HILLEGAS CHAPTER 2
Physiology of the cardiovascular and pulmonary system - chapter 2
The pulmonary system
Functions:
1)
exchange CO2 and oxygen between environment, blood and tissue
by releasing CO2 → it maintains acid-base balance and maintains blood pH
2)
temperature homeostasis → by evaporating heat loss from lungs
3)
it helps to filter and metabolize toxic substances, as it’s only organ to receive all blood from heart
Note recall → oxygen for energy (ATP production)
with oxygen, aerobic → 36 ATP
without oxygen, anaerobic → 2 ATP
Ventilation
ventilation = aka breathing (it’s different from respiration)
Definition = ventilation involves the mechanical movement of gas in and out the lungs
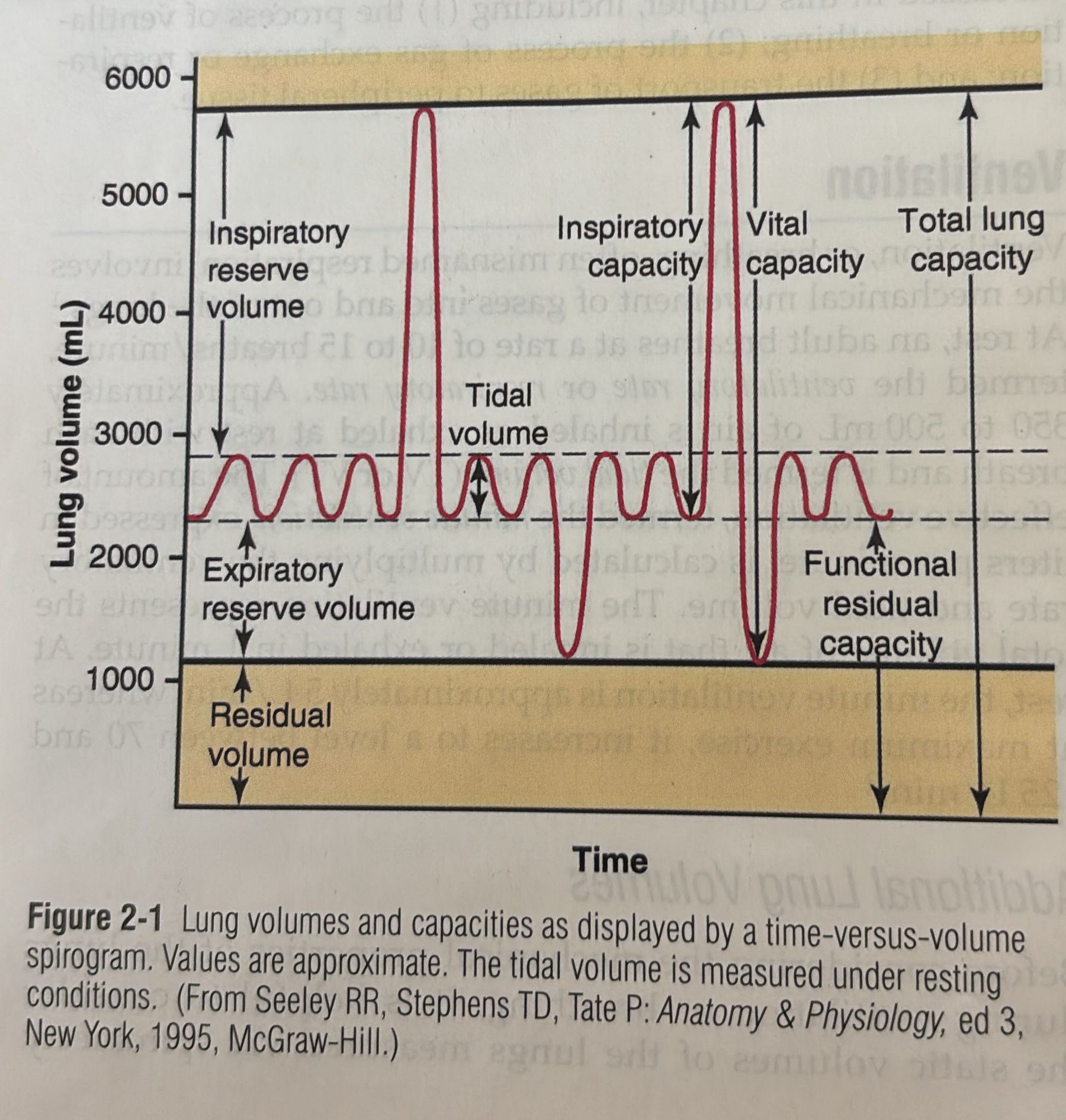
Normal values
ventilatory rate/ respiratory rate (VR) = adult → 10 to 15 breaths x minute
tidal volume (TV, VT) = air inhaled or exhaled with each breath
350mL to 500 mL at rest
minute ventilation = effective ventilation expressed in liters x minute, it’s calculated by VR x TV. It represent the total amount of air inhaled or exhaled in 1 minute
5 L / min at rest
70 to 125 L / min at max exercise
Additional lung volumes
inspiratory reserve volume volume (IRV) = additional volume of air that can be taken beyond the tidal inhalation
expiratory reserve volume (ERV) = the additional volume of air that can be let out beyond the normal tidal exhalation
residual volume (RV) = the volume of air that remains in the lungs after a forceful expiration
inspiratory capacity (IC) = TV + RV → max amount of air that can be inhaled after normal Tidal expiration
functional residual capacity (FRC) = point in which the forces that tend to collapse the lungs are balanced with the forces that tend to expand the chest wall
vital capacity (VC) = IRV + TV + ERV → max amount of air that can be expel after forceful inhalation
total lung capacity (TLC) = max volume to which the lunges can be expanded, sum of all pulmonary volumes
Control of ventilation
breathing → repetitive stimulation from the brain + SKL MSK for respiration + the nerves that contract them
What regulates ventilation/ breathing?
