AUBF-lec W4 Physical Examination of Urine
WEEK 3: PHYSICAL EXAMINATION OF URINE
- A method used way back in the early days of medicine
- Oldest clinical laboratory test as they only rely in physical/observable characteristics of urine
- Color, clarity, odor, taste are included
- Until now, it is still performed
- Continue to play an important role in Clinical Microscopy
FOUR PARTS OF ROUTINE URINALYSIS
- Specimen Evaluation
- Check label of specimen for any:
- Internal and external contamination.
- Requested test of doctor to be performed – can also be the reason whether to accept or reject the sample
- Transportation delay – whether sample is properly preserved. If not, reject
- Physical Examination – Physical or observable characteristics of urine.
- First examination to perform before chemical and microscopic examination. Follow the step-by-step
- The chemical and sediment examination can explain the findings of physical examination
- Ex: Physical Examination: Color Red
- Perform chemical examination (expect presence of blood)
- Microscopic/Sediment examination (Further confirm the presence of blood through visualizing it)
- Chemical Examination
- Sediment Examination
I. URINE COLOR
- Usually, the indicator of the degree of hydration
- Depends primarily on the body’s homeostasis and the degree of hydration
- Fluid intake is one to the reason whether urine color is lighter or darker
- Low fluid intake = darker urine color (concentrated) = higher amount of solute = increased specific gravity = dehydrated
- High fluid intake = lighter urine color (diluted) = lower amount of solute = decreased specific gravity = hydrated
- Signifies important disease processes since there are some abnormalities that changes in urine color
- Correlate/associate urine color with other parameters
- Usually, the specific gravity and clarity
- Normal: Colorless (straw) to Deep Yellow
- Normal urine color is yellow due to urochrome pigment
- Check urine color in a white background with sufficient light to assess/measure it correctly
- Abnormal: Red/Red-Brown (Most Common)
Recommendations for the Evaluation of Urine Physical Characteristics
- Use a well-mixed specimen
- View through a clear container – plastic or glass.
- View against a white background.
- Evaluate a consistent depth or volume of the specimen.
- View using room lighting that is adequate and consistent.
URINE PIGMENT
Urochrome (YELLOW)
- Product of endogenous metabolism – produces normally by our body during metabolic processes
- Constantly produced by the body and is excreted in the urine
- Major pigment (Yellow pigment)
- Actual amount of urochrome cannot be determined as it depends excreted or produced urochrome on our body’s metabolic state
- ↑ metabolism = ↑ urochrome
- ex. hyperthyroidism, starvation, fasting, and fever
- When doing intermittent fasting, urine color is much darker because more urochrome produced and excreted
- If patient has hyperthyroidism, increase thyroid hormones occur which also increase the metabolism = increase urochrome in urine
- It is a lipid-soluble pigment / Fat soluble
- Patient with renal disease, failure, or Chronic-Kidney Disease may not excrete urochrome
- The filtering capacity of kidney is damaged
- The urochrome will be deposited under the skin (subcutaneous fats) causing yellowish pigmentation of skin
- Urochrome can also be seen in plasma and serum
Uroerythrin (PINK)
- May deposit in amorphous urates and uric acid crystals
- Can be seen in crystal/sediments when prolonged standing, in a refrigerated sample, or when sample is centrifuged
- Has reddish or brick-red crystals
- Crystals only formed at acidic pH only
- Pinkish pigment
- Smaller in quantity compared to urochrome
- Does not always evident
- Has reddish or brick-red crystals
Urobilin
- Bi-product of urobilinogen metabolism
- Imparts an orange-brown color (or amber) of urine that is not fresh
- It is very evident if sample is unpreserved
- Found in old urine specimen due to oxidization or metabolism of urobilinogen
- When urine is fresh, it is colorless but when urobilinogen is oxidized, orange-brown color or amber color is present
FACTORS AFFECTING URINE COLOR
- The amount of the substance present
- More substance = more change in urine color
- Ex: Red color urine = too much blood present in urine
- However, it is possible to be positive in blood even it is not evident in urine
- More Urochrome = More yellow in urine color
- The urine pH
- Some pigments/substances when exposed to alkaline pH results darker color
- Ex: Alkaptonuria (melanin pigment gives dark brown color to the urine)
- Freshly voided urine (with melanin) can be seen in yellow color, but when in prolonged standing, it can give dark brown color
- In acidic pH, ingesting of blackberries can make urine color red
- The structural form of the substance
- Substances that when oxidized can cause changes in urine color
- Ex: Urobilinogen, once oxidized, can urobilin
- Bilirubin (orange) when oxidize can be converted to biliverdin can yield yellow-green color
LABORATORY CORRELATIONS URINE COLOR
- Change is urine color is not always pathologic process some are not clinically significant
- It is possible that there are variations of color due to ingested food or drug and etc.
