Cardiomyopathy, Myocarditis and Pericarditis
dilated cardiomyopathy is usually the left ventricle, very large and dilated, hypertrophic left ventricles, cardiomyocytes on histology and contraction band necrosis
some causes reversible, treated underlying issues e.g. haemotopomosis
symptoms:
SOB, fatigue, orthopnea, paroxysmal nocturnal dyspnoea, weight gain, peripheral oedema
any systemic illnesses - viral illness could cause affected cardiomyopathy
examination - breathless, thready pulse, more likely to get Atrial fibrillation, as ventricles dilate atria more likely to dilate?, JVP elevated, displaced apex, 3rd or 4th heart sound, pan systolic murmur - mitral regurgitation (not primary cause), pulmonary oedema, fine crepitations
tests and medications:
ECG, CXR, BNP, Bloods - FBC, U&E, Echo, CMRI (cardiac MRI) to see areas of fibrosis and distribution, Coronary angiogram, sometimes biopsy depending on time course of cardiomyopathy
if people anemic correct anaemia
remove any unideal drugs eg NSAIDs
correct hypo/hyperthyroidism - endocrine disturbance
reduce salt
managing weight, keep record, if weight changes changing diet
ACEi, ATII blockers, diuertics, sac/val
beta blockers
spironolactone
anticogulants
SLE II inhibitors
risk of cardiac death
prognosis generally poor but improved a little
restrictive and infiltrative cardiomyopathy - don’t relax so blood less likely to fill
seen in younger patients
restrictitve and infiltrative cardiomyopathy:
diuretics mostly
beta blockers
anticoagulants
SCD risk
cardiac transplant
endomyocardial fibrosis less specific treatment
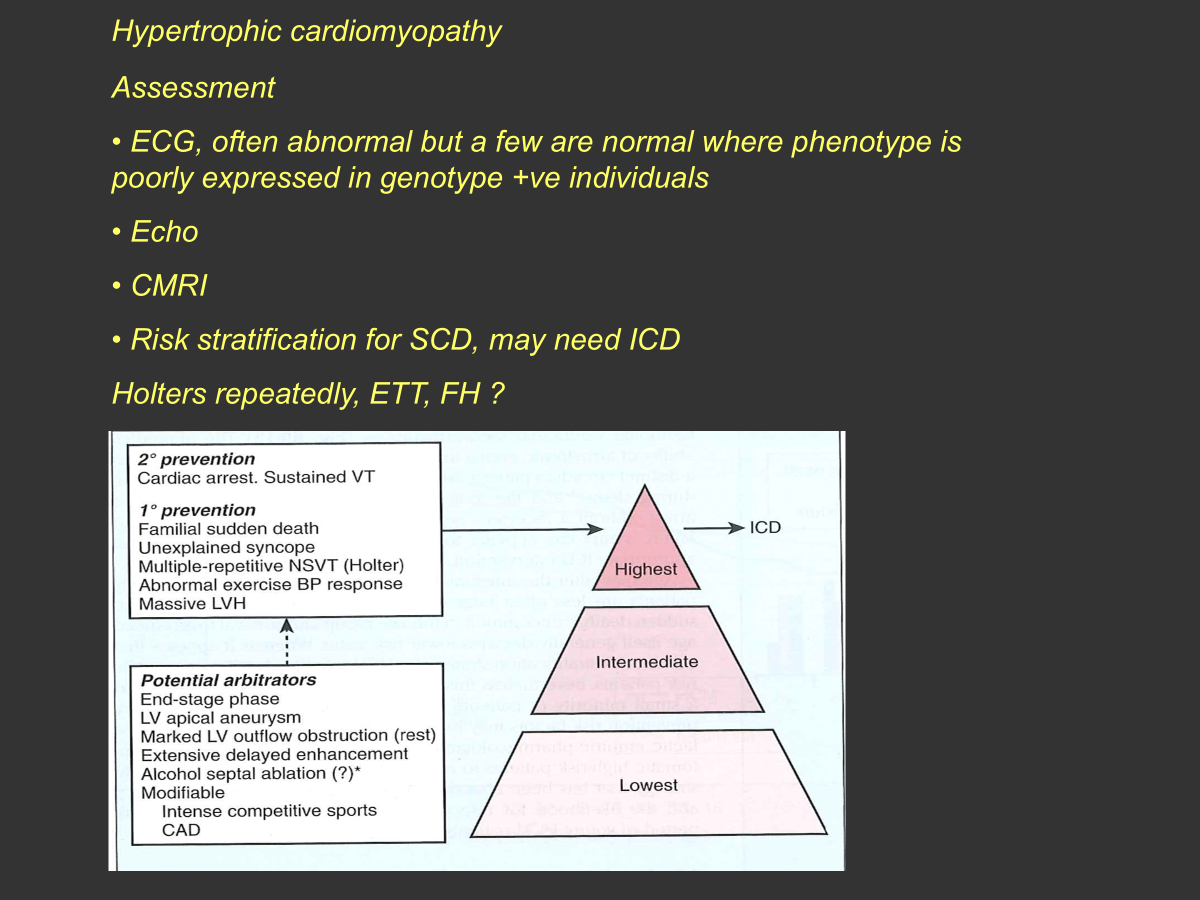
hypertrophic cardiomyopathy:
impaired relaxation common feature and systolic function adequate
most common form is myocyte hypertrophy and disarray
impaired relaxation so behaves in a restrictive manner
asymptomatic
can be breathless, can have raised JVP, palpitations, syncope, anginal like chest pain
ECG abnormal, LV hypertrophy pattern on ECG on lateral leads
echo
CMRI, conclusive for hypertrophic phenotype or not, patterns of fibrosis