neurons in brain stem, medulla oblongata and pons → automatic breathing, they adjust TV for normal gas exchange
Medulla oblongata
it contains inspiratory neurons that produce inspiration (located in the inspiratory center and dorsal respiratory group) + expiratory neurons are triggered with forceful expiration (expiratory center, anterior posterior respiratory group)
The trigger of these neurons increase the motor units and results in a deeper breath
If it takes longer to fire these neurons → slower respiratory rate
If there is no neural stimulation → elastic recoil of lung and passive expiration
if there is neural stimulation of expiratory neurons (deep expiration) → inhibition of inspiratory neurons
Pons
2 major centers that assist with ventilation
1) pneumotaxic center → upper pons
rythm of ventilation, time breath in - breath out , it inhibits the other center
2) apneustic center → lower pons “inspiratory center of medulla“
it facilitates prolonged breathing patterns when the other center is inhibited
Breathing with conscious change in motor pattern involves the motor cortex → signal is send to the cortico-spinal tract bypassing respiratory centers in brainstem to change ventilation
Mechanics of breathing
Definition: “movement of air in and out the lungs that occurs to a results of pressure differences between the 2 ends of the airways“.
airflow is proportional to the difference in pressure and inversely proportional to the resistance within the airway
more air → more pressure difference
more air → less resistance
Ventilation is affected by different physical properties of lungs:
Properties of lungs: (how do they affect ventilation?)
elasticity
compliance
surface tension
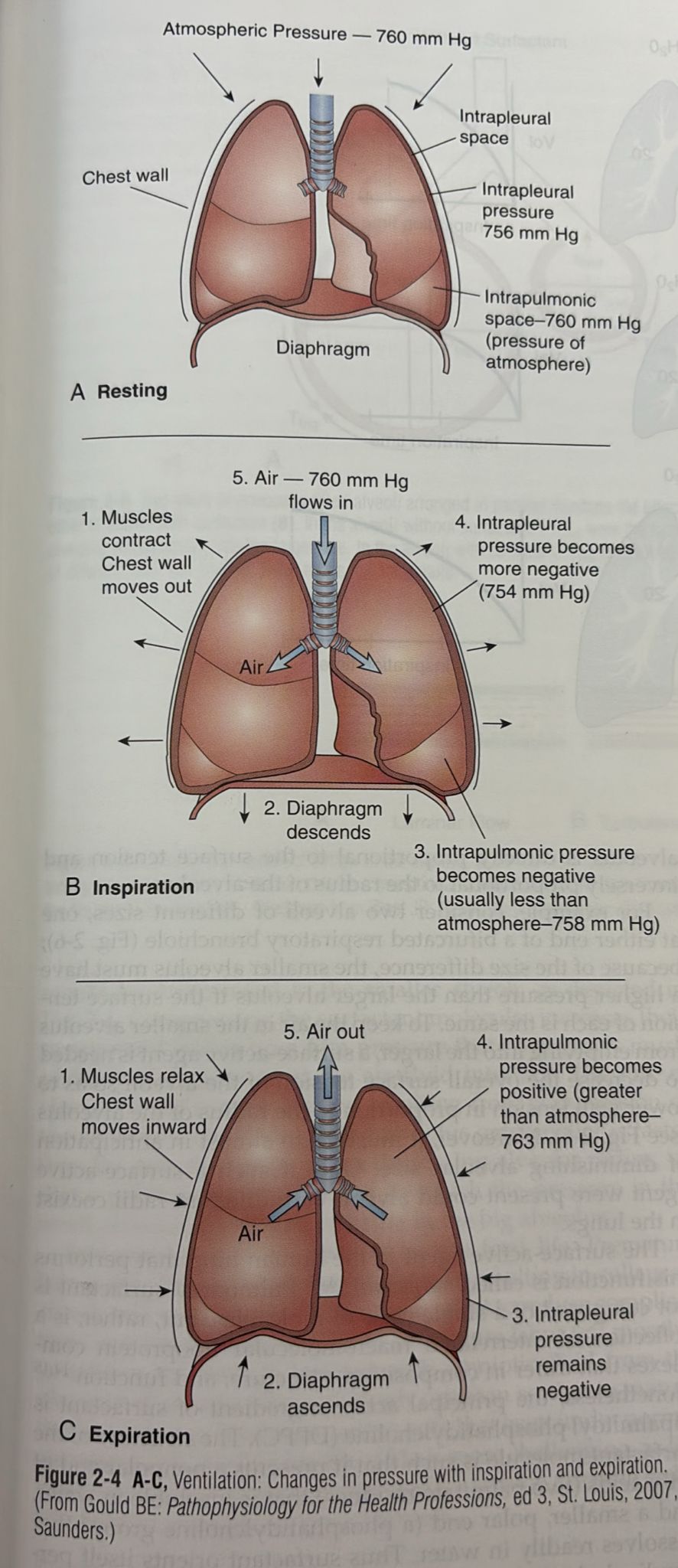
Pressure changes that allow ventilation to occur
Intrapulmonary and atmospheric pressure
Inspiration = active process, it involves contraction of respiratory muscles
when diaphragm and ext. intercostal contract → increase volume of thorax and lungs
Intrapulmonary pressure decrease below atmospheric level (pressure in the lung) = Subatmospheric or negavitve intrapulmonary pressure (→ Boyle’s law)
