explanation and treatment of disorders
phobias
A phobia is an irrational fear of an object or situation. It is a type of anxiety disorder that produces emotional reactions to potentially dangerous stimulus, they are uncontrollable and out of proportion to any actual risk.
Symptoms:
Behavioural:
Panic — crying, screaming, running away
Avoidance — reinforces fear
Disruption of functioning — strong anxiety causes failure to function adequately (e.g not just avoiding the situation, but not going out at all)
Emotional:
Persistent, excessive fear — high levels of anxiety due to fear of object, prevents from relaxing
Fear from exposure to stimulus — produces immediate fear response (e.g panic attacks, fight or flight response)
Cognitive:
Selective attention — sufferer finds it hard to look away from phobic stimulus (keeping attention on something dangerous gives us a better chance to react)
Irrational beliefs — recognition of exaggerated anxiety, usually sufferer is aware that their anxiety is overstated but can’t change it
Cognitive distortions — perceiving phobic stimulus differently
Types of phobias:
Simple phobias — fear of specific objects or situations
Includes: animals (e.g spider), injuries (e.g blood), situational (e.g flying), natural environment (e.g water)
Social phobias — fear of a social situation
Includes: performance (e.g playing in a concert), interaction (e.g date/interview), generalised (lot’s of people)
Agoraphobia — fear of leaving a safe space (usually home)/fear of open spaces
behaviourist explanation and treatment of phobias
Two process model:
Acquisition (CC):
Phobic stimulus (neutral) is paired with unconditioned stimulus, creating an association
Phobic stimulus creates fear response originally created by UCS
Fear response can also be generalised for other stimuli
Maintenance (OC):
The avoidance behaviour reduces anxiety
Negative reinforcement occurs, strengthens the behaviour and the likelihood that it will be repeated
Little Albert study (Watson and Rayner):
Aim: see if it’s possible to induce a fear to a previously neutral stimulus, through classical conditioning
Procedure:
11 month old Albert
He was presented with a rat and initially had no reaction
He was then presented with the rat paired with loud bang (which he would reflexively be scared of) repeatedly
Results: he showed signs of fear towards rat and objects similar like white rabbits, santa beard, cotton wool ect. — generalisation
Conclusion: a fear response has been conditioned using CC and generalisation also occurred
Other studies:
Bagby — reported case study of a woman with phobia of running water that originated from getting her feet stuck in rocks near a waterfall (time stuck made her increasing more panic stricken).
King et al 1998 — case studies that showed children tend to acquire strong phobias after traumatic experience (supports idea of acquisition through CC)
Evaluation:
P — applicable
E — this is because it allows us to identify how a phobia may have been learned and then devise an effective means of treating this phobia, specifically using systematic desensitisation to erase conditioned fear
E — therefore, explaining phobias through this approach is beneficial to society
P — reductionist
E — this is because it is based on the idea that phobias are learnt through association/reinforcement so excludes biological basis that phobia may form, for instance, by abnormal abnormal NT levels or genetic influence
E — therefore = simplistic and ineffective
P — individual differences ignored (assumes everyone’s reaction will be the same)
E — the intensity of the phobia and the support network available to individual will affect their reaction, e.g someone with social anxiety but supportive friends and family may be more able to engage in social situations than someone without
E — therefore, explanation of phobias and idea that they’re all the same is invalid
Treatment for phobias:
Systematic desensitisation is a type of behaviourist therapy to treat phobias/anxiety, created by Wolpe 1961.
Principles of CC, to replace conditioned response (anxiety or fear) with a relaxation response
Client is gradually exposed to (or imagines) the threatening situation under relaxed conditions until the anxiety is extinguished
Stages:
Functional analysis — client and therapist construct a fear hierarchy (list of situations where client would feel anxiety, arranged from least to most) and treatment goals
Relaxation training — client is taught different techniques for relaxing, including breathing and muscle control
Gradual exposure — over the course (6 to 12 sessions), client is gradually brought into contract with phobia, starting at the bottom of fear hierarchy and working way up using relaxation techniques to feel comfortable with exposure
Systematic desensitisation works on the key principle of reciprocal inhibition:
Individual can’t have negative thoughts about something if they have positive thoughts instead
Suggests that conditioned fear response =/= fear and calm together, so fear must be replaced with calmness
Another type of behaviourist treatment for phobias is flooding (implosion therapy), where patient is immediately exposed to fear.
