Exam 2 - Chapter 6 & 8
Chapter 6 - Trauma & Stressor Related Disorders
Intro
stressors - external events or situations, e.g. challenging or difficult life circumstances
stress - internal psychological or physiological response to a stressor
exposure to worrisome but less traumatic events can also significantly influence our health and well-being
everyday stress can negatively influence our health → development of both psychological and physical conditions
long-term exposure to adversities can suppress our immune system and subsequently increase the risk of illness
Trauma & Stressor Related Disorders
category includes disorders involving intense reactions to traumatic or stressful events
Adjustment Disorder
occurs when someone has difficulty coping with or adjusting to a specific life stressor—the reactions to the stressor are disproportionate to the severity or intensity of the event or situation
the following is necessary for a diagnosis of AD:
Exposure to an identifiable stressor that results in the onset of significant emotional or behavioral symptoms that occur within 3 months of the event
Emotional distress and behavioral symptoms that are out of proportion to the severity of the stressor (normal bereavement is excluded from the AD diagnosis) and result in significant impairment in social, academic, or work-related functioning, or other life activities
These symptoms last no longer than 6 months after the stressor or consequences of the stressor have ended
common diagnosis among people seeking help from medical or mental health professionals
prevalence in the general population is about 2 percent and is higher in certain groups, such as the unemployed (27.5 percent) and recently bereaved (18 percent)
more common in women and those with disadvantaged life circumstances
most adults recover, adolescents may be at risk for other disorders
can be acute, occurring immediately after a specific onetime stressor, or chronic, involving multiple or repeated stressors
time-limited, often resolves without treatment BUT symptoms can remain 12 months after the traumatic event
often involve mood or behavioral changes, including symptoms of anxiety or depression → not always easy to distinguish
look at emotional functioning prior to stressor
a specific stressor precedes the symptoms seen in AD and that the person experiences an unusually intense reaction to the stressor
concern - category may be pathologizing normal responses to stressors
how to decide if “out of proportion”?
four common outcomes or trajectories after exposure to traumatic incidents:
resilience - relatively stable functioning & few symptoms resulting from the trauma
recovery - initial distress with reduction in symptoms over time
delayed symptoms - few initial symptoms followed by increasing symptoms over time
chronic symptoms - consistently high trauma-related symptoms that begin soon after the event
Acute Stress Disorder
DSM:
Direct or indirect exposure to a traumatic stressor involving actual or threatened death, serious injury, or sexual violence
Nine or more symptoms involving
intrusive memories
avoidance of reminders of event
negative thoughts or emotions
heightened arousal
dissociation or inability to remember details
disturbance persists from 3 days to 1 month after exposure to trauma
prevalence
about 2% in the general population
from 7% to 28% in medical and psychiatric samples, recently bereaved, and unemployed
More common in women and those with disadvantaged life circumstances
most adults recover
adolescents may be at risk for other disorders
Posttraumatic Stress Disorder
DSM
Direct or indirect exposure to a traumatic stressor involving actual or threatened death, serious injury, or sexual violence
One or two symptoms involving each of the following:
intrusive memories
avoidance of reminders of the event
negative thoughts or emotions
heightened arousal and hypervigilance
symptoms are present for at least 1 month
prevalence
Lifetime prevalence for U.S. adults is about 8.7%
12-month prevalence is 3.5%
Varies according to the traumatic stressor and population involved; higher rates for rape, military combat, and emergency responders
Twice as prevalent in women
Female adolescents have higher prevalence (6.6%) compared to males (1.6%)
Low prevalence in Asian Americans
Higher prevalence in Latinx and African Americans
Symptoms may vary cross-culturally
Symptoms fluctuate
Over 50% recover within the first 3 months
For a minority, PTSD is a chronic condition
Diagnosis of Acute & Posttraumatic Stress Disorders
begin with direct or indirect exposure to specific traumatizing stressors (actual/threatened death, serious injury, sexual violence)
initial stress reactions that occur shortly after a traumatic event are normative responses to an overwhelming and threatening stimulus
most individuals recover from traumatic events and demonstrate a marked lessening of symptoms as time passes, but for some…
lasts for more than several days
heightened reactivity
ongoing fear, alarm, distress
Indirect exposure to trauma such as witnessing a traumatic event involving others, learning of a traumatic event involving loved ones, or repeated contact with aversive details of a traumatic event can also result in ASD or PTSD
diagnosis requires symptoms from major symptom clusters:
intrusive symptoms
intrusive thoughts, including distressing recollections, nightmares, or flashbacks of the trauma
psychological distress triggered by external or internal reminds of the trauma
physical symptoms such as increased heart rate or sweating
avoidance
avoidance of thoughts, feelings, or physical reminders associated with the trauma (& places, events, or objects that trigger distressing memories of the experience)
negative alterations in mood or cognition
difficulty remembering details of the event
persistent negative views about oneself or the world
distorted cognitions leading to self-blame or blaming others
frequent negative emotions
limited interest in important activities
feeling emotionally numb, detached, or estranged from others
persistent inability to experience positive emotions
arousal and changes in reactivity
feelings of irritability that may result in verbal or physical aggression
engaging in reckless or self-destructive behaviors
hypervigilance involving constantly remaining alert for danger
heightened physiological reactivity such as exaggerated startle response
difficulty concentrating
sleep disturbance
clinicians also specify if there are recurrent symptoms of:
depersonalization - feeling detached from one’s body or thoughts
derealization - a persistent sense of unreality
dissociation - protective reaction involving mental disconnection from an overwhelming situation, commonly associated with trauma