Note Boyle’s law
“pressure or given quantity of gas is inversely proportional to its volume“
is volume high → pressure low
if volume low → pressure high
In lung → more air with inspiration = more volume, therefore pressure low
how do the changes in pressure affect ventilation?
The difference in pressure between atmosphere and lungs → helps air flow into lungs to normalize pressure differences
expiration occur when IPP exceed atmpspheric pressure (EXP → IPP > ATMP)
lungs recoil inward to expel air
Differences between mechanical ventilation and and normal ventilation
normal ventilation = process we explained above
mechanical ventilation = PT lacks ability to generate negative IPP
reduced strength of inspiratory muscles
Note: we put mechanical ventilators because it pushes air into the lungs by creating even a greater ATMP that is in the lung so that the pressure in the lung becomes negative
How to train PT?
breathing exercises
re-positioning
use of inspiratory muscles (train them)
Physical properties of lungs
3 physical processes that help ventilation
1) Compliance
allows lung tissue to stretch during inspiration (balloon)
Compliance = describes the distensibility of lung tissue
defined as the change in lung volume x change in transpulmonary pressure
because of this relationship, the greater the pressure, the more lung expansion and vice-versa
Compliance is reduced as it reaches TLC (stiff because full)
Compliance can be reduced by increasing resistance to distension
1) emphysema (disease): destruction of recoil elasticity results in hyperinflation of the lung (transpulmonary pressure low → compliance low)
2) pulmonary fibrosis: lung fibrotic and stiff, with small changes in lung volume because of small transpulmonary pressure → therefore small compliance
In PT with these conditions
increase in RF
use accessory muscles
work hard to increase lung volume
2) Elasticity
Definition: the tendency of a structure to return to its initial size after being distended
collagen + elastin fibers with the alveolar wall, bronchi, and pulmonary capillaries give the lung this propriety
