Schizophrenia
Diagnosis and Classification
Classification: Taking a set of symptoms and categorising them. If an individual has a particular set of symptoms it can then be said that they have schizophrenia.
Diagnosis: The clinical judgment that the individual is suffering from the disorder.
Introduction
Only 1% of the population have a diagnosis.
Men are more likely to be diagnosed.
Lower class are more likely to be diagnosed
Diagnosis is a very inexact science
Onset begins at 16 to 25
Committed suicide is 10%
Schizophrenia is a type of psychotic illness, a disorder where people lose touch with reality. Sufferers tend to think things which cannot be true and/or hearing voices or seeing visions when there is no sensory stimuli to create them, it can affect any of the senses.
People with schizophrenia do not always display psychotic symptoms, the episodic illness occurs in periods of psychotic disturbance interspersed with more normal periods of functioning.
It is characterised by profound disruption of cognition and emotion, which affects language, thought, perception, and sense of self.
Psychosis: Used to describe a severe mental health problem where the individual loses contact with reality. They are unaware they have a problem.
Neurosis: They are aware they have a problem.
Stirling and Hellewell (1999)
About 25% of sufferers will get better after only one episode, 50-65% will improve but continue to have bouts of the illness. The remainder will have persistent difficulties.
Classification
Kraepelin claimed that certain groups of symptoms occur together often, thus allowing diagnosis of diseases or syndromes, this is the stem of all mental disorders and diagnosis from today. He regarded each mental illness as distinct from all others with its own origins, symptoms, course and outcomes.
DSM: The Diagnostic Statistical Manual of Mental Disorders, the official system used by APA.
ICD: The International Classification of Diseases, published by World Health Organisation.
Classification is important to make diagnosis more reliable and valid by laying down rules for the inclusion or exclusion of cases. Its function is to inform effective treatment selection, administrate functions (legal systems), to provide vocabulary for professionals to communicate with, and to provide information on prognosis.
Without a classification, then individuals cannot be diagnosed. Classification ensures clinicians are referring to the same thing, and allows comparable groups for research.
When evaluating symptoms and deciding what is abnormal these things need to be considered:
Patient’s self-control
Patient’s self-awareness
Extremes of the patient’s behaviour
Distress caused for self and/or others
Subjectivity of definitions
Context
Homeless or drunk on the street, which is perceived as abnormal
Therefore, there is no single definition of what ‘abnormal’ is. Identification and treatment of people with mental illness is not always helpful or effective, a more reliable system needs to be established.
Symptoms
Prodrome: An early symptom indicating the onset of a disease or illness, found in hindsight.
Prodromal symptoms may be exhibited by an individual weeks or months preceding schizophrenia. These symptoms are not enough to diagnose the illness as they also occur in other illnesses. Prodromal symptoms include:
Anhedonia - loss of interest in usual activities
Avoiding the company of others
Staying away from work or school
Being irritable and oversensitive
Lack of interest in personal appearance and hygiene
generalised anxiety mild degrees of depression
Positive Symptoms: The addition of something to normal functioning
Hallucinations
Sensory experiences, some are related to events in the environment whereas others bear no relationship to what the senses are picking up on.
For example, hearing voices talking to/commenting on the sufferer, often criticising them. The sufferer may see distorted facial expressions or people or animals that are not there.
Delusions
Irrational beliefs. Delusions of grandeur can involve being important historical, political, or religious figures. Delusions of paranoia can also involve being persecuted by the government, aliens, or superpowers (Russia). These delusions can concern the body, the sufferer may believe a part of them is under external control.
Echolalia
Pathological repetition of the words of others.
Negative Symptoms: The removal of something from normal functioning
Alogia
Speech poverty is characterised by changes/reductions in speech. ICD-10 recognises this as a negative symptom whereas the DSM focuses more on speech disorganisation, a positive symptom - incoherent speech.
It is a negative symptom as it is a reduction in amount and quality of speech, there may be a delay in the sufferer’s verbal responses during conversation.
Avolition
More commonly known as apathy - loss of motivation to carry out tasks and results in lower activity levels.
Andreason (1982) identified 3 signs of avolition: poor hygiene and grooming, lack of persistence in work/education, lack of energy.
Blunted Affect
Lack of emotional response.
Diagnosis is important for informed judgements about treatment to alleviate symptoms to be made. It can be comforting for the individual, it allows them to know there is something medically wrong and something can be done. It can give patients information about the course of disorder.
DSM versus ICD
DSM: The Diagnostic Statistical Manual of Mental Disorders, the official system used by APA.
ICD: The International Classification of Diseases, published by World Health Organisation.
DSM-IV | ICD-10 |
Requires 1 month of symptoms and 6 months of disturbance. | Requires 1 month of symptoms. |
2 symptoms and at least one is positive. | Only 1 symptom if it is positive, or 2 symptoms if it is negative. |
Takes into consideration social and/or occupational dysfunction. | Does not take into consideration any social or occupational dysfunction. |
0 sub-types | 7 sub-types. |
Types of Schizophrenia according to ICD
Paranoid
The extreme feeling of suspicion or grandeur; strong delusions and hallucinations interspersed with moments of being fine.
Catatonic
A person is withdrawn, mute, negative and often assumes very unusual body positions. There is a disturbance to movements, making sufferers either immobile or very mobile.
Hebephrenic
Primarily negative symptoms: apathy, lacks motivation.
Co-Morbidity and Symptom Overlap
The reliability and validity is made difficult because of co-morbidity.
Co-Morbidity: When two or more medical conditions occur at the same time. There is a tendency of medical conditions to co-exist alongside each other in one individual.
As co-morbidity exists, there is considerable symptom overlap.
Symptom Overlap: Shared symptoms could lead to an unreliable/incorrect diagnosis. A patient could have a symptom typical of schizophrenia but actually have another condition with the same symptom.
Reliability: the consistency of symptom measurement.
Inter-clinician reliability: Different clinicians make identical independent diagnoses of the same person. (Different clinicians, same diagnosis)
Test-retest reliability: When tests used to deliver these diagnoses are consistent over time. (Different time, same diagnosis)
Validity: The extent that a diagnosis represents something that is real and distinct from other disorders. It tests what is intended to be and is distinct from others.
Descriptive validity: Patients with schizophrenia should differ in symptoms from patients with other disorders.
Predictive validity: If diagnosis leads to successful treatment, then diagnosis is seen as valid.
Aetiological validity: All schizophrenia should have the same cause for the disorder, but it doesn’t. It might be claimed that because a treatment works, then something can be learnt about the disorder in the first place. (Taking ibuprofen and not having a headache, does not mean there was a headache to begin with.)
Reliability and Validity are inextricably linked. If scientists cannot agree who has schizophrenia (low reliability) then what it is, is questioned and becomes essentially meaningless. If what schizophrenia actually it is not agreed (low validity), then it cannot be agreed who has it.
