage 3)
30-49%
- Significant limitation in daily activities.
- Frequent exacerbations requiring hospitalization.
- Increased risk of respiratory failure.Very Severe (Stage 4)
<30% (or <50% with chronic respiratory failure)
- Extreme breathlessness (even at rest).
- Recurrent exacerbations affecting quality of life.
- May require long-term oxygen therapy (LTOT) or mechanical ventilation.• Other Pulmonary function tests (used to measure lung volumes
and gas diffusion)
• Chest x-ray
• Blood gas analysis
• Physical examination
COPD Management
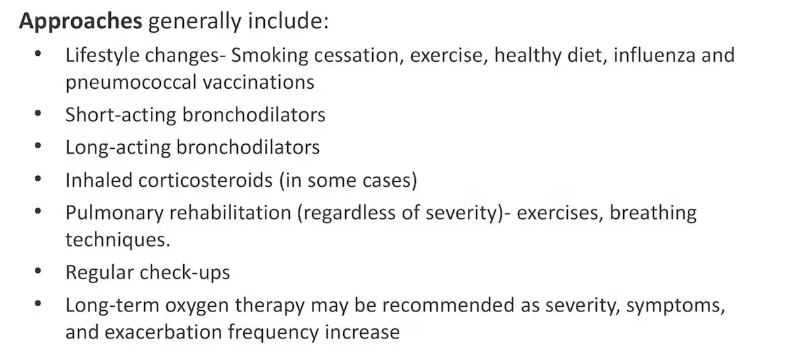
Understanding COPD
Chronic Obstructive Pulmonary Disease (COPD) causes irreversible lung damage.
Early treatment is crucial to enhance quality of life and manage symptoms effectively.
Strategies can be employed to slow progression and minimize flare-ups.
Steps to Improve Quality of Life
Individuals can adopt various approaches for better health and energy, including:
Emotional Self-Care: Focusing on mental and emotional well-being.
Regular Exercise: Essential to prevent muscle weakness and loss of fitness.
Smoking Cessation: Quitting smoking is paramount; it is the most significant lifestyle change one can make.
Importance of Exercise
Everyday Activities: Breathlessness during tasks like walking or washing can deter exercise.
Research Findings: Regular exercise helps:
Maintain fitness
Improve overall well-being
Mitigate symptoms like breathlessness
Pulmonary Rehabilitation:
Specifically designed for individuals with lung conditions.
Programs led by trained specialists (physiotherapists, exercise physiologists).
Tailored to individual fitness levels, emphasizing adaptability rather than traditional exercises.
Benefits of Pulmonary Rehabilitation
Facilitates social interaction and provides a supportive environment.
Improves both physical fitness and mental health.
Teaches essential techniques:
Breathing Techniques: Helps to manage breathlessness.
Sputum Clearance Techniques: Useful for home management.
Post-completion, it is critical to remain active and continue exercise for optimal lung health.
Continuing Support
Lungs in Action Programs:
Offered across Australia, focuses on continued exercise with peers.
Provides a supportive network for those with similar lung conditions.
Emotional Health Considerations
Recognizing that individuals experience COPD differently.
Emotional health directly correlates with symptom severity, affecting social interactions and activity levels.
Importance of maintaining social connections, even during tough days.
Support Groups: Patients are encouraged to seek support from groups or health professionals if feeling overwhelmed.
Additional Health Guidelines
Dietary Approach: Eating a healthy, nutritious diet.
Rest and Sleep: Prioritize sufficient rest and quality sleep.
Vaccinations: Keep vaccinations up-to-date (annual flu shot and pneumonia vaccination) to prevent additional health complications.
Reading Chest X-ray
X-rays are a common diagnostic test used for various conditions and to confirm the position of medical devices such as peripherally inserted central catheters (PICC), intercostal catheters (ICC) and nasogastric tubes.
Interpreting a chest x-ray is an extremely advanced skill however, as a nurse, it is important that you have the ability to identify the normal anatomical structures as well as perform a basic interpretation.
