Schizophrenia
Key terms
Schizophrenia - a severe mental disorder where contact with reality and insight are impaired, example of psychosis.
Classification of schizophrenia - the process of organising symptoms into categories based on which symptoms cluster together in people with mental disorders
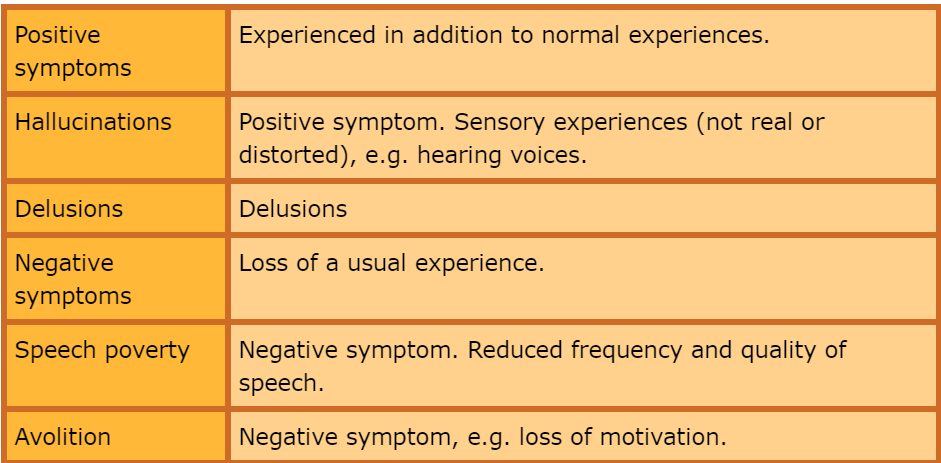
Positive symptoms of schizophrenia - Atypical symptoms experienced in addition to normal experiences. They include hallucinations and delusions
Hallucinations - a positive symptom of schizophrenia. They are sensory experiences of stimuli that have either no basis in reality or are distorted perception of things that are there.
Delusions - a positive symptom of schizophrenia. They involve beliefs that have no basis in reality, for example that the person with schizophrenia is someone else of that they are a victim of conspiracy.
Negative symptoms of schizophrenia - Atypical experiences that represent the loss of a usual experience such as clear thinking or normal levels of motivation.
Speech poverty - A negative symptom of schizophrenia. It involves reduced frequency and quality of speech.
Avolition - A negative symptom of schizophrenia. It involves loss of motivation to carry out tasks and results in lowered activity levels.
Co-morbidity - The occurrence of two disorders or conditions together, for example a person has both schizophrenia and a personality disorder. Where two conditions are frequently diagnosed together it calls into question the validity of classifying the two disorders separately.
Symptom overlap - Occurs when two or more conditions share symptoms. Where conditions share many symptoms this calls into question the validity of classifying the two disorders separately.
Diagnosis and classification of schizophrenia
Schizophrenia is a serious mental disorder experienced around 1% of the world population. More commonly diagnosed in men than women and cities than countryside and in working class. Symptoms can interfere with everyday tasks, so many end up homeless or in hospital.
Classification of schizophrenia
It has a cluster of symptoms which seem to be unrelated. There are two major systems for the classification of mental disorder
World Health Organisation’s international classification of disease edition 10 (ICD-10)
American psychiatric association’s diagnostic and statistical manual edition 5 (DSM-5)
They differ in their classification.
DSM 5 -positive symptoms - delusion, hallucination or speech disorganisation must be present. Previous editions had recognised subtypes of schizophrenia.
ICD - two or more negative symptoms are sufficient. ICD-10 recognises a range of subtypes of schizophrenia.
Paranoid schizophrenia - characterised by powerful delusion and hallucination but relatively few other symptoms
hebephrenia schizophrenia - involves priminaly negative symptoms
Catatonic schizophrenia - disturbance to movement, leaving the person immobile or alternatively overaction.
Positive symptoms - the additional experiences beyond those of ordinary experience, they include hallucinations and delusions.
