Diabetes - Plaque, Periodontal Disease 3.03
Diabetes
1/50 to 1/100 patients you will see may be diabetic
May present with
Increased caries
Candidal infection
Xerostomia (salivary hypofunction)
Increased frequency of severe, rapidly progressing forms of periodontitis
“diabetes is an acquired risk factor” for chronic periodontal disease

Activity of microbes in the plaque
Conditions prevailing in the plaque environment
Microflora in Health and Disease
Change in habitat
Alter stability of bacterial population
e.g. “unusual” nutrients – sugar, GCF components, defences decreased (e.g. AIDs)
“Opportunistic pathogens”
Potential to cause disease
This is an example of the “Ecological Plaque Hypothesis”
Potential Contributory Factors in Plaque Accumulation in Diabetes
Elevated [glucose] in saliva, blood, GCF
Resting levels 4-5mmol, in diabetics 9+mmol
Impaired neutrophil function
Dry mouth – reduced salivary flow
Low tissue oxygen levels
Increased tissue carbon dioxide levels
AGE – Advanced Glycation End-products e.g. haemoglobin, albumin, etc.
AGE-Receptors of AGE (AGE-RAGE) interactions
Reduced Saliva Flow
Host defences in saliva
Saliva flow (can’t wash things away)
Mucins/agglutinins (can’t bind bacterial for effective removal)
Lysozyme (can’t bust cell walls)
Lactoferrin (can’t bind iron)
Histatins – antimicrobial cationic peptides
Secretory IgA
Complement
Glucose Levels in Saliva
Only slightly elevated in diabetes vs normal
Mirrors plasma [glucose]
Normal 3-6mM
Diabetic 10mM
Predisposes supra-gingival plaque build-up
Increases buccal caries
GCF [glucose]
Environmental Change and Sub-gingival Ecology
Diabetes leads to vascular thickening which leads to reduced blood flow
Lead to poor oxygen perfusion and increased [carbon dioxide]
Increased carbon dioxide is directly proportional to the number of “capnophiles” (carbon dioxide-loving)
Capnocytophaga spp
Known to be proteolytic
Peptidases – render peptides down to amino acids
Can damage the tissues
Helps growth of other pathogens
Phagocyte Function in Diabetes
Hyperglycaemia impacts:
Impaired chemotaxis
Impaired phagocytosis
Impaired bactericidal activity
Are proportionally decreased and correlate with [AGEs]
[AGEs] goes up if hyperglycaemic
Chemotaxis: movement toward or away from a chemical stimulus
Chemo-attractants:
Cytokines (stimulate this)
Bacterially-derived
Peptides (kick it off)
Complement factors
These functions are depressed when you are chronically hyperglycaemic
Accepted Paradigm
Plaque causes periodontal disease
Problem?
Plaque load does not appear to correlate with disease severity
AGEs
AGEs are major pathophysiological features of diabetes
Proteins (& lipids) react with reducing sugars
e.g. albumin, haemoglobin, etc
Non-enzymic glycation
With 1. Glucose
2. Fructose (more so than glucose)
Occurs when there is long-standing hyperglycaemia
Long-lived proteins
Extra-cellular proteins
Glycation can alter molecular shape/function
[AGE-proteins] – a measure of diabetic glucose control
E.g. HbA1c
Formulation of Advanced Glycation End-products
Examples of AGEs: chips, crisps, bread, roast chicken, roasted chestnuts, sausages, etc
Essentially the same reactions involved in browning of chips, crisps, cooked meat, baked bread
Maillard Reaction
General Properties/Effects of AGEs
AGEs form via a chemical/non-enzymic reaction
Sugar + protein = protein-sugar
Glucose and fructose bind to certain amino acids
e.g. valine and lysine (more likely due to long side-chain with an extra amino group) in haemoglobin (and other proteins)
Molecular rearrangements
Factors dictating the formation of AGEs
(Law of Mass Action)
Sugar + protein = AGE-protein
Concentrations of reactants
Temperature
Time
Type of protein/sugar
Properties of AGEs and their Effects
Form slowly
Cross-link with other proteins
Turned over slowly i.e. because they are broken down slowly
Lead to thickening/occlusion in vessels
Can result in chemical radical generation and fragmentation damage to proteins/DNA
Collagen (Tropocollagen)
3 polypeptide chains in helix
Each chain is approx. 1000 amino acids
General sequence repeated
1/3 glycine
Abundant in lysine – approx. 106 per tropocollagen
Has an ε amino side chain
Important target for glycation
Collagen Glycation
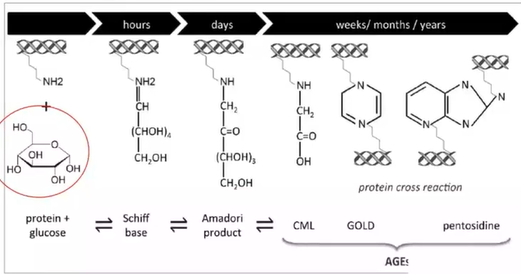
Glucose attaches to lysine and then over a number of hours and days, you get modifications to an end result of an AGE.
