Essential of cardiopulmonary physiotherapy chapter 1
The cardio vascular system
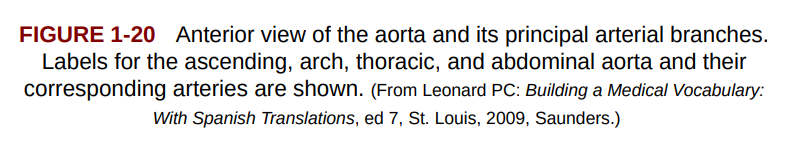
Mediastinum
lies between RG and LF pleura of the lungs
located in the sagittal plane of the chest
it extends from sternum to vertebral column (anterior view)
It contains all thoracic viscera except lungs
central compartment of thoracic cavity
It contains e heart, the great vessels of the heart, esophagus, trachea, phrenic nerve, cardiac nerve, thoracic duct, thymus, and lymph nodes of the central chest.
Heart
pump that circulates the blood in the vascular system
size of a fist, located obliquely un the mediastinum
Superior portion: “base of the heart“ = 2 artrias
broad portion
in adults located at the level of 2nd intercostal space
Inferior portion: “apex“
defined by the tip pf the left ventricle
extends to the 5th intercostal space at midclavicular line
Movement of the heart
it moves freely
it changes position during contraction, relaxation phase and during breathing
Contraction = it moves anteriorly and it moves towards chest wall
“point of maximum impulse“ (PMI) = portion of the heart that strikes the chest wall (apex)
Ventilation
normal breathing doesn’t alter heart PMI
deep inspiration → significant inferior depression of diaphragm → Heart goes lower and rotates to the right (displaces PMI)
Note:
PT with LF ventricular hypertrophy → PMI more lateral due to increase in ventricular mass
PT with pneumothorax → mediastinal shift, PMI changes
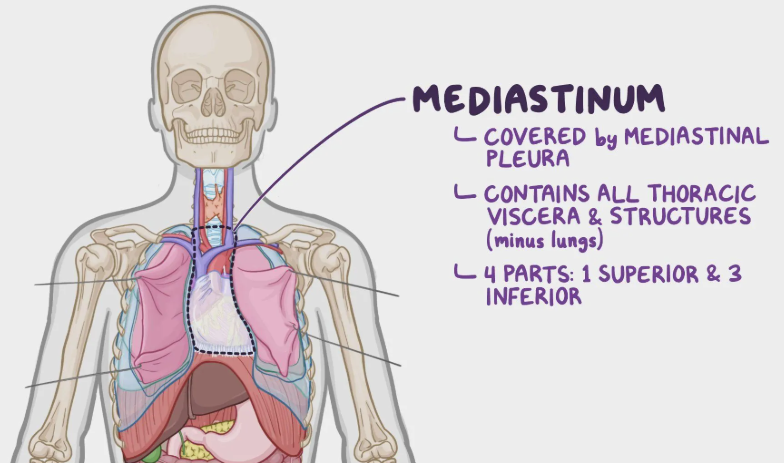
Tissue layers
Heart wall made oof 3 tissue layers
1) pericardium = outer layer
anchored to diaphragm inferiorly and the connective tissue of great vessel superiorly
There are 2 layers of pericardium
outer parietal pericardium
tough, fibrous dense layer
irregular connective tissue
inner visceral pericardium (epicardium)
thin, smooth and moist serous layer
Between these 2 layer there is a space called “pericardial space or pericardial cavity“
this cavity id filled with “pericardial fluid“ (10 to 20 mL)
Function: minimize friction during cardiac contraction
PT with inflammation of the pericardium (pericarditis)
fluid might accumulate in the pericardial space → cardiac tamponade
might happen after by coronary pass surgery or coronary artery bypass grafting procedure
2) Myocardium
middle layer
function: facilitates pumping function due to contractile elements
Myocardial cells → 3 traits
1) automaticity: the ability to contract in the absence of stimuli
2) rhythmicity: the ability to contract in a rhythmic manner
3) conductivity: the ability to transmit nerve impulses
These myocardial cells are organized into 2 groups based on their function