Understanding X-Rays
X-rays are high-energy photons that penetrate body tissues, allowing visualization of internal structures.
They behave similarly to visible light, having reduced penetration in denser materials.
Conventional X-rays display white bones on a black background, resembling photographic negatives:
Dark areas (e.g., lungs) represent regions where more photons penetrate.
Bright white areas show dense bones that block photons.
Importance of a Systematic Approach
Especially crucial for less experienced clinicians.
Reduces chance of missing important findings.
All aspects of interpretation must be included.
Sequence of examination should be logical and easy to remember.
No single best system, but all should start with assessing film quality.
Checklist for Analyzing Chest X-Rays (A to G)
A: Assessment
Begin with patient and exam data verification to avoid errors and ensure the correct study is being examined.
Assess image quality:
Check for proper patient rotation by ensuring medial ends of spinous processes are equidistant from vertebral body borders.
Evaluate inspiration quality; the film should show at least the 10th or 11th ribs for full lung expansion.
Ensure exposure is adequate; adjust brightness to visualize fine lung markings clearly.
Check for air in unintended locations (e.g., pneumothorax, pneumomediastinum). This is crucial for diagnosing surgical emergencies relative to air presence.
B: Bones
Inspect both clavicles and all 12 pairs of ribs for:
Fractures
Deformities
Missing bones
Examine body wall and soft tissues for swelling, masses, or irregularities; often overlooked.
C: Cardiac Silhouette and Size
Assess the cardiac silhouette:
Features include the right atrium, left ventricle, and atrial appendage.
Orientation: Right atrium appears on the left side of the X-ray; left ventricle is on the right.
Normal heart size should be less than 50% of the rib cage's greatest diameter; larger sizes may indicate pathology.
D: Diaphragms
Diaphragms should be symmetric, with appropriate contour.
In lateral views:
Estimate that a normal hemidiaphragm is 1.5 centimeters above the line connecting costophrenic and sternophrenic angles.
E: Equipment and Effusions
Note the placement of lines, tubes, and wires associated with life support:
Endotracheal tubes should be centered in the trachea, at least 2 cm from the tracheal bifurcation.
Nasogastric tubes should be positioned within the stomach.
Check for pleural effusion:
Fluid at costophrenic angles indicates blunting, affecting diagnostic interpretation.
F: Lung Fields
Lung fields should appear symmetric with the absence of:
Haziness
White dots or blotches
Use frontal and lateral X-rays to localize abnormalities:
Example: A nodular mass in the left lung's anterior segment can often be confirmed with CT scans.
G: Great Vessels
Evaluate positioning and size of the great vessels:
Key structures: superior and inferior vena cava, ascending aorta, aortic arch, pulmonary artery, descending aorta.
Orientation: Aortic arch should be positioned highest on the left side; other heart structures should be correctly aligned.
Deviations may indicate underlying congenital issues or disease.
Recap of ABCDEFG Checkpoints
A: Assessment of data, quality, and identifying air abnormalities.
B: Bones in the body wall condition.
C: Cardiac silhouette measurement and size assessment.
D: Diaphragm evaluation for symmetry and flatness.
E: Check equipment placement and effusions.
F: Analysis of lung fields for symmetry and abnormalities.
G: Assessment of the great vessels' position and size.
Focus of the video: systematic approach and normal chest X-ray anatomy.
Learning objectives:
Familiarity with systematic approach for interpreting chest X-rays.
Understanding the correlation between anatomy and normal shadows on an X-ray.
ABCDEF System for Chest X-ray Interpretation
Informally referred to in teaching as the ABCDEF system.
Commonly used in the US, though not perfect.
Breakdown of the system:
A: Airways - trachea in midline, right & left main bronchus.
B: Bones and Soft Tissue - assessment of visible bones.
C: Cardiac Silhouette and Mediastinum - various structures of the heart.
D: Diaphragm - includes gastric air bubble.
E: Effusions - assessment of the pleura.
F: Fields - examination of the lung fields.
Additional consideration: assessing lines, tubes, devices, and prior surgeries.
