Chapter 5 - Anxiety and Obsessive-Compulsive & Related Disorders
Understanding Anxiety Disorders from a Multipath Perspective
Anxiety - often produces tension, worry, physiological reactivity
frequently an anticipatory emotion - sense of unease about a dreaded event or situation
anxiety might be adaptive from evolutionary perspective, prepare us for “fight or flight”
Fear - more intense emotion, unfounded fear or anxiety that interferes with daily living or produces clinically significant distress or life impairment = sign of anxiety disorder
anxiety disorders = most common mental health condition in US
Anxiety disorders disproportionately affect Latinx, African American, and transgender students, groups who traditionally experience the stress of everyday discrimination
often accompanied by depression or substance abuse
anxiety reactions like phobias can interfere w quality of life
etiological models (bio, psych, social, sociocultural) do not adequately explain why people vary in responses to fearful situations
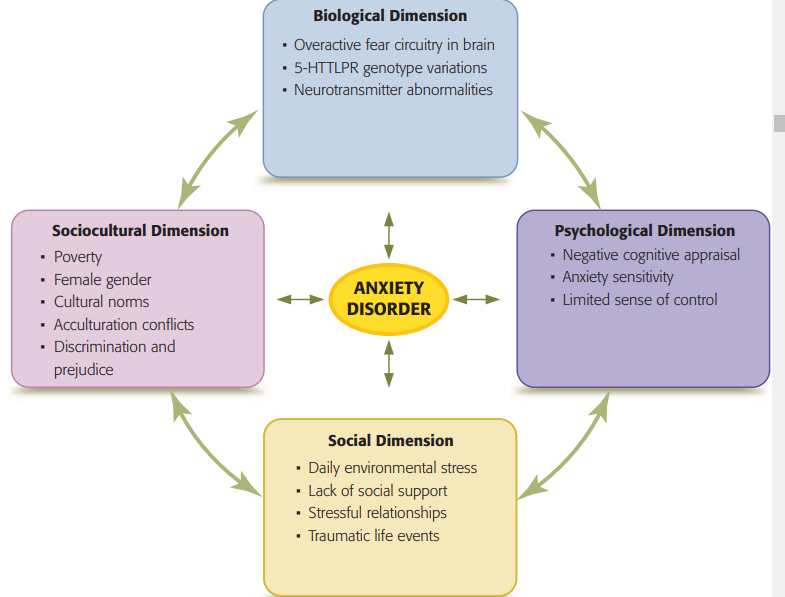
Biological Dimension
Fear Circuitry in the Brain
in situation that may affect our safety and security, two neural pathways activated
1 - amygdala, hypothalamic-pituitary-adrenal (HPA) axis → fight or flight response (prepare to defend or flee or freeze)
2 - slower pathway - sensory signals go to hippocampus & prefrontal cortex to evaluate potential danger, if determines no threat - signals sent to amygdala to stop HPA axis activity (overriding initial fear response)
when HPA axis is activated frequently, the neural connections about environmental triggers are strengthened → increased emotional reactivity like heightened or more frequent anxiety
sometimes overactivity in fear network associated with insufficient amounts of certain neurotransmitters that inhibit neural activity
reduction in GABA (reduced neural communication) activity in hippocampus and amygdala
certain medications and therapies produce a reduction in limbic activity → symptom improvement
medication appears to directly decrease activity in amygdala and “normalize” anxiety reactions
therapy appears to reduce physiological arousal by strengthening distress tolerance and ability of the prefrontal cortex to inhibit fear responses
Genetic Influences
genetic effects are most pronounced when genetic factors interact with stressful environmental influences
serotonin is strongly associated with anxiety disorders
polymorphic variation (DNA mutation) in serotonin transporter gene (5-HTTLPR) → affects length of one region of the associated alleles, possible to inherit two short alleles/two long alleles/one short and one long allele
short alleles of the (5-HTTLPR) gene are associated with both a reduction in serotonin activity and increased fear and anxiety related behaviors
long alleles of the (5-HTTLPR) gene seem to protect against negative effects from exposure to distressing circumstances
identified genes only influence an individual’s predisposition to develop an anxiety disorder → the presence of certain alleles increases the chances that a characteristic such as anxiety is expressed, actual expression of the gene depends on interactions between the genotype and the environment
Interactions between Biological and Environmental Influences
If the short allele of the 5-HTTLPR genotype is associated with anxiety, why do only some children who are carriers of this allele demonstrate persistent behavioral inhibition or significant shyness?
