Ch5 - Tissues - Introduction to Histology
Instructor Information
Dr. Nusrat Sajid
Course: Bio25 Anatomy and Physiology
Institution: Carrington College
Outline of Tissue Types
5.1 Epithelial tissue: Covers body surfaces and lines cavities.
5.2 Connective tissue: Supports and binds other tissues.
5.3 Muscle tissue: Responsible for movement.
5.4 Nervous tissue: Transmits nerve impulses.
5.5 Tissue integration: Discusses how tissues work together to form organs and membranes.
5.6 Processes: Development, change, aging, and the role of tissue death in the body.
Introduction to Histology
Definition of Tissues: Tissues are defined as groups of similar cells and their supporting extracellular matrix working together to perform specific functions essential for the organism's survival.
Types of Tissues:
Epithelial: Forms protective barriers and is involved in absorption, secretion, and sensation.
Connective: Provides structure and support, stores energy, and transports substances.
Muscle: Facilitates body movements through contraction and relaxation.

Nervous: Responsible for transmitting signals throughout the body, ensuring communication between different systems.

Summary of Composition and Function of Tissues
Epithelial Tissue:
Structure: Composed predominantly of tightly packed cells with minimal extracellular matrix, allowing for protective functions.
Function:
Essential for providing barriers, facilitating absorption, secretion, and sensation in various organs.
protection from pathogens
absorption of nutrients
secretion of substances
sensation.
Subtypes:
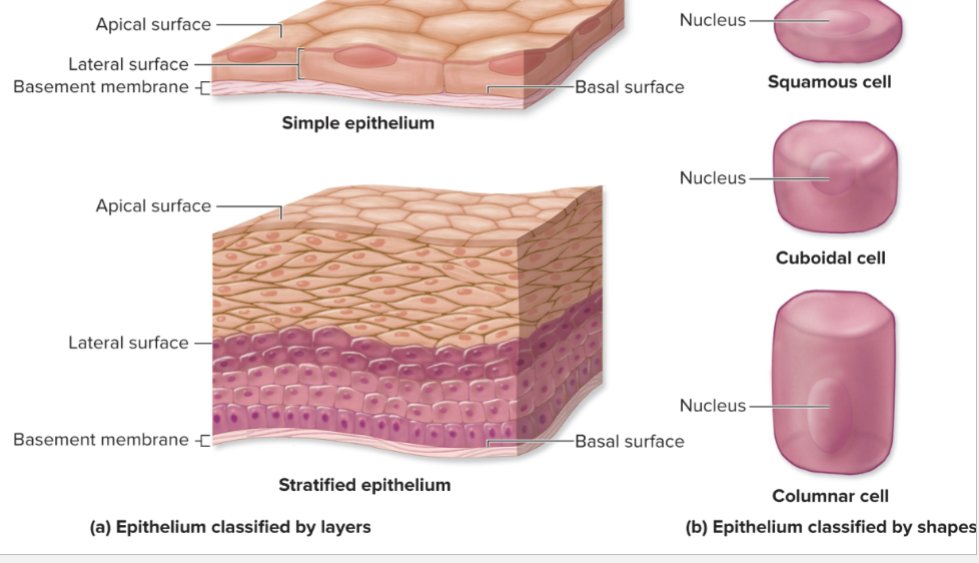
Simple Epithelia: Single layer of cells (squamous, cuboidal, columnar) allowing for more efficient exchange of materials.
Stratified Epithelia: Multiple cell layers providing enhanced protection against physical and chemical abrasions.
Connective Tissue:
Structure: A diverse group characterized by the presence of a significant amount of extracellular matrix comprised of protein fibers (collagen, elastin) embedded in a ground substance.
Function: Functions include binding and supporting other tissues, insulating and storing energy, and facilitating transport (e.g., blood).
Subtypes:
Various forms such as proper (loose and dense)
specialized (adipose, cartilage, bone, blood).
