PBS 3.2 Emergency Response Review
3.2.1 Survey and Assess:
Members of an Emergency Response Team - In-Field
Paramedic: They carry out the duty of a physician and can examine, evaluate, and treat patients with equipment and medications and are
also utilized as emergency care practitioners on ambulances or first response emergency vehicles.
Emergency Medicine Technician: Conducts assessments for medical, trauma, CPR, airway devices, or basic life-saving
First to arrive on the scene
Disaster Response Technician: Helps clear and clean the scene of toxins or debris
Cleans up toxic chemicals, lifts heavy objects, and is usually at the sites of oil spills or trucking accidents
Emergency Medicine Physician: ER Doctor who specializes in emergent care
assists patients, takes care of medical planning/history, and requests testing and or diagnostics
Many don’t work in the field
Members of an Emergency Response Team - In-Facility
Emergency Services Coordinator: In charge of assisting and leading the response before or after emergencies
Provides technical expertise
Triage Nurse: Sorts patients based on emergent cases
They also release, transport, and give treatment to patients
Emergency Medicine Nurse-Practitioner: Evaluate, treat, and diagnose patients without supervision from a physician
Provides critical care and psychological support
Many work in the field
Emergency Communications Specialist: Operates and receives/relays calls on emergencies
Operatees on public safety law and consoles for a regional 911 communication center
Assessing the Scene
Control the situation
Stay calm and act quickly to ensure everyone’s safety.
Look for potential hazards
Assess whether there is anything that could harm your team, the patient, or a bystander (a person who is present but uninjured).
Assess the situation
Quickly gather any available information about the situation using your own senses and also asking questions of the patient or any bystanders.
Protect and prioritize
Use personal protective equipment to protect yourself, keep bystanders out of harm’s way, and prioritize individuals who appear to be in the most need of help.
Listen for unusual sounds and use your sense of smell to detect any unusual odors.
Assessing your Patient
Steps of Primary Assessment
Form a general impression of the patient
What appears to have happened? How serious is the patient’s condition?
Determine the Mechanism of Injury (MOI)