researchers observed and rated characteristics of behavioral inhibition in 153 children at age 14 months and again at 7 years & the mothers’ nurturing behaviors and tendency to provide social support to their children
Based on DNA genotyping, divided the children into two groups: those with and those without a short 5-HTTLPR allele
researchers found that children with the short allele showed behavioral inhibition only when they were raised in a stressful environment with low levels of maternal social support
presence of the short allele of 5-HTTLPR increases neuroplasticity in response to environmental influence
social & cultural influences (positive family, community support) → can reduce or eliminate the behavioral inhibition associated with short variant of 5-HTTLPR
Psychological Dimension
Anxiety Sensitivity - tendency to interpret physiological changes in body as signs of danger, particularly vulnerable to developing anxiety symptoms
Negative Appraisal - interpreting events as threatening even when ambiguous, likelihood of developing an anxiety disorder
Reappraisal - minimizing negative responses by looking at a situation from various perspectives, tend to demonstrate fewer anxiety symptoms if practicing this
Research - young monkeys reared in environments in which they could control access to water and food showed less fear when exposed to anxiety-provoking situations compared to monkeys without this control
sense of self-control and mastery → reduce susceptibility to anxiety
Social & Sociocultural Dimensions
daily stress can produce anxiety, especially in individuals who have biological or psychological vulnerabilities
environmental conditions such as experiencing poverty, an unsafe environment, or adverse working conditions can lead to or exacerbate anxiety
events such as terrorist attacks, school shootings, and natural disasters are also associated with increased rates of anxiety disorders
limited social support from family, friends, and peers can exacerbate these anxiety reactions
women more frequently experience anxiety disorders compared to men
due to their lack of power and status, and stressors associated with poverty, lack of respect, and limited choices
may increase production of stress hormones that increase vulnerability to both depression and anxiety
exposure to discrimination and prejudice can increase the anxiety of people who are members of ethnic minorities or other marginalized groups
One longitudinal study found that discrimination experienced by Mexican-born 5th graders living in the United States was associated with anxiety symptoms in the 12th grade, particularly among the students who continued to experience racism during their middle school and early high school years
internalized racism (consciously or subconsciously believing negative cultural messages about one’s race) has also been linked to increases in anxiety symptoms
fear over raids, discovery, or deportations has resulted in traumatic stress and anxiety for undocumented immigrants and their families and friends
acculturation conflicts also contribute to anxiety disorders among ethnic minorities
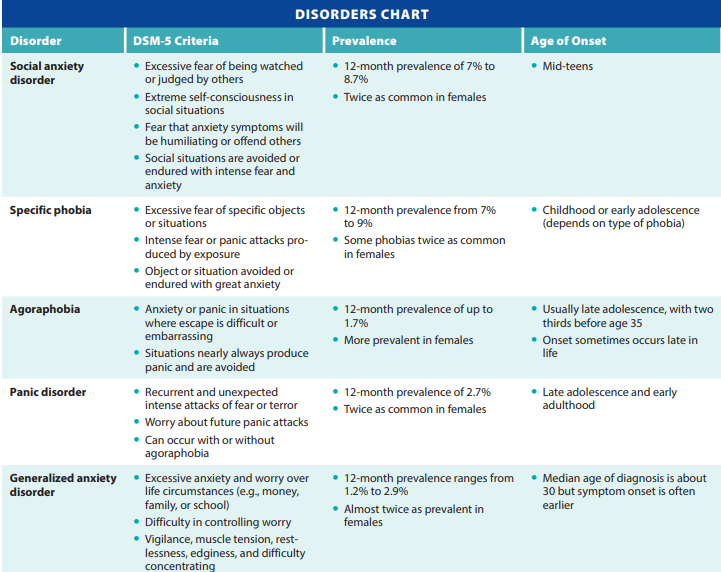
Social Anxiety Disorder - SAD
aka social phobia
criteria
fear or anxiety about 1 or more social situations in which individual is exposed to possible scrutiny
fear of displaying anxiety symptoms that will be negatively evaluated
social situations almost always provoke anxiety
social situations are avoided or endured with intense fear/anxiety
fear/anxiety is out of proportion
causes impairment
not attributable to anything else, not better explained by something
6+ months
often involves high levels of anxiety in most social situations, but some only experience it in situations where they must speak or perform in public (performance only type)
most common forms = public speaking, meeting new people
more than 48% of those with SAD rate symptoms as “mild”, but can be chronic & disabling
chronic nature of SAD within oppressed groups may be explained by the ongoing nature of everyday experiences of discrimination in social settings
comorbid with depressive disorders, substance-use disorders, suicidal thoughts or attempts
“safety behaviors” such as avoiding eye contact, talking less, sitting alone, holding a glass tightly to prevent tremors, or wearing makeup to hide blushing
those with SAD also tend to be socially submissive in an effort to avoid conflicts with others
individuals with SAD often report stressful interpersonal relationships
Etiology - Biology
between 27%-56% heritable - wide range
increased blood flow to the amygdala
underactive PFC
serotonin, dopamine
Etiology - Psychological
social learning
high standards for social performance
focus on negative aspects of social interactions, harsh evaluations
believe others are paying close attention + judging them
Etiology - Social & Sociocultural
parenting
overprotective
punitive and/or very critical
victimization by peers during childhood
i am going to be teased → gets teased → i was right
for those in treatment for social anxiety, higher level or perceived social support are associated with a more favorable prognosis
collectivistic cultures’
Treatments - Biological
SSRIs
Treatments - Psychological
exposure therapy - role play
CBT - cognitive restructuring
Specific Phobias
primary types:
living creatures
natural environment
blood/injections or injury
situational