Muscle Tissue:
Structure: Composed of elongated cells, capable of contracting to enable movement.
Function: Primary function is for movement; categorized into voluntary (skeletal) and involuntary (smooth and cardiac) types, essential for bodily functions.
Nervous Tissue:
Structure: Primarily made up of neurons (nerve cells) and supporting glial cells, which are essential for the proper function of the nervous system.
Function: Responsible for transmitting and processing electrical signals, facilitating communication between different body parts.
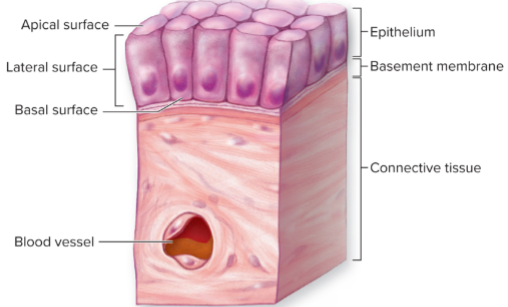
Characteristics of Epithelium
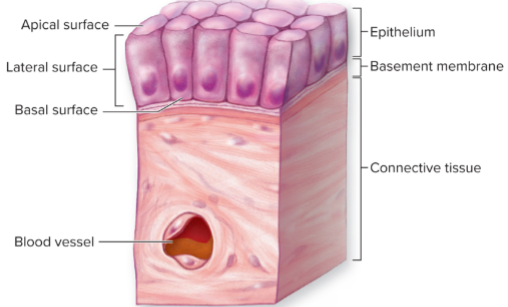
Characterized by closely packed cells with minimal extracellular matrix, enhancing their protective functions.
Functions: Serves multiple roles such as covering body surfaces, lining internal cavities, and forming glandular structures.
Polarity:
Apical Surface: Exposed to external environment or internal body space, may be equipped with microvilli for absorption or cilia for movement.
Lateral Surface: with intercellular junctions
Basal Surface: Anchored to the basal membrane, connecting to underlying connective tissue.
Nerves: Highly innervated tissue aiding in sensory reception despite lack of blood vessels (avascular).
Regeneration: These tissues exhibit a high capacity for regeneration, critical for maintaining their integrity.
Functions of Epithelial Tissue
Protection:
Guards against dehydration, mechanical impacts, and invasion by pathogens.
Absorption:
Selectively allows for the transport of essential substances into the body, such as nutrients in the intestines.
Secretions:
Glandular epithelium plays a crucial role in producing and releasing various substances, including enzymes and hormones.
Sensations:
Works closely with the nervous system to relay information regarding the external environment, crucial for reflex actions and responses.
Tissue Types Continued:
5.1 Epithelial Tissue (Continued):
Classification of Epithelial Tissues:
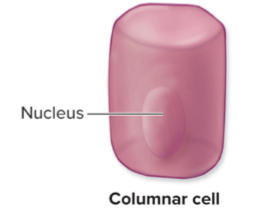
Squamous Cell:
- Flat, wide, irregular in shape. Nucleus flat
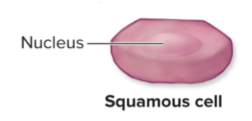
Cuboidal Cells:
About tall and Wide, Nucleus spherical. Center of cell
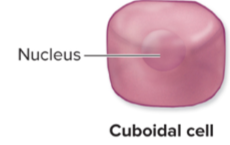
Columnar Cells:
Slender and taller than Wide. Nucleus oval; oriented lengthwise in basal region.