“myocytes“ mechanical cells → mechanical contraction
large cells, contain myosin myofilaments, many mitochondria to produce ATP (because heart can’t stop won’t stop until it decides to do so)
the myocytes are joined together by:
“syncytium“ conductive cells → electrical conduction
protoplasm of one cell is continuous with that of adjecent cells (aka they hold hands)
they create junctions that allows electrical flow and it spreads to one cell to the other
the junctions work together through a “low resistance pathway“
Note:
if myocardial cells die it cannot be replace, the death of these cells affects the contractile function
3) Endocardium
innermost layer of heart
made of endothelium overlaying a thin areolar tissue layer
it forms the inner layer of the chambers and has similar tissue of vessels and valves
Endocarditis (aka infection of this tissue) → because its similar to the one of vessels and valves, the infection can spread → it develops “vegetation“ (aka something growing in there that shouldn’t be growing there)
therefore, in PT with this condition, it is not suggested to perform Bronchopulmonary hygiene procedure (treating PT as empty ketchup bottle) because it can move the vegetation and it can transform in an emboli and then PT gets a stokes (we don’t want the ketchup to move from there)
Chambers of the heart
Heart is divided in right and left valves
they are divided by a “longitudinal septum“
Right side → receives deoxygenated venous blood (returning from the body)
Left side → receives oxygenated blood (returning from the lungs)
Each side (R/L) has 2 chambers
atria (superior side)
ventricle (inferior side)
THEREFORE
heart has 2 side, each side has 2 chambers → 4 chambers in total (math ++)
* looking further specifically into Right and left chambers * → PTSD from 1st year block 1.1
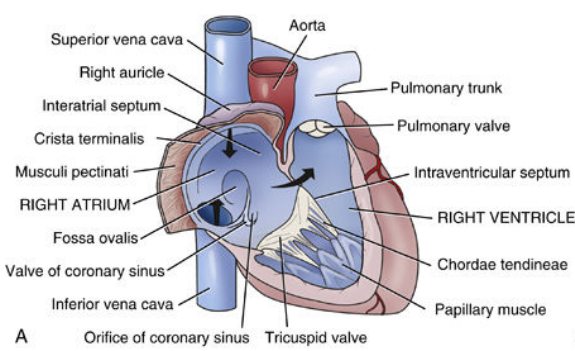
Right atrium
located at the top right side
smooth posterior and medial inner wall
it receives DEOX blood from 3 major blood vessels
superior vena cava (blood from UPPEX)
inferior vena cava (blood from LOWEX + trunk)
coronary sinus (blood from heart) → through the “tricuspid valve“
Normal diastolic pressure (central venous pressure) = 0 - 8 Hg
Pectinate muscle bundles exit anteriorly and laterally
the contraction of these muscles is 15%-20% of cardiac output (known as “atrial kick“)
RA has “auricles“ (earlike extensions) → they increase volume in the chamber (Left atrim has them too)
Note:
in PT with abnormal electrical conduction → atrial fibrillation
contract ability of pectineal muscles is reduced
this results in a low “atrial kick“ (= less cardiac output)
Question: In AF PT, because CO is reduced, does the heart beat faster to compensate?