early fears are common and most remit (disappear) without treatment
blood phobias differ from others because associated with physiological response: fainting
due to initial increase in physiological arousal followed by sudden drop in blood pressure and heart rate
Agoraphobia
intense fear of at least two of the following situations: (
a) being outside of the home alone
(b) traveling via public transportation
(c) being in open spaces (e.g., a parking lot or playground)
(d) being in stores or theaters
(e) standing in line or being in a crowd
panic attack - episode of intense fear and uncomfortable physiological symptoms
individuals with this often have anxiety sensitivity - tendency to misinterpret and overreact to normal physiological changes
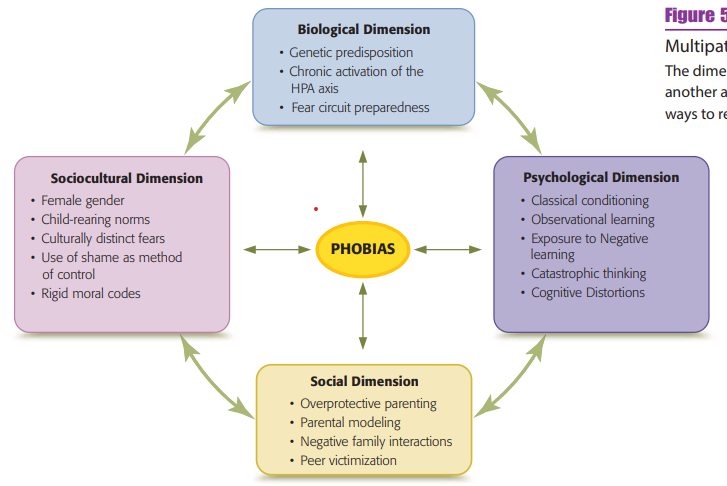
Etiology of Phobias
Biological Dimension
some individuals with phobias appear to have an innate tendency to be anxious and experience strong emotional responses - more likely to develop a phobia
Franco, 2014 - when a man underwent brain surgery designed to eliminate seizures by removing part of his left amygdala (an area associated with the storage and retrieval of frightening stimuli), he lost his intense fear of spiders. He now views them with interest, can observe them closely and even touch them. However, his fear of public speaking remained—suggesting that this fear may be processed in a different part of the amygdala
preparedness - fears do not develop randomly, easier for humans to develop fears to which we are physiologically predisposed (fears necessary to human survival), such as a fear of heights or snakes
evolutionarily prepared fears (e.g., fear of fire or deep water) occur even without exposure to traumatic conditioning experiences
Psychological Dimension
classical conditioning
Watson’s Little Albert experiment
observational learning perspective
Olsson et al., 2007 - participants in a study watched a video in which a man received an uncomfortable shock in response to a stimulus. After viewing the video, they were shown the stimulus that was associated with the shock. Not surprisingly, the participants responded with fear. Their fear response was documented by neuroimaging scans that showed activation of the amygdala
not only results in avoidance but also has been shown to affect physiological responses such heart rates
Children can develop fear responses by observing others displaying fear in real life or in the media
Burstein & Ginsburg, 2010 - parents of children ages 8 to 12 were trained to act anxiously or in a relaxed manner before their child took a spelling test
children exposed to an anxious-acting parent reported higher anxiety levels, more anxious thoughts, and a greater avoidance of the spelling test than did those in the relaxed parent condition
Van Lierde 2020 - children who watched adults display an expression of genuine pain while performing a pain-inducing task with their hands immersed in colored water developed a fear response to the color of water associated with the painful look on the adult’s face; this fear reaction did not generalize to water of a different color
Negative Information Perspective
parents were given descriptions regarding an unfamiliar animal (a cuscus) and were asked to use the information to tell their children how the cuscus might behave in certain situations. Parents received one of three descriptions:
(a) negative (has sharp claws and long teeth, can jump at your throat)
(b) ambiguous (has white teeth, can jump, likes to drink all sorts of things)
(c) positive (has nice tiny teeth, eats tasty strawberries, likes to play with other animals)
Children whose parents received the negative description reacted with more fear to the cuscus than those whose parents received positive or ambiguous information
Cognitive-Behavioral Perspective
catastrophic thoughts and cognitive distortions (including overestimating possible threat) may cause strong fears to develop
compared with people with a low fear of spiders, those who are highly fearful overestimate the size of spiders and report thinking that the spider “will attack” or “will take revenge”
Social Dimension
parental behaviors & family interaction patterns influence development of phobias & social anxiety
overprotection, lack of support for independence - insecurity & less opportunities for practice in novel situations, prevented from developing emotional regulation and coping skills
children with high levels of behavioral inhibition (social anxiety) - more vulnerable to the effects of poor parenting
victimization by peers during childhood is an unequivocal risk factor for the development of social anxiety
ongoing ostracism and bullying maintain and exacerbate social anxiety symptoms
Sociocultural Dimension
women & girls more likely to have phobias - gender difference as early as 9 yo, mostly involves repulsive animals rather than harmless animals
possibly because women show a stronger disgust response than men and because some phobic objects produce feelings of both fear and disgust
fewer gender differences for social fears, fears of bodily injury, fears of enclosed spaces
gender differences could be due to combo of biological & temperamental factors, social norms, socialization experiences
social anxiety more common in collectivistic cultures - individual behaviors seen to reflect on the entire family or group
social actions can result in higher anxiety since they implicate the individual and reflect on the family or cultural group