Diagnosis and Classification: Evaluation
Problems with Reliability and Validity
One issue is that there are two classifications. Despite this, individuals should receive the same diagnosis from each if the diagnosis is reliable and classification is valid. The time taken into consideration differs from each manual, therefore it is more likely that someone will be diagnosed using the ICD than DSM. However, in practice this is not the case. Furthermore, for schizophrenia to a valid, distinct disorder there should be no variation in diagnosis, but the sub-types classified in ICD makes this not the case.
Cooper et al (1972) conducted a study which found that New York psychiatrists diagnosed schizophrenia twice as often compared to London psychiatrists. It was also found that the London psychiatrists diagnosed mania and depression twice as often. The study used the same videotaped clinical interviews thus showing issues with reliability.
The World Health Organisation (1973) compared psychiatrists from nine countries and found substantial agreement in 7 of them. The exceptions were USA and USSR which both seemed to have subjective concepts.
Elie Cheniaux et al (2009)
Two psychiatrists independently diagnosed 100 patients using both the DSM and ICD criteria.
Results found poor inter-clinician reliability
Using the DSM one psychiatrist diagnosed 26 patients, the other diagnosed 13.
Using the ICD one psychiatrist diagnosed 44 patients, the other diagnosed 24.
Results found poor validity
It is expected that one psychiatrist should diagnose the same number of patients regardless of classification manual.
It was found that a psychiatrist diagnosed 26 using the DSM and 44 using the ICD.
The definition of the disorder is invalid as it is not distinct enough to within the various manuals.
Counterpoint
One possibility of the inconsistency is that the psychiatrists may be more familiar with one diagnostic manual.
This can skew the results as the accustomed knowledge may lead the clinician to unconsciously fall into a habitual approach to diagnosis.
The study would need to be repeated to test reliability.
Flávia Osório et al (2019)
Reported excellent reliability for the diagnosis of schizophrenia in 180 individuals using the DSM-5 in which the WHO and APA collaborated.
Pairs of interviewers achieved inter-reviewer reliability of +0.97 and test-retest reliability of +0.92.
However, it could be argued that the situation is slowly improving.
As the manuals get a closer matching definition (get closer in validity), reliability gets more consistent (the more consistent diagnosis gets).
Osório was only using the DSM-5, therefore did not test the validity of schizophrenia as it did not compare the definitions given in the two manuals.
Cultural Bias
These systems of classification can be argued to be culturally biased. The classifications are created in the Western world based on Western ideals of mental health. Furthermore, the research systems are predominantly conducted in Western countries.
Acculturative Stress: The stress of living in another unfamiliar culture particularly relevant to immigrant populations who face multiple problems when living in an unfamiliar country/place or for those who have to move from place to place.
Research Evidence
Lewis (1990)
139 psychiatrists were shown case studies where the race was changed in some cases. (Race was the IV)
Psychiatrists prescribed more drugs and though behaviour was more criminal if the patient was black. A result of social stereotypes.
Simon et al (1973)
Black people are more likely to be diagnosed as schizophrenic.
However, Littlewood (1980) suggested that the judgement of insanity may be a result of a life of disadvantages and racism over actual symptoms.
Cochrane and Sashidharan (1995)
Black Afro-Caribbean people are seven times more likely to be diagnosed with schizophrenia as whites.
However, this suggests there may be a biological explanation to schizophrenia. This suggests a genetic disadvantage/predisposition to the disorder.
Attitudes
In South America, ayahuasca (a plant-based psychedelic) is an integral part of some tribal rituals.
The Peru government recognised its status in 2008 as “one of the basic pillars of the identity of the Amazon peoples.”
It is believed that this psychedelic and the hallucinations it causes are a gateway to the spiritual world.
However, according to Western ideas of mental health, hallucinations are a positive symptom of schizophrenia and this practice would be frowned upon.
In Maori culture matakites are visionaries (prophets) who hear voices and they are highly respected in the community.
The voices are not regarded as auditory hallucinations and the matakites are not diagnosed with schizophrenia (Lakeman 2001).
Gender Bias
Gender Bias is another issue with the current systems of classification. Generally, the systems are created by men and are based on typical male ideals of mental health. Research is also predominantly conducted on males.
Research Evidence
Leo and Cartagena (1999)
Most studies exclude women because of hormonal fluctuations which act as as a confounding variable.
Studies are androcentric due to this.
Furthermore textbooks focus on male behaviour and psychiatrists are familiar with male-based examples.
This assumes that men and women behave in the same way.
Robins et al (1984)
Men are more likely to have problems with alcohol whereas women are more likely to have problems with depression/phobias, more mental problems.
Men are more likely to be diagnosed with schizophrenia.
On the other hand, this could be due to the stress of being female such as the sexism, stereotyping, and dual roles women have been handed.
Goldstein (1993)
Women are more likely to be voluntary schizophrenia patients.
This means that women are more likely to admit to themselves and others there is something wrong mentally.
This highlights the stereotypes within modern society.
Thus, the gender bias within the classifications exacerbates discrimination through defining schizophrenia using deviation from social norms.
Biological Explanation
Assumptions:
All mental disorders have a physical cause
Eg are caused by micro-organisms, genetics, biochemistry or neuroanatomy
Mental illnesses can be described in terms of clusters of symptoms.
Symptoms can be identified, leading to diagnosis.
Diagnosis leads to appropriate physical treatments.
Genetic Basis
Evidence suggests that the closer the biological relationship, the greater risk of developing schizophrenia. There isn’t one gene that seems to be responsible for the disorder, instead it is thought of as a polygenetic disorder.
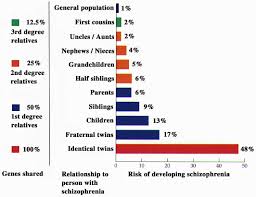
Gottesman and Shields graph shows there is a strong relationship between genetic material and prevalence of schizophrenia. On the other hand:
If schizophrenia was purely caused by biological factors, the prevalence of Monozygotic twins (identical twins) should be 100%. This highlights the fact that there are other factors to be considered.
The graph may show the risk of schizophrenia due to the time spent with people.
Concordance Rates
Gottesman and Shields (1991) - Twin Studies
Twin studies have identified strong concordance rates of 48% in MZ twins and 17% in DZ twins.
Twin studies are used as Monozygotic twins share 100% DNA, therefore genetics can be isolated as a variable.
If the concordance rate is 100% then means the disorder is genetically determined.
Family Studies are used as children share 50% of their DNA with parents. Adoption studies are used to test whether genetics have a higher influence or the environment does.
Only 1% prevalence rate in the general population which is the same all over the world.
There are variations within broad geographical areas.
Torrey (2002) found high rates in Ireland of about 4% of the population, it is also high in Croatia and Scandinavian countries but is low in Spain and Italy. The rate is very low in parts of Africa.
This could be due to many different factors including access to high level healthcare.
This suggests there are environmental factors which play a role in Schizophrenia.
Neural Correlates: Dopamine Hypothesis
Dopamine appears to work differently in patients with schizophrenia. It is particularly important in the functioning of several brain systems which are linked with symptoms of the disorder, specifically with the cortex and the subcortex.
