Lecture 11: Alteration in digestive function
clinical manifestations of gastrointestinal dysfunction
anorexia
anorexia is a lack of a desire to eat despite physiologic stimuli that would normally produce hunger
vomiting
vomiting is the forceful emptying of the stomach and intestinal contents through the mouth
several types of stimuli initiate the vomiting reflex
chemoreceptor trigger zone (ctz) for vomiting is in the medulla oblongata
5-hydroxytryptamine (5-ht, aka serotonin) stimulates the emetic center
antiemetics, such as ondansetron and granisetron block the effects of 5-ht serotonin and are used to treat vomiting and nausea
nausea
nausea is a subjective experience that is associated with a number of conditions
the common symptoms of vomiting are hypersalivation and tachycardia
projectile vomiting
projectile vomiting is spontaneous vomiting that does not follow nausea or retching
it is caused by direct stimulation of the vomiting center by neurologic lesions involving the brainstem
constipation
constipation is defined as infrequent or difficult defecation
normal bowel habits range from two or three evacuations per day to one per week
pathophysiology
neurogenic disorders, functional or mechanical conditions, low residue diet, sedentary lifestyle, excessive use of antacids, changes in bowel habits
diarrhea
increased frequency of bowel movements
increased volume, fluidity, weight of the feces
more than three stools per day is considered abnormal (diarrhea)
adult intestine processes approximately 9L (2L ingested and 7L is intestinal secretion) of luminal content per day, of which 99% of the fluid is normally reabsorbed
with losses of more than 1000mL or more, the heart rate is greater than 100bpm and systolic bp is less than 100 mmhg
major mechanisms of diarrhea
osmotic diarrhea- nonabsorbable substance in the intestine draws water into the lumen by osmosis