diagnostic criteria for ASD and PTSD are very similar
ASD requires at least 9 from symptom clusters
involves symptoms that persist for at least 3 days but no longer than 1 month after event
PTSD requires one or two from each cluster
symptoms present for at least 1 month
expression is occasionally delayed
Etiology of Trauma & Stressor-Related Disorders
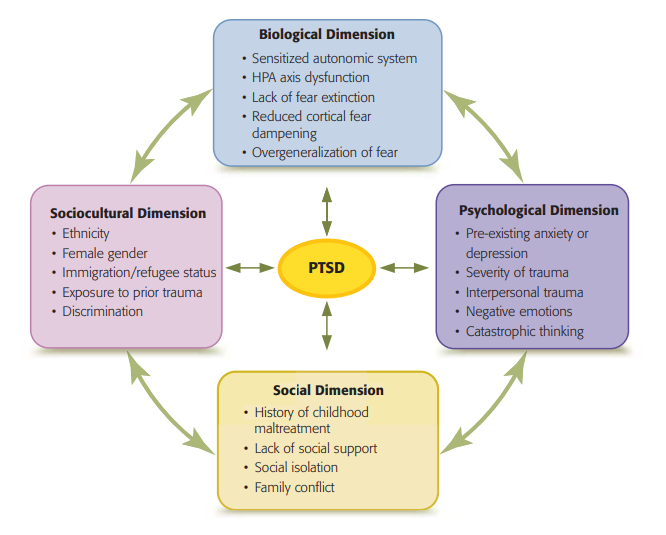
Biological Etiology
normal response to a fear-producing stimulus is quite rapid, occurring in milliseconds, and involves the amygdala
amygdala - part of the brain that is involved with threat detection, major interface between events occurring in the environment and physiological fear responses, multiple connections to regions of prefrontal cortex (attention, managing emotional reactions, and anticipating events)
sends out a signal to the prefrontal cortex and the sympathetic nervous system, preparing the body for action (i.e., to fight or to flee)
HPA - releases hormones, including epinephrine and cortisol
prepare the body for “fight or flight” by raising blood pressure, blood sugar levels, and heart rate
Homeostasis returns once it becomes evident that the danger has passed and the “fight or flight” response is dampened
with PTSD, continue to demonstrate an enhanced startle response and exaggerated physiological sensitivity to stimuli associated with the traumatic event
persist even when the stressor is no longer present
exhibit minimal fear extinction, their trauma-related fear responses do not decline with the passage of time
possible that the chronic release of stress hormones such as cortisol alters brain structures associated with stress regulation
disruptions caused by excess cortisol can lead to neuronal loss and affect brain structure in the hippocampus, amygdala, and cerebral cortex
heightened physiological arousal and cortisol production associated with PTSD have been associated with oxidative stress and inflammation throughout the brain and body
alterations in connectivity within the orbitofrontal cortex may also help explain the vigilance and cognitive rigidity
individuals with PTSD show altered structural and functional connectivity between the amygdala and the ventromedial prefrontal cortex
genetics
Psychological Etiology
Preexisting conditions such as anxiety and depression and negative emotions such as hostility and anger are risk factors
Individuals with higher anxiety or negative emotions may react more intensely to a traumatic event because they ruminate about the event or overestimate the probability that additional aversive events will follow
tendency to generalize trauma-related stimuli to other situations and to avoid circumstances associated with the trauma
individuals with specific cognitive styles or dysfunctional thoughts about themselves or the environment are more likely to develop PTSD
a negative worldview may have difficulty envisioning a positive future → sustain hyperarousal, trauma-related symptoms, negative appraisals
a cognitive style that results in active problem solving, reframing traumatic events in a more positive light, and optimistic thinking can increase resilience and reduce risk of PTSD
recovery from PTSD symptoms is also more prevalent with individuals who possess psychological flexibility, practice mindfulness, and demonstrate self-compassion
Social Etiology
Social support can prevent or diminish PTSD symptoms by affecting brain processes (such as the release of endorphins) that reduce stress and anxiety
may dampen anxiety associated with trauma or prevent negative cognitions from occurring
Preexisting family conflict or overprotective family interactions may also increase the impact of stress following exposure to a traumatic event
increase anxiety
lead to negative cognitive styles
alter stress-related physiological activity & HPA axis functioning
trigger genetic predisposition toward greater physiological reactivity
Sociocultural Dimension
ethnic differences have been found in the prevalence of PTSD
race-based discrimination:
“being called names or insulted,”
“witnessing friends of your ethnic group treated unfairly,”
“being treated as not as smart because of your ethnic group”
differential exposure to previous trauma or cultural differences in responding to stress
women are twice as likely as men to suffer from a trauma-related disorder
physiological differences or because women have greater risk of exposure to stressors
Medication Treatment of Trauma-Related Disorders
certain anti-depressant medications (SSRIs) → moderate effectiveness in some
alter serotonin levels, decrease reactivity of the amygdala, desensitize fear network
effective in less than 60% of people with PTSD, & only 20-30% of those who respond show full recovery
D-cycloserine - a medication that appears to act on the brain to boost fear extinction processes
initially promising, but further findings → mixed findings (some improved, others reported increases in symptom severity)
appears to have a small augmentative effect on improving the outcome of cognitive-behavioral therapy for PTSD
Prazosin - a hypertension medication sometimes prescribed to reduce nightmares associated with PTSD → has not demonstrated substantial effectiveness in reducing distressing dreams or improving sleep quality
Propranolol - a beta-blocker believed to reduce memory consolidation of traumatic memories, has been investigated as a treatment for the intrusive reexperiencing of trauma → appear to produce significant improvement in sleep quality and reductions in symptoms of hyperarousal
MDMA - shows promise when combined with exposure-based therapy; suppressing the emotional memory circuits involved with intrusive memories, thus permitting the use of exposure therapy (without client being overwhelmed by fear)
Psychotherapy for Trauma-Related Disorders
CBT - most effective form of treatment for PTSD
generally focus on extinguishing the fear of trauma-related stimuli and correcting dysfunctional cognitions that perpetuate symptoms
Prolonged exposure therapy (PE), cognitive-behavioral therapy (CBT), trauma-focused cognitive-behavioral therapy (TF-CBT), and eye movement desensitization and reprocessing (EMDR) have all proven to be effective
all are more successful than use of medication and also preferred
Prolonged exposure therapy (PE)
involves imaginary and real-life exposure to trauma-related cues
extended exposure to avoided thoughts, places, or people can help them to realize that those situations do not pose a danger
more commonly, exposure therapy involves asking participants to re-create the traumatic event in their imagination
a preferred treatment modality among military personnel and is used in both individual and group sessions