What caused the trauma, or physical damage, to the patient’s body?
Determine the patient’s responsiveness
Is the patient alert, able to speak, in too much pain to respond, or unconscious?
Consider stabilizing the patient’s spine
Is a spinal injury suspected based on their position and MOI? If so, the patient’s back and neck must be held in place to prevent further injury.
Check the patient’s ABCs (Airway, Breathing, and Circulation)
A - Airway
Is the patient’s airway partially or completely blocked? Can you feel air moving from their mouth or nose? Is their breathing noisy or high-pitched?
B - Breathing
Is the patient breathing properly? What is their respiration rate? Are their breaths sporadic?
C - Circulation
Does the patient have an adequate pulse? Is there any bleeding?
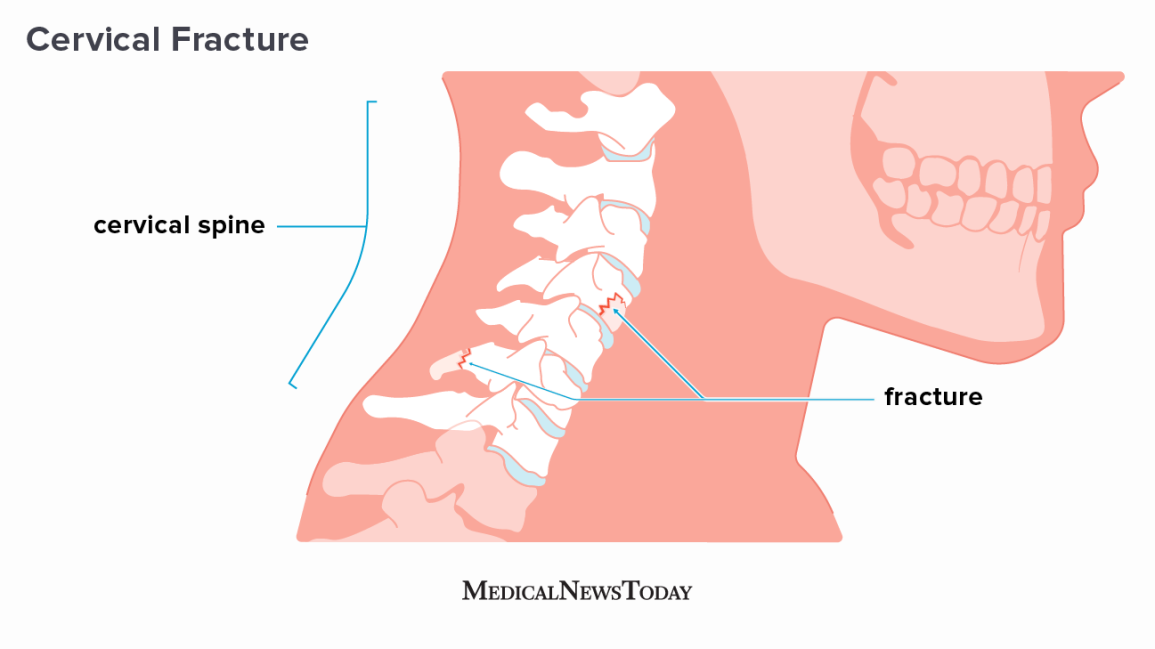
In a trauma case where injury to the back, head, or neck has occurred, the spine must be immobilized with a spinal board or other device. Failure to immobilize an injured spine could lead to permanent paralysis or death.

Cervical Fracture: A cervical fracture is a traumatic injury that results from excessive force on the spine of the neck, they can put increased pressure on the spinal cord at the level of the fracture and can cause a spinal cord injury resulting in loss of sensation, paralysis, or even instant death
To assess the airway for a patient who has not suffered a spinal, neck, or head injury, you can use the following head-tilt/chin-lift maneuver:
Kneel beside the patient’s head and neck.
Place one hand on the patient’s forehead.
Place the fingertips of your other hand under the bony part of the patient’s lower jaw near the chin.
Use firm backward pressure from the palm of your hand to tilt the head back while lifting the jaw up with the fingertips to extend the chin forward.
Keep pressure on the patient’s forehead to help maintain the airway in an open position.
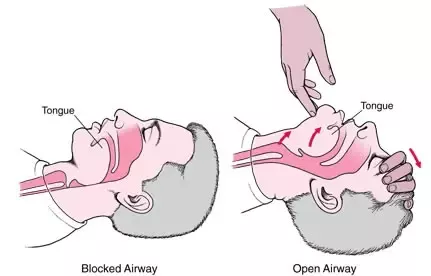
Note: If the patient is a child, tilt the head so the airway is only slightly past neutral. For an infant, tilt the head so the airway is in a neutral position.
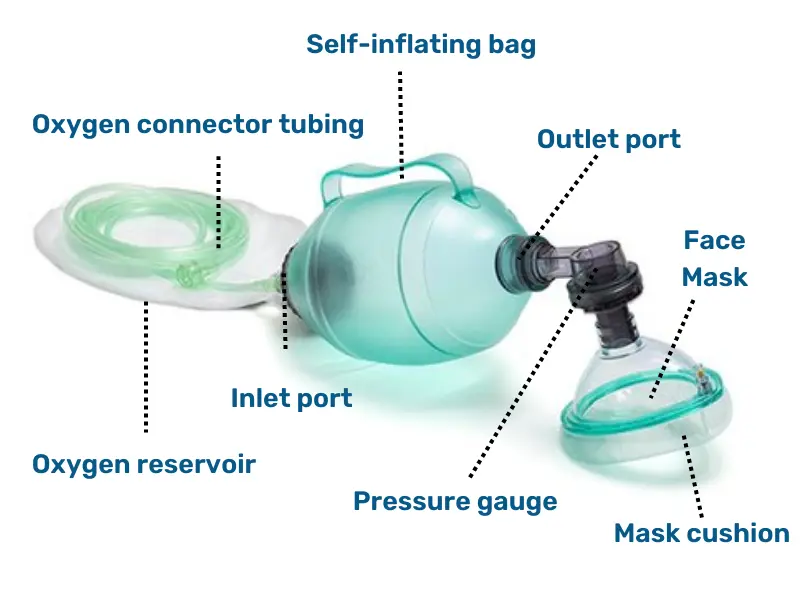
Stridor, or noisy, wheezing breaths are due to a constricted airway. A bag-valve-mask resuscitator is a mask with a handheld pump that is used for manual ventilation, or the providing of air, of a patient suffering a respiratory emergency.