if a person lacks the enzyme lactase and ingests lactose, the lactose will not be hydrolyzed and absorbed into the intestinal wall and result osmotic diarrhea
secretory diarrhea- large volume diarrhea caused by excessive mucosal secretion such as chloride
cholera is a form of secretory diarrhea
motility diarrhea- caused by resection of small intestine or surgical bypass of an area of the intestine
abdominal pain
abdominal pain is a symptom of a number of gi disorders
the casual mechanisms of abdominal pain are mechanical, chemical mediators of inflammation, or ischemic
chemical mediators, such as histamine, bradykinin, and serotonin produce abdominal pain
edema and vascular congestion produce abdominal pain by stretching
ischemia caused by distention of bowel obstruction or mesenteric vessel thrombosis produce abdominal pain
abdominal pain can be
parietal pain- arise from parietal peritoneum
the pain is more localized and intense
visceral pain- arise from stimulus acting on abdominal organ
visceral pain is diffuse, vague, poorly localized, and dull
referred pain- pain felt at some distance from disease or an affected organ ex. intense gallbladder pain is felt btwn the shoulder blades
pain is well localized
gastrointestinal bleeding
upper gastrointestinal bleeding
esophagus, stomach, or duodenum
lower gastrointestinal bleeding
below the ligament of treitz, or bleeding from the jejunum, ileum, colon, or rectum
acute blood loss is characterized by
hematemesis- the presence of blood in vomit
hematochezia- blood from rectum (frank bleeding of the rectum)
melena- dark tarry stool
occult bleeding- caused by slow chronic blood loss
disorders of motility:
dysphagia
dysphagia is difficulty swallowing
types
mechanical obstructions
functional obstructions
caused by a neural or muscular disorder
achalasia
denervation of smooth muscle in the esophagus and lower esophageal sphincter relaxation