3) surface tension
Definition = surface tension at the air-liquid interface on the alveolar surface
it has a greater influence on resisting compliance (distension) aka the same thing as elasticity but more
surface tension: force between 2 water molecules at the surface being attracted more by each other than other molecules
role: increase the pressure of air within the alveolus
Note: the law of Laplace “the pressure created within the alveolus is directly proportional to the surface tension and inversely proportional to the radius of the alveolus“
- more/less pressure with alveolus = more/less surface tension
- more pressure within the alveolus = smaller alveolus (aka radius)
why? Keep the air inside the small alveolus to ensure the air within doesn’t flow into the bigger alveolus. To do so, SURFACTANT (surface active agent) decreases surface tension in proportion to radius
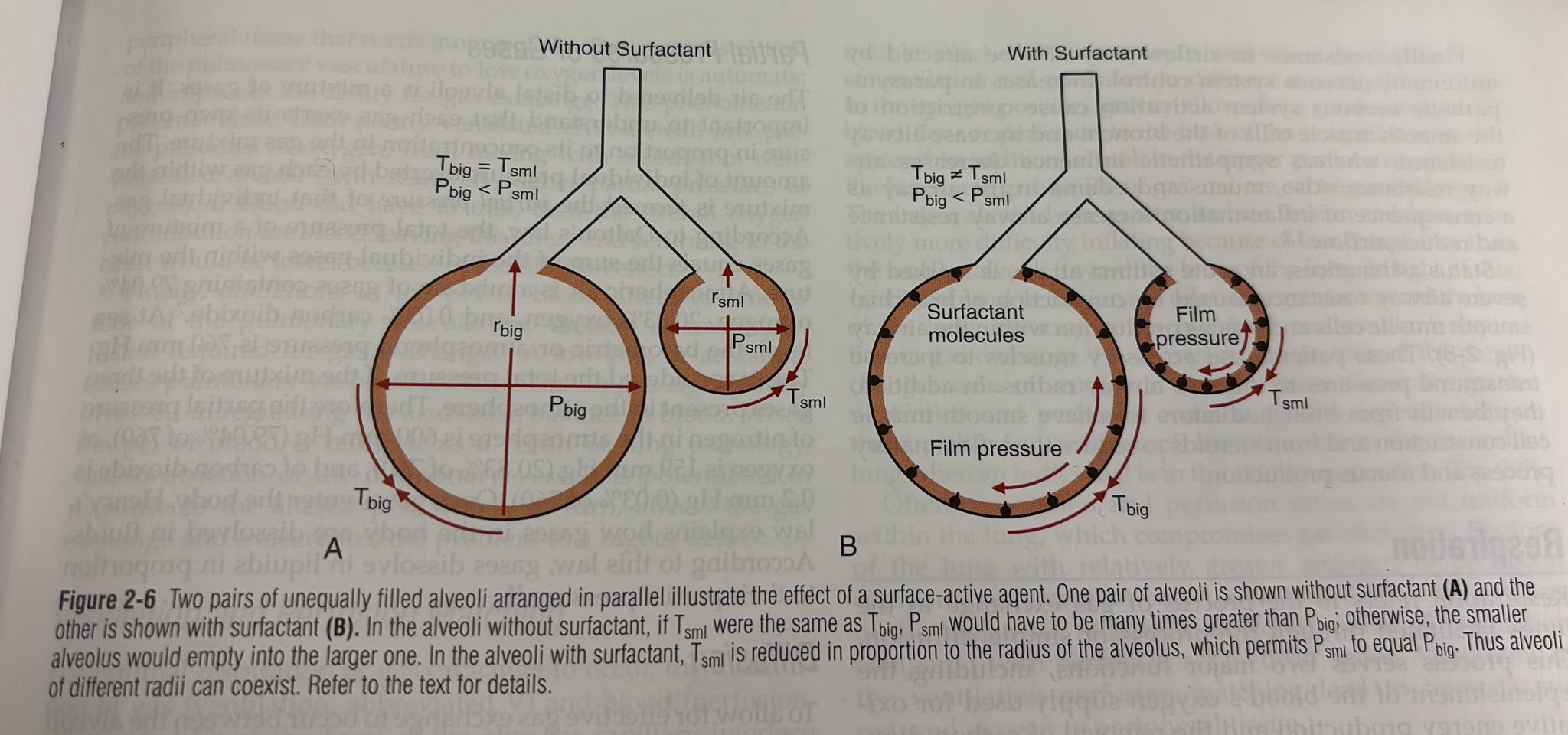
who doesn’t have surfactant?
31 weeks old babies starts to have it → before no
drawing people (washed away)
Respiration
respiration definition: the process of gas exchange in the lungs facilitated through the process of simple diffusion
2 functions:
1) oxygen to blood (nutrition) → production of ATP (aka energy)
2) removal of CO2
How does diffusion occur?
1) oxygen to lungs (alveolar ventilation)
2) oxygen and CO2 exchange in the blood (pulmonary perfusion)
1) Air is delivered to distal alveoli for gas exchange (so-called pulmonary ventilation)
2) blood comes to the lungs from the RT side of HR through the pulmonary artery and goes to the pulmonary capillaries
3) (respiration =) gas exchange between pulmonary capillaries and alveoli through the “respiratory membrane” (alveolar-capillaries membrane)
Partial pressure of gases
every gas has its pressure
at the alveoli, there is a mix of gases
Dalton’s law → gases dissolve in liquids in proportion to their partial pressure
Easy explanation of what’s going on by chat:
Diffusion
to allow gas exchange in alveoli and capillaries, different partial pressures of O2 and CO2 must exist in both parts