has also reduced depressive symptoms among veterans
trauma-focused cognitive-behavioral therapy (TF-CBT)
combination of CBT techniques and trauma-sensitive principles, focus on helping clients identify and challenge dysfunctional cognitions about the traumatic event and current beliefs about themselves and others
address underlying dysfunctional thinking or pervasive concerns about safety
may include education about PTSD, developing a solution-oriented focus, reducing negative self-talk, and receiving therapeutic exposure to fear triggers
mindfulness training - paying attention to emotions & thoughts on a nonjudgment basis without reacting to symptoms
eye movement desensitization and reprocessing (EMDR)
nontraditional
decrease physiological reactivity, weaken impact of negative emotions
clients visualize their traumatic experience while engaged in an activity involving both sides of the body, such as visually following a therapist’s fingers moving from side to side
therapist prompts with substitute positive cognitions for negative cognitions associated with experience
Processing the trauma in a relaxed state allows the client to detach from negative emotions and replace them with more adaptive appraisals
many individuals with PTSD report significant reductions in hyperarousal and other trauma-related symptoms
Psychological Factors Affecting Medical Conditions
Stress causes a multitude of physiological, psychological, and social changes that influence health conditions
psychosomatic was the term applied to physical disorders—such as asthma, hypertension, and headaches—made worse by psychological influences
refers to situations where psychological or behavioral factors adversely influence the course or treatment of a medical disorder, constitute an additional risk factor for the medical condition, or make the illness worse
examples - emotional states, patterns of interpersonal interaction, and coping styles
sometimes substitute the term psychophysiological disorder (any physical disorder that has a strong psychological basis or component) instead of “psychological factors affecting other medical conditions.”
Medical Conditions Influenced by Psychological Factors
Broken Heart Syndrome - reversible cardiac condition
occurs when severe stress results in the release of high levels of norepinephrine (i.e., noradrenaline) and a sudden reduction in heart function
symptoms & test results very similar to those of hear attack but with no evidence of blocked heart arteries or other cardiac abnormalities
7.5 times more likely to occur in women, particularly between 65 and 70
can involved actual tissue damage, a disease response, physiological dysfunction
Coronary Heart Disease (CVD)
narrowing of cardiac arteries due to atherosclerosis (hardening of the arterial walls), resulting in complete or partial blockage of the flow of blood and oxygen to the heart
less oxygen-rich blood reaches heart muscle → angina (chest pain) or if blood flow to the heart is completely blocked, a heart attack
leading cause of death in the US, someone dies every 38 seconds
risk factors/affect on prognosis
unhealthy eating habits
hypertension
cigarette smoking
diabetes
cholesterol
obesity
lack of physical activity
depression
perceived stress
difficult life events
stress can also affect heart rhythm - stressor causes the release of hormones that activate the sympathetic nervous system → heart rhythm changes
ventricular fibrillation - rapid, ineffective contractions
bradycardia - slowing of heartbeat
tachycardia - speeding up of heartbeat
arrhythmia - irregular heartbeat
hypertension
blood pressure - measurement of the force of blood against the walls of the arteries
normal blood pressure - systolic pressure (contraction) lower than 120 & diastolic pressure (relaxation after contraction) lower than 80
hypertension = systolic blood pressure equals or exceeds 130 or the diastolic pressure is 80 or higher
elevated blood pressure - borderline level of blood pressure - systolic pressure between 120 & 129, diastolic pressure less than 80
precursor to hypertension, stroke, heart disease
Chronic hypertension leads to arteriosclerosis (hardening of the arteries) and to increased risk of stroke and heart attack
Migraine, Tension, Cluster Headaches
headaches very common
intensity of headaches can vary from dull and annoying to excruciating
debilitating headaches decrease quality of life and impair family, social, and occupational functioning
medication-overuse headache is a common secondary headache disorder that affects up to 5 percent of some population groups
results from rebound headache effects associated with excessive use of headache medication
Migraine
often one side of head but location varies
hours to 4 days
mild to severe
nausea, sensitivity to light, sound, odors, and movement
more common in young adult women (3-4x more common than men)
often hereditary
Up to 1/3 of individuals with migraines experience an aura prior to the headache— unusual physical sensations or visual symptoms such as flashes of light, unusual visual patterns, or blind spots
associated with an increased risk of cardiovascular events such as strokes and heart attack
associated with modifiable risk factors such as high levels of caffeine consumption, overeating, and poor sleep quality
affect about 20 percent of the U.S. population
Tension Headache
both sides of head, often concentrated
hours to days
mild to moderate
tightness or pressure around neck, head, or shoulders
more common in women
probably not hereditary
produced when stress creates prolonged contraction of the scalp and neck muscles, resulting in vascular constriction and steady pain
most common form of headache
70 percent of adolescents and adults experience tension headaches each year
Cluster Headache
centered on one eye on same side of head
usually less than an house
excrutiating
eye often teary, nose clogged on side of head with pain; pacing and rubbing head
more common in men
sometimes hereditary
rapid onset of an excruciating stabbing or burning sensation located in the eye or cheek
often causing tears and redness of the eye, and sometimes resulting in drooping of the eyelid and nasal congestion on the affected side
55 percent of affected individuals in one study reported suicidal thoughts while enduring an episode of cluster headaches
relatively uncommon, affecting about 1 in 1,000 adults
generally develop during adulthood and are six times more prevalent in men
occur in cycles, with incapacitating episodes that may arise several times a day
each attack - 15 min to 3 hrs
may continue over period of a few days to sever months, followed by pain-free periods