manifestation: during eating or drinking may cause mild or severe stabbing pain at the level of obstruction
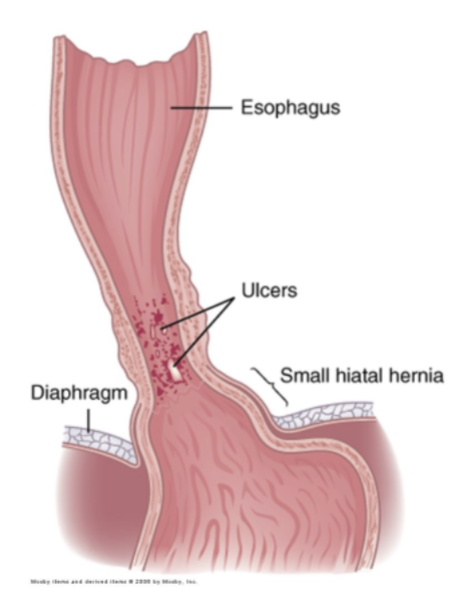
gastroesophageal reflux disease (gerd)
gerd is the reflux of chyme from the stomach to the esophagus
if gerd causes inflammation of the esophagus, it is called reflux esophagitis
a normal functioning lower esophageal sphincter maintains a zone of high pressure to prevent chyme reflux
a zone of low pressure of the lower esophageal sphincter (les) causes gastroesophageal reflux disease
inflammatory response to gastroesophageal reflux
inflammatory response to gastroesophageal reflux is defined as esophagitis
conditions that increase abdominal pressure can contribute to gerd
manifestations
heartburn, regurgitation of chyme, and upper abdominal pain within 1 hour of eating
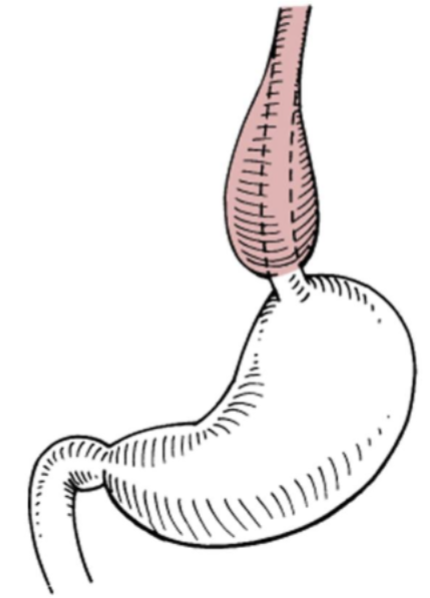
pyloric obstruction
pyloric obstruction is the blocking or narrowing of the opening btwn the stomach and the duodenum
pyloric obstruction can be acquired or congenital
manifestations
epigastric pain and fullness, nausea, succession splash (a specific sound heard in physical exam, occurs when theres a lot of fluid or gas trapped in the stomach), vomiting, and with a prolonged obstruction, malnutrition, dehydration, and extreme debilitation
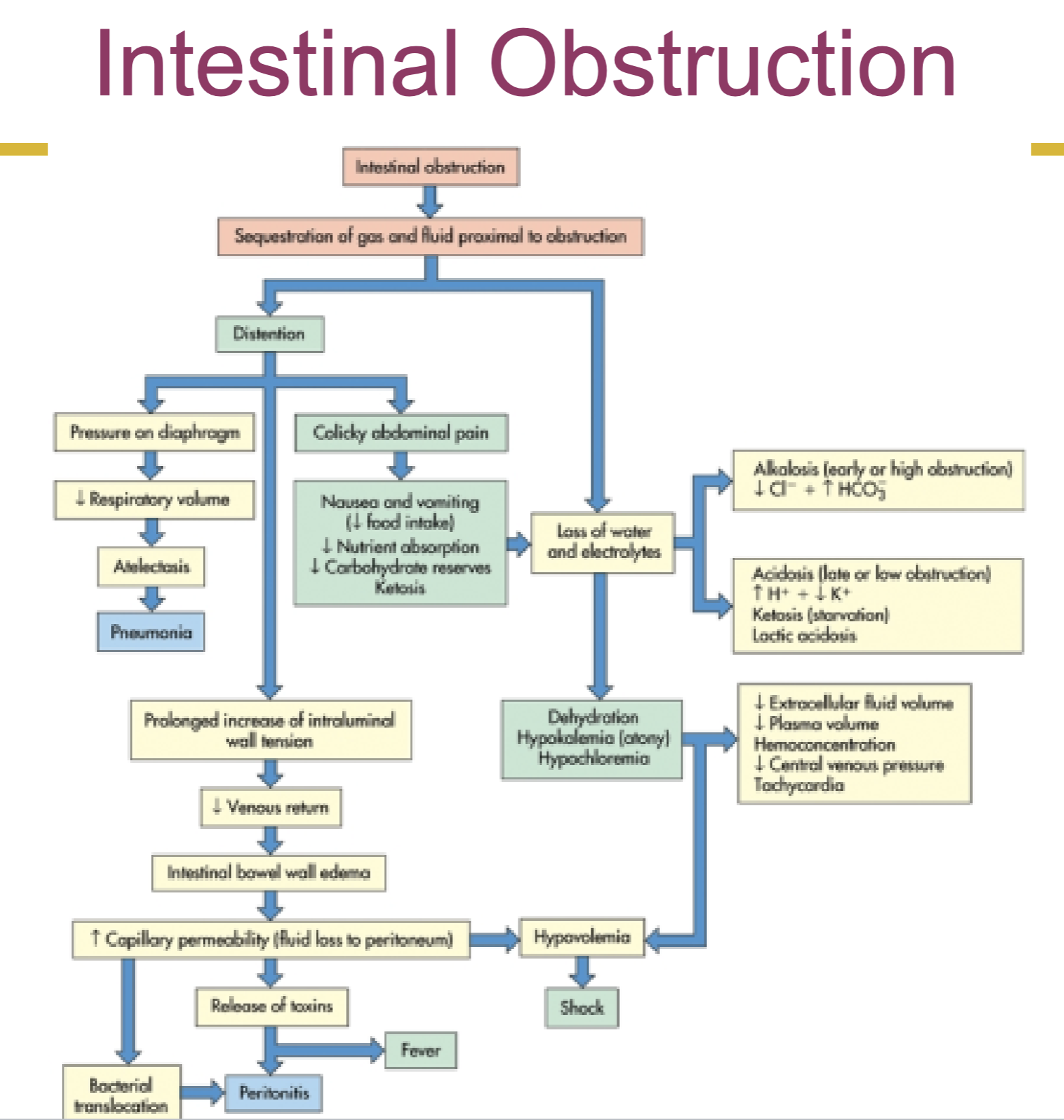
intestinal obstruction and ileus
an intestinal obstruction is any condition that prevents the flow of chyme through the intestinal lumen or failure of normal intestinal motility in the absence of an obstructing lesion
an ileus is an obstruction of the intestines
intestinal obstruction is a physical blockage often due to adhesions, tumors, or hernias. ileus is a functional issue (impaired intestinal motility, lack of normal muscle movement) w/o a physical obstruction
simple obstruction- mechanical blockage of lumen by lesion