- It can also indicate disease progress, excessive physical activity (exercise)
- Check the history and correlate urine result in other tests in the laboratory
Normal Urine Color
Depending on the amount of pigment found in urine
- Colorless / Straw – Recent fluid consumption
- Even if urine color is similar with water, it is okay if one is always drinking water/overhydrated.
- Normal urine color ranges from colorless to dark yellow depending on the amount of pigment present in the urine
- Pale yellow
- Dilute random specimen
- Having pale yellow urine color does not equate to being healthy
- Usually if one is experiencing Polyuria (increase urine output)
- Diabetes mellitus: increased/excessive glucose and water excretion
- Experiencing insulin problem which can be either non-responsive or deficient
- Excessive glucose will be excreted in urine
- In kidney filtration, we always maintain the osmolarity. Hence, if there is an excess solute present, water will be excreted
- Diabetes insipidus: deficiency in antidiuretic hormone
- Water will be excreted even the patient is already dehydrated
- Both has Increased water excretions
- More than 2 liters per day
- Both diabetes types suffer from polydipsia or the excessive thirst due to the increase of solute. Hence, causing polyuria
- If overhydrated = increase blood volume = changes in blood pressure
- Diabetes insipidus: deficiency in antidiuretic hormone
- Possibility of circulatory overload increase.
- Heart may be drowned sue to increase blood volume
- Dark Yellow
- Concentrated specimen or urine output due to increase metabolism
- Usually in the first morning specimen
- Depends on the increased urochrome
- Dehydration
- Strenuous exercise
Urine Color Chart
Urine Color | Possible Meaning |
Clear | Good hydration, overhydration, or mild dehydration |
Pale Yellow | Good hydration or mild dehydration |
Bright Yellow |
|
Orange, Amber | Moderate or severe dehydration |
Tea-Colored or Ice tea | Severe dehydration or burned patients |
- Make sure you are hydrated because if not, our body organs will not function well.
- Lesser fluid intake = lesser circulation of blood = increase blood pressure
Abnormal Urine Color
- Dark Yellow / Amber / Orange
- Presence of the abnormal pigment bilirubin
- Depending on the amount of bilirubin can cause the mentioned color
- Bilirubin came from the metabolization of the heme portion of hemoglobin in the liver
- If one has liver problem, an increase of bilirubin and yellow pigment on skin and eyes are expected due to its deposition in the skin
- Possible disease is Liver disease, hepatitis virus, and hemolytic anemia (destruction of RBC) (Must treat all sample as infectious)
- Bilirubin should be converted to urobilinogen in order for it to be excreted in feces and urine.
- If there is liver problem, bilirubin cannot be converted to urobilinogen. Thus, it can accumulate.
- It is water-soluble which can pass through glomerulus and be excreted through urine
- When checking the urine sample whether there is a presence of bilirubin and not oxidized to biliverdin, transportation and handling of specimen should be done properly
- Specimen must be placed in amber-colored container. If it is transparent, cover it with carbon paper to avoid artificial or natural light
- Bilirubin is photosensitive that when exposed to light it can be converted to biliverdin (has yellow green pigment)
- Make sure the bilirubin must not oxidize
Differentiation between Urobilin and Bilirubin
Urobilin | Bilirubin |
Shake specimen well | |
|
|
- Yellow-Green
- Biliverdin (photo-oxidation of bilirubin)
- Upon standing or improper storage, bilirubin may be oxidized to biliverdin
- Oxidation of bilirubin to biliverdin
- Yellow-Orange
- If patient’s specimen produces yellow foam but upon checking their history, they have no problem with liver or hemolytic anemia. MedTech must check for any interfering medication that causes the yellow/orange/amber urine color
- Phenazopyridine (Pyridium) or azogantrisin (produce a yellow foam when shaken)
- Treatment/drug for UTI
- Also interferes with chemical tests that are based on color reactions
- High consumption of food such as vegetables rich in beta carotene
- If urine color is dark or orange, it can interfere with the chemical examination since in the reagent strip test, there are super light-colored pads that when dip with dark urine or orange, it can change the result since chemical reagent strip testing is color-dependent reading.