The Original Hypothesis
The hypothesis states that the brain of schizophrenic patients produces more dopamine than the brain of a neurotypical person. These patients broadly suffered from having too much dopamine in their neural networks. Dopamine receptors are known to play a key role in guiding attention and perception.
This is supported by the fact that suffers of schizophrenia who were given dopamine antagonists found that, although the drugs were effective, mainly for positive symptoms, they gave them side-effects including Parkinsonism. (Vice versa for sufferers of Parkinson’s - they developed schizophrenic like symptoms.)
The hypothesis is based on the knowledge that antipsychotic drugs reduce dopamine activity.
Antipsychotic drugs
can produce side effects similar to Parkinson’s disease which is caused by low dopamine in the brain.
Agonist - initiates a physiological response when combined with a receptor.
Grilly (2002)
Individuals with Parkinson’s were prescribed L-Dopa (the precursor to dopamine) to raise dopamine levels in the brain.
Some individuals went on to develop schizophrenia-like symptoms.
Antagonist - depresses the effects of an agonist.
The Newer Hypothesis
The newer hypothesis is more nuanced, in that it claims the issue may be more about having more dopamine receptors, rather than actual dopamine. The sufferers experience hyperdopaminergia in the subcortex and hypodopaminergia in the cortex.
HypERdopaminergia - Excessive levels of dopamine in the subcortex and Broca’s area.
HypOdopaminergia - Low levels of dopamine in the prefrontal cortex.
Biological Explanation: Evaluation
Genetic Basis
Gottesman and Shields (1991)
The graph shows that MZ twins have a concordance rate of 48%.
Despite the graph showing a strong biological explanation for schizophrenia:
If schizophrenia was purely caused by biological factors, the prevalence of Monozygotic twins (identical twins) should be 100%. This highlights the fact that there are other factors to be considered.
The graph may show the risk of schizophrenia due to the time spent with people.
Furthermore, no study has found a 100% concordance rate between MZ twins implying there is another, non biological factor which influences schizophrenia.
A more holistic explanation may be needed such as the diathesis-stress model.
An interactionist approach which states that people can have a genetic predisposition but the symptoms only develop when triggered by an environmental stressor, (drugs, bereavement).
Environmental Factors
Research limits the biological explanation as it provides clear evidence that there are environmental and psychological factors that increase the risk of developing schizophrenia.
Di Forti et al (2015) found that smoking THC-rich cannabis in teenage years increasing the risk of developing the disorder.
Nina Mørkved et al (2017) found that 67% of schizophrenic patients reported at least one childhood trauma compared to only 38% of a matched control group.
However, Tienari et al (2004) showed heightened risk due to genetics.
Biological children of schizophrenic parents have a heightened risk even if they grow up in an adoptive family.
Supports biological explanation, as genetics played a significant role in the development of the disorder.
Neural Correlates: Dopamine Hypothesis
Research Evidence
There is evidence that supports the dopamine hypothesis.
Falkai et al (1988) found increases dopamine levels in the left amygdala in post-mortems of schizophrenic patients.
This is supported by Seidman (1990) who found larger dopamine receptors in the post-mortems of schizophrenic patients.
However, post-mortems are purely correlational. It cannot be determined what caused schizophrenia from a post-mortem.
Is the increased level of dopamine a cause of schizophrenia, or does schizophrenia cause higher dopamine levels?
The hypothesis is only correlational as the method is not fully scientific because an individual cannot be tested before schizophrenia.
However, Farde et al (199)
No difference
Real World Application
The hypothesis is strengthened by the application to drug-based treatments.
Antipsychotic drugs such as chlorpromazine reduce symptoms by inhibiting dopamine transmission.
Tauscher et al (2014) found that antipsychotic drugs reduce dopamine activity and reduce the intensity of symptoms.
However, the treatment-aetiology fallacy needs to be considered. The fact that biological therapies are effective, does not show that the biological explanation is in-fact true.
In-fact, antipsychotics only reduce all symptoms in around 20% of patients.
Additionally, some antipsychotics take several weeks to reduce positive symptoms despite blocking dopamine receptors straightaway.
This suggests that there may be other non-biological factors which influence schizophrenia.
Other Neurotransmitters
One limitation is that evidence suggests dopamine is not the only neurotransmitter involved.
Moghaddam and Javitt (2012) found evidence for the role of glutamate.
It was found that schizophrenic patients have a deficiency in glutamate function in several brain regions. (McCutcheon et al, 2020)
Deterministic
The biological explanation is high deterministic.
It states that the disorder is completely out of the individuals hands, there is nothing that they can do to change this.
However this may be the case. Schizophrenics often have no control over their behaviour and symptoms.
On the other hand, this approach suggests that the individual cannot do anything to alleviate their symptoms, which may hinder their recovery.
Psychological Explanation
Many theories explaining schizophrenia ignore culture and society. Family, friends, society, and culture in general could have a role in the development and maintenance of schizophrenia.
Family Dysfunction
Schizophrenogenic Mothers
The theory proposed by Frieda Fromm-Reichmann (Neo-Freudian - Psychodynamic Approach) suggested that schizophrenia was caused by mothers who were overly dominant in the home particularly towards the schizophrenic child.
The schizophrenogenic mother was controlling, overprotective, cold and distant/rejecting. This stifles the child’s development and the distance leaves the child feeling emotionally insecure. These mixed messages and general distrust could lead to the paranoia and delusions.
Double-Bind Theory
Double-bind: Statement which binds the child into losing despite the content being kind.
Double-bind explains that schizophrenia is a consequence of abnormal and inadequate patterns of communication within the families of schizophrenics. It is the way the parents or other family members interact with the child that causes the schizophrenia. Constant exposure to this communication style may lead the child to become unable to respond logically to others.
Bateson (1956) found that families of schizophrenics communicate in a destructively ambiguous fashion. For example, the tone of saying a loving statement suggests hostility. Paralanguage may not match the words.
Paralanguage: tone of voice, body language, facial expressions, non-verbal communication.
The child is getting two contradicting messages causing a conflict often placing the child in a lose-lose situation. Children learn that they have no idea how to respond in a reasonable way in conversations, growing up to believe this is how normal relationships function. Therefore in the future they will struggle in establishing normal relationships.
R.D Laing said that what we call schizophrenia is a reasonable response in an insane world.
Bateson argued double-bind could eventually lead to hallucinations and delusions arsing as a means to escape the conflict caused by the contradiction. Double-bind statements can also cause the child to respond with maladaptive thinking patterns to help them navigate social situations.
Berger (1965) interviewed schizophrenics and found that they have a higher recall of these double-bind statements by their mothers than non-schizophrenic controls.
Mischler and Waxler (1968) found that mothers talking to their schizophrenic daughters were rather aloof and unresponsive. However, the same mothers behaved in a much more normal and responsive way when talking to theri neurotypical daughters.
Expressed Emotion
Families who engage in expressed emotion show high levels of criticism, hostility, and emotional over-protectiveness.
verbal criticism
anger, rejecting, often hostile
over-protectiveness and over-involvement
sometimes to the extent of needless self-sacrifice.