Initially, person is in extreme state of extreme anxiety (sympathetic state) but exhaustion will set in and anxiety levels decrease with switch to parasympathetic
When panic subsides, they realise they have come to no harm and fear (which to a large degree was anticipatory) is extinguished
Studies on phobia treatments:
Bronson and thorpe — 30 technophobes, some assigned to SD programme and the rest given no treatment. control group with 59 non-anxious participants. Results showed that reduction in anxiety was 3x greater than non-treated and after a year, treated group had same anxiety levels as controls
Wolpe — used flooding to remove girl’s phobia of being in cars. She was forced into a car and driven around for 4 hours until her hysteria disappeared
Barlow — flooding shown to be as equally effective as SD but SD preferred by patients because they can tolerate it better
Ost — flooding delivers rapid immediate improvements, esp when patient asked to continue self-directed exposure to feared stimulus outside of sessions
Evaluation of phobia treatments:
Effective
Gilroy et al — 43 patients treated for spider phobia with 3 45-min sessions of SD. Phobia then assessed with questionnaire and response to a spider, control group treated with relaxation but no exposure. SD group was found to be less fearful.
Suitable for a range of patients — learning difficulties and anxiety disorder can also be treated
SD can be extensive with long sessions over long periods
Flooding is cost effective and quick
Flooding is less effective for some types of phobias (complex phobias like social ones)
Flooding is traumatic and breaks ethical guidelines
Both SD and flooding proven effective, aim to replace conditioned response with neutral one as a long term treatment
Environmentally reductionist explanation as uses CC and ignores bio approach that would use drug therapies, some phobias are biological so simplistic idea to say they can just be unlearnt
Both are considered unethical as require patients to undergo intense stress (but SD gradual so more ethical). Therapy should only go ahead if benefits outweigh stress
depression
Depression is a mental disorder characterised by low mood and low energy levels.
It is an affective mood disorder with an average onset at mid-20s
10% diagnosed commit suicide but 60% of suicides linked to depression
5 symptoms everyday for 2 weeks = major depressions and 3 symptoms for 2 weeks = dysthymic depression
DSM5 criteria includes: changes to mood, irritable, decreased interest and at least 5% weight change.
Causes:
Endogenous depression (biochemical)
Exogenous depression (reactive)
Types:
Major depressive disorder — severe/short term
Depressed mood, lost interest
Impaired function (social, occupational, educational)
Change in sleep (insomnia or hypersomnia)
Change in activity
Persistent depressive disorder — long term depression
Disruptive mood dysregulation — childhood tantrums
Premenstrual dysphoric disorder — depression prior/during menstruation
Unipolar depression:
Major depression (without mania)
Behavioural symptoms — loss of energy, social impairment, weight changes, poor personal hygiene, sleep pattern disturbances
Emotional symptoms — loss of enthusiasm, constant depressed mood, guilt and worthlessness
Cognitive symptoms — delusions, reduced concentrations, thoughts of death, poor memory
Bipolar depression:
Manic depression, extreme lows —> highs
Behavioural symptoms — depressive symptoms as well as being energetic, racing thoughts, mixed episodes or rapid cycling, recklessness, talkative
Emotional symptoms — depressive symptoms as well as high self esteem, euphoria, irritability/frustration (not getting their way, lack of guilt
Cognitive symptoms — depressive symptoms as well as delusions of grandeur (intense importance or paranoia), poor decision making
cognitive explanation and treatment of depression
The cognitive approach believes that an individual is the cause of their behaviour because they have control over their thoughts. Abnormality is the result of faulty control and mental disorders are likely to occur as a result of irrational thinking.
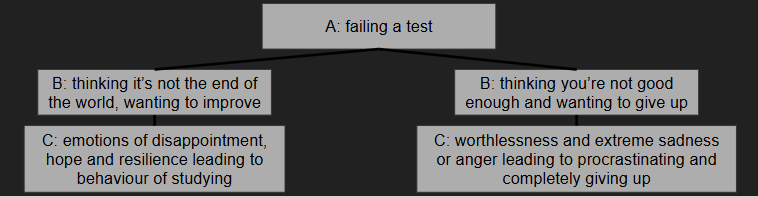
Albert Ellis ABC model:
Cognitions (thinking and expectations) cause behaviour and irrational thinking prevents person behaving adaptively
This creates symptoms of depression
A — activating event
B — belief (rational or irrational)
C — consequence (positive or negative)
Example:
Beck’s negative triad:
Faulty information processing (black and white absolutist thinking) and negative self schema contribute to negative thinking
Negative thinking results in depression
The negative triad is an automatic, dysfunctional response that results in negative views about the self, the world and the future, leading to depressive symptoms.