functional obstruction- failure of mobility
small intestinal obstruction
caused by adhesions, hernia, and tumors
adhesions is the most common type of small intestine obstruction
intestinal obstruction at the pylorus or high in the small intestine cause metabolic alkalosis by an excessive loss of hydrogen ions normally absorbed from gastric juice
cardinal symptoms of small intestinal obstruction are colicky pain caused by distention followed by vomiting
large bowel obstruction
caused by colon cancer (90% of the time), mesenteric ischemia, and other inflammatory disease
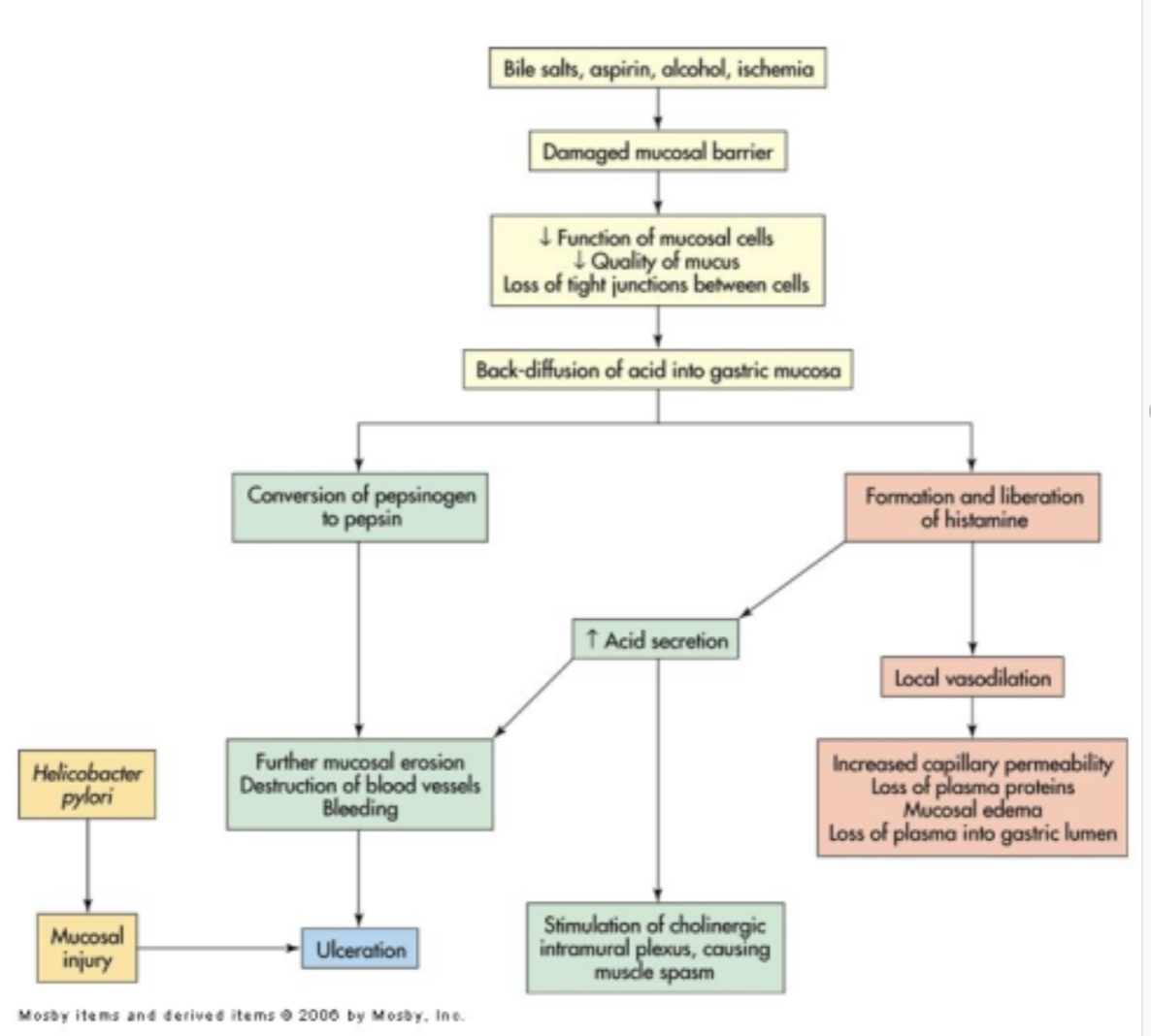
gastritis:
inflammatory disorder of the gastric mucosa
it can be
acute gastritis- is usually injury of protective mucosal barrier by drugs (ex. aspirin inhibits prostaglandin, which normally stimulate production of mucosa)
manifestations: vague abdominal pain, epigastric tenderness and bleeding
chronic gastritis- tends to occur in elderly
in chronic gastritis inflammatory cytokines such as tumor necrosis alpha (tnf-), interleukins (il-6, il-8, il-10), and leukotrienes are released
manifestation: older adults experience hemorrhage or perforation
peptic ulcer disease:
a peptic ulcer is a break or ulceration in the protective mucosal lining
a peptic ulcer may occur in esophagus, stomach, or duodenum
a peptic ulcer can be
acute
chronic
superficial- do not penetrate the muscularis mucosa
erosions
deep
true ulcers
duodenal ulcers
most common of the peptic ulcers
developmental factors:
helicobacter pylori is the primary cause of duodenal ulcers
toxins and enzymes that promote inflammation and ulceration
hypersecretion of stomach acid and pepsin
can be due to greater than usual number of parietal cells in the gastric mucosa
use of nsaids
high gastrin levels- gastrin levels remain high longer than normal after eating