Communication low in expressed emotion is typically characterised by warmth and unconditional positive regard.
Kavanagh (1992) found that schizophrenics in families with high expressed emotion were 4 times more likely to relapse compared with those who live in low expressed emotion families.
Cognitive Explanations
Metarepresentation
Dysfunctional thought processing: metarepresentation
Behaviour is thought to be a product of internal mental processes such as perception, attention, language, and mental illness is caused by problems with these processes.
Internal Mental Processes
Cognition
Perception, Attention, Language
Impairments with processing emotion, social cues and ToM.
Frith (1992)
Schizophrenics misattribute their inner voice to the outside world. Frith speculated that the cognitive deficits were linked to irregularity in the neuronal pathways between the septo-hippocampal system (linked to learning, memory) and the prefrontal cortext.
Theory of Mind (ToM)
The ability to understand one’s self has their own mind, each individual has their own mind, and that one’s mind acts differently and distinctively from everyone else.
ToM starts to develop at 2-3 years old but does not fully form until much later in life. Young children are unable to understand that other people have minds seperate from their own.
Functions
Understanding that desires and points of views are not necessarily the same.
Understanding that people may not have access to the same information.
Understanding that actions and thoughts are caused by ourselves, and are generated internally rather than by any external force.
Frith (1992)
Frith argued that some of the cognitive impairments shown by schizophrenics are due to faulty ToM.
Schizophrenics do not have a clear grasp of their own mind, misunderstanding their own thought processes.
They are unable to distinguish between actions that are brought about by external forces and those that generate internally.
This is dysfunctional metarepresentation.
He argued that most symptoms can be explained in terms of deficits in three cognitive processes:
Inability to generate willed action (Avolition)
Unable to effectively generate action, may not be able to do tasks that they need to do or may forget which tasks that they have and haven’t done.
Inability to monitor willed action
Unaware of their own intentions and the ‘sense of effort’ that goes into generating behaviour. They are only able to monitor their actions on the basis of observing the consequences of their behaviour once it has already been carried out. They may misinterpret their actions as being caused by an external force.
Inability to monitor the beliefs and intentions of others.
They may struggle to monitor and interpret the behaviour of others leading to misinterpretation that could result in delusions of persecution.
He argued that problems with the ToM are due to a disconnection between the frontal areas of the brain concerned with action and the more posterior areas that control perception.
Central Control
Dysfunctional thought processing: central control
Brains are constantly receiving vast amounts of information from the world around yet humans have an ability to suppress automatic responses and perform deliberate actions instead.
Frith (1979): Attention Deficit Theory
Schizophrenia is the result of the breakdown of thought filtering processes, such as issues with attention which can lead to an inability to effectively filter non-pertinent information. This causes an inability to focus properly causing disordered thinking possibly accounting for hallucinations, delusions, and disorganised speech.
These cognitive deficits may be caused by abnormalities in those areas of the brain that use dopamine, especially the prefrontal cortex.
Bentall (1994) found that schizophrenics have attentional bias towards stimuli of a threatening and emotional nature making them more likely to perceive a stimuli as threatening when it isn’t. The inability of schizophrenics to effectively focus their attention on the appropriate elements of the environment may also account for why many schizophrenics have problems with memory recall of events.
Psychological Explanation: Evaluation
Dysfunctional Families
Schizophrenogenic Mother
Research Evidence
There is very little evidence instead research shows the opposite
Waring and Ricks (1965) found mothers tended to be anxious, shy, withdrawn and incoherent instead of controlling, overprotective, cold and distant/rejecting.
Wild et al (1975) found that it was the fathers of schizophrenics rather than mothers that play the more dominant role.
Cause and Effect
There is an issue with cause and effect.
It is difficult to determine whether the mother’s personality actually leads to schizophrenia.
It instead could be the fact the child is schizophrenic that causes a mother to respond and treat the child in a more distant and cold manner.
It is possible that the mother’s behaviour is caused by a genetic vulnerability to mental illness which has been passed to the child.
The Genain Quadruplets all developed schizophrenia by the age of 24 highlighting a genetic vulnerability.
Incomplete
This explanation does not explain why some people do not develop schizophrenia.
It does not explain the case for those with schizophrenia and warm mothers
The case for non-schizophrenics but a cold, controlling mother.
It does not explain why some people without a mother figure develop schizophrenia.
Sexist
The theory places blame, shame and guilt on the mother which is blatantly sexist.
Double Bind
Research Evidence
Evidence for the influence of double-bind is conflicted and weak.
Ringuette and Kennedy (1966) found that experts in the double bind theory were no better than non-experts at identifying double bind statements in letters written to schizophrenics.
Schuman (1967) argued that there is confusion around defining what double-bind statements even are. This has impeded the research and provided little support to the theory.
Cause and Effect
The theory argues that ambiguous communication from the parents leads to schizophrenia.
However, it could be that being schizophrenic changes the way in which family members communicate with that person.
Frustration and hostility from dealing with a difficult disorder is masked in verbal linguistics but not paralinguistics.
Perhaps there is a third factor causing both the schizophrenia and the double-bind communication.
Genes could cause the parent’s poor communication which are passed to the child and cause schizophrenia.
Environment such poverty can cause very stressful and frustrating environment. This may trigger the disorder and leads to double-bind communication.
Incomplete
Although the explanation could explain why schizophrenia runs in families, it does not explain everything.
Parents may communicate in the same way to every child yet not every child develops schizophrenia.
It brings to question whether one child is singled out.
Sexist
Child typically spend more time with mothers, so mothers are more likely to be held accountable.
Expressed Emotion
Expressed Emotion is more common in cases of relapse.
Research Evidence
Expressed Emotion cannot provide a complete explanation as it cannot explain what caused the illness in the first place.
There is no evidence that expressed emotions can trigger schizophrenia in someone who has never had it before.
Cutting et al (2006) found that schizophrenic patients were able to understand the criticisms of others and that affected their wellbeing. Yet those patients could not perceive the emotional over-involvement.
This suggests that not all elements of expressed emotion have an impact on schizophrenia.
Cause and Effect
The theory describes that expressed emotion can trigger the relapse of schizophrenia, and that the higher the level of expressed emotion the more likely relapse is.
Maybe being schizophrenic changes the way in which family members communicate with their family. Living with a schizophrenic may be stressful, the behaviour causes family to communicate with them in a more hostile, destructive way.
Perhaps there is a third factor causing both schizophrenia and expressed emotions.
Genes
Environment
Incomplete
Families do not communicate in a consistent manner all the time.
Some days there may be stressful events occurring so expressed emotion is high. Other days are dull thus expressed emotion is low.
Sexist
There is an implicit sense blame in expressed emotion theory.
Schizophrenia is seen as the fault of the family, yet it can be argued that the blame is actually with the mother who is typically the primary caregiver.
Overall
There is evidence supporting the role of dysfunctional families in general
Berry et al (2008) showed that adults with insecure attachments were far more likely to have schizophrenia.
Read et al (2005) showed that a very high number of schizophrenics suffered some kind of abuse when they were children.
However, there are methodological issues.