Lungs evaluated near the end to avoid distraction from significant abnormalities.
Airway Structures (A)
Key anatomical structures visible on normal X-ray:
Trachea - located midline.
Right Main Bronchus - more vertical angle.
Left Main Bronchus - more horizontal angle.
Implications:
Increased likelihood of foreign body aspiration into right lung.
Risk of endotracheal tube misplacement into right bronchus.
Bones and Soft Tissue (B)
Identifiable bones on PA/lateral X-ray:
Ribs: posterior and anterior components.
Clavicles: right and left visible.
Sternum: may be obscured on lateral view.
Vertebral Bodies: usually visible on PA when quality is adequate.
Cardiac Silhouette and Mediastinum (C)
Components to evaluate:
Shapes and sizes forming the cardiac silhouette.
Notable structures include the aortopulmonary window (location for recurrent laryngeal nerve and lymph nodes).
Visualization techniques:
Use drawings for anatomy understanding.
Diaphragm and Pleura (D)
Diaphragm characteristics:
Right hemidiaphragm generally higher due to liver.
Curvature represents 3D structure; assess both views.
Pleura:
Surrounds lungs, usually invisible due to thinness.
Costophrenic angles:
Right and left angles assess pleural spaces.
Posterior costophrenic angle visible on lateral.
Gastric air bubble under left hemidiaphragm indicates stomach position.
Lung Fields and Fissures (F)
Structures to examine in lungs:
Fissures:
One horizontal fissure visible on right, not usually visible in left lung.
Two oblique fissures on right, and one on left.
Lobes:
Right lung: divided into three lobes (upper, middle, lower).
Left lung: divided into two lobes (upper, lower).
Fissure visibility aids in localization of lung abnormalities.
Passive Smoking & Its Impact on Asthma and COPD
Passive smoking (also known as secondhand smoke) occurs when a person inhales smoke from burning tobacco products or exhaled smoke from a smoker. It contains harmful chemicals like carbon monoxide, nicotine, formaldehyde, and benzene, which can damage lung tissue and trigger respiratory conditions.
Here’s how passive smoking affects asthma and COPD:
Impact of Passive Smoking on Asthma
Trigger for Asthma Attacks – Secondhand smoke is a common asthma trigger, leading to bronchoconstriction, inflammation, and excess mucus production.
Increased Severity & Frequency of Attacks – Children exposed to secondhand smoke have more frequent and severe asthma attacks than those in smoke-free environments.
Higher Risk of Developing Asthma – Long-term exposure to passive smoke increases the risk of developing asthma, especially in children.
Reduced Response to Treatment – Asthma patients exposed to secondhand smoke often respond poorly to medications, such as inhaled corticosteroids.
💡 Key Point: Passive smoking does not cause asthma directly, but it significantly worsens symptoms, increases attacks, and reduces treatment effectiveness.
Impact of Passive Smoking on COPD
Increased Risk of Developing COPD – Long-term exposure to secondhand smoke can lead to chronic bronchitis, airway inflammation, and lung damage, increasing the risk of COPD later in life.
Accelerated Lung Function Decline – Even in non-smokers, exposure to secondhand smoke can cause irreversible lung damage, leading to progressive airway obstruction.
More Frequent COPD Exacerbations – Passive smoking worsens COPD symptoms, leading to more frequent flare-ups, hospitalizations, and faster disease progression.
Increased Mortality Risk – Studies suggest that long-term secondhand smoke exposure raises the risk of premature death in COPD patients.
💡 Key Point: Passive smoking is a major risk factor for COPD, contributing to its development, worsening symptoms, and faster disease progression.