parents who are highly concerned about the opinions of others tend to use shame as a method of control
fear of negative evaluation by others is more common in Asian children and adolescents than in Western comparison groups
higher levels of social anxiety found in people of Asian heritage may result, in part, from discrepancies between traditional cultural behavioral norms and social expectations of the mainstream culture
social fears may be expressed differently in different cultures
Taijin kyofusho - japan, fear of offending or embarrassing others, a concept consistent with cultural emphasis on maintaining interpersonal harmony, e fearful that their appearance, facial expression, eye contact, body parts, or body odor are offensive
Treatment of Phobias
Biochemical Treatments
SSRI antidepressants - first line treatment for chronic conditions (agoraphobia & social anxiety disorder)
SNRIs & MAOIs - have some efficacy in treating those disorders
require about 4-6 weeks before they begin to reduce symptoms
Beta-blockers, medications used to treat high blood pressure and heart conditions, can also reduce the physical symptoms that accompany certain anxiety disorders, particularly social phobia
Benzodiazepines (a class of antianxiety medication) have been found to have some effectiveness for anxiety disorders
reduce symptoms of anxiety by increasing the activity of the inhibitory neurotransmitter GABA
short-acting - orazapam (Ativan) and alprazolam (Xanax), used in short-term situations such as a traveler with a fear of flying
long acting - diazepam (Valium), longer-term treatment needs
guidelines suggest prescribing benzodiazepines only for a limited period to avoid drug dependency or misuse
Cognitive-Behavioral Treatments
exposure therapy: gradually introducing the individual to the feared situation or object until the fear dissipates
applied tension - treatment of blood and injection phobia, recognize the first signs of a drop in blood pressure and then to combat this autonomic response by tensing the muscles of arms, chest, and legs until face feels warm, stop for 15-20 seconds, reapply & repeat process
virtual reality therapy - replacing real-life exposure with an immersive virtual environment, effective alternative to conventional exposure therapy
device screens can enhance the effects of exposure-based psychotherapy
systematic desensitization: exposure to the feared situation or object combined with a competing response, such as relaxation
Wolpe
a man who had a fear of urinating in restrooms when others were present. He was trained in muscle relaxation and, while relaxed, learned to urinate under the following conditions: no one in the bathroom, therapist in the stall, therapist washing hands, therapist at adjacent urinal, therapist waiting behind client. The easier items were practiced first until anxiety was sufficiently reduced
cognitive restructuring: identifying and changing irrational or anxiety-arousing thoughts associated with the phobia
help clients “normalize” social anxiety by encouraging them to question their negative thoughts, generate alternative views, and create new rational and positive thoughts regarding the situation
modeling therapy: viewing another person’s successful interactions with the feared object or situation
99 children saw a film in which a peer interacted positively with an unfamiliar animal. After watching positive peer modeling, the children’s fear toward the animal decreased significantly
Panic Disorder
for 1 month or more: recurrent unexpected panic attacks in combination with
apprehension over having another attack or worry about the consequences of an attack or
changes in behavior or activities designed to avoid another panic attack
often involve strong physiological reactions and occur without warning
cultural variations in the manner in which symptoms are expressed
panic attacks are fairly common, panic episodes often begin in late adolescence or early adulthood.
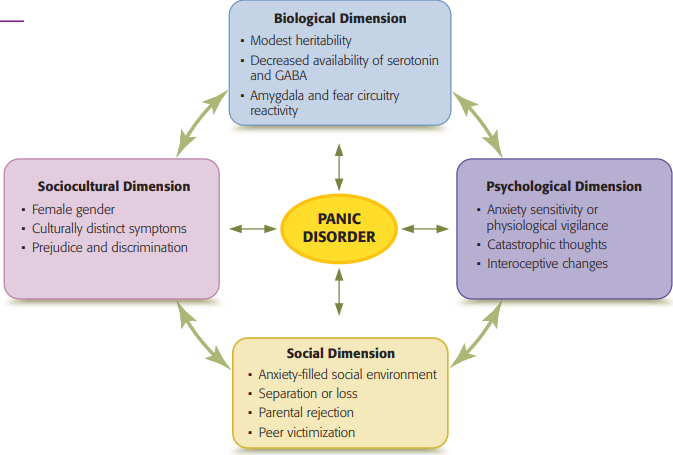
Etiology
biological dimension
higher concordance rates (percentages of relatives sharing the same disorder) in monozygotic twins compared to dizygotic twins
heritability is estimated to be between 30 and 40 percent
neurotransmitter abnormalities involving GABA and serotonin, both of which play an important role in emotions such as fear
GABA and serotonin both inhibit nerve impulses and thereby regulate neuronal excitability
hyperarousal associated with panic episodes may occur in individuals who have decreased availability of them
SSRIs, antidepressant medications designed to increase levels of serotonin, are effective in treating panic disorders, as well as other anxiety disorders
panic disorder is associated with hypersensitivity in the neural network associated with respiratory and carbon dioxide regulation
psychological dimension
cognitive-behavioral perspective: panic attacks occur when unpleasant bodily sensations are misinterpreted as indicators of an impending disaster - create a feedback loop that results in increasing anxiety
e following pattern is associated with the development of a panic disorder:
A physiological change occurs (e.g., faster breathing or increased heart rate) due to factors such as exercise, excitement, or stress
Catastrophic thoughts develop, such as “Something is wrong,” “I’m having a heart attack,” or “I’m going to die.”