this difference creates a pressure
because of the pressure, the gases from the high-pressure area move to the low-pressure area (physics) and therefore we have diffusion across the respiratory membrane
Perfusion
Perfusion = blood flow to the lungs available for gas exchange
pressure pulmonary circulation < pressure systemic circulation BUT flow rates here are the same because of reduced vascular resistance within Pulmonary circulation
Pulmonary circulation = low-resistance, low-pressure pathway → why? protection of the lung from edema and fluid
perfusion is affected by partial pressures of oxygen, how?:
arterioles (blood vessels) constrict when PP in alveoli low and the other way around when opposite
→ These vasomotor changes occur to reduce blood flow to areas in the lung that are poorly ventilated and increase blood flow where they are more ventilated (autonomic)
It avoids the mix of well-ventilated alveoli and bad-ventilated alveoli → efficiency
Pulmonary vasoconstriction is also caused by a low pH (acidic) and therefore it affects perfusion
Ventilation and perfusion matching
optimal respiration and gas exchange: V = Q
ventilation (V) = exchange of gas and its distribution
perfusion (Q) = blood flow to the lungs at the level of capillaries
V= Q is gravity-dependent and it happens in gravity-dependent areas:
standing/ sitting → gravity allows Q to be more at the base of the lung, therefore in this case V = Q at the base of the lung
alveoli smaller at the base of the lung
Residual ventilation > in the higher portion of the lung = more gas
A change in position changes V=Q (supine, side-lying)
Also, the V=Q ratio is not uniform within the lung, some areas have more V, and the body tries to match it giving more Q, but some areas have less V, therefore poor Q because of less oxygen and capacity to exchange gases
How to measure respiration? saturation
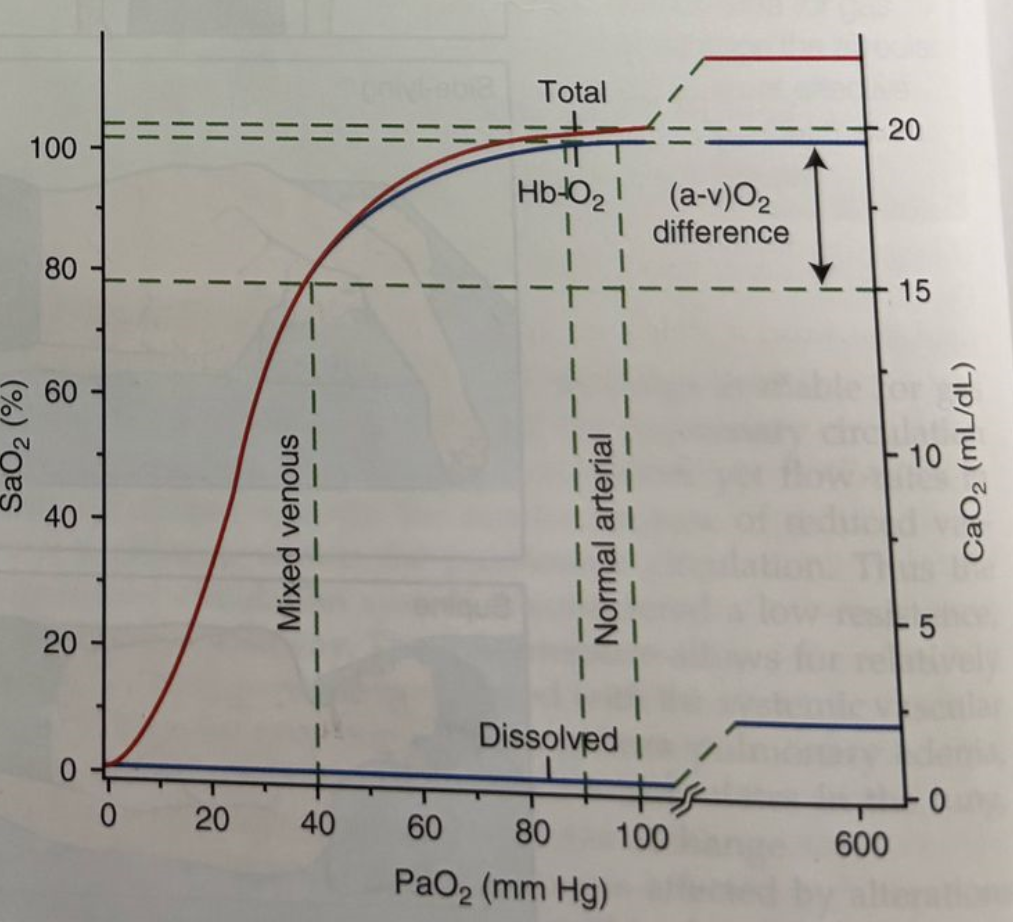
Saturation = percentage of hemoglobin in the blood that is carrying oxygen compared to the total hemoglobin available. It indicates how well oxygen is being transported in the bloodstream to the body’s tissues.