Only about 10–20 percent of cluster headaches are chronic, with no periods of respite
about 25 percent of cases, cluster headaches are preceded by migraine-like symptoms such as nausea and sensitivity to light and noise
Asthma
chronic inflammatory disease of the lungs, can be aggravated by stress or anxiety
various environmental influences trigger excessive mucus secretion as well as spasms and swelling of the airways → reduce the amount of air that can be inhaled
range from mild and infrequent wheezing or coughing to severe respiratory distress requiring emergency care
often underestimate magnitude of airflow obstruction, may neglect to self-administer medication/seek treatment
ongoing psychological or economic stressors can interfere with adherence to protocols for the use of preventative medications or rescue inhalers
prevalence of asthma has increased dramatically since the 1980s - affects up to 8.2 percent of the U.S. population, more prevalent among women, those living on poverty, African Americans, Puerto Ricans
youth between the ages of 12 and 17 have the highest prevalence rate, 16.7 percent
Biological Etiology on Physical Disorders
stressors can dysregulate physiological processes occurring throughout the brain and body
stressor activates HPA axis & sympathetic nervous system → hormones released (epinephrine, norepinephrine, cortisol) → prepare body for emergency action (increasing heart rate, respiration, alertness) → when occurring over extended period of time, psychophysiological disorder can develop
while brief exposure to stressors enhances immune functioning, long-lasting stress can impair immune response
results in increased cortisol production, which can have a detrimental effect on physiological processes
suppresses the immune system → white blood cells, responsible for destroying pathogens such as bacteria, viruses, fungi, and tumors, may be less able to multiply and we are therefore less capable of fighting infection
genetic influences contribute to psychophysiological disorders
cardiovascular stress reactivity, as measured by blood pressure, is more similar among identical twins than among fraternal twins
having purer African ancestry increases the risk of developing severe asthma
twin studies have estimated the heritability of asthma to be around 35 percent
early environmental influences (traumatic childhood experiences) interacting with the alleles of certain genes → changes in stress-responsive neurobiological systems → increased vulnerability to the development of a psychophysiological disorder through epigenetic mechanisms
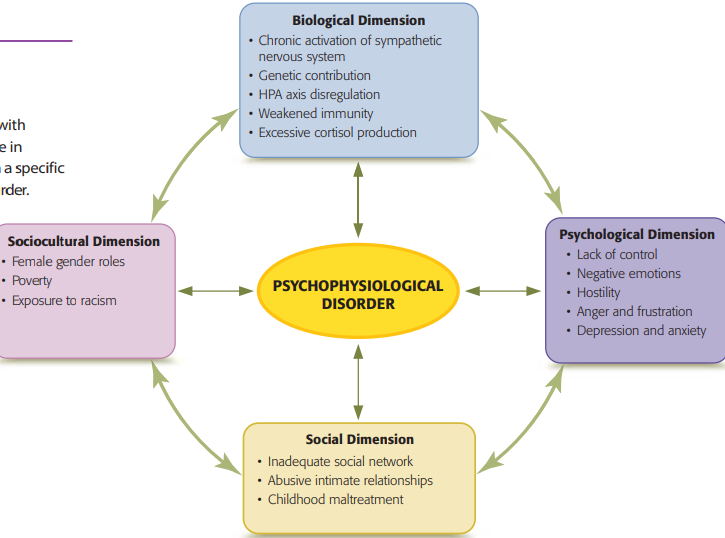
Psychological Etiology on Physical Disorders
Positive emotions, such as optimism, happiness, joy, and contentment, can help regulate heart rate, blood pressure, and other physiological stress reactions, whereas negative emotions accentuate the stress response
High levels of well-being and life satisfaction are associated with increased likelihood of disease-free living and six more years of life compared to low levels of well-being
Control and the perception of control over the environment and its stressors can mitigate the negative effects of stress
negative emotional states such as depression, hostility, anxiety, and cynicism increase the risk for psychophysiological disorders
depression and anxiety can influence both physiological functioning and behaviors that affect health
exhibit irregularities in the autonomic nervous system → exaggerated cardiovascular responses to stressors
depression may result in behaviors - excessive sleep, reduced exercise, consumption of unhealthy food, increased use of alcohol or cigarettes
Hostility is associated with several psychophysiological disorders, particularly CVD
negative emotions such as hostility can increase cardiovascular reactivity, subsequently increasing the risk of developing CVD
anger produces pathophysiological reactions such as coronary vascular constriction and the formation of plaques
Social Etiology on Physical Disorders
social stressors can influence immunological functioning and produce undesired health outcomes
acute and chronic stress associated with the physical or emotional abuse that occurs in intimate partner relationship violence can produce a wide range of health conditions
adversities such as physical, emotional, or sexual abuse in pregnant women increase the likelihood of headaches and hypertension
asthma symptoms increase in response to social stress
lack of social support can lead to immune system dysregulation with less natural killer cell activity and elevated inflammation
good relationships may moderate the link between hostility and poor health
social isolation is more likely to negatively affect the health of women
Sociocultural Etiology on Physical Disorders
factors associated with gender, race, or ethnicity can have a major impact on health
women:
have an increased likelihood of exposure to stressors associated with their role as caregivers for children, partners, and parents
more likely to live in poverty and experience the sociocultural stressors and chronic disparities associated with having limited economic resources
more likely to report physical or emotional reactions to stress, not getting enough sleep, and using food as a way of dealing with stress
married - have a greater frequency of suffering from headaches or experiencing emotions such as fatigue, irritability, anger, or feeling as if they are on the verge of tears
stressful experiences associated with race and ethnicity affect the health of people who are socially oppressed
exposure to discrimination has been found to heighten stress responses and elevate blood pressure and heart rate among African Americans—conditions that increase risk for chronic hypertension and CVD
higher risk of sudden cardiac deaths compared to European Americans
incidence of sudden cardiac arrest
come from severely disadvantaged backgrounds, but who excel in school, succeed at work, and achieve upward mobility experience an unusual degree of adverse health consequences was up to 80 percent greater in low socioeconomic neighborhoods compared to the neighborhoods with the highest income level
Treatment of Psychophysiological Disorders
Relaxation Treatment
therapeutic technique in which a person acquires the ability to relax the muscles of the body under almost any circumstance
tightening and relaxing cycle
the contrast between the feelings produced during tensing and those produced during relaxing
effective in reducing physiological arousal and mitigating the physiological impact of stressors
experience decreases in stress hormones and autonomic reactivity, and report less pain, less anxiety, improved sleep, and a higher quality of life