Self-report reduces the validity as it is common for schizophrenics have a negative outlook.
Many theories are controversial, often observed and unscientific. There has been significant backlash against ‘parent-blaming.
Cognitive Explanations
Metarepresentation
An impaired ToM has been heavily implicated in people who are diagnosed with autism.
This weakens the theory as how can the same thing manifest as autism in one person but schizophrenia in another.
It does not explain where the impairment came from.
Central Control
Stirling et al (2006) showed how schizophrenics got on with various cognitive tasks - including the Stroop test - their low scores underlined the central control theory.
Overall
This provides good explanation for positive symptoms but it is limited as it ignores biological theories.
Neuroscience provides a better explanation than cognitive and biological theories alone.
One methodological issue is that many studies are lab experiments.
Many schizophrenics are on medication.
The medication can affect the brain, weakening the validity of the study.
The medication could mask cognitive deficits and so the patient may perform better.
The medication may worsen cognitive skills so the results are not directly derived from schizophrenia.
The studies can lack generalisability.
However, conducting research on non-medicated schizophrenics may be impractical and unethical.
CBT is limited in its effectiveness when not combined with antipsychotics.
Cognitive explanations cannot be the only theory.
These explanations can be useful to help develop methods to cope with symptoms.
Cause and Effect
It is uncertain whether the cognitive errors cause the symptoms of schizophrenia, and it is unknown where these then came from.
It could be that schizophrenia caused the cognitive errors, but then it is unknown where the disorder came from.
Biological Therapies
Introduction
Antipsychotics work by altering levels of neurotransmitters in the brain. This links to the dopamine hypothesis.
There are a number of types of Dopamine (D) receptors which correspond to the different areas of the brain. D2 receptors, found in the limbic system are the receptors that seem to be linked to schizophrenia, specifically positive symptoms.
Kapur et al (2000)
Approximately, 60-75% of D2 receptors need to be blocked, in the mesolimbic pathway, for drugs to be effective. However, D2 receptors are found in the rest of the brain as well which means that blocking these receptors can lead to negative side effects.
The first antipsychotic drug developed was Chlorpromazine in the 1950’s. However, how the drug actually worked was unknown, as it also acted as sedative. Since the 50s, many more antipsychotics have been developed which have a great variety in effectiveness and side-effects, thus there is no one cure-all drug. Antipsychotics are only a treatment, not a cure.
Typical
Example: Chlorpromazine
Dopamine Antagonists
There is a strong association between the use of typical antipsychotics and the original dopamine hypothesis. Thus, typical antipsychotics work by acting as antagonists, reducing the action of a neurotransmitter.
Dopamine antagonists work by blocking receptors in the synapses of the brain, reducing the action of dopamine. According to the hypothesis, this normalises neurotransmission in key areas of the brain, reducing symptoms like hallucinations (positive symptoms).
Sedation Effect
Chlorpromazine is also an effective sedative. This is believed to be related to its effect on histamine receptors but it is not fully understood.
Side-Effects
When the extrapyramidal network in the cerebral cortex is impacted: this is the motor area, which is concerned with movements and motor activity.
Prolonged use of typical neuroleptics can lead to side effects such as involuntary movements of the tongue, face, jaw, etc, (this is Tardive Dyskinesia), dizziness, agitation, stiff jaw, weight gain, and itchy skin, even NMS.
NMS - Neuroleptic Malignant Syndrome is characterised by high fever, stiff, rigid muscles, altered mental status, autonomic nervous system dysfunction.
Typical antipsychotics are used primarily to combat the positive symptoms of schizophrenia. An example of a typical antipsychotic is the drug chlorpromazine. The basic function of this drug is to reduce or block the effects of dopamine and therefore reduce the symptoms. Drugs like chlorpromazine are dopamine antagonists, as they bing to dopamine receptors (particularly the D2 receptors), reducing their action and not stimulating them. By reducing stimulation of the dopamine system in the limbic system in the brain, antipsychotic drugs can eliminate the hallucinations and delusions experienced by sufferers. Therefore, antipsychotic drugs like chlorpromazine work by blocking dopamine production through blocking the receptors in synapses that absorb dopamine and eventually normalising neurotransmitters by ensuring the post-synaptic cells receive less and can’t be affected by dopamine.
Atypical
Example: Clozapine
Partial Dopamine Agonists
Clozapine binds to dopamine receptors just the same as chlorpromazine, but in addition it acts upon serotonin, glutamate, and ACh. This helps improve mood and reduce depression and anxiety, and it may improve cognitive functioning. The mood-enhancing effects means that the drug is sometimes prescribed when an individual is suicidal.
In areas of the brain where dopamine is too high, it occupies the receptors, but only gives partial response so that the result is reduced activity. In areas of the brain where dopamine is too low, it acts to boost the levels of dopamine activity.
Side-Effects
Agranulocytosis is a life-threatening condition that involves having severely low levels of white blood cells needed to fight infection.
Atypical antipsychotics also combat the positive symptoms, but there are claims that they also have beneficial effects on negative symptoms as well. An example of an atypical antipsychotic is clozapine. These drugs also work on the dopamine system but also block serotonin and glutamate receptors. Drugs like clozapine work by temporarily occupying the D2 receptors and then rapidly dissociating it to allow normal dopamine distribution, as this means the receptors still receive dopamine but just in smaller levels. These drugs are thought to be responsible for lower levels of side effects (such as Tardive dyskinesia) compared with typical antipsychotics. Tardive dyskinesia is associated with a variety of involuntary repetitive movement caused by long-term or high-dose typical antipsychotics. The term tardive dyskinesia was introduced in 1964: Dyskinesia refers to an involuntary movement. The effect of these drugs can be tardive, meaning the dyskinesia sometimes continues or appears even after the drugs are no longer taken.
Overview
Typical | Atypical |
First commonly used in the 50s. | First commonly used in the 70s. |
Primarily acts as dopamine antagonists. | Act as partial dopamine agonists. |
Reduces positive symptoms. | Reduces positive symptoms, more notably reduces negative. |
Acts on dopamine. | Acts on dopamine, serotonin, glutamate, and ACh (acetylcholine). |
Side-Effects: Tardive Dyskinesia, Parkinsonism, dizziness, agitation, stiff jaw, weight gain, NMS, itchy skin. | Side-Effect: Agranulocytosis |
Biological Therapies: Evaluation
Effectiveness
Research Evidence
Lobos (2010)
He compared clozapine with a number of other atypical antipsychotics and found that it faired very favourably in reducing the positive symptoms of the illness.
However, the risk of serious side effects caused many patients to drop out of the study. (High attrition rates)
Furthermore, he found that clozapine did not work very well in patients resistant to treatment, so it was often paired with another antipsychotic, therefore causation is questioned.
Valenstein et al (2004)
A study on over 63000 schizophrenics taking antipsychotic medication, found that about 40% of cases, adherence to the regime was poor.
The only drug where this was not a problem was clozapine, which had only 4.6% of patients showing poor adherence. This is opposite of what Lobos found.
Adherence varied for different groups.
