Ab Psych Chapter 11: Schizophrenia
DSM Criteria for Schizophrenia→
- Two or more of the following, present significantly during a 1 month period:
- Delusions (at least 1 of these 3 must)
- Hallucinations (at least 1 of these 3 must)
- Disorganized speech (at least 1 of these 3 must)
- Grossly disorganized or catatonic behavior
- Negative symptoms (blunted affect, anhedonia, etc)
- Disturbance continuously for 6 months
- Social, occupation, self-care dysfunction
- Schizoaffective, depressive, bipolar rule out
- Substance and medical rule out
Schizophrenia vs Psychosis:
Positive & Negative Symptoms:
Delusions: An erroneous belief that is fixed and firmly held despite clear contradictory evidence
- Common types:
- Delusions of persecution or paranoia: “The CIA is out to get me”
- Delusions of reference: “People on TV are making fun of me”
- Delusions of being controlled: “believing own thoughts, feelings, impulses, actions, are controlled by external forces”
- Delusions of grandeur: “believing to be Jesus or have grand but illogical plans for saving the world”
- Thought broadcasting:
- Thought insertion:
- Thought withdrawal:
Hallucinations: sensory perceptions experienced in the absence of any external perceptual stimulus.
- Most common: auditory hallucinations (hearing voices)
- Also common- Tactile (tingling, electrical, burning sensations) or Somatic (e.g., feeling like snakes are crawling inside body)
- Less common- Visual (seeing things that are not there), Olfactory (smelling odors that are not there), and Gustatory (tasting things that aren’t present)
Disorganized Speech: a breakdown in the organization, processing, and control of thoughts
- Looseness of associations: words combined incoherently; jumping from one topic to another
- Less common-
- Neologisms: made up words
- Perseveration: persistent repetition
- Clanging: stringing together words or sounds based on rhyming
- Blocking: Involuntary, abrupt, interruption of speech or thought
- Incoherence: word salad
Disorganized Behavior:
- Avolition - apathy, lack of interest or engagement in goal-directed behavior (can’t convert desires into actions)
- Catatonia - state of unresponsiveness to external stimuli (odd gestures & facial expressions, may become stuck in odd postures)
Negative Symptoms: Loss of motivation, disinterest, social withdrawal, blunted affect
- Blunted/flat affect: absence of emotional expression in the face and voice
- Exaggerated or inappropriate affect: e.g., laughing for no reason or giggling at bad news. Internal experience of emotions doesn’t seem to match external expression of emotions
Three Phases of Schizophrenia:
- Prodromal phase: early, subtle signs of deterioration. e.g., subtle unusable thoughts or abnormal perceptions
- Acute phase: Apparent psychotic symptoms present, Behavior becomes increasingly odd over time
- Residual phase: Return to prodromal-like levels
- Behavior stabilizes (i.e., obvious psychotic symptoms gone)
- Cognitive, social, emotional impairment remains that makes it hard to function in social, occupational roles
Prevalence of Schizophrenia→
1% world prevalence
<1% US prevalence
Mixed evidence for racial/ethnic differences
Slightly more prevalent in males than females
Typically diagnosed in late teens to early thirties
- Males - Single peak age for onset: 21-25
- Females - Two peak ages for onset: 25-30 & 45+
Sex differences: females have more functioning before onset, tend to respond more favorably to treatment

Patterns of Schizophrenia:
- Chronic condition - occasional acute psychotic episodes & cognitive, emotional, and motivational impairment
- With continued drug treatment, 60%+ have long periods of remission
- Many improve significantly over time but low likelihood of returning to pre-morbid levels of functioning
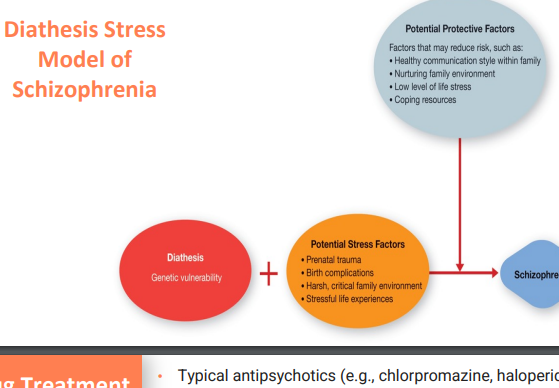
Theoretical Perspectives of Schizophrenia→
Genes, biochemical factors, abnormalities in brain structure, viral infections
Genes: Offspring of older fathers are at higher risk for schizophrenia and autism (No increased risk of genetic mutations in older mothers)
Biochemical: Overactivity of dopamine transmission in the brain (dopamine hypothesis). Two sources of evidence:
- Neuroleptics - block dopamine receptors, reduce hallucinations and delusions
- Amphetamines - increase concentration of dopamine, in high doses of amphetamines - can cause schizophrenia-like symptoms
Brain abnormalities: people with schizophrenia have abnormally enlarged ventricles, decreased gray matter
- Especially in prefrontal cortex
- Associated deficits: regulating attention, organizing thoughts, formulating goal, planning action
Viral infections: Higher risk for disability if pregnant women are exposed to flu virus in 1st trimester. Or if born in winter and early spring in northern hemisphere
- Viral agents could act on the developing brain during prenatal development in ways that increase risk of developing schizophrenia later on.
Treatments for Schizophrenia→
- Schizophrenia requires lifelong treatment
- Drug treatment: Typical antipsychotics (e.g., chlorpromazine, haloperidol)
- First generation of drugs; block dopamine in the brain
- Effective for most patients but risk of tardive dyskinesia (involuntary repetitive movements) with long-term use
- Most common among older people and women
- Improves over time but can be disabling
- Atypical antipsychotics (e.g, clozapine, risperidone, olanzapine)
- Second-generation drugs with lower risk of TD
- Drug therapy + psychological approaches better than drug therapy alone, according to a large study of 400+ patients with schizophrenia.
- Assertive Community Treatment (ACT): Team-based approach, Support available 24/7, Help person address every aspect of life
- Medication management, Social support, Vocational training and support, For people who have transferred out of an inpatient hospital but need similar level of care, Shown to reduce hospitalizations by 20%
- Social Skills Training: how they will do daily tasks
- CBT: goal isn’t to cure schizophrenia, but rather to manage symptoms and reduce stress
- Helping the person become more flexible in thinking patterns - replacing delusional beliefs with alternative explanations
- Change thinking patterns regarding hallucinations (reattributing voices to own internal voice or self)
- Help patients identify cognitive errors, such as jumping to conclusions
- Combat negative symptoms, such as lack of motivation and apathy, that make it difficult for them to adjust to demands of community living
- A large and growing body of evidence shows therapeutic benefits from using CBT and similar techniques in treating patients with schizophrenia
- Family Intervention Programs: educating family about schizophrenia, demonstrating how to relate it in a less hostile way, aims at reducing family conflict and improving social functioning in schizophrenia
- Related Disorders:
- Brief Psychotic Disorder: at least one of the symptoms (delusions, hallucinations, disorganized speech, catatonic behavior) and lasts from a day to a month
- Schizophreniform Disorder: Similar to schizophrenia but symptoms occur for a shorter period of time (1 to 6 months)
- Delusional Disorder: Bizarre delusions but no other odd behavior
- Schizoaffective Disorder: “Mixed bag” of symptoms. Mood disorder + schizophrenia