Lecture 11_Muscles-1 Copy
Chapter 9: Muscles & Muscle Tissues
Muscle Tissue
Comprises nearly half of the body's mass
Converts chemical energy (ATP) into directed mechanical energy, exerting force
Three types of muscle:
Skeletal Muscle
Cardiac Muscle
Smooth Muscle
Prefixes related to muscle: myo, mys, and sarco
Types of Muscle Tissue
Skeletal Muscle
Attached to bones and skin
Composed of elongated cells known as muscle fibers (or skeletal muscle cell) that are striated in appearance and under voluntary control, allowing for conscious movement.
Features:
Striated (striped appearance)
Voluntary (under conscious control)
Contracts rapidly, tires easily, exerting power
Requires nervous system stimulation for contraction
Cardiac Muscle (Myocardium)
Exclusive to the heart, forming the bulk of its walls
Characteristics:
Striated
Can contract without nervous system stimulation
Involuntary
Smooth Muscle (Visceral)
Found in walls of hollow organs (e.g., stomach, urinary bladder, airways)
Characteristics:
Not striated
Can contract without nervous system stimulation
Involuntary muscle type, such as smooth muscle, plays a crucial role in various bodily functions, including digestion and blood vessel regulation.
Special Characteristics of Muscle Tissue
Excitability (Responsiveness): Ability to receive and respond to stimuli
Contractility: Ability to shorten forcibly when stimulated
Extensibility: Ability to be stretched
Elasticity: Ability to recoil to resting length
Muscle Functions
Primary Functions