Transition Cells:
Can change shape, depend on stretch of epithelium
Organization and relationship of Epithelium Types
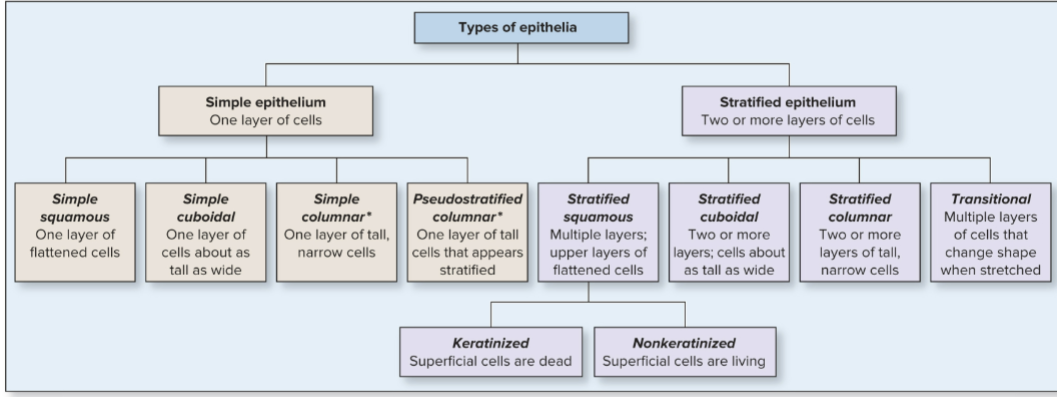
Types of Epithelial Tissue: Each type serves different functions based on location and structure.
5.1D: Types of Epithelial Tissue
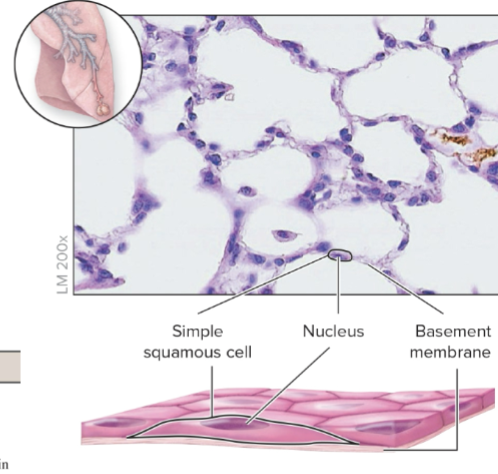
Simple Squamous Epithelium:
Structure: Composed of a single layer of flat cells, facilitating rapid diffusion and filtration processes.
Location: Found in areas where passive diffusion occurs, such as alveoli of lungs (for gas exchange), endothelium of blood vessels (reducing friction), and mesothelium lining body cavities.
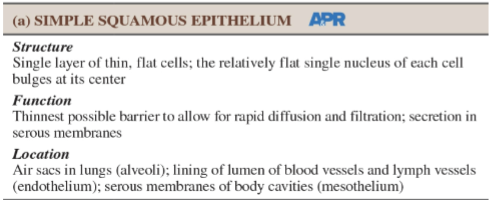
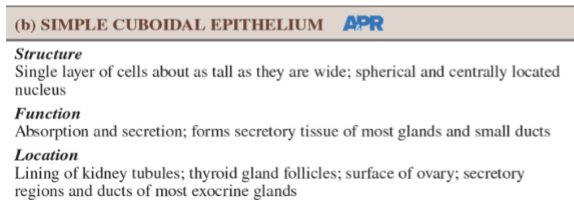
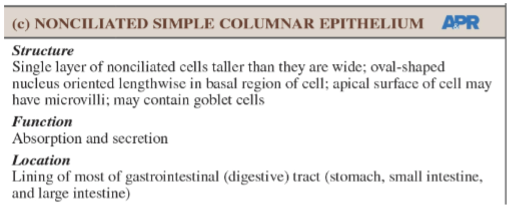
Simple Cuboidal Epithelium:
Structure: Composed of cube-shaped cells that are suited for secretion and absorption.
Location: Commonly located in kidney tubules, ducts of small glands, and on the surface of the ovaries, playing key roles in urine production and glandular functions.