Note: In the field, an emergency responder would typically assess a patient’s airway and pulse at the same time.
Steps of Secondary Assessment
Perform a rapid physical assessment
Check the patient head to toe for injuries or signs of illness, including the head, neck, chest, abdomen, and extremities.
Take the patient’s vitals
Using medical devices to obtain more accurate readings, record the patient’s pulse, blood pressure, and respiration rate.
Get a patient history
If the patient is not responsive, get a history from any family members or bystanders if possible.
Provide appropriate emergency care
Ensure adequate airflow, provide oxygen if necessary, stop bleeding, and provide any medicines deemed appropriate.
Pupillary response is the involuntary changing of size of the pupil and can serve as a useful tool to determine the health of the patient’s nervous system, whether they’ve suffered any nerve or brain damage, or are under the influence of certain drugs
Constriction, or narrowing, of the pupil, followed by the dilation, or widening, of the pupil
A response in the opposite eye from the one in which they’re shining a light is called a consensual pupillary reflex
Neurological problems may be present if the pupil stays dilated when exposed to light, stays constricted even in the dark, or if the consensual reflex is not observed
Endotracheal tube are sometimes put down a patient’s trachea so air can then be delivered to the patient through the endotracheal tube
3.2.2 Drug Delivery
Live-Saving Medication
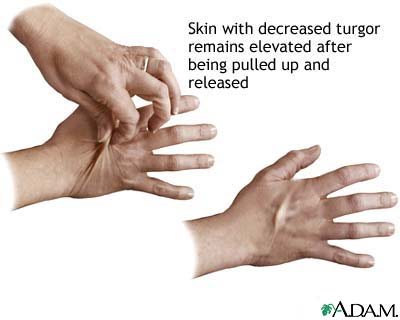
Skin turgor is a measure of the elasticity of the skin and is used as an indicator of dehydration. To test skin turgor, you gently pinch, pull up, and release the skin on the back of the hand. Skin that remains raised after being pulled up and released
Anaphylaxis: Severe allergic reaction
Antigen: Anything that stimulates an immune response
Antibody: A protein produced by B cells in the blood; that works to impair pathogens. Also called an immunoglobulin
When an individual encounters a substance they are allergic to, the immune system recognizes it as an antigen and goes into attack mode, producing antibodies
The result can be mild symptoms, such as itchy, watery eyes or runny nose, or it can be severe, as in the case of your patient who is in anaphylaxis
An allergic reaction is a condition in which the body's immune system overreacts to a foreign substance
Common triggers of an allergic reaction include nuts or fruits, certain medications, latex, metal or fabric dye, and insect stings. In patients with a stinging insect allergy, the venom from the sting elicits a broad, systemic allergic reaction
Anaphylaxis is a severe systemic allergic reaction affecting multiple organ systems, often including the respiratory system and integumentary system (skin)
Patients undergoing a systemic allergic reaction may experience swelling of the face, tongue, throat, or airways. Other symptoms of anaphylaxis include hives, flushed skin, nausea, and dizziness.
When a person with an allergy comes in contact with their allergen trigger, white blood cells release chemicals to attack the allergen
One of the chemicals released during anaphylaxis is histamine. Histamine causes the dilation (widening) of blood vessels and increases heart rate and gland secretion
Other chemicals released during the immune response cause constriction of the airways and increase the permeability of blood vessels
Hives (urticaria) is a common dermatological condition characterized by raised, itchy welts on the skin
Welts associated with hives have well-defined edges, may vary in size, and are often grouped together spanning a large area
The appearance of hives is initiated by the release of inflammatory molecules from skin cells, commonly due to allergic reactions.
Swelling of the lips, eyes, and face is a common characteristic of anaphylaxis.
Swelling and constriction of the throat and airways can lead to wheezing and difficulty breathing.