- Red / Pink / Brown
- One of the most common causes of abnormal urine color
- Cause by the presence of blood (RBC) or hemolyzed RBC
- There is presence of hemoglobin or myoglobin.
- To differentiate Intact RBC from Hemoglobin and Myoglobin, Check for the clarity.
How to differentiate: check the clarity
- Intact RBC: cloudy red or pink
- Hemolyzed RBCs (both hemoglobin or myoglobin): clear red
- Myoglobin pigment is found in skeletal muscle
- To differentiate hemoglobin and myoglobin, perform plasma examination.
- Observed what will be the color of plasma
Plasma Examination Test | |
Hemoglobin | Myoglobin |
|
(Does not stay in plasma) |
- Myoglobin is used when checking hazing victim
- Hazing lead to muscle tissue destruction. Thus, the myoglobin is excreted from it.
- Blood may range from pink to brown, depending on:
- The Amount of Blood
- Too Much Blood is Present
- ↑ Blood = ↑ red color.
- ↓ Blood = ↓ color (pinkish)
- The pH of the Urine
- Alkaline environment = hemolyzed RBC (change in the color)
- The Length of Contact
- If sample is left undisturbed or prolonged standing, the hemoglobin (at first) is color red, but once oxidized, it will become brown (conversion of hemoglobin to methemoglobin)
- Oxidation Of Hemoglobin to Methemoglobin (Brown)
- Fresh Urine but Brown Color
- Glomerular bleeding
- Hemoglobin is oxidized in vivo
- Alkaline urine with red blood cell gives reddish brown in color
7. Port wine / Burgundy red / Purplish red
- Because of Porphyrins
- Oxidation of porphobilinogen
- Patients that have Porphyria
- Disorder; problem with Heme synthesis
- Increase in porphyrins (chemical build-up that changes the urine color)
- A hereditary/genetic disease
- Porphyrins, sometimes deposit on teeth
- Rusty color of teeth, mouth bleeding—reason why they are mistaken as vampires—cause also of their pale skin.
Non-Pathologic causes of Red urine color
Menstrual Contamination
- If urine has menstrual contaminants, ACCEPT it. But take note that you must include that the patient has menstruation upon release of test results.
Ingestion of Highly pigmented foods
- Due to diet; some foods contribute to the color pigment of urine.
Medications (Rifampin, Phenolphthalein, Phenindione, Phenothiazines)
- Such medications that change the color of urine.
- Patients with Tuberculosis (taking medications for anti-tuberculosis—Rifampin/Rifampicin)
- Highly pigmented fluid that makes all of your body fluids red (not just urine; sinovial fluid, cerebrospinal fluid, etc.,)
Genetically Susceptible Person (Eating fresh beets causes red color in alkaline urine)
- Beets are root crops 🡪 Produces red urine.
- Although, not all people who consume beets produces red urine color, only some individuals—and is hereditary.
Ingestion of Blackberries (Produces red color in acidic urine)
- When pigment of blackberries exposed to acidic urine causes red urine color.
8. Blue / Green
- Bacterial infections (Urinary tract infection)
- Usually caused by Pseudomonas aeruginosa
- P. aeruginosa capable of producing pyoverdine
- Intestinal tract infection (High pathologic bacteria in Gastrointestinal tract)
- Tryptophan (amino acid) that normally excretes by human through feces in the form of Indole)
- Bacteria converts the Indole to Indican—water soluble bluish/purplish substance)
- Indican 🡪 Indicanuria disorder (the more indican produced, the more pathologic bacteria)
- Ingestion of breath deodorizers
- Chlorophyl containing (Clorets, mouthwash)
- Chlorophyl substances causes greenish urine
- Phenol derivatives
- Medication (Blue)
- Methocarbamol (Robaxin)
- Methylene blue
- Amitriptyline (Elavil) – antidepressant
9. Purple
- Found in catheter bags (AKA Purple Bag Indole)
- Used for catheterized patients
- Increased Indican in urine (converted Indole)
- Bacterial infection
10. Brown / Black
- Methemoglobin (most common)
- Once blood left at room temperature, prolonged standing, and urine becomes alkaline 🡪 Hemoglobin will be oxidized becoming Methemoglobin
- Melanin
- Oxidation product of melanogen
- Water-soluble substance that excretes through urine
- Derived from melanocytes (from skin)
- Skin produces melanogen (colorless)
- Homogentisic acid
- Metabolite phenylalanine (Alkaptonuria) – means that they are produced in alkaline.