Biofeedback Training
self-regulation technique that allows people to alter physiological processes in order to improve physical or mental health
therapist teaches you to voluntarily control a physiological function, such as heart rate or blood pressure
continue the improvement in physiological responses outside of the training setting
visual and auditory feedback reinforces relaxation responses
help people lower their heart rates and decrease their blood pressure during stressful situations, treat migraine and tension headaches, and reduce stress-induced airway constriction
Cognitive-Behavioral Therapy
designed to enhance coping skills and stress management can improve physiological functioning and psychological distress in individuals with chronic illness
proven effective in controlling asthma symptoms, reducing anxiety levels, and enhancing the quality of life for those living with illness
Mindfulness strategies have proven effective in improving emotional regulation and reducing symptoms of stress
nonjudgmental awareness of sensations and feelings
producing significant decreases in stress, anxiety, depression, and physiological markers associated with stress
acceptance and commitment therapy
helping clients accept life difficulties and commit to behaviors that are consistent with their personal values
Chapter 8 - Depressive & Bipolar Disorders (pg 280-316)
mood - refers to our emotional state or our prevailing frame of mind
mood can significantly affect our perceptions of the world, sense of well-being, and interactions with others
Symptoms Associated with Depressive and Bipolar Disorders
the mood symptoms in depressive and bipolar disorders:
affect the person’s well-being and school, work, or social functioning
continue for days, weeks, or months
often occur for no apparent reason
involve extreme reactions that cannot be easily explained by what is happening in the person’s life
depressive disorders involve only one troubling mood (depression), those with bipolar disorders (previously called manic-depression) often cope with two mood extremes—overwhelming depression and periods involving an elevated or abnormally energized mood
Bipolar refers to the fact that the condition involves mood extremes at both emotional “poles'“
Depression
sadness, emptiness & worthlessness, apathy, hopelessness
pessimism, guilt, difficulty concentrating, negative thinking, suicidal thoughts
social withdrawal, crying, low energy, lowered productivity, agitation, poor hygiene
appetite and weight changes, sleep disturbance, aches and pain, loss of sex drive
Hypomania/Mania
elevated mood, extreme confidence, grandiosity, irritability, hostility
disorientation, racing thoughts, decreased focus, and attention, creativity, poor judgment
overactivity, rapid or incoherent speech, impulsivity, risk-taking behaviors
high levels of arousal, decreased sleep, increased sex drive
Depression
involves intense sadness or loss of interest in normally enjoyed activities
emotional symptoms
sadness, emptiness, hopelessness, worthlessness, or low self-esteem
little enthusiasm for things they once enjoyed, including spending time with family and friends
feeling irritable or anxious and worried is also common
cognitive symptoms
pessimistic, self-critical beliefs
rumination - continually thinking about upsetting topics or repeatedly reviewing distressing events
intensify feelings of depression, especially when it involves self-criticism, feelings of guilt, irrational beliefs
distractibility
interfere with ability to concentrate, remember things, or make decisions
thoughts of suicide
may be from feelings of being a burden to friends and family or belief that there is little hope for the future
belief that emotional pain will never end can lead to thoughts of suicide
behavioral symptoms
fatigue, social withdrawal, and reduced motivation are common with depression
some speak slowly or quietly, may respond only in short phrases or not respond at all
some appear agitated and restless, pacing, finding it difficult to sit still
may cry for no particular reason or in reaction to sadness, frustration, or anger
may appear to no longer care about their grooming or personal cleanliness - occurs because daily activities such as getting out of bed, bathing, dressing, or preparing for work or class may feel overwhelming
physiological symptoms
appetite and weight changes
increased or decreased eating
sleep disturbance
difficulty falling asleep or staying asleep
sleep much more than usual, but wake up feeling tired and unrefreshed
unexplained aches and pain
headaches, stomachaches, other body aches
aversion to sexual activity
reduced sexual interest and arousal
Hypomania or Mania
elevated mood
hypomania - characterized by increased levels of activity or energy combined with a self-important, expansive mood or an irritable, agitated mood
distractible, change topics frequently, have many ideas, talk excessively, dominate conversations
may feel creative and start various projects
mania - even more pronounced mood change involving extremely exaggerated activity levels and emotionality that significantly impair normal functioning
range from extreme giddiness, excitement, euphoria (exceptionally elevated mood) to intense irritability, hostility, agitation
marked impairment in social or occupational functioning
may involve psychosis (loss of contact with reality) and need for psychiatric hospitalization
manic episode - obvious to others, hypomania - more subtle
emotional symptoms of hypomania/mania
unusually high spirits, full of energy & enthusiasm
uncharacteristically irritable, low tolerance for frustration, overreact with anger or hostility in response to environmental stimuli or people around them
emotional lability - unstable and rapidly changing emotions and mood
inappropriate use of humor, poor judgment in expressing feelings or opinions
grandiosity - inflated self-esteem and beliefs of being special, chosen, or superior to others
cognitive symptoms of hypomania/mania
energized, goal-oriented behavior
seem excited and talk more than usual, engage in one-sided conversations, demonstrate little concern about giving others opportunity to speak
difficulty focusing their attention, show a flight of ideas/racing thoughts, distractibility, poor judgement
fail to recognize the inappropriateness of their behavior
mania - more likely to appear disoriented and exhibit cognitive difficulties
pressured speech - rapid, loud, difficult to understand
flight of ideas - change topics, become distracted with new thoughts, make irrelevant or illogical comments
behavioral symptoms
appear energetic, productive, display mood of extreme confidence and self-importance, taking on complex or creative tasks