Hallucinations - Unusual sensory experiences. Some are relevant to events in the environment whereas others bear no relationship to what the senses are picking up from the environment e.g voices heard of people criticising them. Hallucinations can be experienced in any sense, person may see distorted facial expressions on people that are not there.
Delusions - Also known as paranoia, there are irrational beliefs. Common delusions may involve an important historical, political or religious figure. Delusions commonly involve being persecuted. Another class of delusions involve the body, people believe that they or part of them in under external control, some can lead to aggression.
Negative symptoms - Involve the loss of usual abilities and experiences. Examples include avolition and speech poverty.
Avolition - Sometimes called apathy can be described as finding it difficult to begin or keep up with goal orientated activity. They often have sharply reduced motivation to carry out a range of activities. Andreason (1982) identified three identifying signs of avolition
poor hygiene and grooming
lack of persistence in work or education
lack of energy
Speech poverty - The ICD-10 recognises speech poverty as a negative symptom, the emphasis on reduction in the amount and quality of speech, sometimes accompanied by a delay in the persons verbal responses during conversation.
DSM places emphasis on speech disorganisation, where speech becomes incoherent of the speaker changes topic mid-sentence, this is classified as a positive symptom of schizophrenia, whilst speech poverty remains negative.
Evaluation
Reliability
Means consistency. An important measure of reliability is inter-rater reliability, the extent to which different assessors agree on their assessments. Elie Cheniaux et al (2009) had two psychiatrists independently diagnose 100 people using both DSM and ICD. Inter-rater reliability was poor, one diagnosing 26 according to DSM and 44 according to ICD whereas the other diagnosing 13 according to DSM and 24 according to ICD.
Validity
This is the extent to which we are measuring what we are intending to measure. There are a number of validity issues and one standard way to assess validity of a diagnosis is criterion validity, do different assessment of symptoms arrive at the same diagnosis for the same person? Schizophrenia is more likely to be diagnosed using ICD shown by Cheniaux et al.
Comorbidity
Morbidity refers to a medical condition or how common it is. Comorbidity is the phenomenon that two or more conditions occur together. If conditions occurs together lots of times then this called into question the validity of their diagnosis and classification because it might just be a single condition. Peter Buckley et al (2009) concluded that around half of people with a diagnosis of schizophrenia also have a diagnosis of depression (50%) or substance abuse (47%). Post-traumatic stress disorder also occurred in 29% of cases and OCD in 23%. This poses a challenge of both classification and diagnosis.
Symptoms overlap
There is a considerable overlap between schizophrenia and other conditions. Both schizophrenia and bipolar disorder involve positive symptoms like delusion and negative symptoms like avolition. Also calls into question the validity of both classification and diagnosis. Under ICD may be diagnosed with schizophrenia however under DSM would be diagnosed as bipolar.
Gender bias diagnosis
Longnecker et al (2010) reviewed studies of the prevalence of schizophrenia and concluded that since the 1980’s men have been diagnosed with schizophrenia rather more often than women, prior there was no difference. This led to them suggesting that men had a genetic vulnerability, however another possible explanation is gender bias. It appears that women typically function better than men, being more likely to work and have good family relationships. (Cotton et al 2009)
If women are under-diagnosed then this suggests that the validity of the diagnosis of schizophrenia is poor, because our procedures for diagnosis work well only on patients of one gender.
Cultural bias in diagnosis
African americans and english people of Afro-Caribbean origin are several times more likely than white people to be diagnosed. Rates however are not particularly high in Africa and West Indies, therefore not due to genetic vulnerability, may be issues of cultural bias.
Positive symptoms such as hearing voices may be considered more acceptable in African cultures because of beliefs in communication with ancestors. Javier Escobar (2012) has pointed out that white psycharistics may tend to over-interpret symptoms and distrust the honestly of Afro-Caribbean during diagnosis.
It suggests that the validity of the diagnosis is poor because either it is confounded by cultural beliefs and behaviours in patients, or by a racist distrust of black patients on the part of mental health practitioners.