- Usually caused by in-born error of metabolism (rare genetic disorder)
- Since Alkaptonuria is an alkaline lover; when prolonged standing of urine, it becomes black because of homogentisic acid.
- Medications (Levodopa, Methylodopa, Phenol derivatives, Metronidazole)
Drug | Effect |
Levodopa | Cola-colored (may also because of myoglobin) |
Mepacrine (Atabrine) | Yellow |
Methyldopa (Aldomet) | Green-brown |
Metronidazole (Flagyl) | Darkening, reddish-brown |
Phenazopyridine (Pyridium) | Orange-red, acidic pH |
Rifampin | Bright orange-red |
Riboflavin | Bright yellow |
COLOR | CAUSE | CLINICAL/LABORATORY CORRELATTION |
Colorless | Recent fluid consumption | Commonly observed with random specimens |
Pale yellow | Polyuria or diabetes insipidus | Increased 24-hour volume and low specific gravity |
Diabetes mellitus | Elevated specific gravity and positive glucose test result | |
Dilute random specimen | Recent fluid consumption | |
Dark yellow | Concentrated specimen | May be normal after strenuous exercise or in first morning specimen |
B complex vitamins | ||
Dehydration | Fever or burns | |
Bilirubin | Yellow foam when shaken and positive chemical test results for bilirubin | |
Acriflavine | Negative bile test results and possible green fluorescence | |
Nitrofurantoin | Antibiotic administered for urinary tract infections | |
Orange-yellow | Phenazopyridine (Pyridium) | Drug commonly administered for urinary tract infections |
Phenindione | Anticoagulant, orange in alkaline urine, colorless in acid urine | |
Sulfasalazine (Azulfidine) | Anti-inflammatory drug | |
Yellow-green | Bilirubin oxidized to biliverdin | Colored foam in acidic urine and false-negative chemical test results for bilirubin |
Green | Pseudomonas infection | Positive urine culture |
Asparagus | None | |
Blue-green | Amitriptyline | Antidepressant |
Methocarbamol (Robaxin) | Muscle relaxant, may be green-brown | |
Clorets | None | |
Indican | Bacterial infections, intestinal disorders | |
Methylene blue | Fistulas | |
Phenol | When oxidized | |
Propofol | Anesthetic | |
Familial hypercalcemia | “Blue diaper syndrome” | |
Indomethacin (Indocin, Tivorbex) | Nonsteroidal anti-inflammatory drug | |
Pink Red | RBCs | Cloudy urine with positive chemical test results for blood and RBCs visible microscopically |
Hemoglobin | Clear urine with positive chemical test results for blood; intravascular hemolysis | |
Myoglobin | Clear urine with positive chemical test results for blood; muscle damage | |
Beets | Alkaline urine of people who are genetically susceptible | |
Rifampin | Tuberculosis medication | |
Menstrual contamination | Cloudy specimen with RBCs, mucus, and clots | |
Port wine | Porphyrins | Negative test for blood, may require additional testing |
Red-brown | RBCs oxidized to methemoglobin | Seen in acidic urine after standing; positive chemical test result for blood |
Myoglobin | ||
Brown Black | Homogentisic acid (alkaptonuria) | Seen in alkaline urine after standing; specific tests are available |
Malignant melanoma Melanin or melanogen | Urine darkens on standing and reacts with nitroprusside and ferric chloride | |
Phenol derivatives | Interfere with copper reduction tests | |
Argyrol (antiseptic) | Color disappears with ferric chloride | |
Methyldopa or levodopa | Anti-hypertensive | |
Metronidazole (Flagyl) | Darkens on standing, intestinal and vaginal infections | |
Chloroquine and primaquine | Antimalarial drugs | |
Methocarbamol | Muscle relaxant | |
Fava beans, rhubarb, or aloe | None |
II. URINE VOLUME
Renal Blood Flow | 1200 mL per minute |
Renal Plasma Flow | 600-700 mL per minute |
Normal Range of Urine (24 hours) | 600-2000 mL per day |
Average urine output for healthy individual (24 hours) | 1200-1500 per day |
Night-day ratio | 1:2 / 1:3 (more output release during the day because our body is more active) |
- Output depends on the:
- Amount of water that kidney excretes
- Body’s state of hydration
- Factors that influence urine volume:
- Fluid intake (water)
- Water can also excrete through sweats, vomits, diarrhea, and burns.