might also become easily agitated and react angrily with little provocation
seem uninhibited and act impulsively
engage in uncharacteristic behaviors like reckless driving, excessive drinking, illegal drug use, promiscuous behavior, uncontrolled spending, making impulsive decisions such as changing jobs or developing plans to move to a new location
difficulty with delayed gratification
motor movement rapid, incoherent speech
wild excitement, ranting, constant movement, agitation
psychotic symptoms - paranoia, hallucinations, delusions (false beliefs)
Physiological Symptoms of Hypomania/Mania
high levels of physiological arousal
intense activity, extreme recklessness, need to be constantly on the go
increased libido (sex drive) - reckless sexual activity or other impulsive behaviors
decreased need for sleep - a person may go for days without sleep
Evaluating Mood Symptoms
careful assessment because…
brief depressive or hypomanic symptoms also occur in people who don’t have a mood disorder
depression occurs in both depressive and bipolar disorders
symptoms may vary considerable from person to person
people often fail to report hypomanic symptoms to their medical or mental health providers because energetic episodes often do not cause significant problems or impair functioning
people experiencing a depressive or hypomanic/manic episode sometimes exhibit symptoms from the opposite pole
When extreme mood changes the clinician specifies that the mood episode has mixed features
take note of: frequency, duration, seasonal changes, are they mild/moderate/severe symptoms, medical conditions, drug use
Depressive Disorders
Major Depressive Disorder
diagnosis occurs when a person experiences impaired functioning due to a major depressive episode - severe depressive symptoms that have negatively affected functioning most of the day, nearly every day, for at least 2 full weeks
DSM-5 → major depressive episode involves
depressed mood, feelings of sadness or emptiness and/or…
loss of interest or pleasure in previously enjoyed activities
four additional changes in functioning
significant alteration in weight or appetite
atypical sleep patterns
restlessness or sluggishness, low energy, feelings of guilt or worthless ness, difficulty concentrating making decisions
preoccupation with death or suicide
anxious distress
feel unusally tense or restless or experience pervasive worries that make it difficult to concentrate
worry about losing self-control or something bad will happen
suicide
people who feel hopeless may act on suicidal thoughts
up to 45% of those with MDD also have a substance use disorder - further increases suicide risk
MDD with a seasonal pattern
some begin to develop depression when daylight decreases as the seasons change
depressive symptoms begin in the fall or winter and remit during the spring or summer
small number of people have the opposite pattern
vegetative depressive symptoms
low energy, social withdrawal, increased need for sleep, carbohydrate craving
winter depressive episodes occur most frequently
among younger individuals
in regions with less light in the winter months (northern latitudes)
among those whoa re sensitive to the influence of environmental light on their circadian rhythm
many clinicians use seasonal affective disorder (SAD) for this seasonal pattern
affect up to 3% of world’s population
more prevalent in women than men
not an official DSM-5 diagnostic category
MDD with a seasonal pattern instead - at least two seasonal episodes of severe depression ending at a predictable time of year combined with a pattern of depressive episodes that occur seasonally more than nonseasonally
Persistent Depressive Disorder
chronic depressive symptoms that are present most of the day for more days than not during a 2 year period (w no more than 2 months symptom-free)
ongoing presence of at least 2 of the following symptoms
feelings of hopelessness
low self-esteem
poor appetite or overeating
low energy or fatigue
difficulty concentrating or making decisions
sleeping too little or too much
negative thinking patterns, pessimistic outlook on future
for many - lifelong, pervasive → long periods of depression, few periods without symptoms, poor response to treatment
Premenstrual Dysphoric Disorder
controversial
serious symptoms of depression, irratibility, tension that appear the week before menstruation and disappear soon after menstruation beings
between 3 and 8% of women meet the criteria for PMDD
presence of five premenstrual symptoms
at least one - significantly depressed mood, mood swings, anger, anxiety, tenssion, irritability, or increased interpersonal conflict
others - difficulty concentrating, social withdrawal, lack of energy, food cravings or overeating, insomnia or excessive sleepiness, feeling overwhelmed
physical symptoms - bloating, weight gain, breast tenderness
similar to premenstrual syndrome but produces much greater distress and interferes with social, interpersonal, academic, or occupational function
Depressive Reactions to Grief
important to distinguish normal grief-related reactions from the severe depression and impaired functioning associated with MDD
Grief often involves feelings of emptiness associated with the loss rather than the more persistent depressed mood or inability to experience pleasure that occurs with MDD
persistent complex bereavement disorder
apply to individuals who have intense and persistent preoccupation or debilitating sorrow that continues for over a year after the death of a loved one
experience continued longing for the deceased, preoccupation with the way the person died, distress or anger over the death, or difficulty accepting the death
diagnosis would require that the death have a significant effect on the person’s interpersonal relationships or sense of identity
Prevalence of Depressive Disorders-
one of the most common psychiatric disorders and the second leading disability worldwide
264 million people each year
21% of US population will experience a mejor depressive episode at some point in their lives
women have nearly twice the risk
2-5% of women experience PMDD
symptoms also subject to external stressors
for many, chronic disorder and chances of relapse
Childhood maltreatment, rumination, and residual depressive symptoms after treatment increase the risk of recurrent depressive episodes
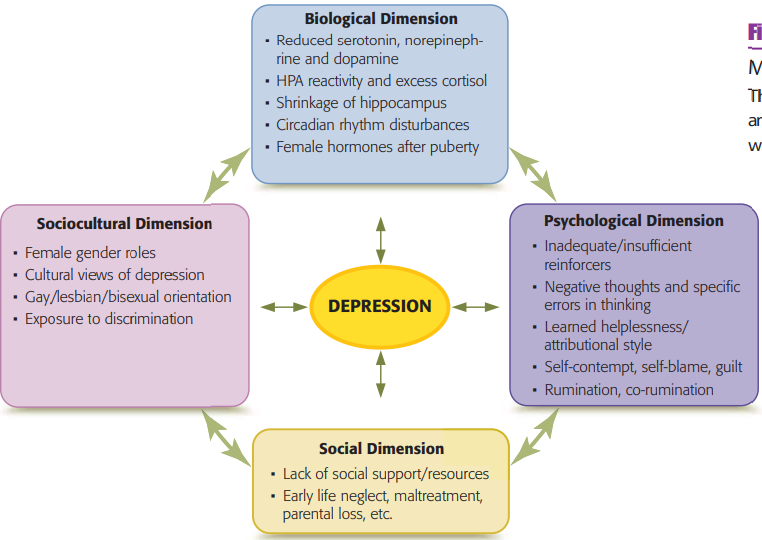
Biological Etiology of Depressive Disorders
neurotransmitters and depressive disorders
low levels of certain neurotransmitters (serotonin, norepinephrine, and dopamine) are associated with depression
neurotransmitters regulate our emotions and basic physiological processes involving appetite, sleep, energy, and libido; however, biochemical irregularities can produce the physiological symptoms