Right ventricle
located at lower right side
shaped like a triangle
Function → ejects large volumes of blood through a small valve into “low pressure pulmonary system”
Blood comes from right atrium to right ventricle through “tricuspid atrioventricular valve“
one-way valve
located between right atrium and right ventricle
After the right ventricle is full, it ejects the blood into lungs through “pulmonic semilunar valve“ into the pulmonary artery
The right ventricle has 2 parts
“body“ → posteroinferior inflow tract
body = tricuspid valve + chordae tendineae + papillary muscles + trabeculated myocardium
“infundibulum“ → anterosuperior outflow tract
pulmonary trunk arises here
There are 4 muscular bands that separates inflow - outflow portion of RV:
infundibular septum
parietal band
septal band
moderator band
pressure in the RV
lower than left ventricle
diastolic pressure: 0 to 8 Hg
systolic pressure 15 - 30 Hg
Note:
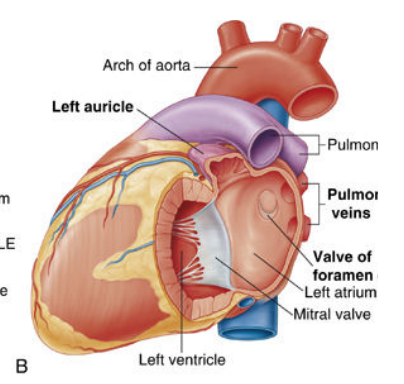
Left atrium
divided from right atrium through “interatrial septum“
located in the superior left side
it has a thicker wall to adapt to the higher pressures of blood entering the chamber from the lung
OXY Blood from lungs enters LA posteriorly through “Pulmonary veins“
these vessels have NO VALVES
BUT pectineus muscles extend from atria to pulmonary veins to prevent backflow of blood during contraction of atria
Pressure in LA
filling pressure: 4 - 12 mm Hg
OXY blood ejected into Left ventricle through “mitral atrioventricular“ (BICUSPID) valve
Note:
regurgitation of mitral valve (LA - LV) → causes blood to accumulate in LA, and it elevates Atrial pressure
These elevated pressure can cause AF and blood clots (emboli) in LA
Left ventricle
located to left low side
longer and thicker than RV (walls are 3x thicker)
the chamber is “circular“
the R and L ventricles are separated by “intraventricular septum“
LV receives OXY blood from LA through mitral valve
It ejects blood into aorta through aortic valve to the peripheral vasculature system (aka body)
Pressure
Normal systolic pressure: 80 to 120 mm Hg
diastolic pressure 4 - 12 mm Hg
(because of these elevated pressure LV is the thicker chamber of the heart)
Note:
Pathological thickening of LV in PT with cardiovascular complications (a consequence of increase load).
hypertension
aortic stenosis
HR failure
It alters contractile ability and it reduces filling capacity, causing reduction in cardiac output
Question: again, how does the body adapt? does the heart rate increase due to less CO?
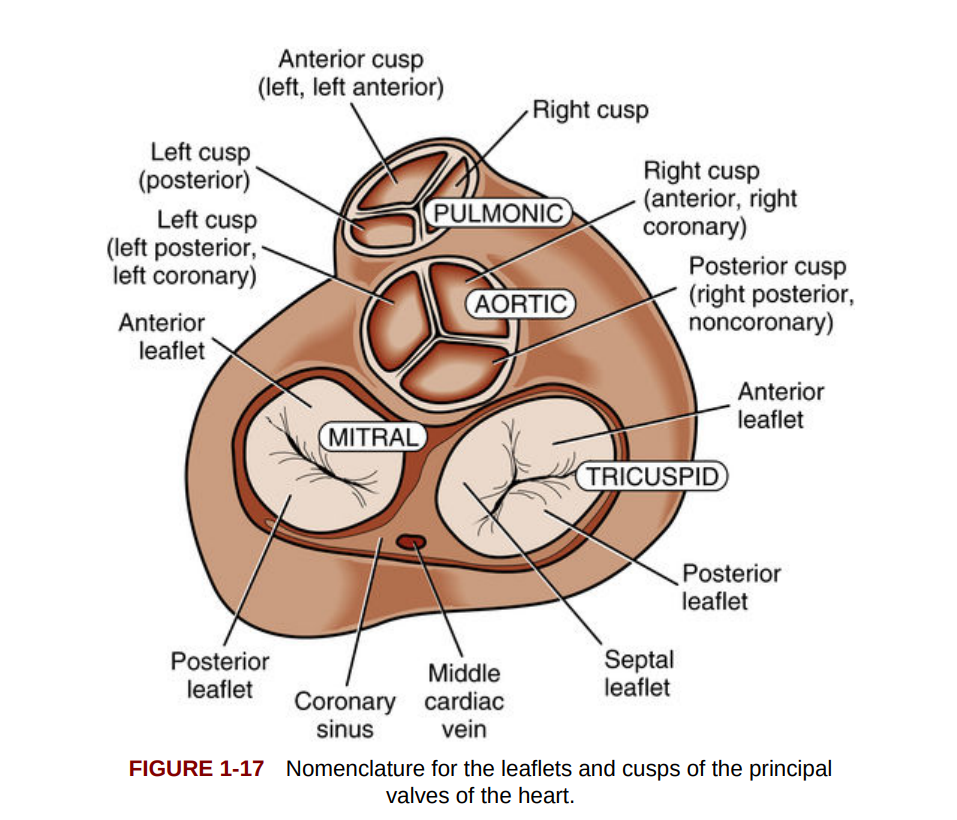
Heart valves
The heart has 4 valves
Function: they ensure the one-way blood flow through the heart
2 antrioventricular valves between atria and ventricle
Tricuspid valve on right side
bicuspid (mitral valve) on the left side
Role → prevent backflow of blood into the atria during ventricular contraction or systole
2 Semilunar valves are located between ventricles and arteries
pulmonic valve: right side (pulmonary artery)
aortic valve: left side (aorta)
Role → prevent backflow of blood from the aorta and pulmonary artery into the ventricles during diastole
Flaps of tissues called “leaflets“ or “cusps“ guard heart valves from opening
the right atrioventricular valve has 3 cusps, “tricuspid“
the left atrioventricular valve has 2 cusps “bicuspid“
Where are these cusps attached?