Note: You have a third-degree burn, water will evaporate causing dehydration, thus will decrease the urine output.
- Fluid loss from non-renal sources
- Variations in the excretion of Antidiuretic hormone (ADH)
- Need to excrete increased amount of dissolved solutes (Glucose/Salts)
- Common to patients having Diabetes mellitus; Polyuria (increase urination)
- Increased salt = Increase water
CLASSIFICATION OF URINE OUTPUT VOLUME | |
Oliguria |
Associated disorders:
|
| |
Anuria |
Associated disorders:
|
| |
Polyuria |
Associated disorders:
|
| |
Nocturia |
Associated disorders:
|
| |
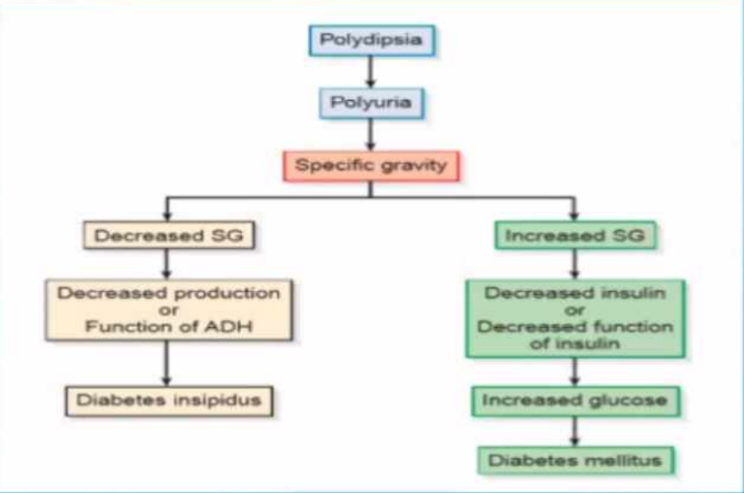
- Since both Diabetes Mellitus and Diabetes Insipidus causes polyuria, we differentiate them by checking the specific gravity.
- In Diabetes Mellitus, increase in glucose causes increase in specific gravity
- In Diabetes Insipidus, there is no problem with the solute concentration so, the specific gravity decreases. However, the problem lies on the urine excretion where too much dilution of urine causes urine specific gravity to decrease down until 1.002
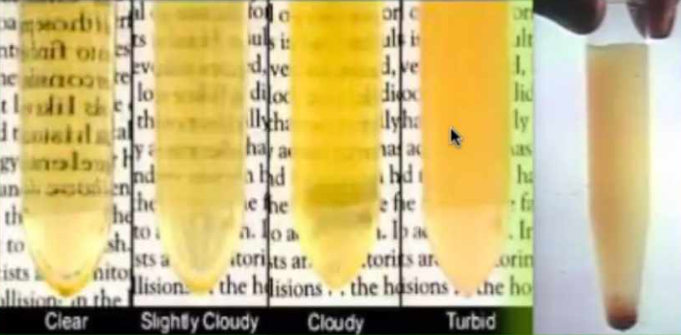
III. URINE CLARITY
- Describes the overall visual appearance of a urine specimen.
- Cloudiness of the urine caused by suspended particulate matter that scatters light
- Refers to the transparency of the specimen.
|
COLOR AND CLARITY PROCEDURE |
|
URINE CLARITY | |
CLARITY | TERM |
Clear |
|
Hazy |
|
Cloudy |
|
Turbid |
|
Milky |
|
|
|
|
|
|
k
NONPATHOLOGIC CAUSES OF URINE TURBIDITY |
|
|
PATHOLOGIC CAUSES OF URINE TURBIDITY |
|
|
LABORATORY CORRELATIONS IN URINE TURBIDITY | |
Acidic Urine |
|
Alkaline Urine |
|
| |
Soluble w/ Heat |
|
Soluble in dilute acetic acid |
|
Insoluble in dilute acetic acid |
|
| |
Soluble in Ether |
|
| |
IV. SPECIFIC GRAVITY
- Specific gravity (SG) is an expression of urine concentration in terms of density
- We have to measure the amount of solute present as well as the density of the urine
- The normal specific gravity of the urine is between 1.003 – 1.035. but for most of the random specimen, the average SG 1.015 – 1.030.