Updated Table Including Passive Smoking:
Category | Asthma | COPD |
|---|---|---|
Age of Onset | Often childhood or adolescence | Usually after 40 years old |
Underlying cause (pathology) | Chronic inflammation due to allergens or irritants | Chronic inflammation due to long-term exposure to irritants (e.g., smoking) |
Part of airway most likely affected | Bronchi (large airways) | Small airways and alveoli |
Clinical symptoms/features | Wheezing, shortness of breath, chest tightness, cough (episodic) | Chronic cough, sputum production, progressive breathlessness |
Diurnal variation | Symptoms often worse at night or early morning | Less variation, symptoms persistent |
Causal relationship to smoking | Not directly related (though can be worsened by smoking, including passive smoking) | Strongly linked to smoking and secondhand smoke exposure |
Triggers of acute exacerbations | Allergens, cold air, exercise, respiratory infections, passive smoking | Infections, air pollution, smoking, passive smoking, environmental exposure |
Symptoms between exacerbations | Often asymptomatic or mild symptoms | Persistent symptoms even between exacerbations |
Disease progression | - Symptoms are usually intermittent and reversible.- Poor control can lead to airway remodeling, making asthma less reversible.- Severe exacerbations can cause respiratory failure, but long-term lung damage is rare with proper treatment. | - Symptoms worsen gradually over time.- Permanent airflow limitation due to fibrosis, airway remodeling, and alveolar damage.- Exacerbations accelerate lung decline, leading to chronic respiratory failure.- Often leads to high mortality in severe stages. |
Reason for Airway Blockage | Inflammation & swelling of the airway walls, bronchoconstriction, and excess mucus production block airflow. The narrowing is reversible with treatment. | Chronic inflammation, structural changes (fibrosis & scarring), mucus hypersecretion, and alveolar damage (leading to trapped air) cause permanent and progressive airway blockage. |
Impact of Passive Smoking | - Triggers asthma attacks and worsens symptoms.- Increases severity and frequency of attacks.- Raises the risk of asthma development, especially in children.- Reduces effectiveness of asthma medications. | - Major risk factor for COPD development.- Causes permanent lung damage, even in non-smokers.- Speeds up disease progression and increases exacerbations.- Increases the risk of premature death in COPD patients. |
Final Thoughts
Asthma patients exposed to secondhand smoke experience more severe attacks and reduced treatment effectiveness.
COPD patients exposed to secondhand smoke suffer faster lung decline, more hospitalizations, and increased mortality risk.
Avoiding passive smoking is critical for managing both conditions and preventing long-term lung damage.
Let me know if you need any further additions! 😊
Category | Asthma | COPD |
|---|---|---|
Age of Onset | Often childhood or adolescence | Usually after 40 years old |
Underlying cause (pathology) | Chronic inflammation due to allergens or irritants | Chronic inflammation due to long-term exposure to irritants (e.g., smoking) |
Part of airway most likely affected | Bronchi (large airways) | Small airways and alveoli |
Clinical symptoms/features | Wheezing, shortness of breath, chest tightness, cough (episodic) | Chronic cough, sputum production, progressive breathlessness |
Diurnal variation | Symptoms often worse at night or early morning | Less variation, symptoms persistent |
Causal relationship to smoking | Not directly related (though can be worsened by smoking, including passive smoking) | Strongly linked to smoking and secondhand smoke exposure |
Triggers of acute exacerbations | Allergens, cold air, exercise, respiratory infections, passive smoking | Infections, air pollution, smoking, passive smoking, environmental exposure |
Symptoms between exacerbations | Often asymptomatic or mild symptoms | Persistent symptoms even between exacerbations |