They are attached to the papillary muscles of the myocardium and the chordae tendineae.
What makes the valve open and close?
Opening and closing of each valve depends on the pressure changes within the heart created during each cardiac cycles
Note:
valvular function initial disturbance → auscultation “murmurs“ + echocardiography
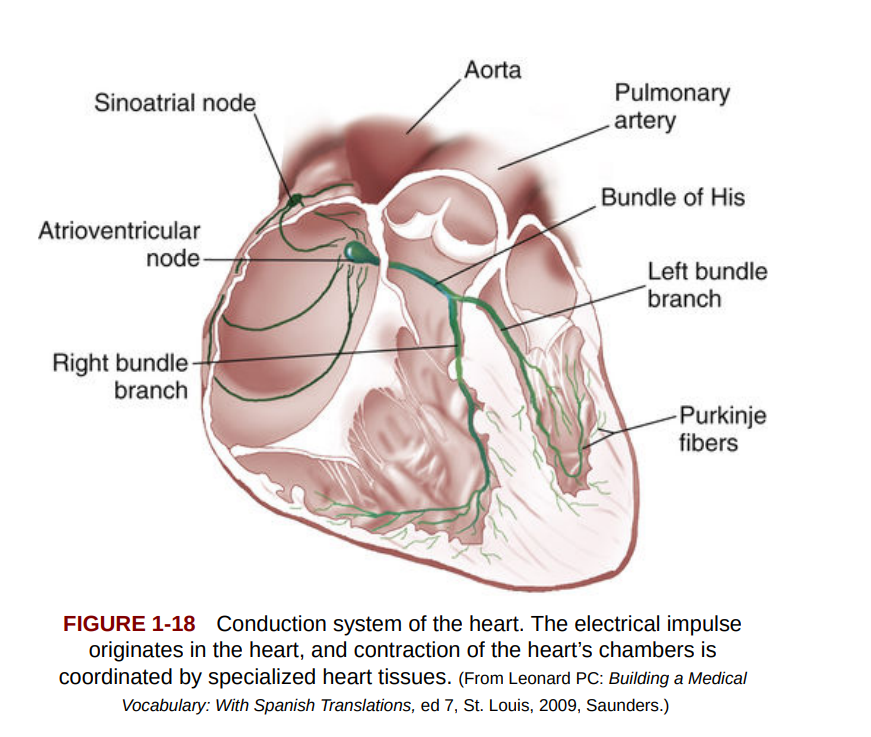
Conduction system
Electrical Impulse starts from SA node (sinoatrial / sinus node)
SA node located at the junction of the RA and superior vena cava
P cells of SA are the site for impulse generation
SA = Pace maker of heart (it creates the impulses)
Normal pace = 60 to 100 beats x minute (bpm) at rest
The impulse generated from SA goes down to 3 internodal tracts to the atrioventricular node (AV node)
The 3 conduction pathways are between SA and AV:
tract of Bachman
middle tract of Wenckebach
posterior tract of Thorel
The impulse travel through these 3 tract and it goes to AV node
AV node is located at the inferior aspect of RA, near the opening of coronary sinus and above tricuspid valve
AV function → slow down cardiac impulse through every cardiac cycle to allow mechanically the ventricle to fill
From AV node, the impulse goes to the “bundle of His“, this bundle bifurcates to carry the impulse to both right and left ventricle
right bundle branch (RBB) → thin, few branches that go towards the apex
left bundle branch (LBB) → it divides in 2 branches (posterior and anterior) and they go to aortic valve (A) and to the LV wall (P)
The bundle of his terminate into “Purkinje fibers“
network of nerve fibers
they extend from apex and expand to the outer myocardium
the electrical stimulation of these fibers cause the mechanical contraction of the ventricles
Innervation
cardiac plexus = sympathetic and parasympathetic fibers
located anterior to the tracheal bifurcation
cardiac plexus is innervated by vagus nerves and its branches innervates SA node and the other components of the conduction system
there is a sympathetic dominance in the functioning of the ventricles
Flight or fight response through the vagus nerve and the effects on the heart
The parasympathetic nervous system (vagal stimulation) slows down the heart and lowers blood pressure by releasing acetylcholine. (sleeping, relaxing)
On the other hand, the sympathetic nervous system speeds up the heart and increases blood pressure by releasing adrenaline (epinephrine) and norepinephrine. This makes the heart beat faster and stronger, helping the body respond to stress (the "fight-or-flight" response).