- The amount of solute present in the sample affects the specific gravity
- Detects possible dehydration or abnormalities in antidiuretic hormone.
- Measure of density of the dissolved chemicals in the specimen.
- We have 4 methods on how to measure specific gravity:
- Direct methods using urinometer (hydrometer) or harmonic oscillation densitometry (HOD)
- Urinometer and HOD directly measures the specific gravity.
- Indirect methods using refractometer or the chemical reagent strip.
- Refractometer measures the specific gravity indirectly using refractive index
- Chemical reagent strip is a rapid test for urine constituents where we use other principle of the urine
PARTICLE CHANGES TO COLLIGATIVE PROPERTIES | ||
PROPERTY | NORMAL PURE WATER POINT | EFFECT OF 1 MOLE OF SOLUTE |
Freezing Point |
|
|
Boiling Point |
|
|
Vapor Pressure |
|
|
Osmotic Pressure |
|
|
| ||
SEVERAL WAYS TO MEASURE SPECIFIC GRAVITY
I. URINOMETER
- Urinometer is less accurate than the other methods currently available and is not recommended by the CLSI
- Urinometer also known as hydrometer is an obsolete test because it doesn’t give accurate test
Disadvantages of urinometer:
- It requires a large volume (10 to 15 mL) of specimen
- Calibration Temperature: 20oC
- The urinometer is only accurate when in this temperature
- Requires Temperature Correction:
- Subtract (-) 0.001 for every 3oC that the specimen temperature is below the calibrating temperature
- Add (+) 0.001 or every 3oC that the specimen temperature is above the calibrating temperature
- Requires Solute Correction:
- 1 g/dL glucose = subtract (-) 0.004
- 1 g/dL Protein = add (+) 0.003
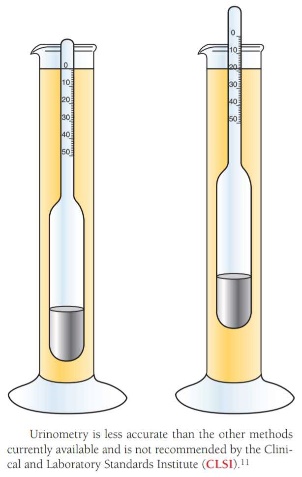
- EXAMPLE:
- A specimen containing 1g/dL protein and 1g/dL glucose has a specific gravity reading of 1.030.
- Specimen Temperature Reading: 26oC
- Calculate the following reading:
- 1.030 – 0.003 (protein) = 1.027
- 1.027 – 0.004 (glucose) = 1.023
- 1.023 + 0.002 (temp) = 1.025
- 1.025 = corrected specific gravity
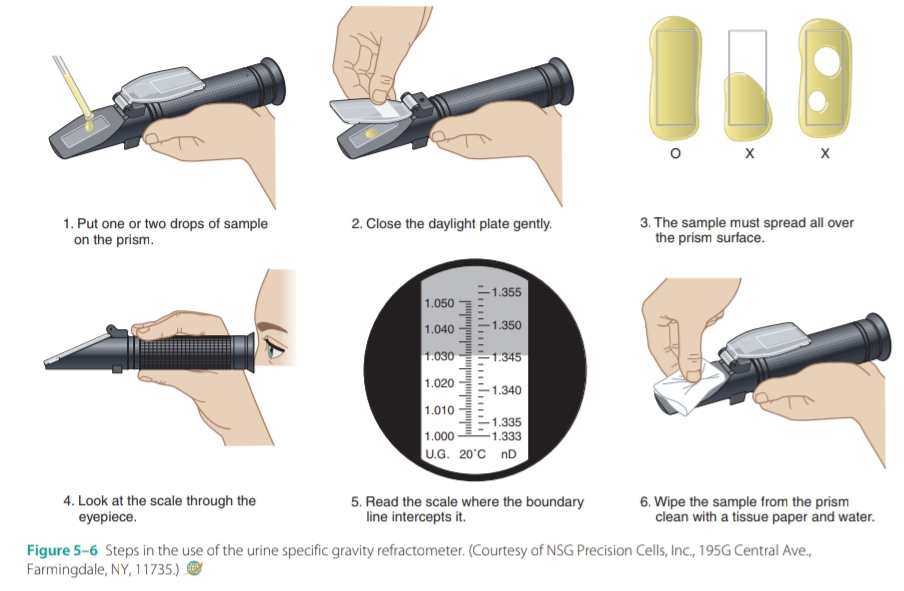
II. REFRACTOMETER
- Due to the disadvantages of urinometer they develop refractometer also known as the total solid meter (TS meter)
- Determines the concentration of dissolved particles in a specimen
- Measures refractive index (a comparison of the velocity of light in air with the velocity of light in a solution)
- Refractometer is an indirect method which depends on the refractive index. The concentration of the solute is determined by the velocity and the angle at which the light pass through the solution.