These thoughts bring about increased apprehension and fear, resulting in even more physiological changes.
A circular pattern develops as the amplified bodily changes now result in even more fearful thoughts. 5.
This pairing of changes in internal bodily sensations with fear results in interoceptive conditioning—a classical conditioning process in which fear is associated with the perception of bodily changes. As this association strengthens, somatic changes can automatically produce panic attacks.
social & sociocultural dimensions
modeling - watching family or friends express fears about physical sensations or use avoidance to cope with fear-producing situations
many individuals with panic disorder report a stressful childhood involving separation anxiety, family conflicts, school problems, or loss of a loved one
parental rejection is a risk factor for panic disorder among adolescents and young adults
exposure to racial or ethnic-based discrimination is also associated with panic attacks
being a victim of bullying also increases vulnerability to developing panic disorder
Treatment
Biochemical Treatment
SSRI antidepressants - first choice, 4-6 weeks to become fully effective
Tricyclic antidepressants
Benzodiazepines - reduce frequency of panic attacks, long-term use is problematic because of dependency issues, sedation effects, cognitive impairment
up to 45 percent of individuals with panic disorder are not responsive to medication
among those who report improvement, one fourth to one half find that their symptoms return when their medication is discontinued
Cognitive-Behavioral Treatment
successful in producing long-term decreases in panic symptoms
steps:
Educating the client about panic disorder and correcting misconceptions regarding the symptoms
Identifying and correcting catastrophic thinking—for example, the therapist might comment, “Maybe you are overreacting to what is going on in your body” or “A panic attack will not stop your breathing”
Teaching the client to self-induce physiological symptoms associated with panic (such as hyperventilating or breathing through a straw) in order to extinguish the interoceptive bodily cues
Instructing the client on breathing techniques that will prevent hyperventilating during a panic attack
Encouraging the client to emotionally face rather than resist the symptoms, both within the session and in the outside world, using statements such as “Allow your body to have its reactions and let the reactions pass”
Reviewing the skills acquired and making a plan to prevent relapse
intervention extinguishes the fear associated with both internal bodily sensations and fear-producing environmental situations
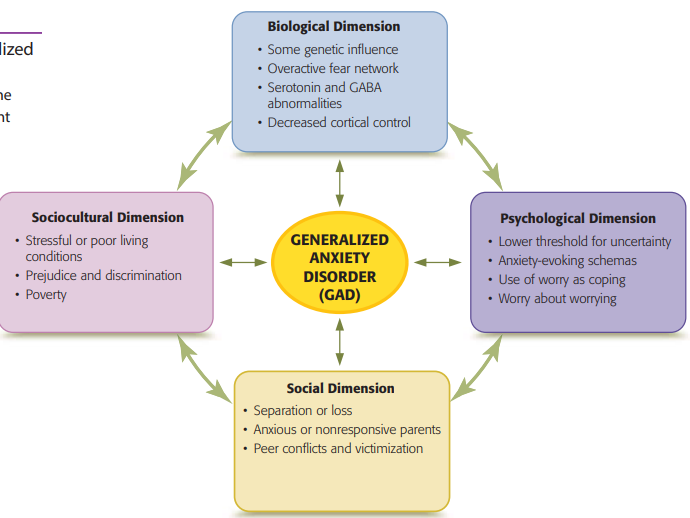
Generalized Anxiety Disorder (GAD)
the symptoms must be present on the majority of days for at least 6 months and cause significant distress or impairment in life activities
Etiology
Biological Dimension
familial and twin studies suggesting heritability of 31 percent (Gottschalk & Domschke, 2017)
Genes associated with anxiety are often expressed in terms of serotonin or GABA abnormalities or overactivity of the HPA axis
irregularities within the limbic system and prefrontal cortex—excessive physiological reactivity combined with failure of the prefrontal cortex to dampen the emotional centers of the brain
Psychological Dimension
role of dysfunctional thinking and beliefs
lower threshold for uncertainty, which leads to worrying and a focus on bodily changes
two types of worry
frequent use of worry to cope with stressful events or situations that might occur
constantly generating solutions to “what if” scenarios (worrying about worrying) - leads to belief that worry is uncontrollable, harmful, and dangerous
One model identifies three interconnected processes that maintain the uncontrollable worry associated with GAD:
Interpretation bias - when ambiguous situations are interpreted negatively
Automatic attentional bias for negative information, focus on negative info and potential negative outcomes
Impaired attentional control, people with GAD have difficulty shifting attention away from worrisome thoughts
Social & Sociocultural
Mothers who themselves have anxiety symptoms may be less responsive and engaged with their infants than mothers who are not anxious - increase likelihood that the child develops GAD
conflict in peer relationships, victim of bullying, stressful conditions - poverty, poor housing, prejudice, systemic racism
Treatment
Benzodiazepines - but, GAD is chronic and drug dependence is a concern
If medication is necessary, antidepressants are usually preferred because they do not have the potential for the physiological dependence
CBT effective psychological treatment for GAD
reducing pathological worry
60% - demonstrating significant improvement that continued 12 months after treatment
CBT has been specifically adapted to treat the dysfunctional cognitive processes that maintain the cycle of worry associated with GAD
therapists encourage clients to:
selective focus on negative concerns and to use attentional control to replace this unhelpful practice with more useful habits
Keep a record of all worries, determining whether a negative outcome actually occurred in any of the worrisome situations