During anaphylaxis, some individuals may stop breathing, and/or their heart stops beating
If this happens, the first step is to administer cardiopulmonary resuscitation (CPR)
Routes of Entry
Enteral Drugs: Medications that enter the body through the digestive tract, like oral medications such as pills or liquids
Parenteral Drugs: Enter the body in a manner other than through the digestive tract
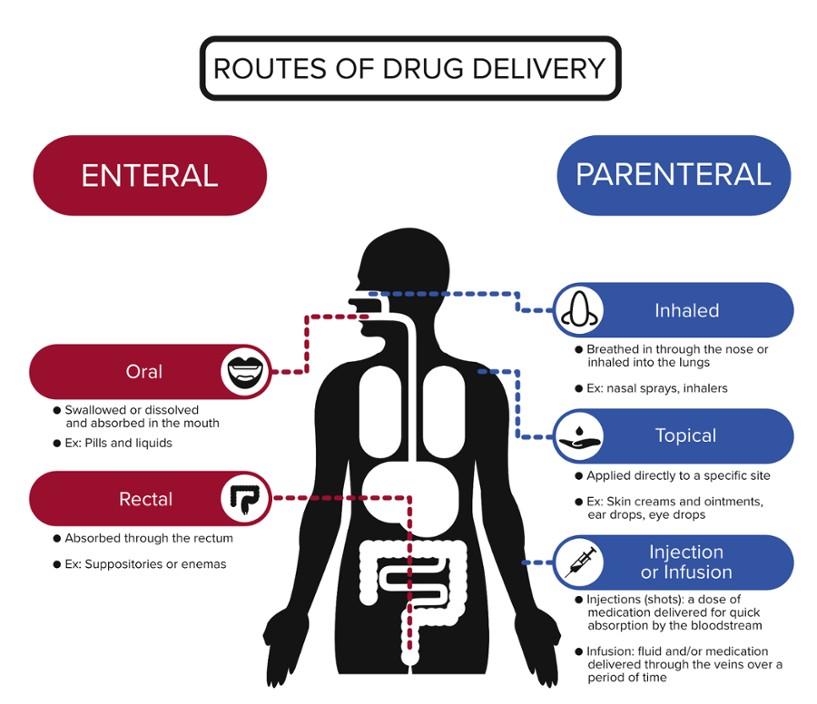
Intravenous injection | Delivers medicine directly into a vein. Used when a medication is needed quickly, if the liquid cannot be taken by mouth, or if it is too irritating for intramuscular or subcutaneous injections. |
Intramuscular injection | Delivers medicine into muscle tissue where it can be quickly absorbed by the bloodstream. Used to administer medication more quickly than a subcutaneous injection and is easier to administer than an IV. |
Subcutaneous injection | Delivers medicine into the tissue layer under the skin and above the muscle. Used to deliver medicine quickly, but it takes longer to go into effect than IV as it needs time to diffuse into the body. |
Determining Dose
Kilograms to Pounds: lb = kg x 2.2046
Weight (kg) | Dose (mg) |
7.5 -14.99 | 0.1 |
15 - 30 | 0.15 |
> 30 | 0.3 |
Healthy Hydration
IV refers to intravenous (IV) therapy, the delivery of medication and/or fluids over a period of time through a vein
A needle is used to place a tube called a catheter in a vein on either the back of the hand or the inside bend of the elbow. Medications and fluids can then be administered to the vein through the catheter.
IV Therapist: A licensed practical nurse (LPN) or registered nurse (RN) who obtains additional certification for IV therapy
IV therapists place IVs in patients, administer IV medications and fluids, and document and monitor patients’ progress.
The fluids in our bodies are not pure water; they’re solutions
Solutions are mixtures of a solvent, the substance doing the dissolving, and a solute, the substance being dissolved
In our bodies, the solvent is typically water. The outer membrane of our cells is semipermeable, meaning smaller molecules are able to pass through, but large molecules are not
Water molecules are able to diffuse or move in and out of the cell through special pores or channels called aquaporins. This movement is of water is called osmosis
Homeostasis: the body’s maintenance of a stable internal environment, the inside of cells and the blood that surrounds them contain the same relative concentration of solutes, and water remains balanced
If the balance of dissolved substances shifts, water will move and cells will either swell or shrink.