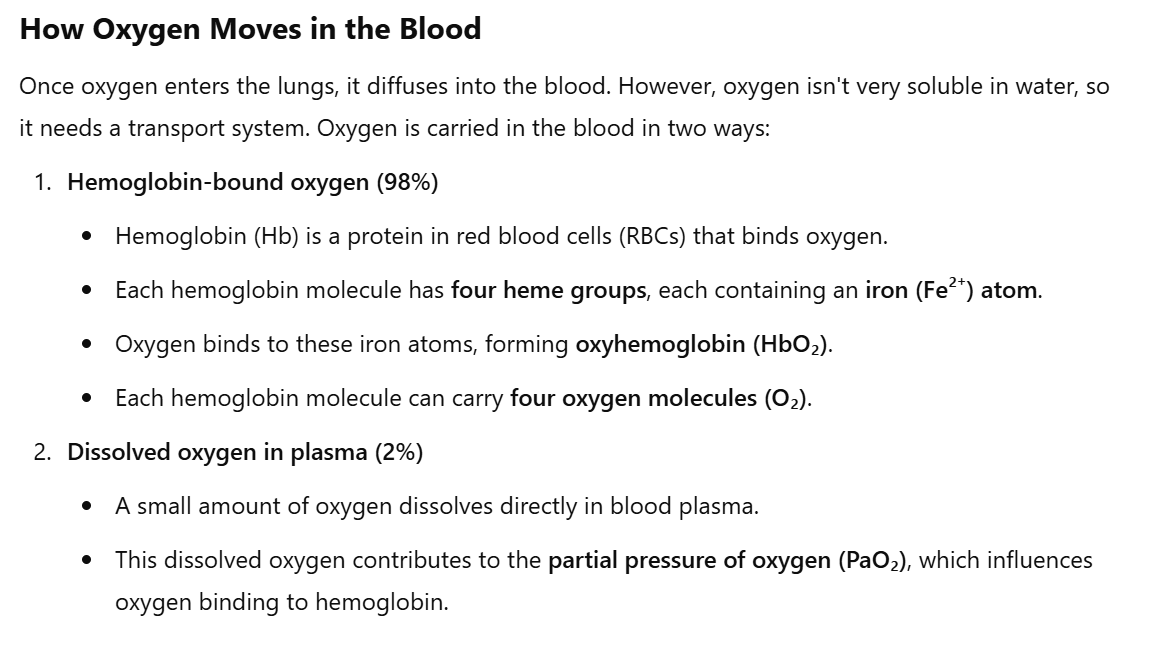
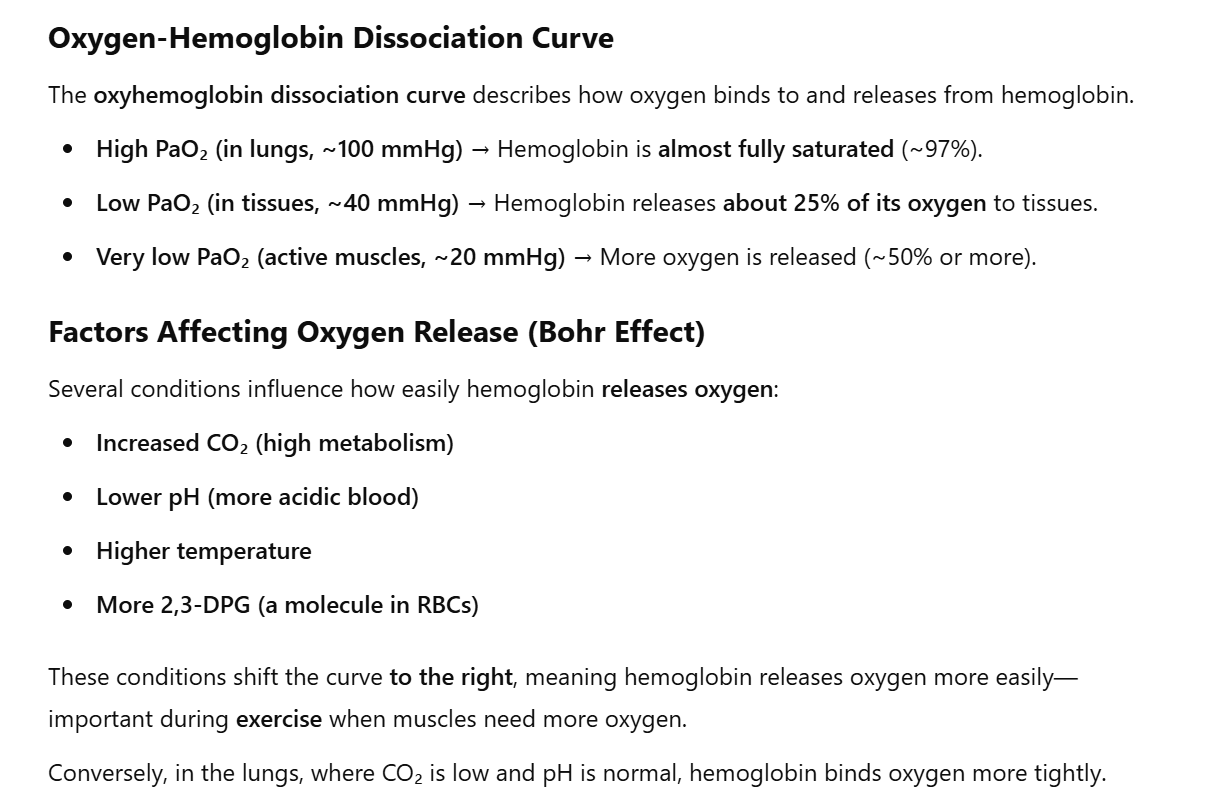
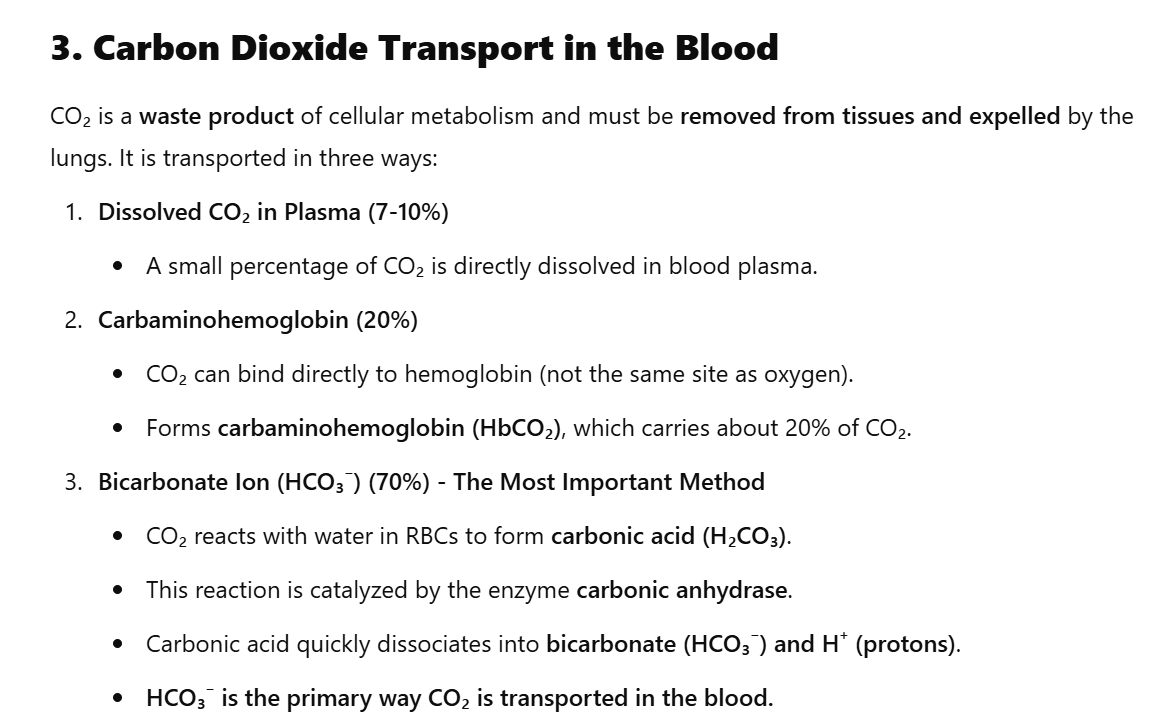
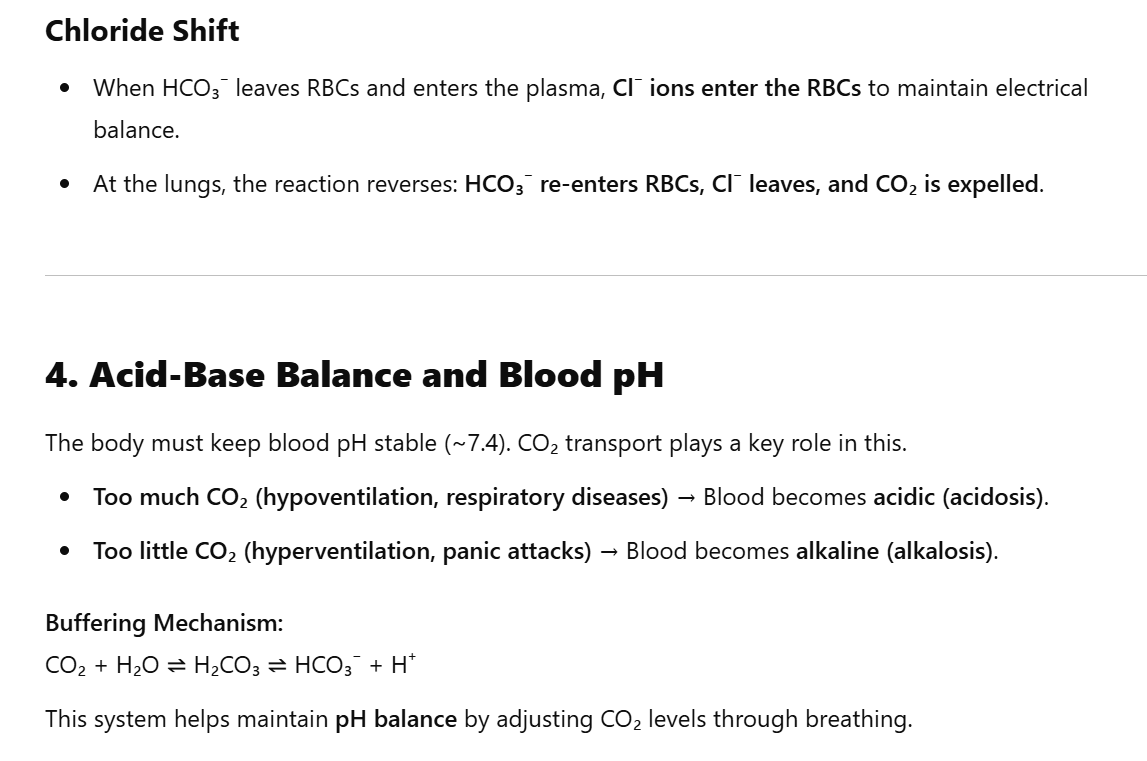