Develop habits of mental self-control including monitoring and challenging irrational thinking and substituting
Create “worry free zones” by deliberately moving attention away from worry to the task at hand
Use muscle relaxation
Keep a positive data log of situations in which the use of adaptive skills has resulted in reduced anxiety
Mindfulness practices can enhance the effectiveness of CBT in the treatment of GAD
remain nonjudgmental in the presence of anxiety—accepting any emotions and bodily sensations that arise
Obsessive-Compulsive and Related Disorders
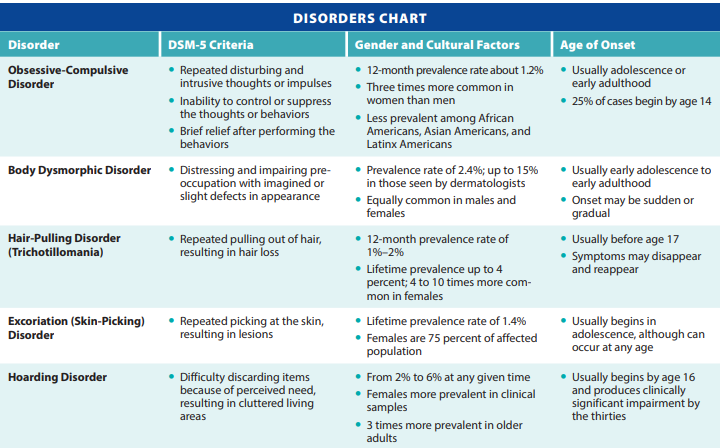
Obsessive-Compulsive Disorder
Obsessions - persistent, anxiety-producing thoughts or images
common themes associated with obsessions include:
contamination (dirt, germs, body wastes, or secretions, and fear of being polluted by contact with items, places, or people considered to be unclean or harmful
errors or uncertainty, obsessing over decisions, anxiety over daily behaviors
unwanted impulses
orderliness, perfect order or symmetry
Compulsions - involve an overwhelming need to engage in activities or mental acts to counteract anxiety or prevent the occurrence of a dreaded event
handwashing, checking, ordering objects
mental acts like praying, counting, repeating words silently
The obsessions and compulsions consume at least 1 hour of time per day and cause significant distress or impairment in life activities.
obsessions are often accompanied by sensory experiences
Distress or anxiety occurs if the behavior is not performed or if it is not done “correctly.”
only 25 percent of those with OCD report distressing obsessions without compulsive behaviors
Compulsions are frequently performed to neutralize or counteract a specific obsession
between 9 percent and 25 percent of the general population report having obsessive-compulsive symptoms, but without the severity required to meet the diagnostic criteria for OCD
with OCD, the obsessions last longer, are more intense, more upsetting, produce more discomfort, and are more difficult to dismiss
Mild compulsions include superstitions such as refusing to walk under a ladder, throwing salt over one’s shoulder, or knocking on wood. In individuals with OCD, the compulsions are much more frequent and intense, and they produce discomfort
behaviors are repetitive and are often conducted in a mechanistic fashion
if compulsive acts are not performed in a certain manner or a specific number of times, anxiety occurs
Hoarding Disorder
diagnosed when
an inability to discard items regardless of their value
a perceived need for items and distress over the thought of giving or throwing them away
an accumulation of items that produces congestion and clutter in the living area
distress or impairment in life activities or interferes with safety within the home
Social pressure to discard possessions or cease hoarding is distressing - irrational emotional attachment to the items
tend to have more difficulties with attention and memory, which has led to the hypothesis that individuals with hoarding disorder may cling to their possessions in order to avoid forgetting
ranges from 2 percent to 6 percent of adults and typically begins by late adolescence
more common among women and is most prevalent in older adults
up to 25 percent of individuals with anxiety disorders report significant hoarding symptoms
Body Dysmorphic Disorder
DSM-5 criteria:
preoccupation with a perceived physical defect in a normal-appearing person or excessive concern over a slight physical defect
repetitive behaviors such as checking one’s appearance in mirrors, applying makeup to mask “flaws,” and comparing one’s appearance to those of others
significant distress or impairment in life activities due to these symptoms
focuses on bodily features such as excessive hair, lack of hair, or the size or shape of the nose, face, or eyes
not better explained by concerns with body fat or weight
specify:
with muscle dysmorphia
level of insight
age of onset = 16yo
may be underdiagnosed because individuals feel embarrassed or ashamed about bringing attention to their “problem”
some individuals with BDD recognize that their beliefs are untrue, up to half maintain strong delusions (false beliefs) about their bodies
Up to 60 percent of individuals with BDD undergo unnecessary cosmetic surgeries
tend to be dissatisfied with the results
more likely than other patients to sue the doctor
The prevalence of BDD ranges from 0.7 percent to 2.4 percent in community samples
Sixty percent of individuals with BDD have experienced an anxiety disorder, including 38 percent who have social anxiety
BDD tends to be chronic and difficult to treat due to comorbidity with depression and substance abuse
About 70 percent of individuals with BDD have poor insight into their condition, which makes attempts to change their delusional beliefs very challenging
CBT useful
Muscle dysmorphia, the belief that one’s body is too small or insufficiently muscular, is a specific type of BDD
Some bodybuilders who show a pathological preoccupation with their muscularity also suffer from BDD; these individuals have high body dissatisfaction and show negative biases and emotions even when observing parts of their body that are large and very muscular
etiology - biological: genetics, serotonin, brain activity when processing visual stimuli (including faces)