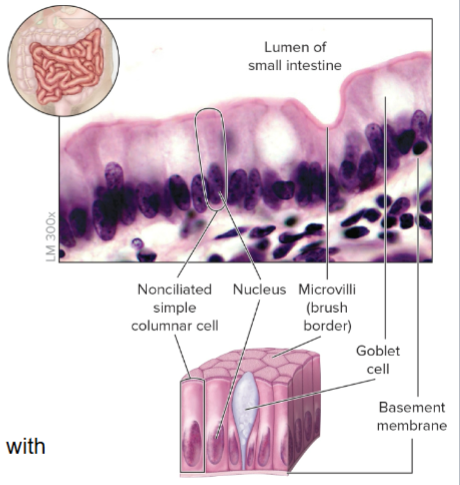
Non-ciliated Simple Columnar Epithelium:
Structure: Features tall, column-like cells that often have microvilli and goblet cells.
Function: Enhances nutrient absorption and secretion of digestive enzymes and mucus in the gastrointestinal tract.
Location: Lines most of the digestive tract from the stomach to the anal canal, with microvilli creating a brush border to increase surface area.
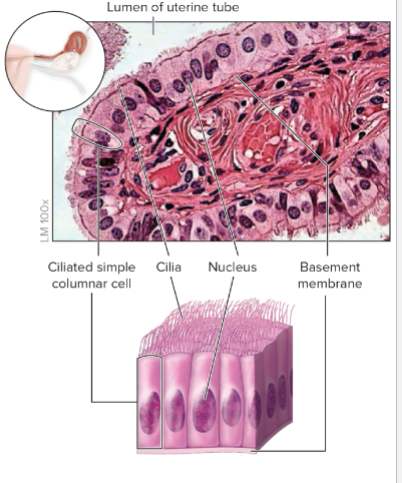
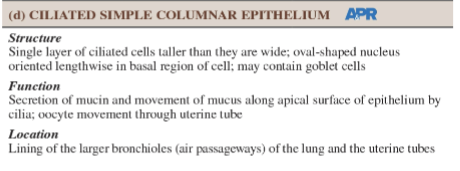
Ciliated Simple Columnar Epithelium:
Structure: Contains cilia on the apical surface aiding in movement of mucus and other substances.
Function: Moves mucus and foreign particles out of the respiratory tract, helping keep airways clear.
Location: Found in the respiratory tract and fallopian tubes.
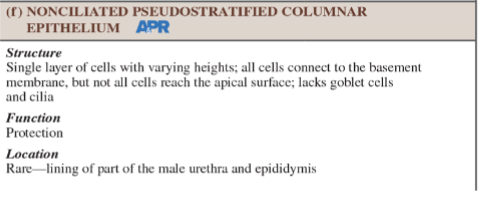
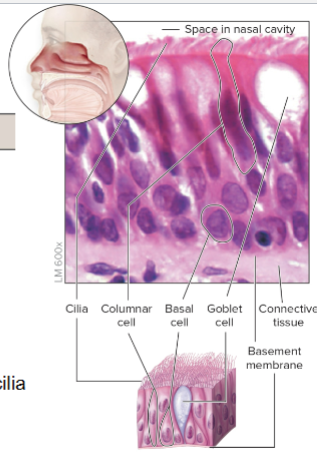
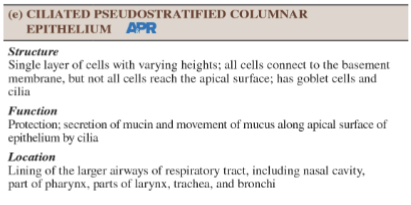
Pseudostratified Columnar Epithelium:
Structure: Appears stratified due to cell height variation but is a single layer of cells with differing heights.
Function: Primarily functions to secrete mucus and protect underlying tissues; mucous transport aided by ciliary action.
Location: Common in the respiratory tract where goblet cells help trap particles.

Stratified Squamous Epithelium:
Structure: Composed of multiple layers of cells to offer robust protection.
Keratinized Variety: Found in the skin, providing a tough barrier against abrasion and water loss.
Non-Keratinized Variety: Found in linings of the mouth and esophagus, protecting underlying tissues from mechanical stress and pathogens.