Young people were less likely to adhere than old people.
African-Americans were less likely to adhere than white Americans.
Adherence to the medication schedule
Some patients may be hospitalised, medicated, discharged but once discharged struggle to adhere to their medication schedule becoming ill again. Readmission to hospital may occur because of the risk of not taking medicine.
The high attrition rate of not taking the drugs leads to the revolving door psychiatry phenomenon.
This may be due to:
Unbearable side-effects
Feeling “normal” as schizophrenia is a psychosis illness.
Feelings of paranoia, or persecutory delusions.
This non-compliance is an issue, as in the real world, adherence may not be straightforward leaving the drug ineffective in ecological validity.
Ethics
Chemical Straightjacket
Not all psychologists and psychiatrists are convinced that medication is the best way to treat schizophrenia.
Moncrieff (2006)
He found that the withdrawal from atypical antipsychotics, especially Clozapine, can cause psychosis even in patients without a history of psychosis. A schizophrenic’s negative symptoms may appear to worsen should they withdraw atypical neuroleptic treatment, so it is important to do so slowly to reduce effects.
Szasz (1960)
Amongst others in the antipsychiatry movement, he argues that medication is being used in the same way as a straightjacket.
It isn’t being used with the aim of reducing the suffering of the schizophrenic, but rather as a way of making the patient more compliant and to make them conform to society’s view of normal.
On the other hand
Many schizophrenics suffer greatly because of their illness, and refusing treatment to these patients would likewise be unethical.
It could be argued that due to the increased risk of self-harm and suicide that goes with schizophrenia, doing something is much more ethical than doing nothing.
Drugs may give an enhanced quality of life.
Mechanism Unclear
How some antipsychotics work is unknown.
Understanding of the mechanism by which antipsychotics work is strongly tied up with the original dopamine hypothesis, however it is known that the original hypothesis is not a complete explanation.
It is unknown why treatments work for some schizophrenics and not others. Similarly it is unknown why some medication have different side-effects for different patients.
This could be stressful and frustrating for the patient (trailing various drugs until the correct combination is found) and in the short-term may even make their symptoms worse.
However, millions of people have benefitted from the use of these drugs. They may not be perfect, but they are the best available.
Social Implications
Impact of antipsychotics
Before antipsychotics, treatment was limited.
Often treatment was institutionalisation, other treatments were cruel and ineffective.
Chlorpromazine sparked a revolution in the treatment of schizophrenia. The impact it had on treating psychosis has been compared to the impact that penicillin had on the treatment of infection.
Antipsychotics have meant that there are less people institutionalised.
Less people in institutional care increases the amount of money that can be spent elsewhere.
However, it could be argued that be releasing schizophrenics from hospital, there is a risk of non-adherence to medication. This could possibly be linked to a risk of violent crime.
Cost
Long-term medication is costly, but so is not providing treatment in the long-term.
Cost must be consider in relation to other treatments, and the analysis of benefit of a patient returning to work.
The cheapest drug to produce is chlorpromazine.
However, due to side-effects, it has generally been phased out in the Western world in favour for more modern antipsychotics with fewer side-effects.
Due to its low cost, it is still regularly used in developing countries.
Social Implications
Some antipsychotics have side-effects that may require further treatment, but this has both social and economical implications.
Antipsychotics that cause weight gain, for example, may lead to high blood pressure or diabetes which require expensive treatment.
The risk of the possibly fatal agranulocytosis means that schizophrenics taking clozapine need constant monitoring which can be expensive.
Psychological Therapies
A principle part of the psychological approach’s explanation is the unhealthy cognitive processes that can occur in individuals suffering from schizophrenia. If that is correct, then psychological therapies should revolve around correcting that.
CBTp
Cognitive Behaviour Therapy psychiatry
Beck - Faulty information processing, negative self-schemas, and the negative triad. This is mostly for reactive depression but also for endogenous depression.
Ellis - The ABC model is for reactive depression (eg depression as a result of bereavement).
The aim of CBTp:
Help the patient identify and challenge their delusions
Use evidence to challenge symptoms
Alter the way in which the patient thinks
Manage and organise their disordered thinking
Challenge maladaptive thoughts and replace them with constructive thinking.
During regular sessions, patients are encouraged to trace back to the origins of their symptoms in order to gain insight into the way in which they may have developed the illness. Schizophrenics are often unaware that they are subject to cognitive errors, so the therapist will try to make these maladaptive thoughts conscious, and then by challenging them, the patient will see that there is no basis for these thoughts.
CBTp does not prevent or cure hallucinations or delusions but instead helps sufferers cope with their symptoms.
Key Components
Reality Testing
Hallucination investigation: For patients who hear voices, CBTp may help them attribute these voices as originating in their own mind, rather than from an external source. This may be done by getting the patient to focus on the nature of the voices they hear. This is normalisation.
Delusion investigation: For patients who experience delusions, these can be tested and challenged in a controlled environment so that the schizophrenic may see them for the false beliefs that they are.
Psychoeducation
The therapist teaches the patient about their illness, and how it can be managed. This decatastrophises, and normalises, the symptoms. Once completed, they will go into more detail, such as identifying specific triggers for the patient, and how to avoid them.
Relapse Prevention Strategies
The schizophrenic can recognise and anticipate the signs and symptoms of relapse. The therapist and patient create a checklist of warning signs that might signal a relapse of the illness, and situations or triggers that might make relapse more likely. This helps to develop a plan, which can be used by the social network and family of the schizophrenic. (links to family therapy)
Socratic Questioning
These are a series of curiosity-driven questions given by the therapist during CBTp sessions to help the schizophrenic identify errors in their thinking. This includes challenging the patient to find evidence that supports their delusions. The aim is that the lack of evidence should undermine the patient’s belief in the delusion.
Gentle questioning is used by the therapist, to avoid double bind statements, to help the patients understand their illogical thought processing.
There needs to be trust between the therapist and the patient. The core conditions of empathy and unconditional positive regard must also be present.
Family Therapy
Usually taken place within the person’s homes (because of the encoding specificity principle), the therapists work with the family and the patient to develop strategies to cope better with the mental disorder and its symptoms. Hopefully, this leads to a more supportive and warmer atmosphere (linking to family dysfunction, especially expressed emotion) which helps the patient make better progress and the relatives to feel more positive and more effective in their supporting roles.
The therapist encourages relatives to:
Ask questions to learn more about the disorder so they can properly understand the difficulties the patient faces.
Learn more constructive ways of communicating
Concentrate on any good things that happen rather than negative events.
Remember it’s normal to feel angry and impatient but that they need to find ways of coping with these feeling without resorting back to EE patterns of behaviour.
Learn to recognise the early signs of relapse so that they can respond rapidly to reduce the severity of it.
The goal is to provide the whole family with practical coping skills which enable them to manage the everyday difficulties arising from having schizophrenia in the family.
Pharoah (2010)
Fiona Pharoah et al identified a range of strategies by which family therapists aim to improve the function of a family member suffering from schizophrenia.