Some of these modifications of glucose can cross-react with others in other peptides. So adjacent tropocollagens can get linked by that.
Structural/functional alteration
Increases thermal unfolding of the triple helix
Glycation decreases turnover and repair
Why is collagen important?
Is within dentine
Some Medical Consequences of Protein and Lipid Glycation
Most common cause of blindness
Increased proliferation of blood vessels
Vascular occlusion, angiogenesis
Micro-aneurysms, haemorrhages and retinal infarction
AGEs contribute towards vascular occlusion
Diabetic Nephropathy
[AGE] in kidney tissues
Correlates with severity of nephropathy
AGE promote
Increase release of transforming growth factor-b
Occurs in the glomerular basement membrane collagen (type 4 collagen)
This can be thickened and affect perfusion which can have a knock-on effect on kidney function
Stimulates collagen synthesis
Thickening of glomerular basement membrane
Traps plasma proteins
Consequences?
Reduce filtration
Loss of glomerular function
Kidney failure – death!
Diabetic Neuropathy
Pain or numbness of limbs
(impotence in men)
Axonal degeneration of peripheral neurones
Reduced nerve conduction and blood flow
Increased glycation of myelin
Stimulates macrophages to secrete proteases and phagocytose myelin
AGEs on myeline trap plasma proteins
e.g. IgG, IgM and complement C3 to elicit immunological reactions contributing to demyelination
AGEs and Periodontal Disease
Thickening of vasculature in periodontal tissues
Poor perfusion of tissues
Poor protein turnover and repair of tissues
Elevated glycated haemoglobin
Glycated Haemoglobin (HbA1c)
Glucose can glycate haemoglobin as it has several lysin residues but not all of them are targets due to a number of physiochemical reasons
If you modify haemoglobin, you have this drastic effect on the functioning of haemoglobin
10% Hb glycosylation in diabetic red cells
(3-6% in normal)
Periodontal disease severity
Directly proportional to [HbA1c] in GCF
[HbA1c] in the blood is a measure of the degree of hyperglycaemia
Higher affinity for oxygen
Erythrocytes do not unload oxygen
Reduced tissue oxygenation
Low oxygen levels
Decrease oxygen-mediated neutrophil killing
Encourages anaerobic bacteria
[HbA1c] in GCF is directly proportional to increased P. gingivalis in plaque
A KNOWN PERIODONTOPATHOGEN
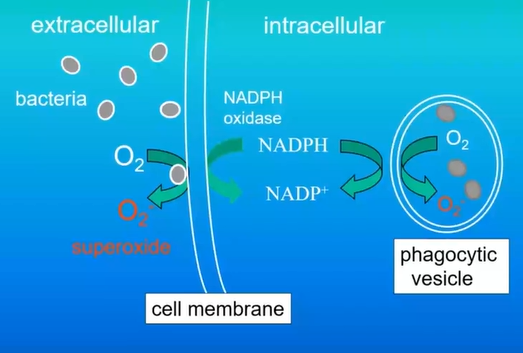
Neutrophil Reactive Oxygen Intermediates
NADPH + 2O2 → H2 + NADP + 2O2- Superoxide
2O2- + 2H+ → O2 + H2O2 Hydrogen peroxide
H2O2 + Cl- → OH- + HOCl Hypochlorous acid
ClO- + H2O2 → Cl- + H2O + 1O2 Singlet oxygen
O2- + H2O2 → OH- + O2 + OH* Hydroxyl radical
Respiratory Burst in Phagocytes
Likely to be depressed
Is a set of processes that are meant to kill organisms
RAGE – Receptors for AGE
AGE proteins are recognised by various cells in the body
Immunoglobulin-related proteins
Cell surface
Mononuclear phagocytes
React with AGEs
AGE-RAGE Interactions
Hyperglycaemia
Proteins get glycated to form AGEs
These bind to the surface of monocytes via RAGE
This activates monocytes to become a bit more aggressive
Activated macrophage:
Reactive oxygen species
Tissue destruction
Release varies pro-inflammatory cytokines such as IL-1β, IL-6, TNF-α
These cytokines increase the inflammatory response
This results in the chemotactic attraction of more neutrophils and white cells.