Negative triad is maintained by 4 cognitive biases/errors:
Arbitrary inference — conclusions drawn in the absence of sufficient evidence (e.g man thinks he is worthless because it rains during his outdoor party)
Selective abstraction — conclusions drawn from 1 part of the situation (e.g worker feeling worthless when product doesn’t work, even though several people helped make it)
Overgeneralisation — conclusions drawn on the basis of a single event (e.g student uses poor performance on 1 test as proof of his whole worthlessness)
Magnification/minimisation — exaggerations in evaluation of performance (e.g man believes he’s ruined his car because of a small scratch and woman downplaying praise)
Studies:
Boury et al — monitored student’s negative thoughts with Beck depression inventory, found that depressive patients misinterpret facts and experiences in a negative fashion (they had pictures shown and asked about the emotions in them) and they also feel hopeless about the future
Rimm and litvak — controlled setting, manipulating individuals into thinking in a negative irrational by giving them negative comments about themselves. They became more and more depressed as a consequence.
Evaluation of cognitive explanation:
Treating depression using cognitive behavioural therapy has proven very effective. This therapy is based on cognitive assumption that negative, irrational beliefs contribute to disorders, and aims to alter these beliefs. It shows support for the approach.
Cognitive approach to depression is less successful in explaining manic depression. The approach focuses on unipolar depressive thinking and ignores mania/bipolar type of depression. Therefore, cognitive approach can be seen as incomplete.
Cognitive treatment of depression:
CBT is a combination of cognitive therapy (a way of changing maladaptive thoughts and beliefs) and behavioural therapy (a way of changing behaviour resulting from maladaptive thoughts.
REBT — rational emotive behavioural therapy (a type of CBT)
1-2 sessions every week for about 15 sessions, with booster sessions given in subsequent years to prevent relapse. 3 stages:
Stage 1: ‘education phase’, patients are taught to recognise and record activating events that lead to distorted thinking in a ‘dysfunctional thought diary’, triggers and negative thoughts/emotions are all noted
Stage 2: ‘behavioural activation’, therapist can then work to help patient challenge their beliefs so they can be disproved, e.g playing devil’s advocate or asking them for evidence for their beliefs (‘stun technique’). This should help break their negative bias like arbitrary inferences and make behaviours more normal
In REBT, therapist focuses on patient’s controlling of their emotions and teach them relaxation strategies like relaxation imagery so they can avoid exaggerated and emotional/behavioural response when coming across an activating event again.
Stage 3: ‘pleasant event scheduling’, therapist plans with client positive things to focus on, for example meeting up with friends or learning a new hobby. This is done to motivate them and decrease symptoms like avolition
Embling study on CBT:
Aim — to examine the process and outcome of the use of CBT to treat depression
Procedure — 38 clients (on drug treatment) in treatment group receiving CBT and control group of matched age/gender/social support which didn’t receive treatment other than drugs. Data from dysfunctional thought diaries and Beck’s depression inventory score analysed
Results — CBT is effective for depression. When reporting emotions on similar activating events, the stronger the emotion invoked, the more abnormal the behaviour (supports need for REBT for coping strategies)
Conclusion — use of drug therapy and CBT has best outcomes in treatment of depression
Evaluations:
Strengths
CBT tackles the root of the disorder (faulty thinking) in hopes of long term effects rather than just inhibiting symptoms
Weaknesses
Only certain types of people can engage in REBT effectively like those with good communication skills and not suffering with developmental issues that affect communication like deafness
CBT costs more to healthcare than drug treatment. at a time of reduced healthcare budgets, CBT access for patients is limited and waiting lists are usually long = patients have negative views of the treatment, all reducing effectiveness
OCD
OCD is an anxiety disorder where sufferers experience persistent and intrusive thoughts occurring as obsession, compulsions or both. It has an incidence rate of 2%.