Exercise Treadmill test for hypertrophic cardiomyopathy score
avoid dehydration- at least 3L, avoid heavy masses
explore family member history if they have kids for genetic testing
beta blockers, verapamil (CCB- non DHP), disopyrimide (sodium channel blocker), mavocantan (myosin inhibitor) - causes drastic reversibility in myocardium sickness, only used in small number of patients
myocarditis = acute or chronic inflammation of the myocardium, can be in association with pericarditis
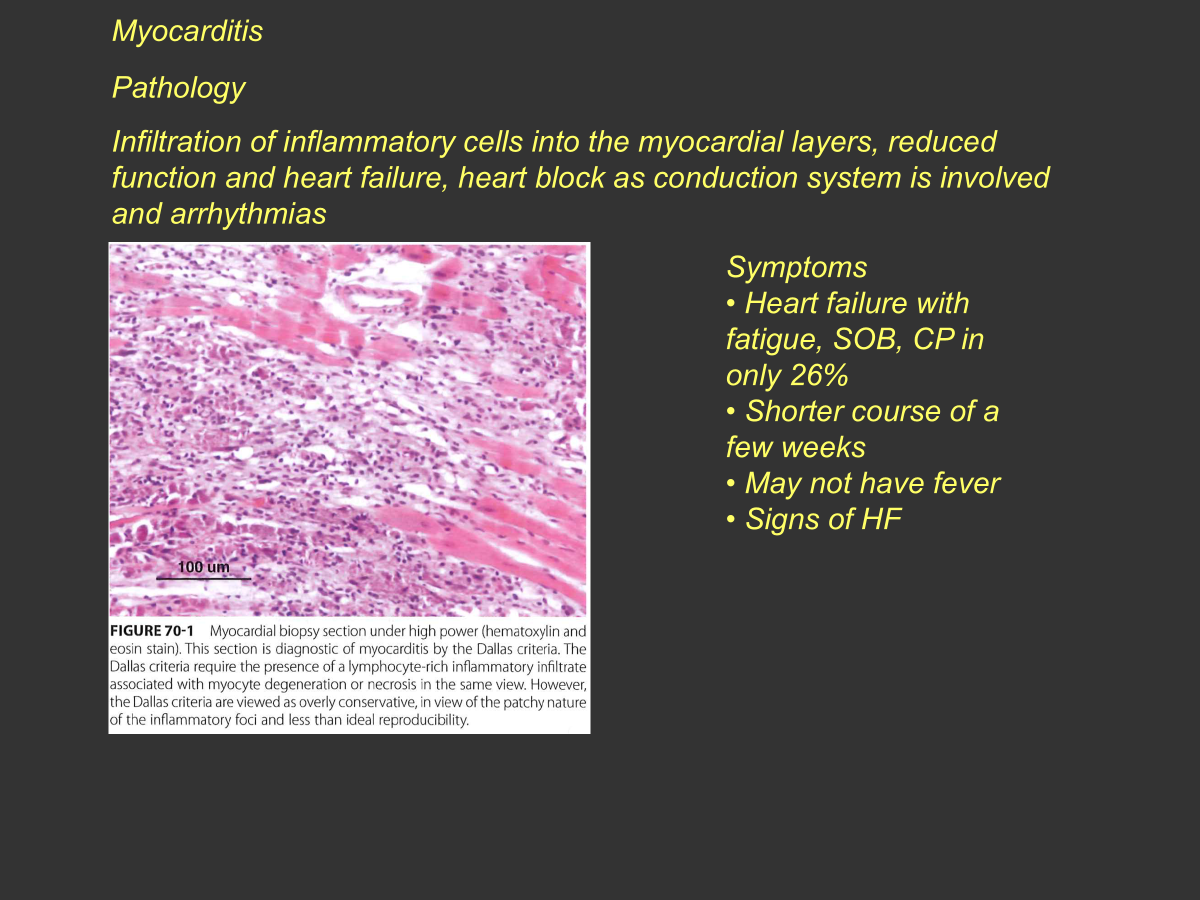
can get VT or even complete heart block
heart failure, fatigue, SOB, CP
may not have fever, present very acutely
ECG usually abnormal, biomarkers often elevated -troponin, don’t fall in pattern with MI, elevated troponin that stays persistently elevated for a long time
observe until biomarkers fall as high risk of VT or VF
Echo, can get RWMA
CMRI can see oedema in certain images
biopsy is unsure, infiltration of immune cells
treatment generally supportive - analgesia, painkillers, amiodarone to suppress arrhythmias, stop any toxic agent exposure or drugs