acid production by cigarette smoking
failure of the feedback mechanism occurs, whereas acid in the gastric antrum inhibits gastrin release
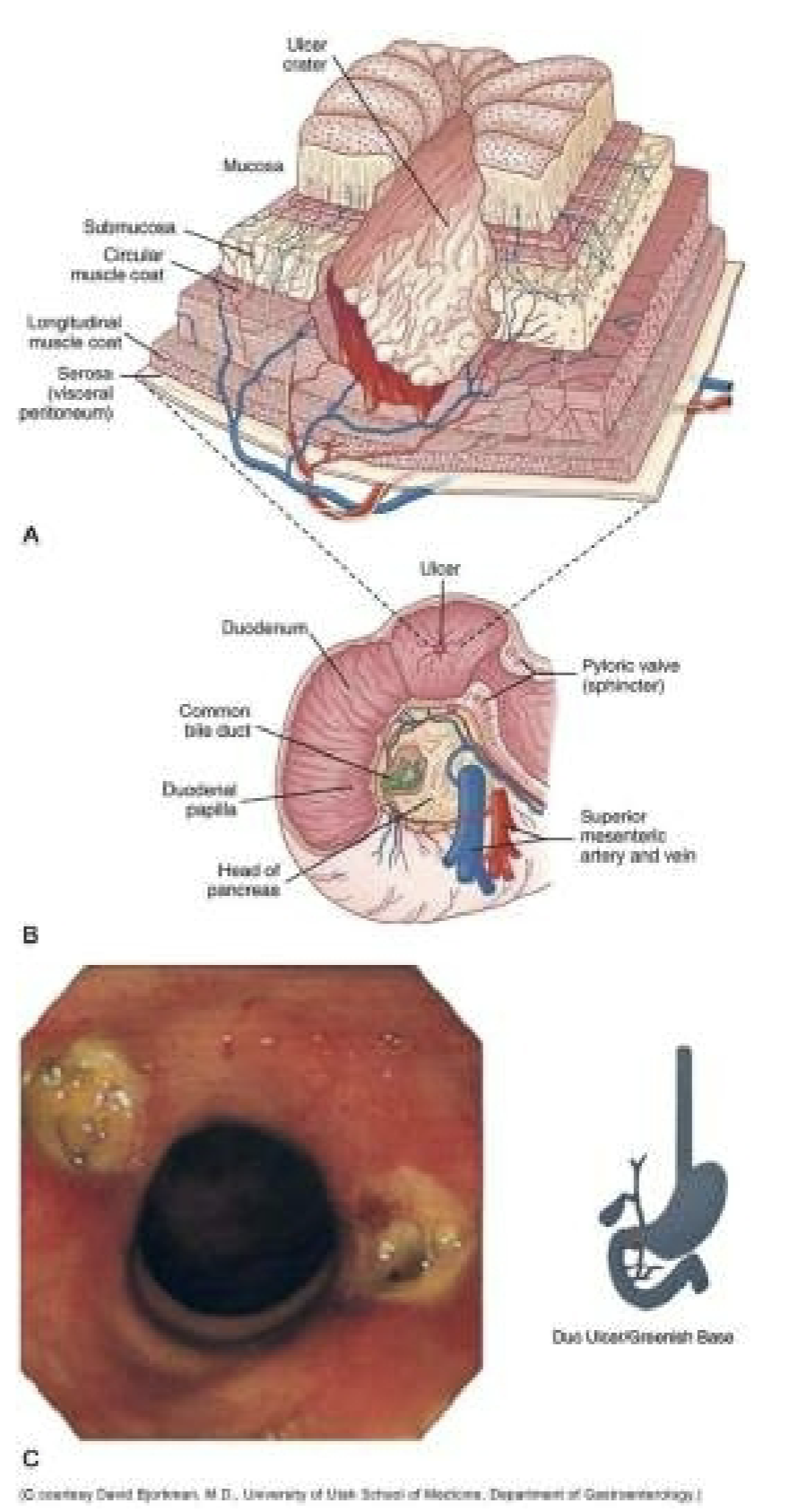
gastric ulcer:
gastric ulcers tend to develop in the antral region of the stomach, adjacent to the acid secreting mucosa of the body
pathophysiology
characterized by an increase in concentration of bile salts that damages the mucosal barrier by permitting hydrogen ions to diffuse into the mucosa, where they disrupt permeability and cellular structure
gastric secretion tends to be normal or less than normal
malabsorption syndromes:
maldigestion
failure of the chemical processes of digestion
malabsorption
failure of the intestinal mucosa to absorb digested nutrients
maldigestion and malabsorption frequently occur together
lactase deficiency
inability to break down lactose into monosaccharides and therefore prevent lactose digestion and monosaccharides absorption
fermentation of lactose by bacteria causes gas (cramping pain, flatulence, etc.) and osmotic diarrhea
fat soluble vitamin deficiencies
vitamin a
night blindness
vitamin d
decreased calcium absorption, bone pain, osteoporosis, fractures
vitamin k
prolonged prothrombin time, purpura, and petechiae
vitamin e
uncertain
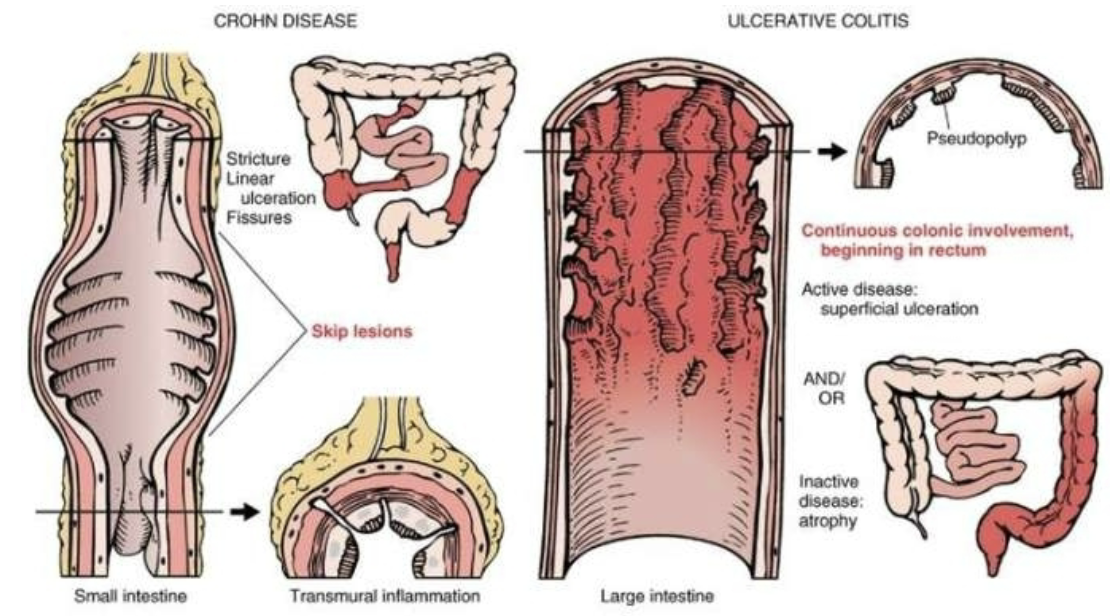
ulcerative colitis:
chronic inflammatory disease that causes ulceration of the colonic mucosa
sigmoid colon and rectum
suggested causes
infectious, immunologic (anticolon antibodies), dietary, genetic (supported by family studies and identical twit studies)
symptoms
diarrhea (10-20/day), bloody stools, cramping
treatment
broad spectrum antibiotics and steroids
immunosuppressive agents
surgery
an increased colon cancer risk demonstrated
appendicitis:
inflammation of the vermiform appendix
possible causes
obstruction, ischemia, increased intraluminal pressure, infection, ulceration, etc.