Transitional Epithelium:
Structure: Specialized to allow stretching; features cells that can change shape from cuboidal to squamous as they stretch.
Function: Supports expansion and contraction of the urinary bladder.
Location: Lines the urinary bladder, ureters, and part of the urethra, allowing for significant changes in volume without compromising integrity.
5.2 Connective Tissue
Overview
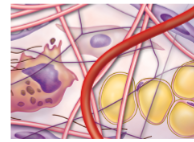
Description: Connective tissue is one of the four primary types of tissue in the body. It provides structural support, binds other tissues together, and plays multiple roles in transport, defense, and energy storage. It is characterized by a large amount of extracellular matrix relative to the cellular component, allowing it to perform diverse functions.
5.2A: Composition of Connective Tissue
Cells: Various cell types are present in connective tissue, including:
Fibroblasts: These are the most common cells, responsible for synthesizing fibers (collagen, elastin) and the ground substance.
Adipocytes (Fat Cells): Store energy in the form of lipids and contribute to insulation and cushioning of organs.
Macrophages: Derived from monocytes, these immune cells engulf and digest cellular debris and pathogens.
Mast Cells: Contain granules rich in histamine and other mediators that play a role in allergic responses and inflammation.
White Blood Cells: Participating in the immune response, wandering cells that can migrate to sites of infection or injury.
Matrix Composition: The matrix consists of:
Fibers:
Collagen Fibers: Thick fibers providing tensile strength, making tissues resistant to stretching.
Elastic Fibers: Composed of the protein elastin; these fibers allow tissues to return to their original shape after stretching.
Reticular Fibers: Fine, branched fibers that form a supportive network in soft tissues and organs.
Ground Substance: A gel-like material that fills the spaces between cells and fibers, which consists of:
Proteoglycans: Large molecules that trap water to form a gel-like matrix.
Glycoproteins: These help in cellular adhesion and signaling.
Water: Serves as a medium for transport and communication between cells.
5.2B: Types of Connective Tissue
Loose Connective Tissue:
Description: Characterized by a generous amount of ground substance and a loose arrangement of fibers.
Examples:
Areolar Tissue: Holds organs in place and provides a reservoir of water and salts.
Adipose Tissue: Stores energy, provides insulation, and cushions organs.
Reticular Tissue: Supports soft organs like the liver, spleen, and lymph nodes.
Dense Connective Tissue:
Description: Contains high concentrations of collagen fibers that provide strength and resistance to tension.
Subtypes:
Dense Regular Connective Tissue: Fibers are arranged in a parallel fashion, providing strong structural support; found in tendons (connect muscle to bone) and ligaments (connect bone to bone).
Dense Irregular Connective Tissue: Fibers are arranged irregularly, allowing for multidirectional strength; found in the dermis of the skin and joint capsules.
Specialized Connective Tissue:
Bone:
Structure: Composed of bone cells (osteocytes) within a mineralized matrix, offering strength and support.
Function: Protects organs, supports the body, facilitates movement, and serves as a reservoir for minerals.
Cartilage:
Types:
Hyaline Cartilage: Most common type, found on the ends of long bones, in the nose and trachea, providing flexible support.
Elastic Cartilage: Contains many elastic fibers allowing flexibility; found in the ear and epiglottis.
Fibrocartilage: Contains thick collagen fibers, providing tensile strength; found in intervertebral discs and symphysis pubis.
Blood:
Structure: Liquid matrix called plasma, containing red blood cells, white blood cells, and platelets.
Function: Transport nutrients, gases, and waste, and play a key role in immune responses.
5.2C: Functions of Connective Tissue
Support: Provides physical support to other tissues and organs, maintaining overall structure.
Binding: Connects various tissues and organs, ensuring they work together effectively; e.g., tendons binding muscle to bone.
Transport: Blood transports oxygen, carbon dioxide, nutrients, and waste throughout the body, providing a vital link between systems.