Host inflammation causes tissue breakdown and remodelling
This can lead to bone resorption and inflammation
If you over-stimulate inflammation, without removing the source, then you get chronic inflammation.
When this happens, you get increased levels of GCF
Increased bacterial growth stimulation and therefore, increased protein-degrading organisms.
More bacteria means more inflammation and the cycle continues
Plaque can also lead to tissue destruction and indirectly through the actions of bacteria-making proteases, destroy tissue.
Bacterial Virulence Factors
Lipopolysaccharide (LPS; endotoxin)
Usually gram-negative, anaerobic and proteolytic
Has long chains of carbohydrates on the surface which are pro-inflammatory
Activated Macrophages
Have toll receptors on them
Innate defence
Transmembrane
Signalling molecules
LPS can interact with toll receptors
This brings a more amplified inflammatory cascade
This then leads to tissue breakdown
Anti-AGE Proteins

There is glucose attached to proteins where rearrangements then occur. These keto groups can react with aminoguanides.
Normally, you get the glucose that modifies the protein and these proteins will crosslink and become difficult to break down.
You can use aminoguanide to stop the AGE-protein cross-linking effect which are in high quantities in garlic, blueberry and pomegranate.
Is there a reverse relationship – i.e. does periodontitis predispose towards diabetes?
Moderate (3.5-5.5mm) and severe (pockets >5.5mm) are significantly associated with an increased risk of diabetes incidence.
Patients with advanced periodontitis at baseline show approx. 5x greater increase in HbA1c 0.106±0.03% vs 0.023±0.02%
What are the Mechanisms?
Periodontitis:
Dysregulated secretion of host inflammatory mediators and tissue breakdown
IL-1β, IL-6, prostaglandin E2, TNF-α,
Receptor Activator of Nuclear Factor KB Ligand (RANKL)
Matrix Metalloproteinases (MMPs)
T-cell regulatory cytokines (e.g. IL-12, IL-18)
(Periodontal lesion area = 8-20cm2)
Diabetes is characterised by:
Elevated serum levels of IL-6, TNF-α → CRP
Predictive of future occurrence of type 2 diabetes
Mechanisms: IL-6, TNF-α, and CRP impair intracellular insulin signalling and contribute to insulin resistance
Reasoning: periodontal inflammation state influences diabetes
Collective evidence: effective periodontitis treatment
→ Improvements in metabolic control
Summary
Increased saliva/GCF [Glucose]
Augments growth supra/sub-gingival bacteria
Hyperglycaemia → Impairs neutrophil function → plaque build-up
AGE proteins → vascular thickening → poor perfusion → CO2
AGE-RAGE interactions
Monocytes → macrophages → tissue damage
 Cytokines → stimulate bacterial growth
Cytokines → stimulate bacterial growth
 Inflammation → increased GCF → plaque → tissue destruction
Inflammation → increased GCF → plaque → tissue destruction
Low tissue O2 levels – promotes anaerobes
Glycated Hb → poor O2 unloading → anaerobiosis
Low saliva flow rate – reduced bacteria clearance/killing
A two-way relationship thought to exist
Periodontitis predisposes to diabetes
Inflammation affects the response of cells to insulin
 Knowt
Knowt