epigastric and rlq pain
rebound tenderness
the most serious complication is peritonitis
obesity:
obesity is an increase in body fat mass
body fat index > 30
a major cause of morbidity, death, and increased health care costs
risk factor for many diseases and conditions
hypothalamus- regulates eating behavior, energy metabolism, and body fat mass
hormones that control appetite and weight
insulin, leptin, peptide yy (decreases appetite by inhibiting nyp/agrp neurons), adiponectin, and resistin
ghrelin (stimulate apetide by activating nyp/agrp)
agouti-related protein stimulates eating and decrease metaboloism
leptin resistance- not responding to leptin
anorexia nervosa and bulimia nervosa:
characterized by abnormal eating behavior, weight regulation, and disturbed attitudes toward body weight, body shape, and size
anorexia nervosa is characterized by:
fear of becoming obese despite weight loss
underweight
can lead to starvation induced cardiac failure
bulimia nervosa is characterized by
recurrent episodes of binge eating with fears of not being able to stop eating
self induced vomiting
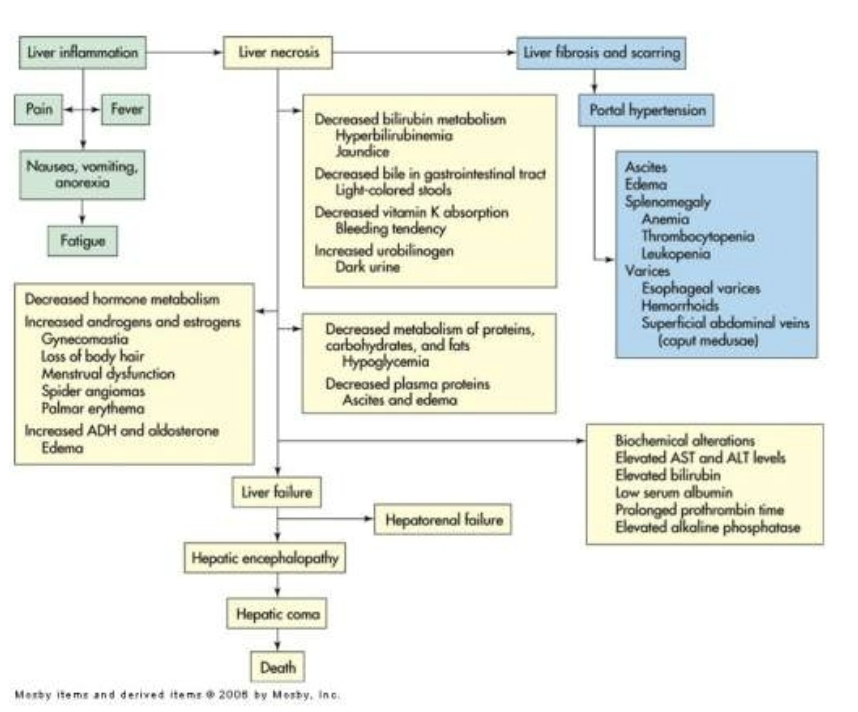
liver disorders:
portal hypertension
portal hypertension is abnormally high blood pressure in the portal venous system due to resistance to portal blood flow
the most common clinical manifestation of portal hypertension is esophageal bleeding
consequences
varices
lower esophagus, stomach, rectum
splenomegaly is an enlargement of the spleen
the most common manifestation of splenomegaly is thrombocytopenia
ascites- accumulation of fluid in the peritoneal cavity
impaired excretion of sodium by the kidneys promotes water retention
decreased oncotic pressure and increased hepatic sinusoidal hydrostatic pressure causes movement fluid into the peritoneal cavity