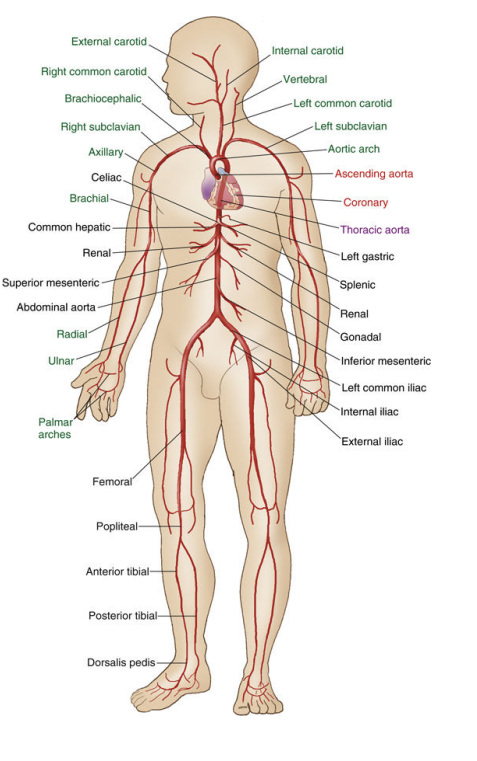
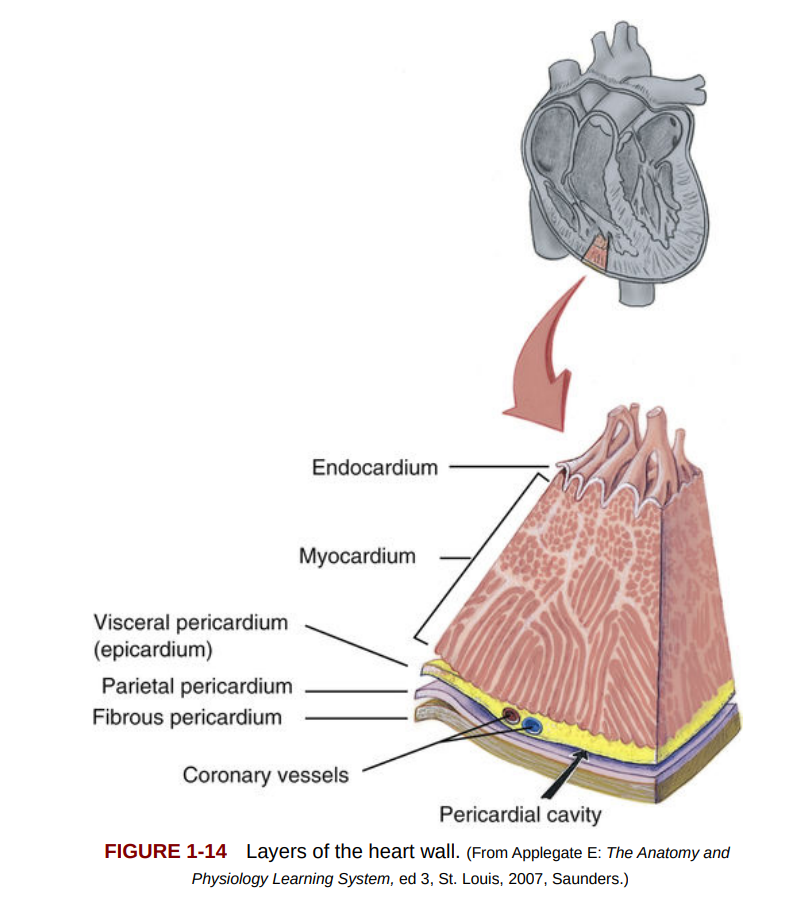
Cardiac and pulmonary vessels
Aorta
The ascending aorta starts at the left ventricle, is about 2 inches long, and moves upward and to the right.