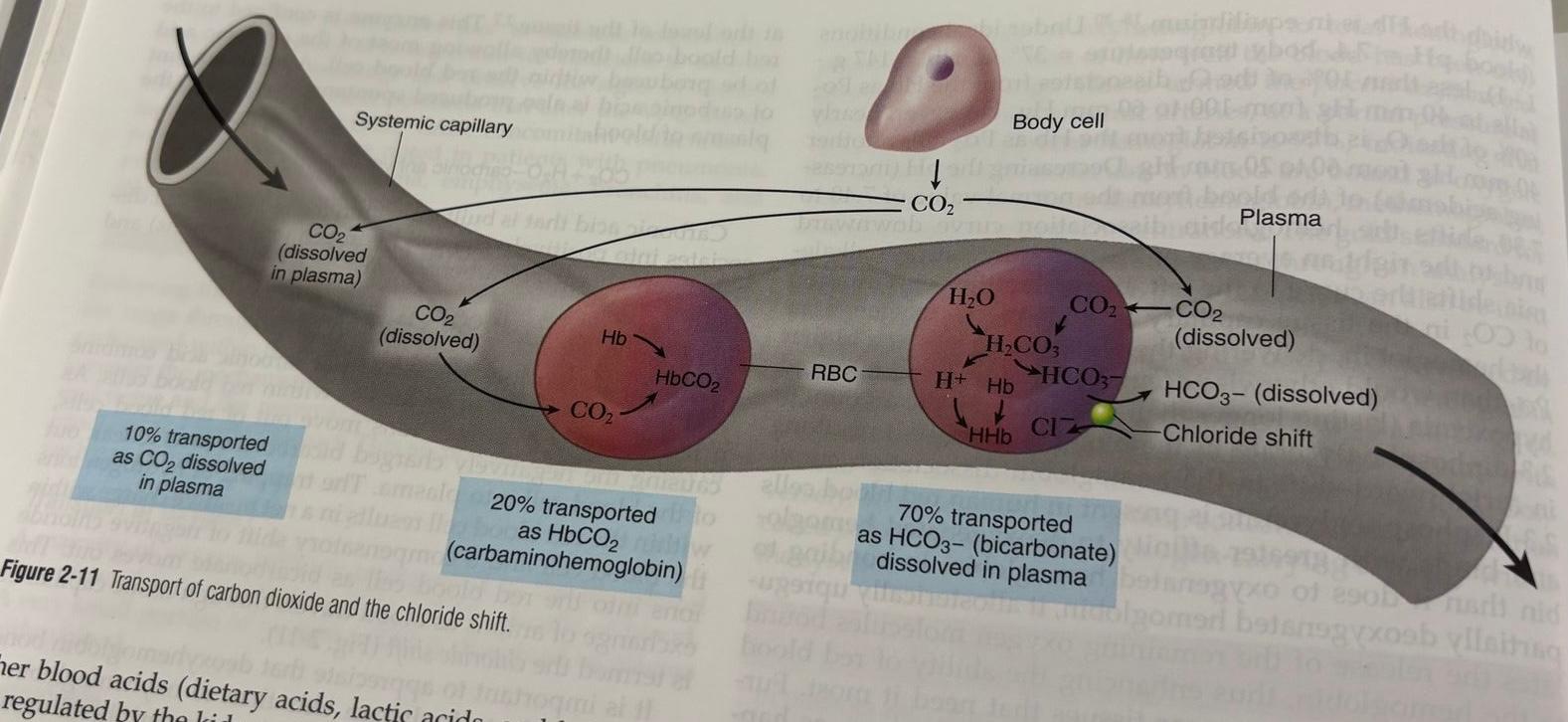
Transport of oxygen and carbon dioxide
Note to self: I asked chat GPT to do a summary of the pages (Chapter 2, 32 - 33 - 34), it was complicated, but it made it clear but info from the book (also other things only from book, just make them easier)