decreased blood flew to the kidneys activates aldosterone, which retains sodium
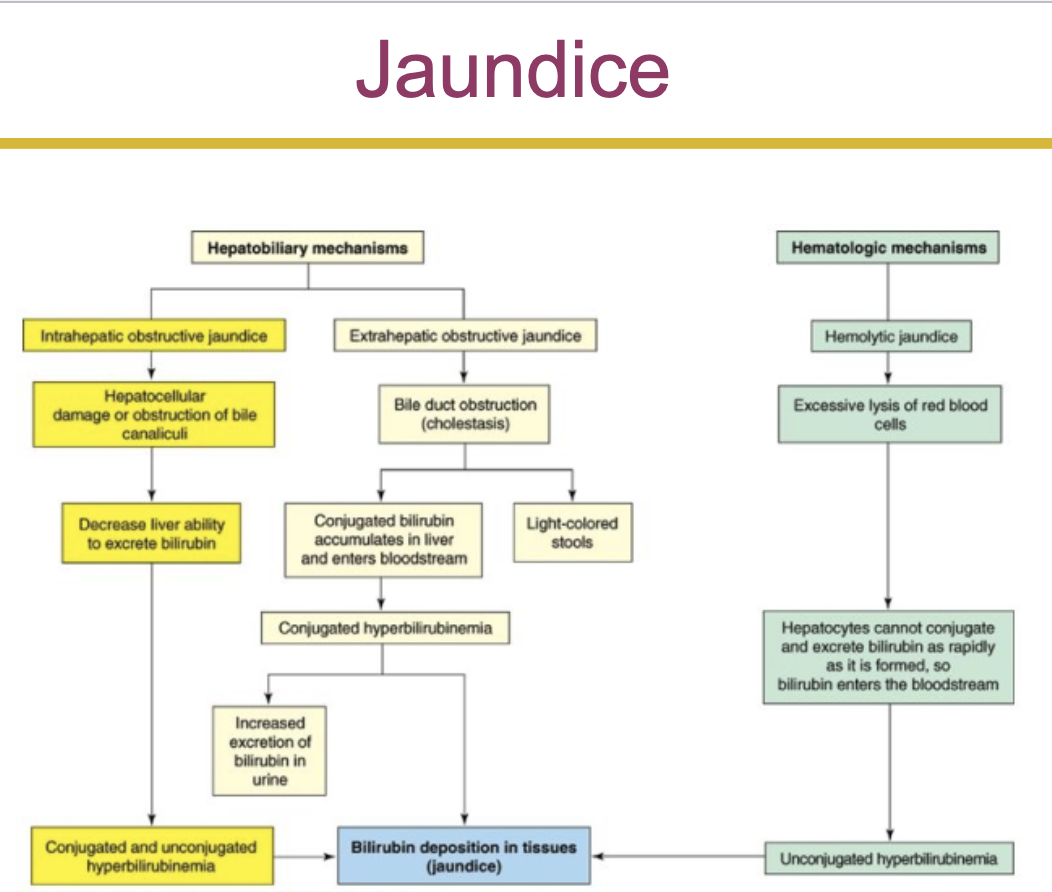
jaundice (icterus)
obstructive jaundice
extrahepatic obstruction
intrahepatic obstruction
hemolytic jaundice
prehepatic jaundice
excessive hemolysis of red blood cells or absorption of a hematoma
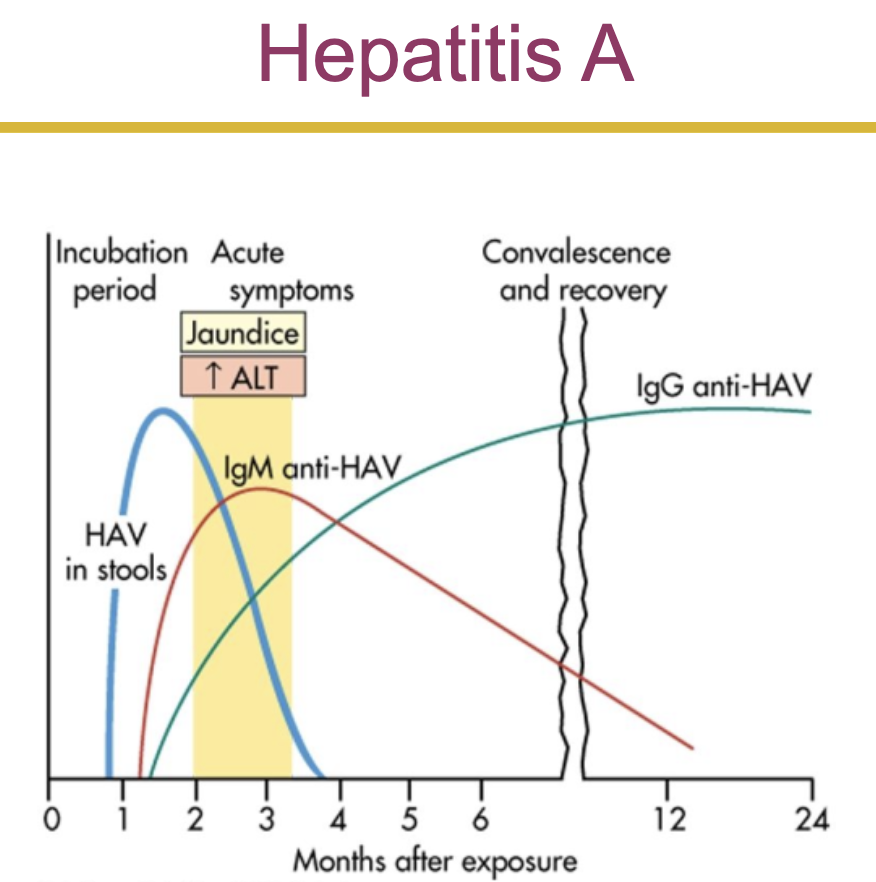
viral hepatitis:
systemic viral disease that primarily affects the liver
the early (prodromal) clinical manifestations of hepatitis are fatigue, fever, hyperalgia, and vomiting
types of hepatitis:
hepatitis a
formally known as infectious hepatitis
hepatitis b
formally known as serum hepatitis
hepatits c, d, e, and g
hepatitis a:
hepatitis a virus can be found in the feces, bile, and sera of infected individuals
usually transmitted by the fecal oral route
risk factors
crowded, unsanitary conditions
food and water contamination
hepatitis b:
transmitted through contact with infected blood, body fluids, or contaminated needles
maternal transmission can occur if the mother is infected during the first trimester
the hepatitis b vaccine prevents transmission and development of hepatitis b
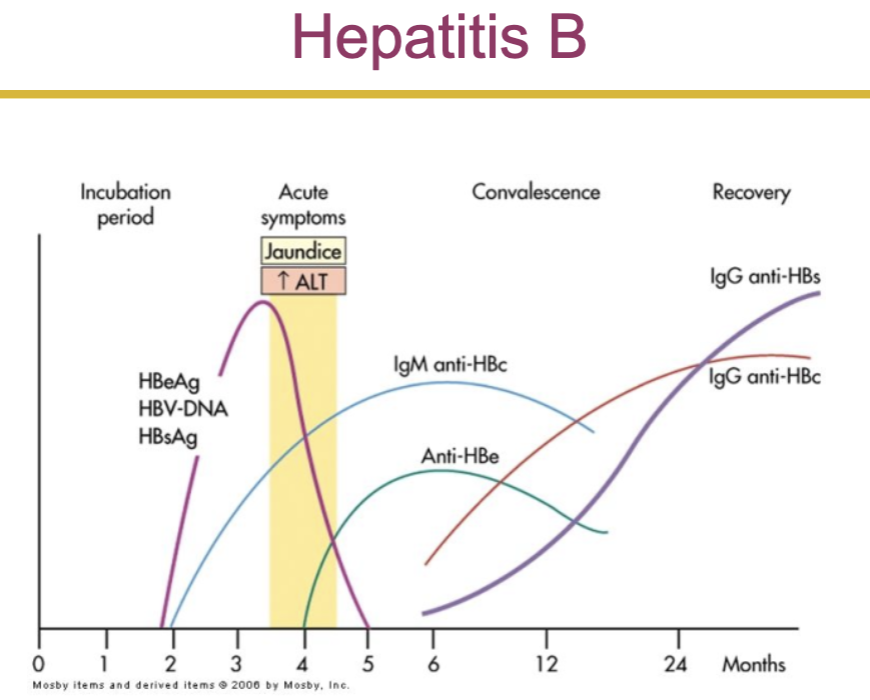
hepatitis:
sequence
incubation phase- varies (ex. for hep a its 30 days and for hep b its 60-180 days)
prodromal (preicteric) phase- when first symptoms appear after exposure
icteric phase- begins about 2 weeks after prodromal phase
recovery phase
cirrhosis:
irreversible inflammatory disease that disrupts liver function and even structure
decreased hepatic function due to nodular and fibrotic tissue synthesis (fibrosis)
biliary channels become obstructed and cause portal hypertension. due to the hypertension, blood can be shunted away from the liver, and a hypoxic necrosis develops