Forming therapeutic alliance with all family members
Reducing the stress of caring for the patient
Improving the ability of the family to anticipate and solve problems
Reduce anger and guilt
Help members achieve a balance between caring for the individual and maintaining their own lives
Improving families’ beliefs about and behaviour towards schizophrenia
Pharoah et al suggested that these strategies work by reducing levels of stress and expressed emotion, whilst increasing the chances of patients’ complying with medication. The combination of benefits tends to result in a reduced likelihood of relapse and re-admission to hospital.
Psychological Therapies: Evaluation
Effectiveness
Research Evidence
Jauhar et al (2014)
Reviewed 32 studies of using CBT with schizophrenia, concluding that there is clear evidence for small but significant effects on both positive and negative symptoms.
Turkington et al (2004)
Uses examples to show CBT designed to challenge schizophrenic thinking.
Pontillo et al (2016)
Found reductions in frequency and severity of auditory hallucinations,.
CBT is rarely used as the sole treatment of schizophrenia. Most of the time it is paired with antipsychotic medication.
This challenges causation
Causation cannot be established as CBT cannot be isolated to measure its effectiveness.
Not for Everyone
CBT is not for everyone.
Severe symptoms that are resistant to treatment make CBT essentially ineffective.
Schizophrenics in denial about their illness makes CBT ineffective.
CBT requires self-awareness and willingness to engage with the process.
Those who get the most out of it are those who want to get better and change their behaviour, it allows the patient to take control and responsibility.
Effectiveness may be enhanced by the fact that the sample used in CBT studies are already biased towards having less severe symptoms, and an increased willingness to work to overcome their illness.
This impacts generalisability.
CBT may not be recommended as an appropriate treatment for everyone as it requires self-awareness, willingness to engage, and can be lengthy (causing attrition).
Addington and Addington (2005) suggested that the initial acute phase is not conductive to self-reflection, therefore engagement to CBT is a problem.
Once symptoms have stabilised with medications, group CBT may be more beneficial.
Quality of Research
Thomas (2015) pointed out that different studies have involved the use of different CBT techniques and people with different combinations of positive and negative symptoms.
There is a lack of a control group in research.
This could be due to the fact that there is no such thing as a placebo CBT.
Reduction in symptoms may be due to the placebo effect and not the CBT techniques itself.
Symptom reduction may be due to being able to talk openly and freely about the illness without judgement, as opposed to the perceived effectiveness of the CBT.
National Institute for Clinical Excellence (NICE)
CBTp is more effective in reducing rehospitalisation rates after 18 months than standard care alone (antipsychotics).
CBT is also effective in reducing severity of symptoms and can improve social functioning.
However
It is difficult to establish the effectiveness of CBT alone, as most patients use it in conjunction with antipsychotics.
It is also recommended to try alternative therapies, like art-therapy or nature-therapy, which are not as costly or time consuming, and have very positive results in trials.
Ethical Issues
Side Effects
CBT does not have the side effects associated with antipsychotics.
However, without antipsychotics CBT is difficult or even impossible.
The lack of side effects may be cancelled out by the lack of symptom reduction that would result from using CBT without medication.
Cognitive Focus
Bentall et al (1994) argued that in CBT the emphasis is on controlling the thought processes rather than understanding the unconscious thoughts and feelings behind them.
However, the nature and content of the delusion may have its roots in the schizophrenic’s childhood.
By only seeking to alter the current behaviour and thoughts rather than searching for the root cause, CBT could be argued to only be training the symptoms.
CBT is not a cure, thus this is a limitation of the therapy.
Social Implications
Not a cure
Despite not being a cure, CBT can reduce the reliance on medication providing additional support for schizophrenics.
It allows schizophrenics to develop the skills needed to cope with the symptoms.
However, CBT is not readily available for patients in some parts of the UK.
There exists a ‘postcode lottery’ where an individual’s access to psychological treatment is determined by the area in which they live.
Approximately 1 in 10 of those who need CBT are able to access it.
Haddock et al (2013)
Of 187 randomly selected schizophrenic patients from the North West of England, 6.9% had been offered CBT.
Cost
CBT may not be offered due to the cost involved.
CBT can be long term and costly
It might be cheaper to not bother with CBT and simply use antipsychotics instead.
Additionally, there is a long waiting list on NHS.
However, medication alone does not always produce the best outcomes.
Family Therapy
Research Evidence
McFarlane (2016)
By reviewing studies, concluded that family therapy was one of the most consistently effective treatment available for schizophrenia.
In particular, relapse rates were found to be reduced, typically by 50-60%.
Using family therapy as mental health starts to decline initially, is particularly promising.
Garety (2008)
Relapse rates are reduced to 25% following family therapy, as opposed to 50% for those receiving standard care alone.
Pharoah et al
Reviewed the evidence for the effectiveness of family therapy.
Concluded that there is moderate evidence to show that family therapy significantly reduces hospital readmission over the course of a year and improves the quality of life for patients and their families.
However, they also noted that results of different studies were inconsistent and that there were problems with the quality of some evidence.
Benefits to whole family
Lobban and Barrowclough (2016)
Concluded that these effects are important because families provide the bulk of care for people with schizophrenia.
By strengthening the functioning of the whole family, family therapy lessens the negative impact of schizophrenia on other family members and strengthens the ability of the family to support the person with schizophrenia.
National Collaborating Centre for Mental Health (2009)
A meta-analysis involving 32 studies and nearly 2500 participants.
Compared those having family therapy to those receiving standard, drug therapy alone.
The relapse rate in the family intervention condition was 26%, and in the control (standard care) condition relapse was 50%.
There was a reduction in hospital admissions during treatment, and in the severity of symptoms both during and up to 24 months following.
Has long-term impact
Management
There are a variety of ways used to help manage schizophrenia for example, token economies.
Token Economies
A token economy programme involves a system of rewards being set up for desired behaviour, sometimes paired with punishments to discourage undesirable behaviour.
Rewards are usually tokens or points (secondary reinforcers), that can be periodically exchanged for something that the individual wants (primary reinforcers). This has to be something they genuinely want. With Delay Discounting, the system becomes more effective as the longer between the receiving the token and getting the reward, the less the patient will link them.
This behaviour modification is based on Skinner’s Operant Conditioning.
Ayllon and Azrin (1968)
Used Token Economies in a women’s ward in a mental institution in the US.
The tokens were rewarded for self-care (brushing teeth, making the bed, showing).
These could be exchanged for privileges like watching films, cigarettes, etc.
It was found that desirable behaviours increased significantly.
However, these decreased significantly once the system was withdrawn.
Matson et al (2016)
Matson identified three categories of problematic behaviours that develop in a hospital, which can be addressed through the use of token economies.
Personal hygiene
Illness-related behaviours (problems due to positive and negative symptoms)
Social behaviours (problems in dealing with other people)
Management: Evaluation
General
The Token Economy programme can be administered by anyone with training, the tokens and rewards are relatively cheap which makes the programme inexpensive, and there are more benefits than there are costs.
However, programmes have to be carefully planned and controlled. There are many areas where problems can occur (such as lack of consistency from staff) which makes the programme less reliable due to lack of standardisation.