Movement of bones or fluids (e.g., blood)
Maintaining posture and body position
Stabilizing joints
Heat generation (especially via skeletal muscle)
Additional Functions
Protects organs
Forms valves
Controls pupil size
Causes "goosebumps" by contracting the arrector pili muscles, which are small muscles attached to hair follicles.
Skeletal Muscle Structure
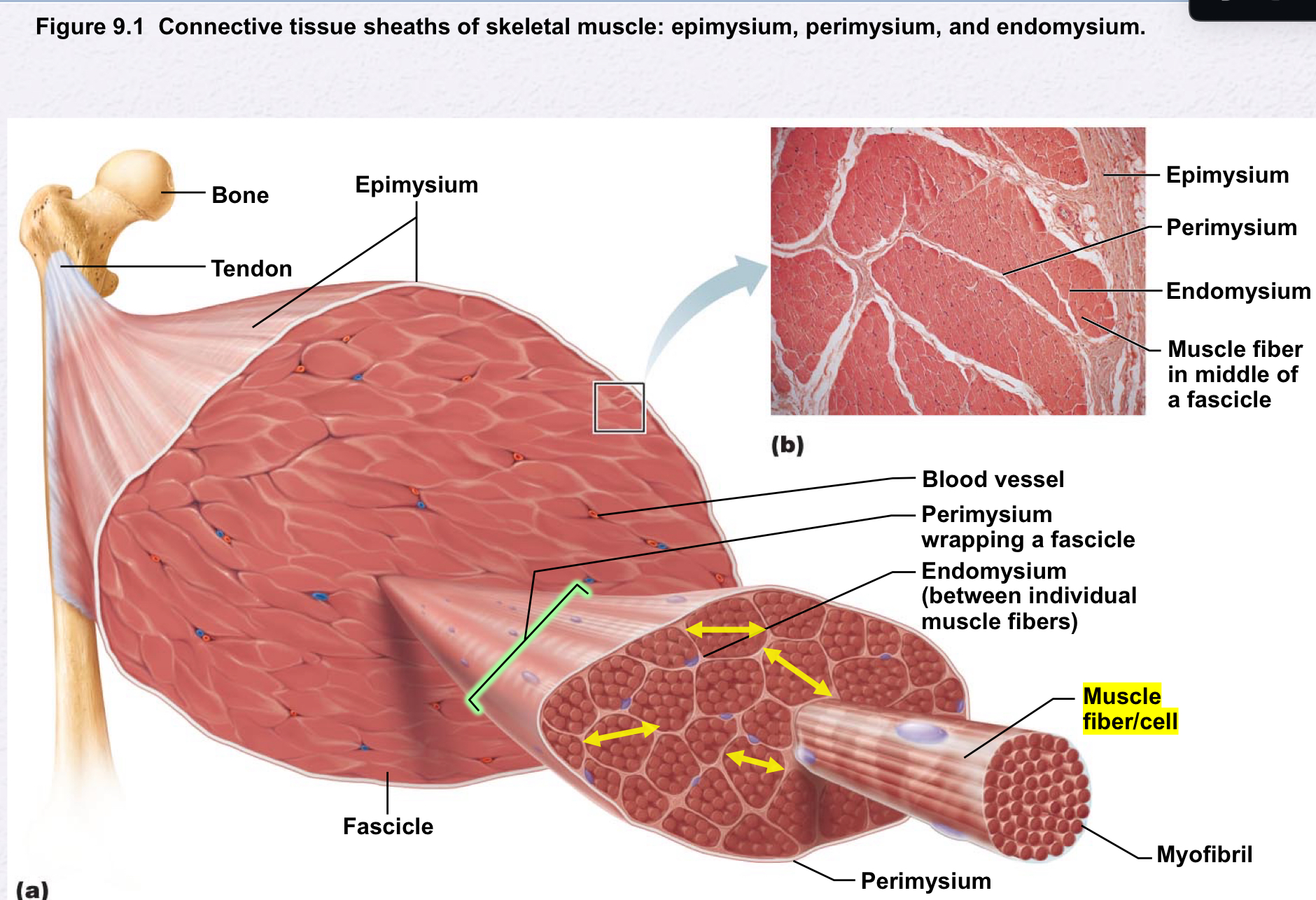
Connective Tissue Sheaths of skeletal muscle consist of three layers: epimysium, perimysium, and endomysium, which encase the muscle fibers and help transmit the force generated during contraction.
Support cells, reinforcing the overall muscle structure:
Epimysium: Dense irregular connective tissue surrounding the entire muscle, may blend with fascia
Perimysium: Fibrous connective tissue surrounding each fascicle (groups of muscle fibers)
Endomysium: Fine areolar connective tissue surrounding each muscle fiber
Microscopic Anatomy of a Skeletal Muscle Fiber
Long cylindrical cell
Diameter: 10 to 100 µm; Length: up to 30 cm
Contains multiple peripheral nuclei
Sarcolemma: Plasma membrane of skeletal muscle fiber
Sarcoplasm: Cytoplasm of a muscle fiber, which contains myofibrils, organelles, and various proteins essential for muscle contraction.
Glycosomes: Glycogen storage
Myoglobin: Oxygen storage
Modified structures: Myofibrils, sarcoplasmic reticulum, T tubules
Myofibrils
Rod-like elements densely packed within muscle fibers
Comprise ~80% of cell volume
Contain sarcomeres, the functional contractile units of skeletal muscle cells