alcoholic
the oxidation of alcohol damages hepatocytes
hepatic fat accumulation is seen in alcoholic cirrhosis
pathophysiology
alcohol is transformed to acetaldehyde, which promotes liver fibrosis
mitochondrial function is impaired, decreasing oxidation of fatty acids
acetaldehyde inhibits export of proteins from the liver
disorders of the gallbladder:
obstruction of inflammation (cholecystitis) is the most common cause of gallbladder problems
cholelithiasis- gallstone formation
types
cholesterol (most common) and pigmented (cirrhosis)
risks
obesity, middle age, female, native american ancestry, and gallbladder, pancreas, or ileal disease
disorders of the pancreas
pancreatitis
inflammation of the pancreas
associated with several other clinical disorders
caused by an injury or damage to pancreatic cells and ducts, causing a leakage of pancreatic enzymes into the pancreatic tissue
these enzymes cause autodigestion of pancreatic tissue and leak into the bloodstream to cause injury to blood vessels and other organs
pathophysiology
pancreatic acinar cells metabolize ethanol, which generates toxic metabolites
injury to the pancreatic acinar cells permit leakage of pancreatic enzymes, which digest pancreatic tissue
when gallstones are present, bile flows into the pancreas contributing to attacks
manifestations and evaluation
epigastric pain radiating to the back
fever and leukocytosis
hypotension and hypovolemia
enzymes increase vascular permeability
characterized by an increase in a patients serum amylase level
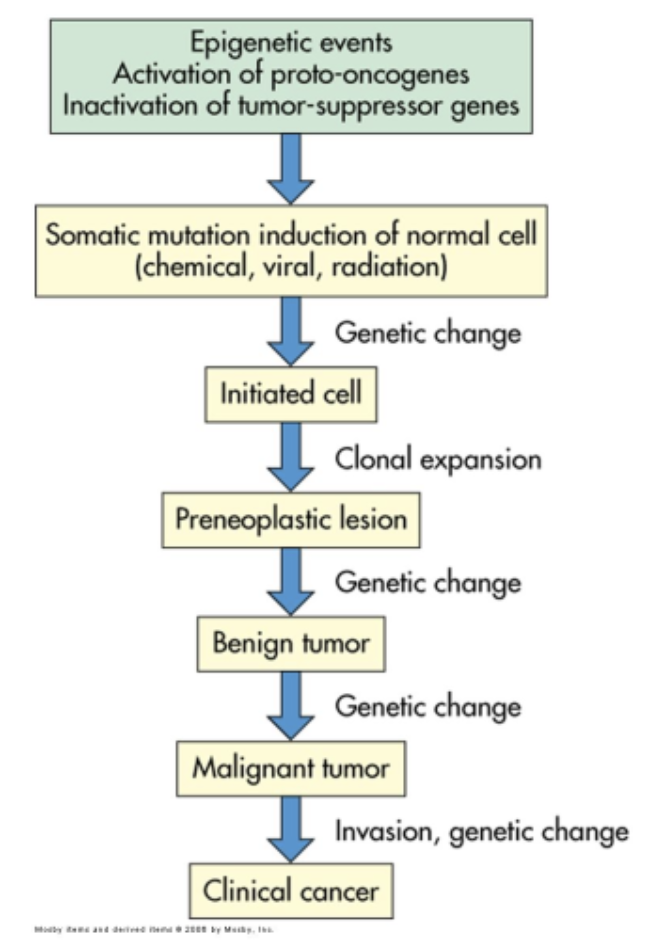
cancer of the gastrointestinal tract:
in gi tract cancer mutation of p53 gene occurs
esophagus
stomach
colon and rectum
liver
gallbladder
pancreas
colon cancer:
manifestation
mahogany colored blood mixed with stool
pain
anemia