Storage: Stores energy reserves in adipose tissue and minerals (calcium phosphate) in bone.
Defense: Helps protect against infection and injury with the action of immune cells like macrophages and mast cells.
5.2D: Healing and Repair of Connective Tissue
Inflammation: Upon tissue injury, inflammation occurs, characterized by redness, heat, swelling, and pain. This is due to increased blood flow and the influx of immune cells to the affected area.
Regeneration: Involves the proliferation of fibroblasts that synthesize collagen and extracellular matrix to repair the tissue. New connective tissue may form, contributing to the healing process.
Scar Formation: If the damage is significant, incomplete repair may lead to scarring. Scar tissue (fibrous tissue) replaces normal tissue, which may alter the function depending on the extent and location of the damage.
Detailed and Elaborated Notes from Page 5-72
5.1 Epithelial Tissue
Overview: Epithelial tissue forms the protective layer of the body, covering surfaces and lining cavities, with specialized functions related to absorption, secretion, and sensation.
5.1A: Composition and Function of Epithelial Tissues
Structure: Epithelial tissues are composed mainly of closely packed cells with minimal extracellular matrix (ECM), allowing for tight junctions and a barrier against pathogens. Depending on the location and function, epithelial cells can be organized in single (simple) or multiple (stratified) layers.
Key Functions:
Protection: Acts as a barrier against mechanical injury, pathogens, and harmful chemicals.
Absorption: Facilitates uptake of nutrients and substances, particularly in the intestines.
Secretion: Includes mucus, hormones, and enzymes produced by glandular epithelium.
Sensation: Contains sensory nerve endings that receive external stimuli.
5.1B: Characteristics of Epithelial Tissue
Regeneration: Epithelial tissues have a high capacity for renewal and regeneration, which is crucial for maintaining their integrity in response to injury.
Polarity:
Apical Surface: Exposed side facing the body exterior or cavity, often has microvilli or cilia for specific functions like absorption and movement respectively.
Lateral Surface: Contains intercellular junctions, such as tight junctions, gap junctions, and desmosomes, which provide structural integrity and communication between cells.
Basal Surface: Anchors epithelial tissue to the underlying connective tissues via the basement membrane, which aids in nutrient exchange and structural support.
5.1C: Functions of Epithelial Tissue
Protection: Shields underlying tissues from dehydration, mechanical injury, and microbial invasion.
Absorption: Active uptake of nutrients, electrolytes, and water in organs like the intestines.
Secretion: Glandular epithelium functions in the production of essential substances, such as digestive enzymes and hormonal products.
Sensory Reception: Works with the nervous system to convey information about external environments, crucial for homeostasis.
5.1D: Types of Epithelial Tissue
Simple Squamous: Flat epithelial cells; permits easy diffusion; found in areas like alveoli and blood vessels.
Simple Cuboidal: Cube-shaped cells adapted for secretion and absorption; primarily located in kidney tubules and glands.
Non-ciliated Simple Columnar: Taller column-like cells with microvilli; enhances absorption in the digestive tract.
Ciliated Simple Columnar: Contains cilia to move mucus and debris; found in the respiratory tract and fallopian tubes.
Pseudostratified Columnar: Appears layered but is a single layer; functions in mucus secretion and is found in the respiratory tract.
Stratified Squamous: Multiple layers for added protection; keratinized forms make up the skin, while non-keratinized types line the mouth and esophagus.
Transitional Epithelium: Specialized to stretch; lines urinary bladder, allowing for significant volume change without loss of integrity.
5.2 Connective Tissue
Overview: Connective tissue encompasses a broad range of tissues supporting, binding, and protecting other tissues and organs throughout the body.
5.2A: Composition of Connective Tissue
Cells: Major cell types include:
Fibroblasts: Produce fibers and ground substance components, crucial for maintaining the ECM.
Adipocytes: Store fat and provide insulation and cushioning for organs.