Symptoms:
Obsession (thought) —
Behavioural symptoms
Hindered everyday functioning — due to reoccurring obsessions
Social impairment — can’t have meaningful social interactions
Emotional
Extreme anxiety — persistent, inappropriate or forbidden ideals (urge to repeat behaviours creates anxiety)
Cognitive
Recurrent and persistent thoughts — repeated and of intrusive nature
Recognised as self generated — understanding that they are self-motivated and not from external agents
Attention bias — perception focused on anxiety generating stimuli
Compulsions (actions) —
Behavioural symptoms
Repetitive — feel compelled to repeat them
Hindered everyday functioning — performing compulsions disrupts life
Social impairment — can’t have meaningful relationships due to behaviours
Emotional
Distress — recognise the urges can’t be controlled which creates anxiety
Embarrassment — the suffer knows they are behaving irrationally and creates shame from others
Cognitive
Uncontrollable thoughts about urges that can be controlled and reduced anxiety by acting out behaviour
Realisation of inappropriateness as they understand that they are inappropriate but can’t do anything about it
biological explanation and treatment of OCD
Genetic explanation of OCD:
Genes:
COMT gene
Regulates NT dopamine that could be involved in OCD
A mutation of COMT gene produces higher levels of dopamine, thought to have occurred in people with OCD
SERT gene / serotonin transporter re-uptaker gene / 5-HTT
Affects the transport of serotonin and a mutation in gene produces lower levels or serotonin
This is thought to have happened in people with OCD
Twin studies — all research into OCD suggests there is influence (MZ concordance rates being higher than DZ) rather than cause (as MZ concordance rate isn’t 100%)
Samuel et al — gene mapping on people with OCD found a possible link to a mutation on chromosome 14
Neural (biochemical and anatomical) explanation of OCD:
Anatomical abnormalities:
Some forms of OCD linked to breakdowns in immune functioning due to infections such as Lyme’s disease and influenza, indicates that damage to neural mechanisms can result in OCD
High levels of activity found in orbital frontal cortex which is associated with higher level thought process, thought to control impulses so more constant activation with OCD
Biochemical abnormalities — brain scans show low levels of serotonin and high dopamine (linked to a result of genetic mutation or development of diseases)
Studies:
Fallon and Nields — 40% of people contracting Lyme’s disease develop neural damage resulting in psychiatric conditions incl. OCD
Hu — 80% of OCD patients have serotonin levels lower than non-sufferers
Evaluation of OCD explanations:
Neural explanation
Highly scientific — uses PET scans to examine neurotransmitter levels, producing objective data that can be analysed
Suggests that low levels of serotonin and high levels of dopamine are the causes of OCD but drug treatments do not work on all sufferers, which suggests there are other causes
Genetic explanation
Reductionist — solely focuses on natural influences that cause OCD and not nurture influences such as environment, making the explanation oversimplified
Treatment for OCD:
Antidepressants are used to treat OCD.
SSRIs work by:
Blocking the transporter
This inhibits the amount of serotonin that is absorbed back into the presynaptic neuron
This means more serotonin will stay in the synapse and has a chance to bind to receptors.
—> In OCD, this can reduce symptoms like repetitive thinking.
Most commonly prescribed for adults: fluoxetine
Children 6+ are given sertraline or fluvoxamine
12-16 weeks of drug treatment, can be longer if symptoms don’t improve. If SSRIs don’t work, antipsychotics are sometimes used
Koran et al study:
Aim — assess ability of olanzapine (antidepressant) with an SSRI to alleviate treatment-resistant forms of OCD
Procedure — 10 adults with OCD (had for at least a year) on fluoxetine, with 2.5mg olanzapine added for 2 weeks, then 5mg for 3 weeks and then 10mg for 4 weeks
Results: 9 completed the trial (sample attrition), mean number of symptoms decreased by 4.6% but only 1 decreased significantly, 6/9 experienced weight gain side effect
Conclusion: some positive effects, simultaneous drug use can be more effective in cases
Evaluation:
Strengths
Drugs are cheap and easy to administer + control, patients can self administer which is important because they can often be reluctant to seek treatment for a psychiatric disorder
Reasonably high success rate
Weaknesses
Little evidence to suggest drugs act directly on OCD symptoms alone, we are not sure if the drugs are treating OCD symptoms (like obsessions) or just the depressive symptoms like distress and low mood) that go with it so disorder easier to cope with. Apparent usefulness may be invalid as it may just be treatment for depression symptoms
Negative side effects, can be addictive and can lead to cognitive impairments like memory problems and poor concentration
Pros and cons need to be balanced out to make sure treatment is ethical
 Knowt
Knowt