It has three aortic sinuses (of Valsalva) where the coronary arteries originate.
Three branches arise from the aortic arch:
Brachiocephalic trunk
Left common carotid artery
Left subclavian artery
Blood enters the coronary arteries during diastole, when the aortic valve is closed.
Coronary Arteries
Right Coronary Artery (RCA)
Arises from the right side of the aorta and supplies the right ventricle, parts of the left ventricle, and the SA & AV nodes.
Gives off branches:
Sinus node artery
Right anterior ventricular branches
Right marginal artery
Posterior interventricular (posterior descending) artery
In 70% of cases, it supplies the AV node.
Left Coronary Artery (LCA)
Arises from the left side of the aorta and splits into:
Left Anterior Descending (LAD) artery: Supplies the front and septum of the left ventricle.
Circumflex artery: Supplies the side of the left ventricle and may give off the left marginal artery.
LAD supplies ~70% of the left ventricle.
Coronary Artery Occlusions & Infarctions
RCA occlusion → Causes inferior or posterior infarctions, affecting the SA node.
LAD occlusion → Causes anterior septal infarctions (widow maker).
Circumflex occlusion → Causes lateral infarctions.
Collateral circulation (angiogenesis) can develop in response to partial blockages.

Pulmonary Circulation
Pulmonary artery: Carries deoxygenated blood from the right ventricle to the lungs.
Splits into right and left pulmonary arteries.
Pulmonary veins: Carry oxygenated blood from the lungs to the left atrium.
Unlike systemic veins, they have no valves.
Venous Drainage of the Heart
Vena Cava:
Superior vena cava (3 inches long) drains the upper body.
Inferior vena cava drains the lower body.
Cardiac Veins: Drain blood from the heart into the right atrium.
Coronary sinus: Main drainage vein, empties into the right atrium.
Anterior cardiac veins: Drain the right ventricle directly into the right atrium.
Thebesian veins: Small veins found in all heart chambers, most numerous in the right atrium and ventricle.
Systematic circulation
Systemic Circulation Process
Oxygenated blood flows from the heart → aorta → systemic arteries → arterioles → capillaries.
Gas and nutrient exchange occurs in the capillaries.
Deoxygenated blood returns through venules → veins → right heart → lungs.
Blood vessels have three layers:
Tunica intima (inner)
Tunica media (middle)
Tunica adventitia (outer)
Arteries
Made of elastic and fibrous connective tissue with smooth muscle.
Two types of arteries:
Elastic arteries (e.g., aorta, pulmonary trunk):
Have more elastic fibers, allowing stretch and recoil to maintain blood pressure.
Muscular arteries (medium/small arteries):
Contain more smooth muscle, allowing vasoconstriction/vasodilation to regulate blood flow.
Controlled by the autonomic nervous system (α-receptors).
Arterioles: Smallest arteries with smooth muscle, regulating blood flow into capillary beds.
Capillaries & Endothelium
Capillary beds are dense in active tissues like muscles for efficient gas and nutrient exchange.
Endothelium (inner lining of blood vessels) plays roles in:
Filtration & permeability
Vasomotion (vessel contraction & relaxation)
Clotting & inflammation
Atherosclerosis starts with endothelial dysfunction, allowing fat and white blood cells to accumulate.
Veins
Thinner walls, larger diameter than arteries, with less elastic tissue.
Vein valves in the lower body prevent backflow.
Muscle pump activity helps move blood back to the heart.
Vein disorders:
Varicose veins: Occur when valves fail, leading to pooling.
Deep vein thrombosis (DVT): Forms due to prolonged inactivity, leading to blood clots.