Cells that take in too much water will swell and can burst
Cells that lose water shrink and become shriveled
During osmosis, water moves from a high concentration to an area of lower concentration in an attempt to balance the concentration of solutes
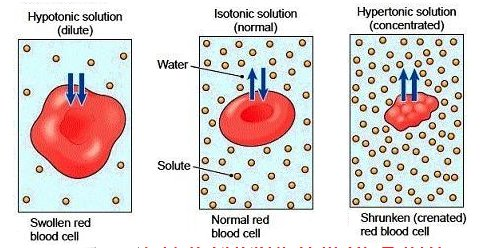
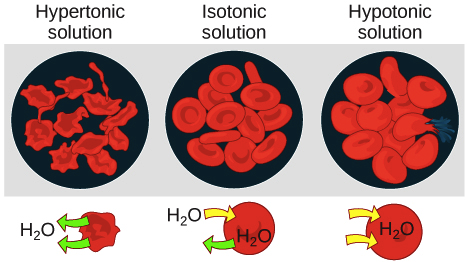
Three terms are used to describe solutions that affect the way water moves during osmosis: isotonic, hypotonic, and hypertonic
Isotonic: The concentration of solutes in the solution outside the cell is the same as that in the cell, there is no net movement of water
Hypotonic: The concentration of solutes outside the cell is less than that inside the cell, water moves into the cell and it swells
Hypertonic: The concentration of solutes outside the cell is greater than that inside the cell, water moves out of the cell and it shrinks
3.2.3 Control Bleeding
Under Pressure
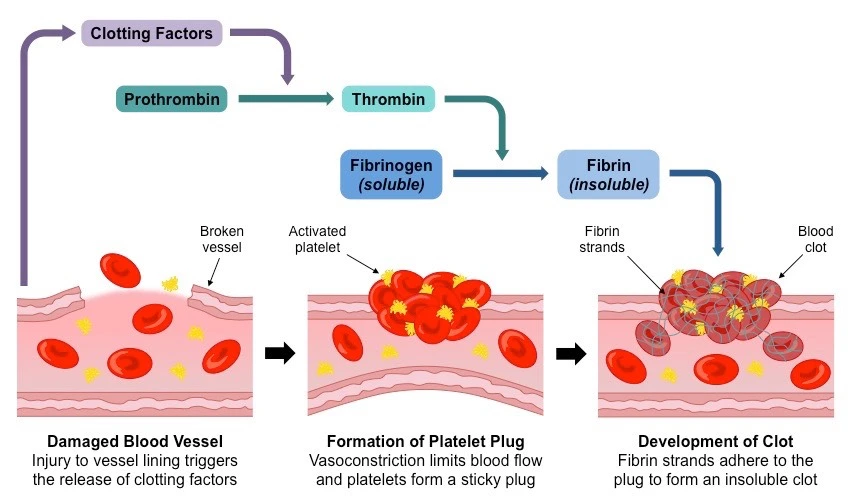
Bleeding occurs due to a damaged blood vessel that has broken open, and bleeding stops when the blood coming out of the injured blood vessel clots
Proteins cause platelets to become a sticky web of fibers, allowing them to stick together across an opening in the blood vessel and close the wound.