Disease progression | - Symptoms are usually intermittent and reversible.- Poor control can lead to airway remodeling, making asthma less reversible.- Severe exacerbations can cause respiratory failure, but long-term lung damage is rare with proper treatment. | - Symptoms worsen gradually over time.- Permanent airflow limitation due to fibrosis, airway remodeling, and alveolar damage.- Exacerbations accelerate lung decline, leading to chronic respiratory failure.- Often leads to high mortality in severe stages. |
Reason for Airway Blockage | Inflammation & swelling of the airway walls, bronchoconstriction, and excess mucus production block airflow. The narrowing is reversible with treatment. | Chronic inflammation, structural changes (fibrosis & scarring), mucus hypersecretion, and alveolar damage (leading to trapped air) cause permanent and progressive airway blockage. |
Impact of Passive Smoking | - Triggers asthma attacks and worsens symptoms.- Increases severity and frequency of attacks.- Raises the risk of asthma development, especially in children.- Reduces effectiveness of asthma medications. | - Major risk factor for COPD development.- Causes permanent lung damage, even in non-smokers.- Speeds up disease progression and increases exacerbations.- Increases the risk of premature death in COPD patients. |
Asthma vs COPD
Category | Asthma | COPD |
|---|---|---|
Age of Onset | Often childhood or adolescence | Usually after 40 years old |
Underlying cause (pathology) | Chronic inflammation due to allergens or irritants | Chronic inflammation due to long-term exposure to irritants (e.g., smoking) |
Part of airway most likely affected | Bronchi (large airways) | Small airways and alveoli |
Clinical symptoms/features | Wheezing, shortness of breath, chest tightness, cough (episodic) | Chronic cough, sputum production, progressive breathlessness |
Diurnal variation | Symptoms often worse at night or early morning | Less variation, symptoms persistent |
Causal relationship to smoking | Not directly related (though can be worsened by smoking, including passive smoking) | Strongly linked to smoking and secondhand smoke exposure |
Triggers of acute exacerbations | Allergens, cold air, exercise, respiratory infections, passive smoking | Infections, air pollution, smoking, passive smoking, environmental exposure |
Symptoms between exacerbations | Often asymptomatic or mild symptoms | Persistent symptoms even between exacerbations |
Disease progression | - Symptoms are usually intermittent and reversible.- Poor control can lead to airway remodeling, making asthma less reversible.- Severe exacerbations can cause respiratory failure, but long-term lung damage is rare with proper treatment. | - Symptoms worsen gradually over time.- Permanent airflow limitation due to fibrosis, airway remodeling, and alveolar damage.- Exacerbations accelerate lung decline, leading to chronic respiratory failure.- Often leads to high mortality in severe stages. |
Reason for Airway Blockage | Inflammation & swelling of the airway walls, bronchoconstriction, and excess mucus production block airflow. The narrowing is reversible with treatment. | Chronic inflammation, structural changes (fibrosis & scarring), mucus hypersecretion, and alveolar damage (leading to trapped air) cause permanent and progressive airway blockage. |
Impact of Passive Smoking | - Triggers asthma attacks and worsens symptoms.- Increases severity and frequency of attacks.- Raises the risk of asthma development, especially in children.- Reduces effectiveness of asthma medications. | - Major risk factor for COPD development.- Causes permanent lung damage, even in non-smokers.- Speeds up disease progression and increases exacerbations.- Increases the risk of premature death in COPD patients. |
Case Study
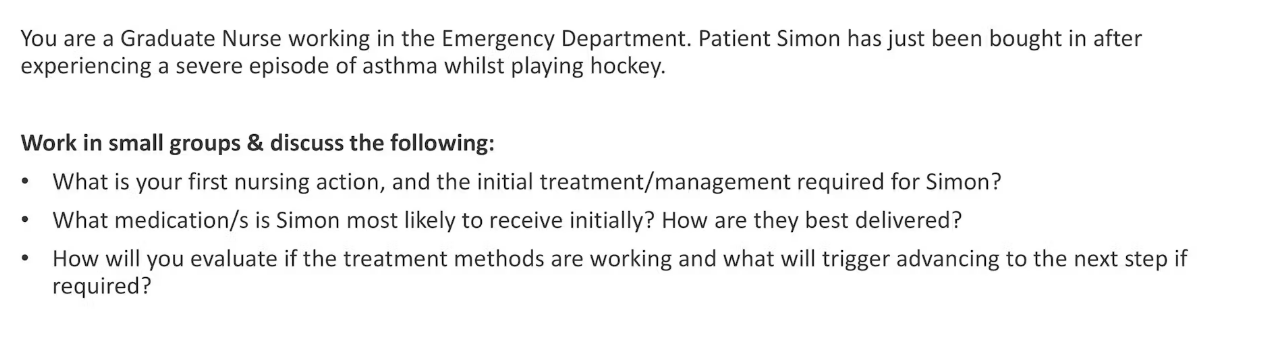
1. First Nursing Action & Initial Treatment/Management for Simon
Rapid Assessment (ABCDE Approach)
Airway: Ensure the airway is open and not obstructed.
