Odontogenic Infections and Periapical Abscesses: Clinical and Therapeutic Approaches with Facial Cavity Abscesses
Clinical Significance of Odontogenic Infections
Prevalence: Dental infections are common and can lead to serious complications.
Complications: Untreated infections can spread and create local and systemic health risks.
Classification of Odontogenic Infections
Localized Infections: Superficial infections confined within a specific area.
Deep Infections: Includes abscesses such as periapical and facial cavity abscesses.
Pathogenesis of Periapical Infections
Process:
Pulpa necrosis leads to periapical inflammation, resulting in the formation of an abscess.
Abscess: A collection of pus that causes swelling and severe pain.
Anatomical Significance of Facial Cavity Abscesses
Facial Cavities: Considered areas of low resistance to spreading infection.
Regions Involved: Submandibular, sublingual, parapharyngeal, temporal; interconnected areas prone to infection.
Diagnosis of Odontogenic Infections
Radiological Imaging:
Panoramic X-ray, CBCT: Effective for detailed visualization of hard tissues.
MRI and USG: Ideal for evaluating soft tissue abscesses.
Types of Tooth Abscess
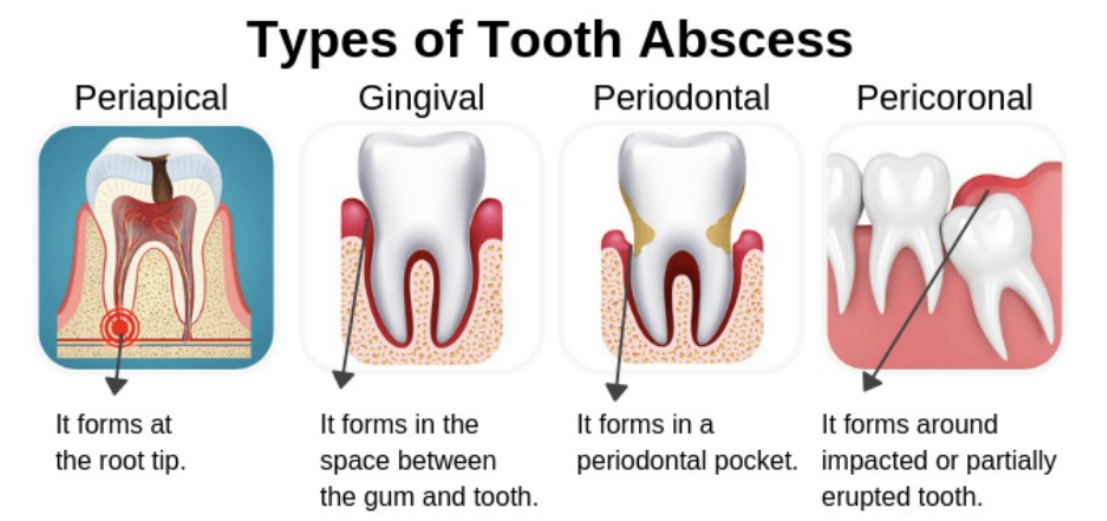
Categories:
Periapical: At root tip.
Gingival: In the gum and tooth region.
Periodontal: In periodontal pockets.
Pericoronal: Around impacted or partially erupted teeth.
Periapical Abscesses and Management
Requires prompt management to prevent complications such as severe pain and infection spread.
Etiology and Risk Factors of Periapical Abscess
Causes:
Primarily due to pulp necrosis and facultative bacteria like viridans streptococci.
Factors like immune response systems play a role in susceptibility.
Clinical Findings in Periapical Abscess
Symptoms:
Severe localized pain, abscess swelling, and sinus tract formation.
Reaction to dental vitality tests often reveals negative to late positive results.
Diagnosing Periapical Abscesses
Clinical Manifestations:
Physical inspection reveals swelling, decay, or mobility in teeth.
Radiological findings include radiolucency indicating infection severity.