accidentally discovered that when the drug reserpine was used to treat hypertension, many patients became depressed (reserpine depletes certain neurotransmitters)
the drug isoniazid, given to patients with tuberculosis, induced biochemical changes that resulted in mood elevation
therapies involving electrical stimulation of brain regions that have high concentrations of brain cells that release dopamine have implicated dopamine deficiencies in depression
treatment-resistant depression - does not respond to antidepressant medications
the role of heredity
depression tends to run in families
genetics estimated to contribute about half of the variance
incidence is significantly higher among biological relatives compared to adoptive family members, although the child-rearing environment exerts an equal influence on the development of major depression in children
the chances of inheriting depression are greatest for female twins, suggesting gender differences
genetic influence on depression becomes most evident after puberty
cortisol, stress, depression
dysregulation and overactivity of the hypothalamic-pituitary-adrenal (HPA) axis and overproduction of the stress-related hormone, cortisol, appear to play an important role in the development of depression
exposure to stress during early development and the resultant increases in cortisol production can increase susceptibility to depression in later life
genetic predisposition, stress, and the timing of stress can interact to increase cortisol production and produce depressive symptoms
chronic stress and associated high levels of cortisol can damage the hippocampus & interfere with systems involved in our stress response
overactive stress response system and excessive cortisol production → depleting certain neurotransmitters (serotonin), affect production of enzymes
functional & anatomical brain changes with depression
decreased brain activity and other brain changes in people with depression
brain alterations have been found in the medial prefrontal cortex, anterior cingulate cortex, and hippocampus → areas associated with negative thoughts and memories, rumination, impairment in executive functioning
ongoing depression is associated with reduced neuroplasticity
decreased neurogenesis in the hippocampus and in synapses around cortex
individuals experiencing depression have increased connectivity in the default mode network, regions that are associated with a wakeful resting state
individuals with depression show different patterns of neural reactivity compared to controls - the pattern of neural activation depends on whether the emotional stimuli are positive or are negative
circadian rhythm disturbances in depression
internal biological rhythms, maintained by the hormone melatonin, that influence a number of our bodily processes, including body temperature and sleeping patterns
insomnia (difficulty falling or staying asleep) increases the risk of developing depression and is related to the severity of depressive symptoms
a study involving twin pairs, excessively short or long sleep duration appeared to activate genes related to depression
Disrupted sleep is also linked to the onset of postpartum depression
people with depression have irregularities in rapid eye movement (REM) sleep, the stage of sleep during which dreaming occurs
Psychological Etiology of Depressive Disorders
behavioral explanations
depression occurs when people receive insufficient social reinforcement - unemployment, divorce, death of a friend or family member
behaviorists believe that those affected by depression can reduce their depressive symptoms if they become more physically and socially active
risk of depression is increased when:
a person has limited opportunities to engage in activities that are potentially reinforcing
there are few reinforcements available in the person’s environment
a person’s behavior reduced the likelihood of positive social interactions
stressful circumstances - disrupt predictable patterns of social reinforcement and initiating a cycle that further reduces social opportunities and increases vulnerability to depression
positive attributes can also increase the risk of depression - people who are prosocial are more likely to develop symptoms than those who are individualist
increased stress & activation of amygdala in situations associated with unfairness and inequality
cognitive explanations
disturbance in thinking rather than a disturbance in mood
our internal responses to what is happening around us and the way we interpret our experiences affects our emotions
pessimism
damaging self-views
feelings of helplessness
Aaron Beck - individuals experiencing depression have a negative self-schema or way of looking at self
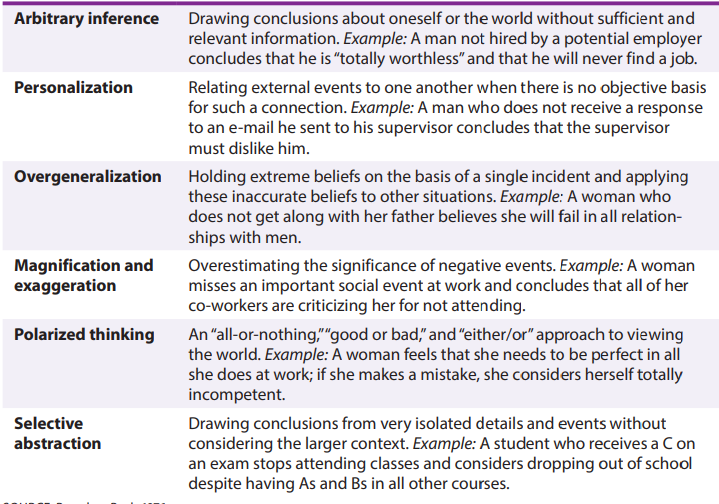
rumination - continually thinking about an upsetting situation keeps the distressing emotions “alive” rather than allowing them to diminish
co-rumination - process of constantly talking over problems or negative events with others, also increases risk for depressions
learned helplessness and attributional style
attributional style - how we explain events that occur in our lives; can have powerful effects on our mood
pessimistic attributional style - focus on causes that are internal, stable, and global
those with a positive attributional style focus on explanations that are external, unstable, and specific
learned helplessness - a belief that we have little influence over what happens to us
factors associated with negative thinking patterns
patterns of pessimistic thinking often interact with biological and social factors
maltreatment occurring during childhood is associated with increased risk of depression - emotional abuse, neglect
self-criticism is strongly associated with depression
Social Etiology of Depressive Disorders
maltreatment during early childhood is strongly associated with later depression
ACEs - appear to modify the expression of genes associated with the HPA axis, increase reactivity to stress and affect the function and structure of cortical and subcortical areas of the brain
parental depression
individuals who fail to develop secure attachments and trusting relationships with caregivers early in life have increased vulnerability to depression
stressful events later in life can also increase the risk of depression
acute stress is much more likely to cause a first depressive episode than is chronic stress but once someone has experienced a serious depression, less severe stressors can subsequently trigger additional depressive episodes
stress generation or engaging in behaviors that lead to stressful events plays an important role in depression