- Use only small volume of specimen (one or two drops)
- Temperature corrections are not necessary (15oC and 38oC)
- Doesn’t require temperature correction but still requires solute concentration correction
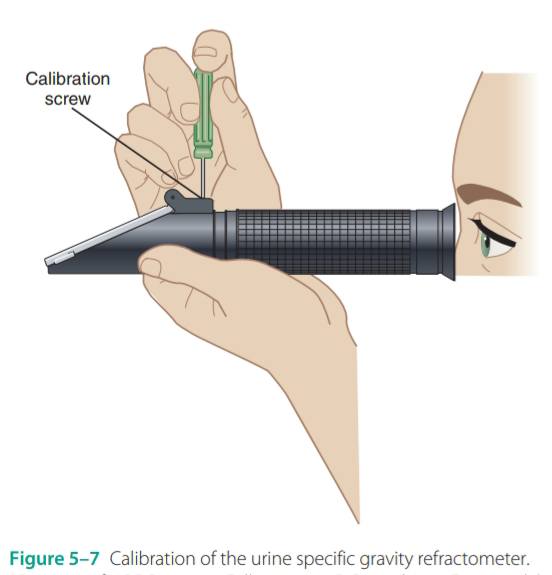
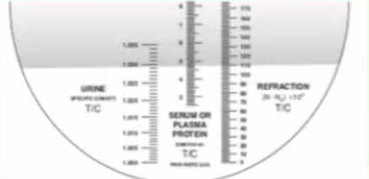
CALIBRATION: | |
SPECIFIC GRAVITY | SOLUTION |
1.000 |
|
1.015 |
|
1.022 |
|
1.034 |
|
| |
III. HARMONIC OSCILLATION DESITOMETRY
- The most accurate among the different measurement of specific gravity. It can measure up to 1.080 SG.
- However, it is no longer being used in the lab.
- Based on the principle that the frequency of a sound wave entering a solution change in proportion to the density of the solution.
- The higher the solute, the higher the sound waves formed
- The harmonic oscillation the principle of the first semi-automated used in clinical microscopy called yellow IRIS machine (International Remote Imaging System)
- In yellow IRIS, we only need 6 mL wherein 4 mL will be used for microscopy and 2 mL for specific gravity
- Shifts in harmonic oscillation are measured, and relative density is calculated.

URINE SPECIFIC GRAVITY MEASURMENTS | |
METHODS | PRINCIPLE |
Urinometry | Density |
Refractometry | Refractive index |
Harmonic Oscillation Densitometry | Density |
Reagent Strip | pKa changes of a polyelectrolyte |
- Due to organic and inorganic substances (byproducts of metabolism)
- Normal urine has a characteristic aromatic odor that is typically faint and unremarkable.
COMMON CAUSES OF URINE ODOR | |
ODOR | CAUSE |
Aromatic | Normal |
Foul, ammonia-like | Bacterial decomposition, urinary tract infection (UTI) |
Fruity, sweet | Ketones (diabetes mellitus, starvation, vomiting) |
Maple syrup | Maple Syrup Urine Disease |
Mousy | Phenylketonuria |
Rancid | Tyrosinemia |
Sweaty feet | Isovaleric acidemia |
Cabbage | Methionine malabsorption |
Bleach | Contamination |
- Urine odor is no longer assessed in the lab as precautions because some organisms can be passed through droplets.
- Normal urine odor is aromatic, it will become foul or ammoniacal if too much bacteria are found in the urine.
- Before, urine odor is the basis for inborn error of metabolism.
- Phenylketonuria is discovered because of urine odor when they smelt a mousy odor in the urine of patient. They concluded that the patient has aminoaciduria (inborn error of metabolism)
- Different odors are caused by aminoaciduria like Tyrosinemia, Isovaleric acidemia, Methionine malabsorption.