Steps to Stop Bleeding
Another set of ABCs to remember when you encounter an injured person and need to get their bleeding under control: Alert, Bleeding, Compress
Life-threatening Bleeding:
Blood will not stop coming out of the wound
Blood spurts out of the wound
Blood is pooling on the ground
Clothing is soaked with blood
Bandages continue to soak through with blood
Victim seems confused or is unconscious
Victim has lost all or part of an arm or leg
A tourniquet is a device that applies extra pressure to the vessels within an arm or leg to slow the flow of blood to that limb
To apply a Tourniquet:
Wrap the tourniquet around the limb about two to three inches above the wound
Important: Do not place the tourniquet onto a joint. Go above the joint if necessary
Pull the free end to make the tourniquet as tight as possible
Secure the free end
Tighten the tourniquet until the bleeding stops
Secure the tourniquet and note the time it was applied
A tourniquet is not a long-term solution, because it cuts off blood supply from all vessels that travel down that arm and will cause permanent tissue death to a limb after about two hour
Under Control
Ligate: tie-off an artery or vessel
An arterial bleed is typically more dangerous than a venous bleed
Arteries are more muscular than veins and carry blood under higher pressure
An arterial bleed spurts out blood in large volumes, whereas a venous bleed, while still dangerous, flows steadily with less volume
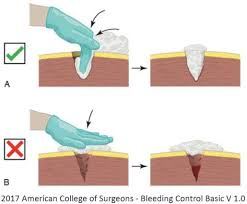
For life-threatening bleeding from the neck, shoulder or groin, or for bleeding from a limb when a tourniquet is not available, you need to pack, or stuff, the wound with gauze
This creates an even stronger barrier to prevent blood from flowing from the vessel
To pack a wound:
1. Wipe away any pooled blood
Stuff the wound with gauze or a clean cloth
Apply steady pressure with both hands directly on the bleeding wound.
Push down as hard as you can, and continue to hold pressure until help arrives
After the emergency medicine physician finishes providing medicine to the patient, you assist them in clamping and then ligating the injured vein.
Hemostat: A tool used to clamp an open blood vessel, and be sure to practice using one before you attempt to stop the bleed
3.2.4 Crisis Communication
The Art of Triage
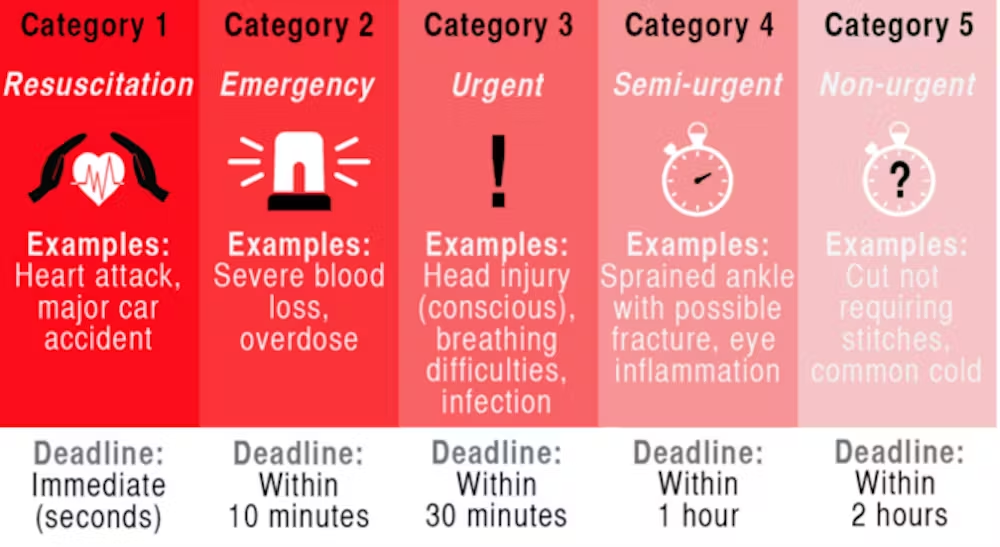
Triage: The process of prioritizing patients based on who is most in need of immediate care. Within triage are levels of priority
Following triage, patients will have a physical examination including measurement of vital signs
Steps of Emergency Care Triage:
Physical exam and diagnostic testing
Medical treatment and reevaluation
Admission to hospital or discharge to home
Triage Nurse: Often trained and licensed as a registered nurse (RN)
The Triage Categories:
Emergent: Highest priority; care needed immediately as the patient may not survive without treatment
Urgent: Care is needed quickly but can be delayed temporarily
Semi-urgent: Care is needed but can wait if other higher-priority patients exist
Non-urgent: Lowest priority; minor conditions which are not time-sensitive and care is not needed immediately
3.2.5 Medical Surge
The Aftermath
Medical Surge: Occurs when the number of new patients challenges or exceeds a hospital’s ability to serve all of them
Surge Capacity: Refers to the ability to care for an increased volume of patients that challenges or exceeds normal operations
This is a measure of how many patients a medical facility can triage, treat, and manage in addition to its normal average number of patients