etiology - social/sociocultural: social media, excessive selfie-use = safety behavior
treatments - biological: SSRIs, symptoms come back when off meds
treatments - psychological: CBT (maladaptive cognitions about body), ERP (feared situations concerning body)
Hair-Pulling Disorder (Trichotillomania)
recurrent & compulsive hair pulling despite repeated attempts to stop the behavior
results in hair loss and significant distress
common areas - scalp, eyebrows, pubic region
occur sporadically throughout day or continue for hours at a time
may be precipitated by boredom, stress, anxiety
sometimes relieves tension or is pleasurable
occurs with some consciousness but often an automatic act
lifetime prevalence of 4 percent
women 4-10x more likely of developing the disorder
many younger children outgrow common hair pulling
up to 11 percent of college-aged individuals continue to pull their hair occasionally
often comorbid with major depressive disorder and skin excoriation disorder
Excoriation (Skin-Picking) Disorder
repetitive and recurrent picking of the skin that results in skin lesions
spend 1 hour or more per day thinking about, resisting, or actually picking the skin
preceded by rising tension; picking results in feelings of relief or pleasure
diagnosis only when the behavior causes clinically significant distress or impairment and when there are repeated unsuccessful attempts to decrease or stop the behavior
1.5 percent in adults and is most prevalent during early adolescence, although the onset for some individuals is during middle age
later onset tend to have less severe symptoms
About three quarters of individuals with this disorder are women or girls
often comorbid with depression, OCD, anxiety disorders, BDD, or trichotillomania
individuals with excoriation disorder report psychosocial impairment and an impaired quality of life
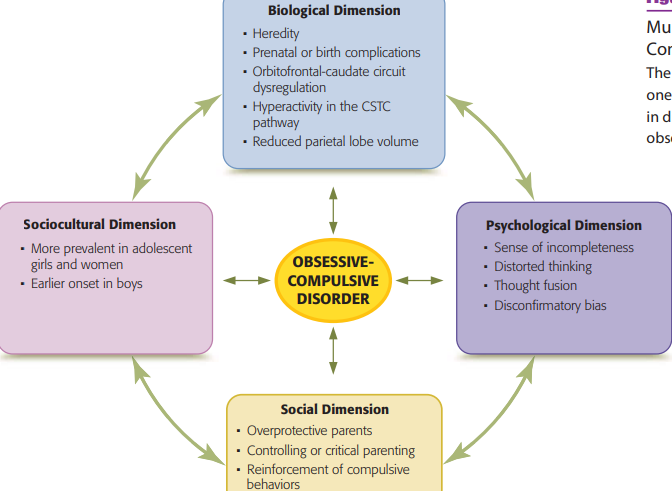
Etiology of Obsessive-Compulsive and Related Disorders
Biological Dimensions
although heredity is involved in OCD, with the greatest risk of OCD occurring in first-degree relatives, nonshared environmental influences are equally important
Genetic factors are also involved in
body dysmorphic disorder
compulsive hoarding
skin-picking disorder
environmental factors play a greater role in their etiology compared with OCD
smoking during pregnancy, cesarean section delivery, preterm birth, unusually low or high weight at birth, and breech presentation at labor
OCD involves alterations in brain structures and neural networks as well as atypical and complex patterns of interactions between separate areas of the brain
First-degree relatives of individuals with OCD show impairment in decision making, planning, and mental flexibility, so these cognitive characteristics may represent an endophenotype for the disorder
OCD is also associated with less volume in certain regions of the prefrontal cortex, most notably the parietal lobe (a brain structure associated with attention, planning, and response inhibition)
Symptoms of OCD are also consistent with dysregulation of the orbitofrontal caudate circuit
alerts the rest of the brain when something is wrong → the amygdala and the HPA axis become activated creating feelings of anxiety → when this system becomes hyperactive, the feeling that something is not right can lead to the sensation that something is “deadly wrong” and needs to be corrected
caudate nuclei, which process information based on memories of prior experiences, may then become overwhelmed and unable to flexibly shift to other activities
those with the disorder have excessive neural connectivity within the cortico-striatal-thalamo-cortical (CSTC) pathway—a looping brain network (connecting the cortex, striatum, and thalamus) that is associated with movement and habit formation
dysfunctional brain circuitry in this area can influence OCD symptoms due to their association with movement, emotion, and memory
Psychological Dimension
Some researchers maintain that obsessive-compulsive behaviors develop because they reduce anxiety
If certain thoughts or behaviors become associated with an unpleasant event, they can become a conditioned stimulus. Because these actions or thoughts are unpleasant, individuals may develop behaviors that help them avoid the initial unpleasant event. These avoidance behaviors reduce anxiety and are thus reinforcing
Individuals with OCD show certain cognitive characteristics, including distorted thinking in the following areas:
Exaggerated estimates regarding the probability of harm
Control
Intolerance of uncertainty
thought-fusion, in which distressing thoughts regarding
(a) an action (e.g., shouting obscenities during church services)
(b) an event (e.g., thoughts of an injury to a loved one)
(c) an object (e.g., seeing a black cat means misfortune) become “fused” with the action, event, or object
having these thoughts produces the same distressing emotions as if the event occurred or the actions were carried out
a disconfirmatory bias—that is, they search for evidence that might show that they failed to perform the ritual correctly
unable to trust their own memories or judgment and feel a need to determine whether they actually performed the behavior or performed it “correctly.”