pericardial disease
pericarditis - inflammation of pericardial layer with or without myocardial involvement
pneumonia, post MI, perforation or dissection- main things of pericarditis
short duration, chest pain, runny nose, temperature, JVP if large pericardial effusion
high fever and very unwell despite no effusion may suggest bacterial
ECG-PR elevation, echo
troponin may be raised if myocardial involvement
paracetamol, ibuprofen, alotrasine? if viral
idiopathic colchicine and NSAIDs
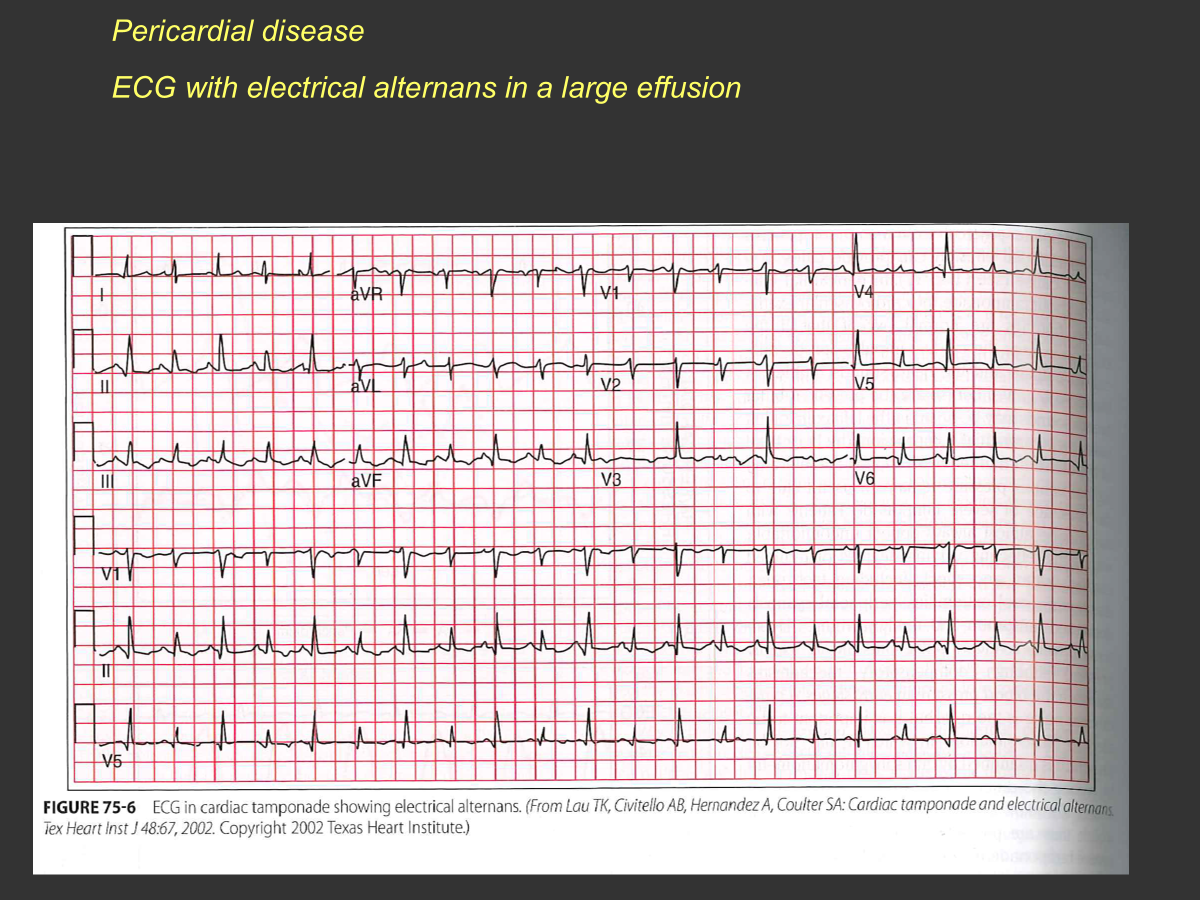
pericardial effusion
may be haemodynamically significant
-drainage main treatment
ECG large QRS, small QRS large QRS …
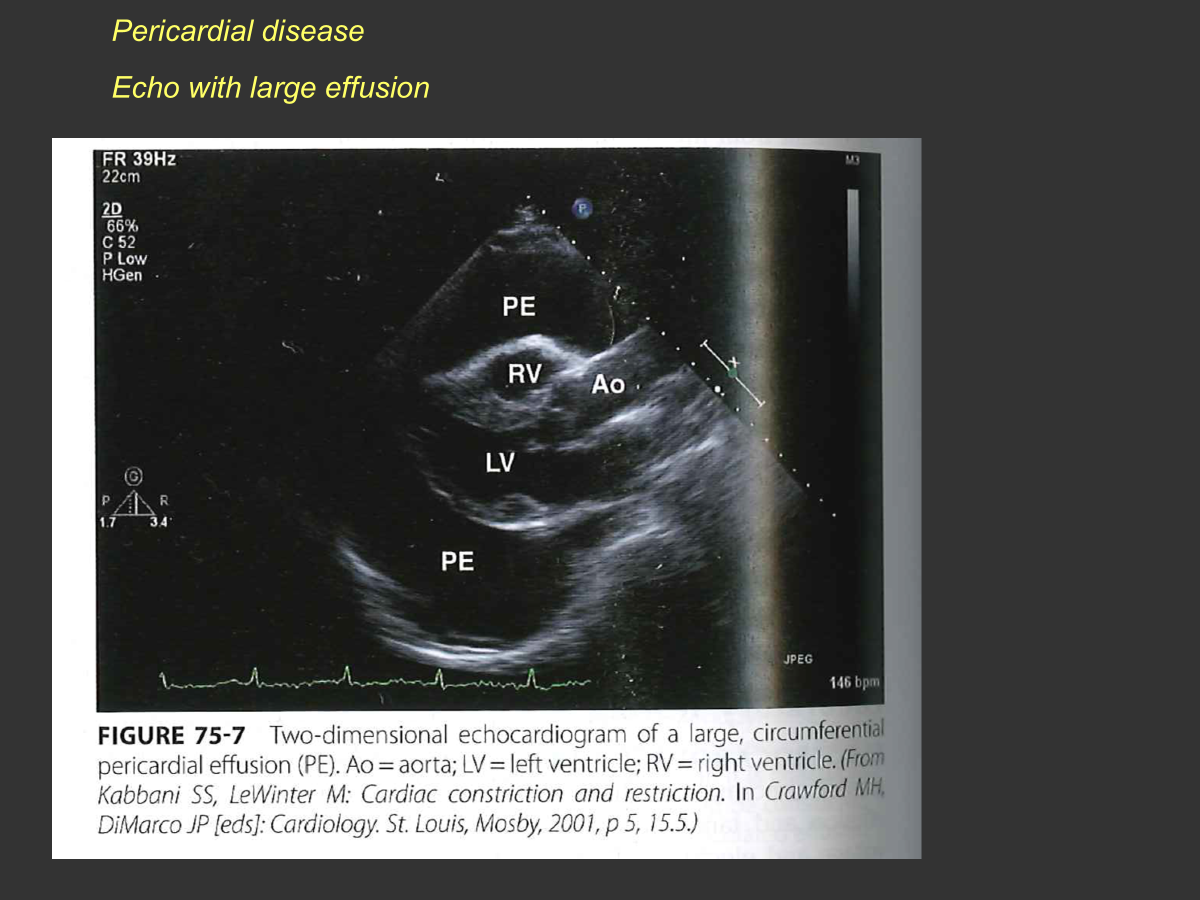
PE= pericardial effusion
constrictive pericarditis is rare, reoccurring, idiopathic, radiation, post surgery, autoimmune, renal failure, sarcoid
impaired filling but myocardium usually normal
fatigue, SOB, cough
signs similar to right heart failure
diuretics and pericardectomy-treatment