distressing social interactions increase likelihood of depression - especially those who have genetic vulnerability, prior life stressors, or previous depressive episodes
Sociocultural Etiology of Depressive Disorders
culture, race and ethnicity, sexual orientation, and gender
people who are struggling financially have high rates of depression
lack of security and self-sufficiency associated with poverty often find it difficult, or even impossible, to access the education, employment, or housing that would allow them to envision a more hopeful future
racial & ethnic influences on depression
influence a variety of factors associated with depression: descriptions of depressive symptoms, decisions about treatment, client–therapist interactions, and the likelihood of outcomes such as suicide
perceived discrimination based on race or ethnicity is strongly associated
influences of sexual and gender orientation of depression
prejudice & discrimination related to LGBTQ orientation
lack of family acceptance, bullying, and societal rejection exert a significant effect on risk of depression
how and when to disclose their sexual or transgender orientation to family and friends
negative reactions that sometimes occur during the disclosure process can further increase risk of depression
gender and depressive disorders
nearly twice as common among women than among men
higher prevalence of depression in women is due to sociological variables such as poverty, violence, restrictive gender roles, and discrimination or if women are simply more likely to seek treatment or to discuss depression
traditional symptoms of depression (such as sadness and hopelessness) are more likely to be displayed by women, whereas men who are depressed are more likely to display symptoms such as anger, aggression, burying themselves in their work, or substance abuse
Gender differences in depression begin appearing during adolescence and are greatest during the reproductive years
Life stressors may interact with physiological factors to influence the development of depression - alterations in connectivity in the fear circuitry of the brain, reduced connectivity between amygdala and hippocampus
social modeling and socialization practices can influence feelings of self-worth
Biomedical Treatment for Depression
medication
antidepressants - increase availability of certain neurotransmitters
tricyclics
monoamine oxidase inhibitors (MAOIs)
serotonin-norepinephrine reuptake inhibitors (SNRIs)
selective serotonin reuptake inhibitors (SSRIs)
atypical antidepressants - affect other neurotransmitters like dopamine
medical providers consider multiple factors:
the presence of other symptoms (such as anxiety, overeating, or nicotine addiction) that might also be helped by certain antidepressants
the person’s prior response to antidepressants (or family patterns of response)
desire to avoid certain side effects such as weight gain, sexual side effects, or gastrointestinal problems
estimated 1/3 - ½ of those taking antidepressants discontinue their use of the medication due to side effects often without informing prescriber
associated with withdrawal symptoms - dizziness, drowsiness, impaired balance, headache, insomnia, confusion, irritability
adjunctive treatments - adding something different to initial treatments
commonly used to supplement antidepressant use
Omega-3 fatty acid supplements have been found to reduce depressive symptoms and are often used in combination with antidepressant medications
Intravenous administration of the anesthetic ketamine has shown some promising results for treatment-resistant depression
nontraditional treatments for depression
efforts to reset the circadian clock
a night of total sleep deprivation followed by a night of sleep recovery has improved depressive symptoms in some individuals with MDD
use of specially designed lights is an effective and well-tolerated treatment for those with a seasonal pattern of depression
probiotics
brain stimulation therapies
electroconvulsive therapy - involves applying moderate electrical voltage to a person’s brain to produce a very brief seizure
typically treated several times weekly under anesthesia
vagus nerve stimulation - implanting a pacemaker-like device in the chest that then delivers a frequent electronic impulse that travels from the vagus nerve to the brain
transcranial magnetic stimulation - noninvasive treatment, which uses magnetic pulses to stimulate specific areas of the brain
5 days per week over a period of 4 to 6 weeks
Psychological & Behavioral Treatments for Depressive Disorders
behavioral activation therapy
helping those who are depressed to increase their participation in enjoyable activities and social interactions → improvements in mood
individuals with depression often lack the motivation to participate in social activities
based on the idea that depression results from diminished reinforcement
treatment focuses on increasing exposure to pleasurable events and activities, improving social skills, and facilitating social interactions
identifying and rating different activities in terms of the pleasure or the feelings of self-confidence they might produce
performing some of the selected activities, thereby increasing feelings of pleasure or mastery
identifying day-to-day problems and developing strategies to deal with them
improving social and assertiveness skills
interpersonal psychotherapy
focused on current interpersonal problems
approach presumes that depression occurs within an interpersonal context, therapy focuses on relationship issues
Clients learn to evaluate their role in interpersonal conflict and make positive changes in their relationships
improving communication
identifying role conflicts
increasing social skills
cognitive-behavioral therapy
altering the negative thought patterns and distorted thinking associated with depression
teach clients to identify thoughts that precede upsetting emotions, distance themselves from these thoughts, and examine the accuracy of their beliefs
less likely to relapse after treatment has stopped compared to individuals taking antidepressants
Cognitive bias modification—a guided self-help intervention aimed at minimizing rumination and overgeneralization and enhancing specific problem-solving skills
mindfulness-based cognitive therapy
calm awareness of one’s present experience, thoughts, and feelings, and promotes an attitude of acceptance rather than judgment, evaluation, or rumination
allows those affected by depression to disrupt the cycle of negative thinking by directing attention to the present moment
prevents the development of maladaptive beliefs and thus reduces depressive thinking
Bipolar Disorders - Page 307