Signs of Serious Infection
Indicators:
High fever (over 38°C), severe facial swelling, and intense pain.
Difficulty with respiration and swelling in the neck area.
Radiological Findings: Periapical Abscesses
Appearance: Radiolucent areas seen in chronic infections; minimal changes in early stages.
Complications of Periapical Abscess
Potential Serious Conditions: Periapical cysts, maxillary sinusitis, Ludwig's angina, osteomyelitis, and sepsis.
Periapical Complications
Progression Risks: Rapidly advancing cellulitis and systemic complications can arise from untreated abscesses.
Development of Periapical Granulomas and Cysts
Histopathological features include an epithelial lining and granulation tissue indicating chronic inflammation.
Treatment Approaches of Periapical Abscess
Endodontic therapy, extraction of the infected tooth, surgical drainage, and medical treatment.
Abscess Drainage
Procedure: Involves incision followed by irrigation to relieve pain and promote healing, but should be complemented with other therapies.
Use of Antibiotics
Preferred Medications: Amoxicillin-clavulanate, ampicillin-sulbactam, metronidazole, and clindamycin are commonly used.
Facial Cavity Abscesses and Types
Anatomical Structures: Categorized into superficial and deep neck cavities.
Vestibular Abscess
Definition: Infection confined between the gingiva and cortex adjacent to roots; treated through intraoral drainage.
Palatal Abscess
Location: Infection accumulates under palatal mucosa, treated with intraoral drainage.
Buccal Abscess
Description: Soft tissue area between the buccinator muscle and cheek mucosa, drainage depends on spread of infection.
Submandibular Abscess
Causes: Spreads from infections of molar teeth; poses risks for airway obstruction and Ludwig's angina.
Sublingual Abscess
Classification: Manifests as infections in the area under the tongue; involves the risk of airway obstruction.
Submental Abscess
Presentation: Swelling and tenderness below the jaw as a consequence of anterior tooth infections.
Ludwig Angina
Description: Bilateral infection involving multiple spaces leading to severe complications like airway obstruction.
Fossa Canina Abscess
Anatomical Boundaries: Related to the upper canine’s apical infection; drainage performed intraorally.
Cavernous Sinus Trombosis
Serious Condition: Retrograde infection spread leading to critical complications.
Submasseteric Abscess
Characterization: Generally caused by infections of mandibular teeth; requires careful management to prevent airway threats.
Pterygomandibular Abscess
Overview: Accumulates between the mandible and pterygoid muscles; often treated via intraoral drainage.
Temporal Abscess
Source: Typically linked to maxillary third molar infections; requires urgent intervention due to potential complications.
Infratemporal Abscess
Clinical Features: Swelling and pain localized to the cheek areas; manage through drainage techniques.
Parapharyngeal Abscess
Overview: Accumulates in parapharyngeal cavity; may require drainage through multiple approaches.
Retropharyngeal Abscess
Characteristics: Soft tissue infection often in children; managed typically through surgical drainage.
Prevertebral Abscess
Spread: Can extend from other body areas; significant complications may arise if untreated.
Systemic Manifestations in Facial Cavity Infections
Symptoms: High fever, weakness, tachycardia, sepsis; indicates systemic infection.
Airway Management
Importance: Critical for survival in infections affecting mouth and neck regions.
Antibiotic Selection and Treatment Principles
Guidelines for Use: Broad-spectrum antibiotics are essential complemented by evacuation of abscess.
Prevention of Infections
Approach: Emphasizes the role of early diagnosis and regular dental check-ups.
Conclusion and Summary
Key Points: Odontogenic infections need rapid intervention; can lead to serious complications.
Diagnosis and Management
Approach: Involves clinically identifying symptoms; therapeutic actions include drainage and antibiotic treatments.
"Take-Home"**
Early intervention is vital to prevent severe outcomes; a multidisciplinary approach is necessary for effective treatment.
 Knowt
Knowt