Exhibit striations - perfectly aligned repeating series of
(dark )A bands and light (I bands).
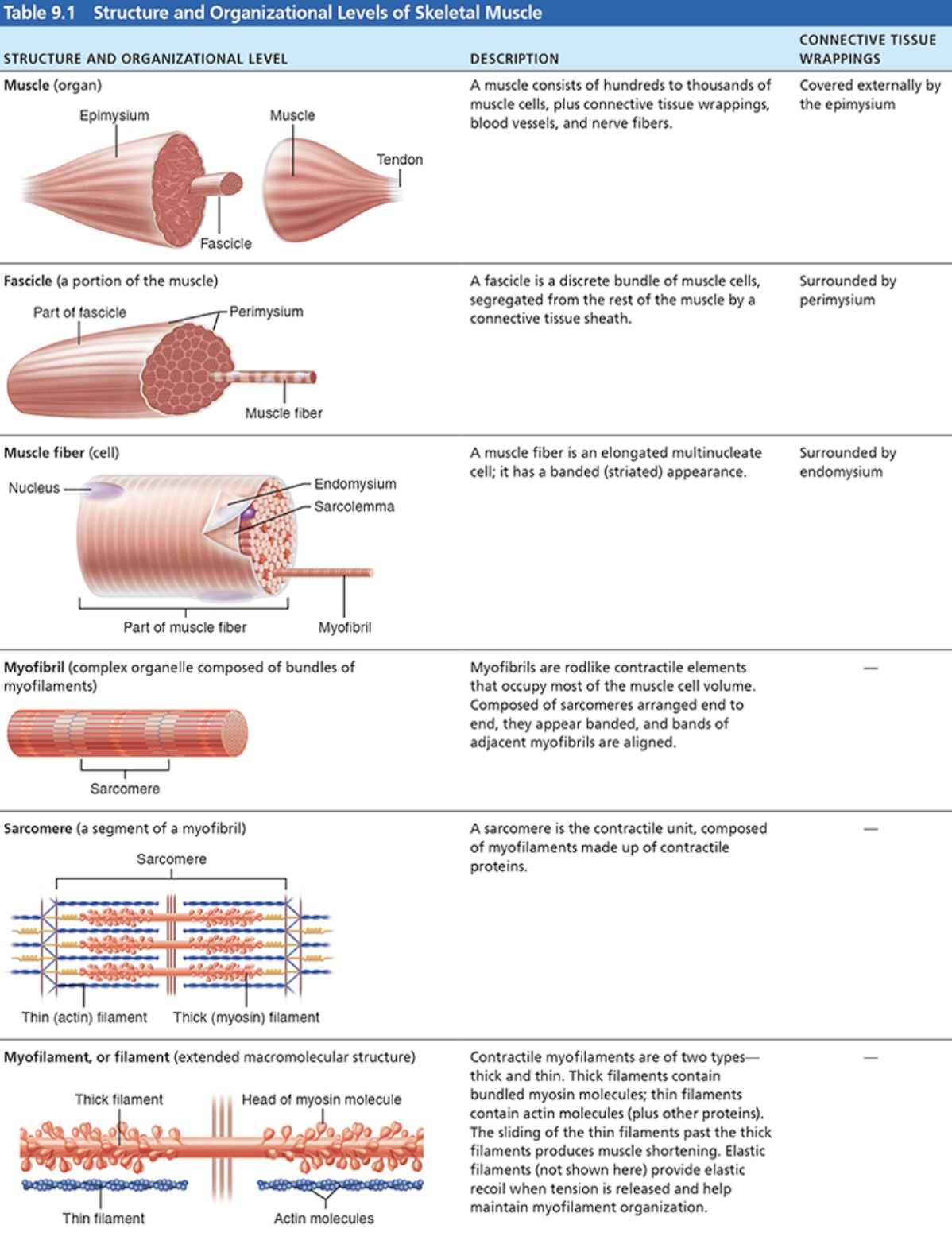
Structural Components of Sarcomere
Sarcomere: smallest contractile unit of muscle fiber(cell), responsible for muscle contraction through the interaction of thick and thin filaments.
1.Thick Filaments-Myosin
Composed of protein myosin - tails and heads.
Myosin heads create cross bridges during contraction
Binding sites for Actin of thin filaments; binding sites for ATP.
2.Thin Filaments- Actin
Twisted double strands of actin protein; has active sites for myosin head attachment during muscle contraction.
Tropomyosin and Troponin- regulatory proteins bound to Actin:
These proteins play a crucial role in the contraction process by controlling the access of myosin to the active sites on actin, thereby regulating muscle contraction and relaxation.
Elastic Filaments:These filaments composed of the protein Titin the thick filaments in place and provide elasticity to the muscle, allowing it to stretch and recoil during contraction; resists excessive stretching.
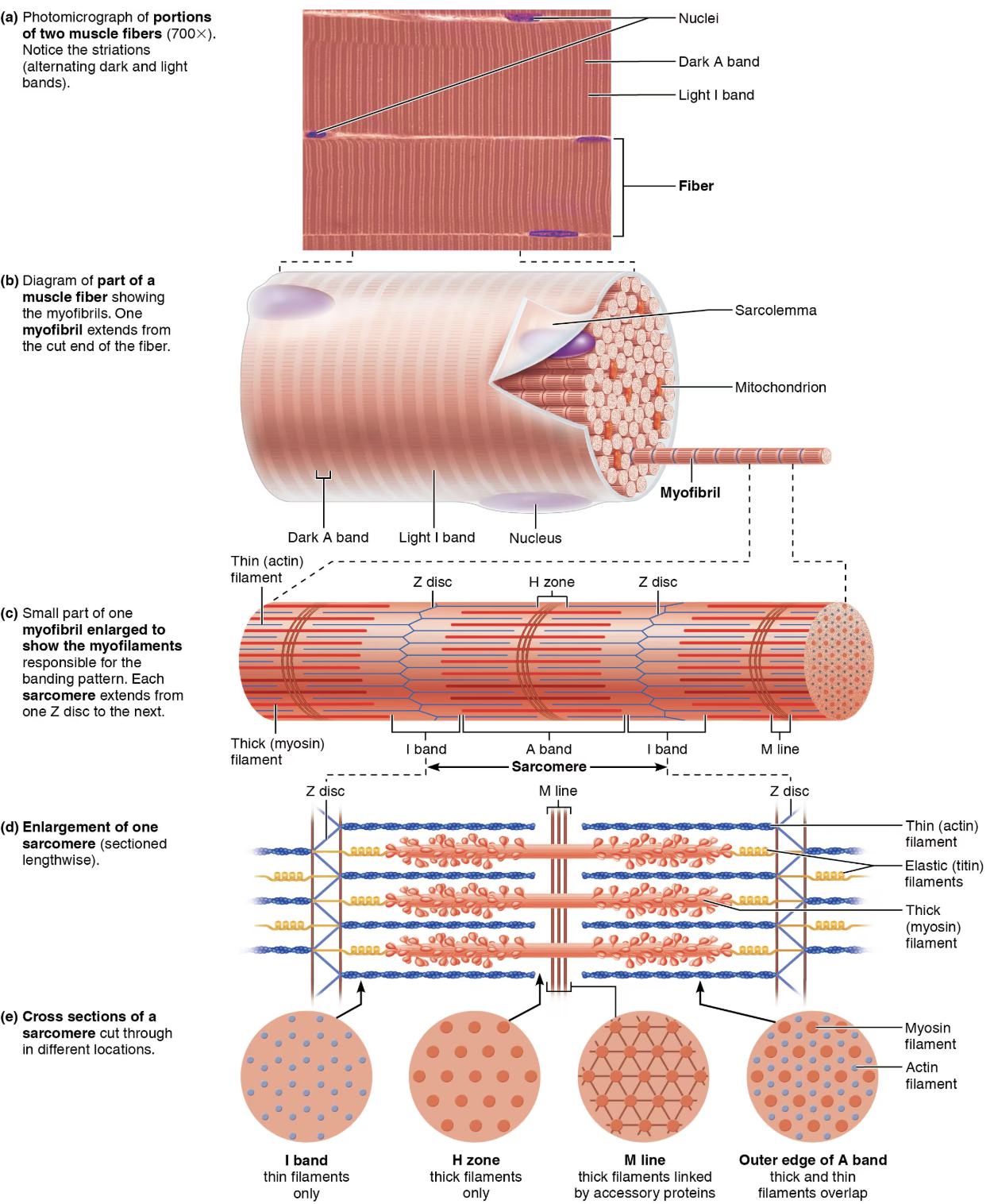
Striations
H zone: Lighter region in the midsection of the dark A band where no filaments overlap.
M line: line of protein myomesin bisecting the H zone.
Z discs: anchoring sites for thin filaments, connecting myofibrils
Sarcomeres :are segments between two successive Z discs. Contains A band with ½ I band at each end:
Myosin myofilaments: run entire length of an A band and connected to M line.
Actin myofilaments (Thin): run length of I band and partway into A band.
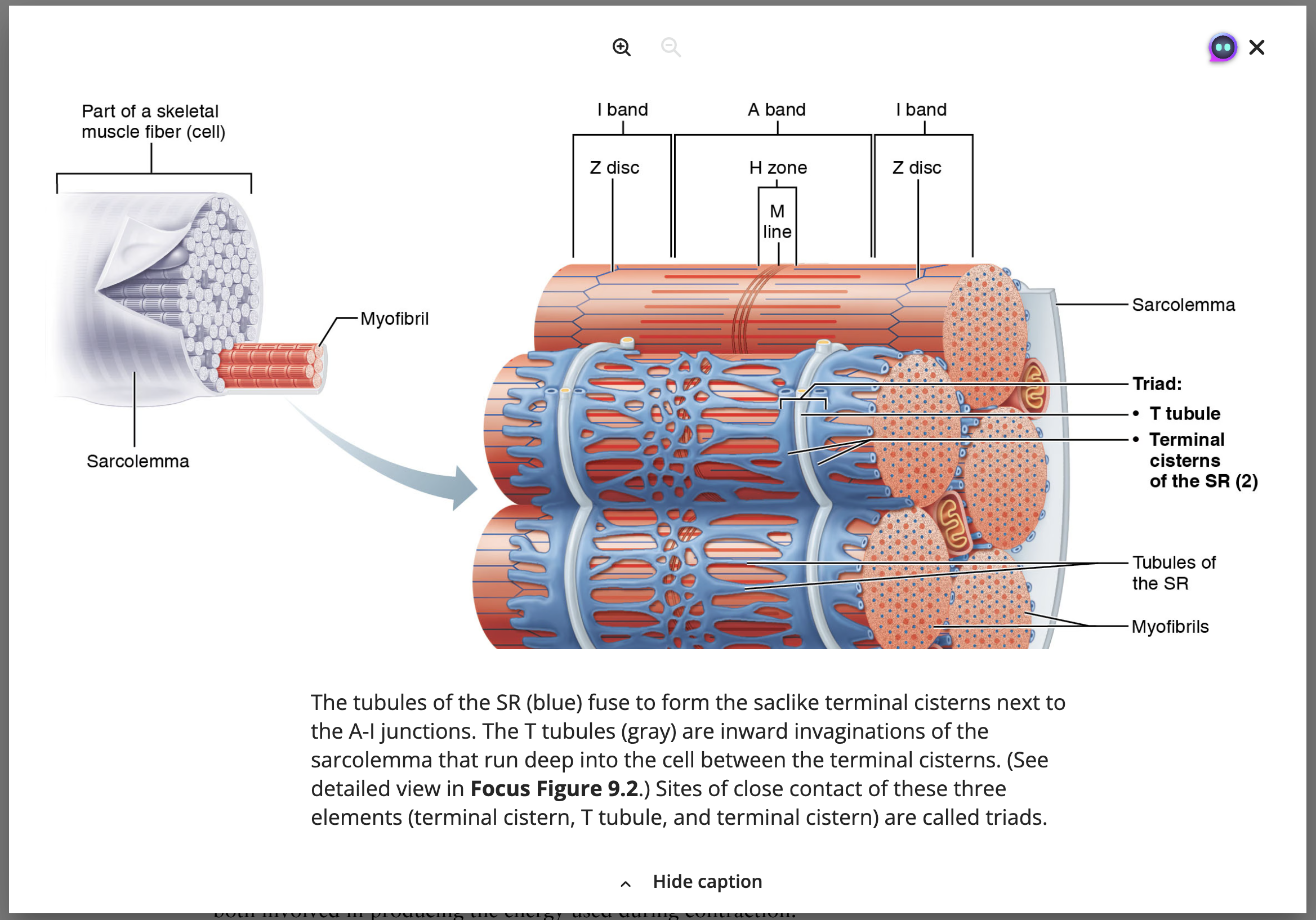
Sarcoplasmic Reticulum (SR) [modified endoplasmic reticulum]
Network of smooth endoplasmic reticulum surrounding each myofibril.
Most run longitudinally.
Pairs of terminal cisterns form perpendicular cross channels.
Functions in regulation of intracellular calcium levels, facilitating muscle contraction and relaxation. This structure is essential for maintaining the necessary calcium ion concentration required for effective muscle fiber function.
Stores and releases Ca2+.
T (transverse) Tubules
Continuation of Sarcolemma
Sarcolemma: The cell membrane of a muscle fiber, which plays a crucial role in action potential propagation and is involved in the uptake and release of calcium ions during muscle contraction.
Lumen continuous with extracellular space ?
Penetrate cell’s interior at each A band - I band junction.
Associate with paired terminal cisterns to form triads that encircle each sarcomere.
Triad Relationships
T tubules conduct impulses deep into muscle fiber (every sarcomere), ensuring that the entire muscle cell contracts simultaneously by triggering the release of calcium ions from the terminal cisterns.
Integral proteins protude into intermembrane space from T tubule and SR (sarcoplasmic reticulum) cistern membranes and connect with each other.