may need to repeat the ritual multiple times until it is “just right.”
Cognitive influences or beliefs also play an important role in hoarding disorder. Individuals with this disorder appear to have the conviction that objects they collected have some type of intrinsic, instrumental or sentimental value
Social & Sociocultural Dimensions
family variables - controlling parents, overly critical parents, little parental warmth, discouragement from autonomy
negative reactions to OCD symptoms can increase symptom severity
symptoms also increase when loved ones provide assistance or reassurance regarding the rituals
temp. reduce stress but…
reinforce or prolong symptoms
contribute to poorer treatment outcome
living with a partner or family member with OCD can produce a shared psychopathology in which two individuals develop the same OCD symptoms
Treatment
Biological
antidepressant medications that increase serotonin availability - SSRIs
only about 60% with OC respond to SSRIs and often relief is only partial
antipsychotics
deep brain stimulation - research continues about optimal brain regions to stimulate and if specific symptoms should guide those decisions
Behavioral
combo of exposure & response prevention (ERP - Exposure & Response Prevention)
effective in reducing symptoms
lower relapse rate compared to treatment by medications
exposure therapy involves actual or imagined exposure to an anxiety-arousing situation, can be gradual or flooding
response prevention involves not allowing the individual with OCD to perform the compulsive behavior once urge is activated
steps in exposure therapy with response prevention generally include
psychoeducation about OCD and the rationale for exposure and response prevention
development of an exposure hierarchy (from somewhat fearful to most-feared situations)
exposure to feared situations (such as contact with the restroom floor) until anxiety has diminished
prevention of the performance of compulsive rituals such as hand washing after exposure to the cues that trigger the compulsion
repeated exposure to a variety of triggering situations without performing compulsive ritual
review of relapse prevention strategies
CBT - correcting dysfunctional beliefs
up to 30 percent of those treated with CBT for OCD do not achieve symptom relief
cognitive behavioral treatments appear to induce neuroplasticity that results in more functional connectivity
modified to treat the specific features of hoarding disorder
motivational interviewing to increase readiness for change
graded exposure involving opportunities to resist the urge to acquire items
identification and correction of maladaptive beliefs about the need for specific possessions
practice in sorting and discarding items
placement of retained items in appropriate places in the home to encourage continued decluttering
CBT for the treatment of skin-picking and trichotillomania
training in awareness of and self-monitoring for the undesirable behavior
habit-reversal training, which involves practicing a competing and incompatible response (such as fist clenching) when the hair-pulling or skin-picking urge occurs
CBT-BDD program that focused on the “core” components of the disorder
motivational enhancement to address ambivalence about complying with treatment
cognitive restructuring focused specifically on negative thoughts about personal appearance
exposure and response prevention focused on eliminating mirror checking, seeking reassurance, and the camouflaging of imagined defects
mindfulness training focused on learning to observe and describe one’s body without judgment
also, move away from self-focus, pay attention to others/environment, base self-esteem on qualities like being a good friend and not physical attractiveness
Contemporary Trends and Future Directions
specialized therapy programs
specific to the needs of those with anxiety and obsessive-compulsive disorders
those who refuse treatment
those who have not benefited from traditional methods of treatment
use of technology to predict response to therapy
interested in determining if there are physiological, demographic, or clinical characteristics that can be used to predict responsiveness to therapy
Frick et al (2020)
group of 47 individuals with social anxiety disorder who were treated either with CBT plus SSRIs or with CBT plus placebo
cortex and the amygdala anterior were scanned during cognitive interference task prior to treatment
which data had the highest level of accuracy in differentiating between participants who responded or didn’t respond to each type of intervention
only one variable—reactivity of the anterior cingulate cortex during the cognitive interference task— predicted treatment response - 83%
Treatment Protocols for Multiple Disorders
Farchione et al. (2012) argued against the “proliferation of diagnosis-specific treatment manuals, many of which have only minor and somewhat trivial variations in treatment procedures”
the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders, which is a CBT program that is applicable to all anxiety and depressive disorders
targets aspects of emotional processing and regulation and consists of five modules focusing on
increasing present emotional awareness
increasing cognitive flexibility
identifying and preventing patterns of emotion avoidance
increasing awareness and tolerance of emotion-related physical sensations
exposure to physiological and emotional triggers
 Knowt
Knowt