Breathing: Assess respiratory rate, oxygen saturation (SpO₂), and auscultate lung sounds for wheezing or silent chest (a dangerous sign of severe obstruction).
Circulation: Monitor heart rate and blood pressure (tachycardia may indicate hypoxia or medication side effects).
Disability: Assess consciousness level (severe hypoxia can lead to confusion or agitation).
Exposure: Identify any environmental triggers (e.g., cold air, allergens).
Administer Oxygen Therapy (if required)
If oxygen saturation <92%, administer high-flow oxygen (via non-rebreather mask at 6-8 L/min) to prevent hypoxia.
Positioning
Sit Simon in an upright position to ease breathing and lung expansion.
Monitor for Life-Threatening Signs
Silent chest (no wheezing, no air entry)
Severe fatigue or confusion (signs of respiratory failure)
Cyanosis (blue lips or fingers)
Respiratory rate >25 or <8 breaths per minute
Unable to speak in full sentences
If any of these signs are present, urgent escalation to critical care is required.
2. Medications Simon is Most Likely to Receive Initially & Delivery Method
1st Line: Short-Acting Beta-2 Agonist (SABA) – Salbutamol (Ventolin)
How is it delivered?
Nebulizer (preferred in severe asthma): 5mg salbutamol nebulized with oxygen, repeated every 20 minutes as needed.
Metered-Dose Inhaler (MDI) with Spacer: 4-10 puffs, repeated every 20 minutes for 1 hour.
Purpose: Quickly relaxes airway muscles, relieving bronchoconstriction.
2nd Line: Anticholinergic – Ipratropium Bromide (Atrovent)
How is it delivered?
Via nebulizer (500 mcg every 20-30 minutes for up to 3 doses).
Purpose: Provides additional bronchodilation, especially in severe cases.
3rd Line: Systemic Corticosteroids – Prednisolone or IV Hydrocortisone
How is it delivered?
Oral Prednisolone: 40-50 mg once daily for 5 days.
IV Hydrocortisone (if unable to take oral medication): 100mg every 6 hours.
Purpose: Reduces airway inflammation and prevents further exacerbation.
If No Improvement:
Consider IV Magnesium Sulfate (1.2-2g over 20 minutes) for severe cases or IV Prednisolone
Epinephrine (IM Adrenaline) if there is suspicion of anaphylaxis or if the patient is not responding to usual treatment.
3. Evaluating Treatment Effectiveness & When to Escalate Care
Monitor Improvement:
Signs of Recovery:
Reduced respiratory rate
Improved oxygen saturation (>95%)
Reduced wheezing, ability to speak in full sentences
Decreased use of accessory muscles (less chest retraction)
Peak expiratory flow rate (PEFR) improving toward baseline
Signs Treatment Is Not Working (Requires Escalation):
Persistent severe breathlessness despite treatment
Deteriorating SpO₂ (<90%) even with oxygen support
Silent chest (no wheezing, no air movement)
Exhaustion, confusion, or drowsiness (impending respiratory failure)
Blood gas abnormalities (respiratory acidosis, CO₂ retention)
🚨 If Simon Deteriorates Further:
Escalate to ICU for ventilation support (Non-Invasive Ventilation or Intubation)
Consider ICU referral if continuous nebulization, IV therapy, and oxygen therapy do not stabilize the patient.
Conclusion
Immediate interventions: Oxygen, bronchodilators (salbutamol + ipratropium), and corticosteroids.
Delivery method: Nebulizer for severe cases, inhaler/spacer if moderate.
Monitor for response: If persistent severe symptoms, consider IV therapy or ICU escalation.
 Knowt
Knowt