Furthermore, ethically it is problematic as standardisation is difficult. Rewards are easier to obtain by people with mild symptoms whose self-control is higher than patients with high functioning symptoms. This gives the professionals a lot of power, allowing them to impose the institution’s norms on the patients.
There have been studies which have found it to be successful - even though approximately 10-20% of people do not respond well to the programme.
However, learning may not transfer to the home environment which might lead to relapse.
There is an issue about effectiveness in the community. Generally, the scheme stops when a patient leaves a hospital and enters community care. In community care it is harder to monitor therefore tokens cannot be easily distributed and redeemed. This then may lead to issues when the incentives are suddenly taken away.
Research Evidence
Milby (1975)
Found that programmes were successful in psychiatric hospitals and helped in preparing to leave hospital.
However, the long-term effects were unknown.
Corrigan (1991)
Token Economies only work in hospitals. With outpatients in the community the programmes were not good.
Dickerson et al (2005)
Conducted a meta-analysis which found that almost all of the studies included were effective.
11 out of 13 studies had reported beneficial effects that were directly attributed to the use of token economies.
However, meta-analyses are subjected to the ‘file drawer problem’, a form of publication bias that can occur when there may be selective reporting of scientific findings to favour positive results.
Furthermore, they did caution that many of the studies reviewed had significant methodological issues that limited their impact in the overall assessment of token economies for schizophrenia.
This is supported by Comer (2013).
Comer (2013)
Suggested a major problem in assessing the effectiveness of token economies is that studies tend to be uncontrolled.
Typically all patients are brought into the programme rather than having an experiment group and a control group without the new token economy.
As a result, patients’ improvements can only be compared with their past behaviour. This comparison may be misleading as other factors, such as increase in staff attention, could be causing patients’ improvements rather than the token economy.
Causation cannot be established.
Interactionist Approach
The principle two approaches to discussing the explanations and treatment for schizophrenia are the biological and psychological. However, contemporarily most professionals in the field prefer an interactionist approach to both.
Explain the DSM is a common model of the interactionist approach.
Research shows the importance of biological factors in schizophrenia, research also shows the significance of environmental factors. The diathesis-stress model demonstrates the link between biological vulnerability (predisposition) and environmental stressors. The model explains that individuals will develop schizophrenia if they have a biological predisposition and if they are exposed to stressful situations.
Explanation
Meehl’s (1962) - Original Diathesis-Stress Model
Diathesis is entirely genetic which is extremely sensitive to stress. Schizophrenia is the result of a single schizogene which leads to a biologically based schizotypic personality that is triggered by a stressor.
No amount of stress will lead to schizophrenia if the gene is not present.
However, chronic stress in someone with the gene could lead to the development of the disorder.
Modern Model
Ripke found that there is not one single Schizogene that is responsible for schizophrenia - instead there are approximately 108 genes.
The modern Diathesis-Stress Model suggests that diathesis (vulnerability) is not just biological. The modern model suggests that diathesis can also be psychological trauma.
Read et al (2001)
Proposed a neuro-developmental model.
Early trauma affects the brain and its development.
For example, child abuse.
In some example, the HPA became over-active (the child was always alert, wary) leading to later vulnerability to stress.
Stress
It used to be seen that stressors were psychological in nature. Now it is seen that stessors can be anything (Houston et al).
There is a strong correlation between vulnerable people and cannabis use.
Shown to make the development up to seven times more likely.
However, since most people who smoke cannabis do not develop schizophrenia, the study shows how schizophrenia must develop with more than just a trigger hence the diathesis-stress model.
Tienari et al (2004)
A prospective study (a longitudinal study) of 19000 Finnish children adopted away from their biological family who had mothers diagnosed with schizophrenia.
The rearing style of the adoptive family was assessed.
The group were compared to a control group of children with no parent diagnosed with schizophrenia.
After 21 years, it was found:
In the adoptees at high genetic risk of schizophrenia, an adoptive-family with a high level of criticism and conflict was a significant predictor of schizophrenia.
However, in the adoptees with low genetic risk of schizophrenia, high level criticism was NOT a predictor of schizophrenia.
This suggests that either factor on its own does not cause schizophrenia, but when combined they increase the risk of developing the disorder.
No Genetic Vulnerability | Genetic Vulnerability | |
Well brought up | No Chance | No chance (basically) |
Not well brought up | No chance (basically) | Reasonable Chance |
Treatment
Treatments should include both biological treatments (drugs) and psychological treatments (CBT or/and family therapy).
Tarrier et al (2000)
It was found that receiving 20 sessions of CBT and 4 booster sessions within a year whilst taking antipsychotics patients functioned better and had lower symptoms levels compared to patients receiving drugs alone or attending counselling and taking drugs. However after 2 years, these patients did no better than the ones taking drugs and attending counselling. However, both groups (CBT and drugs, and drugs and counselling) functioned better than the group only receiving drugs.
Morrison et al (2014)
Found that drug treatment given with CBT lead to lower level in the severity of symptoms, and lower rehospitalisation than drug treatment alone.
Interactionist Approach: Evaluation
Research Evidence: Tienari Study
If in A03, explain the method briefly in A01
The study supports the interactionist approach as either factor on its own does not cause schizophrenia, but when combined they increase the risk of developing the disorder.
The trial had a huge sample size of children at risk of schizophrenia.
Despite being only Finnish children.
The experiment group of adopted children were compared to a control group.
However, the operationalisation of ‘not well brought up’ is a limitation.
Child-rearing style ignores other psychological factors which have been found to lead to schizophrenia.
Some children in the study with genetic vulnerability but not “bad” child-rearing style did develop schizophrenia. This suggests that there are other factors to consider.
Similarly, the operationalisation of genetic vulnerability is a limitation.
Tienari only considered whether the mother of the adoptees were diagnosed with schizophrenia.
This ignores other genetic vulnerability such as fathers or other family members being diagnosed.
Revised Understanding
The original model is too simplistic, the revised new model is more effective.
The new, nuanced model moved focus from purely one single gene effect to polygenic effect.
However, a limitation of the new, revised model is that it does not explain how schizophrenia works.
The understanding that vulnerability could be biological (genetic) or psychological (from trauma) can be vague.
The nuanced understanding makes curing and treatment difficult.
However, Tarrier et al (2000) found support for an interactionist approach to treatment.
Receiving CBT paired with drug therapy, or counselling paired with drug therapy, were more effective at relieving symptoms of schizophrenia than drug therapy alone.
Causation is another limitation of the interactionist approach.
Determining what are actually the causing triggers is complicated.
Furthermore, it would be unethical to isolate the stressors thus causation cannot be established.
Research Support
Read et al (2001) proposed the neurodevelopmental model where early trauma alters developing brains.
Turkington et al (2006) stated that it is fine to believe that schizophrenia has a biological cause but CBT can still be used to relieve symptoms.
Cannon (2002) found that there was a vulnerability of developing schizophrenia from birth trauma.
Wahlberg et al (2000) re-analysed Tienari’s work and found significantly less support for genetic factors.