T tubule integral proteins act as voltage sensors and change shape in response to voltage changes.
SR integral proteins are channels that release Ca2+ from SR cisterns when voltage sensors change shaper.
Slidnig Filament Model of Contraction
Generation of force.
Shortening occurs where tension by cross bridges on thin filaments exceeds forces opposing shortening.
During contraction, Actin(thin) filaments slide past Myosin (thick) filaments, resulting in increased overlap
Myosin heads bind to actin; sliding begins forming cross bridges.
Cross bridges form and break several times, ratcheting thin filaments toward center of sarcomere which results in shortening of the muscle fiber.
This process is known as the sliding filament theory, which explains how muscle contraction occurs at the molecular level.
Changes:
Pulls Z discs toward M line.
I bands shorten.
Z discs closer.
H zones disappear.
A bands move closer but length stays the same.
Muscle Fiber Contraction Physiology
Activation (at neuromuscular junction, somatic division)
Must be nervous system stimulation.
Must generate action potential in sarcolema (called end-plate potential), which then triggers the release of calcium ions from the sarcoplasmic reticulum, leading to muscle contraction.
Excitation-Contraction Coupling:
Action potential propagates along the sarcolemma, increasing intracellular Ca2+ levels briefly.
Cross bridge formation between Actin and Myosin heads occurs, allowing the myosin heads to pull on the actin filaments, resulting in muscle shortening and contraction.