Macrophages: Specialized immune cells that protect against pathogens and facilitate tissue repair.
Mast Cells: Release histamine and other mediators involved in the inflammatory response.
White Blood Cells: Involved in immune responses, migrate to areas of infection or injury.
Matrix Components:
Fibers:
Collagen Fibers: Provide tensile strength and withstand stretching.
Elastic Fibers: Offer flexibility and allow tissues to return to their original shape after deformation.
Reticular Fibers: Form supportive networks in soft tissues and organs.
Ground Substance: A gel-like material consisting of proteoglycans, glycoproteins, and varying amounts of water, which fills the intercellular spaces and facilitates communication and transport.
5.2B: Types of Connective Tissue
Loose Connective Tissue:
Description: Provides support with a relatively high proportion of ground substance and lower fiber concentration.
Examples:
Areolar Tissue: Holds organs in place and acts as a reservoir for water and salts.
Adipose Tissue: Stores energy and provides insulation and cushioning.
Reticular Tissue: Forms a supportive mesh for soft organs like the liver and spleen.
Dense Connective Tissue:
Description: Contains a higher concentration of collagen fibers for added strength and resistance to stretching.
Types:
Dense Regular Connective Tissue: Fibers align in parallel, providing strength with tensile forces; commonly found in tendons and ligaments.
Dense Irregular Connective Tissue: Fibers are arranged randomly, offering multidirectional strength; present in the dermis and joint capsules.
Specialized Connective Tissue:
Bone:
Structure: Mineralized matrix containing osteocytes; offers strong support and protection for body structures and organs.
Function: Facilitates movement, protects organs, and stores minerals.
Cartilage:
Types:
Hyaline Cartilage: Most common, provides flexible support and reduces friction at joints (e.g., at the ends of long bones).
Elastic Cartilage: Contains many elastin fibers for flexibility; found in areas such as the ear and epiglottis.
Fibrocartilage: Contains thick bundles of collagen fibers, providing tensile strength; located in intervertebral discs and joints.
Blood:
Structure: Liquid matrix called plasma, containing red blood cells, white blood cells, and platelets.
Function: Transports nutrients, gases, and waste; plays vital roles in immune responses.
5.2C: Functions of Connective Tissue
Support: Provides physical support that maintains organ structure and shape.
Binding: Connects different tissues and organs, allowing them to function together; such as tendons connecting muscles to bones.
Transport: Blood circulates oxygen, carbon dioxide, nutrients, hormones, and wastes throughout the body, making it critical for homeostasis.
Storage: Stores energy in adipose tissue and minerals like calcium in bones.
Defense: Helps fight infections through immune cells like macrophages and mast cells that act against pathogens.
5.2D: Healing and Repair of Connective Tissue
Inflammation: The initial response to tissue injury characterized by redness, heat, swelling, and pain; results from increased blood flow and immune cell infiltration to the site.
Regeneration: Involves the proliferation of fibroblasts that synthesize collagen and extracellular matrix to heal the damaged area, restoring structure and function.
Scar Formation: If the damage is extensive, scar tissue (fibrous tissue) replaces normal tissue, which may limit the functionality of the affected site, depending on the extent and nature of the original injury.
5.3 Muscle Tissue
Overview: Specialized for contraction and movement, muscle tissue is classified into three main types:
5.3 - Types of Muscle Tissue
Skeletal Muscle:
Characteristics: Voluntary control, striated appearance; composed of long fibers arranged in bundles.
Function: Moves bones and supports voluntary movements.
Cardiac Muscle:
Characteristics: Involuntary control, striated; unique intercalated discs for synchronized contractions.
Function: Pumps blood through the heart and circulatory system.
Smooth Muscle:
Characteristics: Involuntary, non-striated; found in walls of hollow organs (e.g., intestines, blood vessels).
Function: Facilitates involuntary movements such as peristalsis and blood vessel constriction.
5.4 Tissue Integration
Overview: Tissues do not act independently; they work together to form organs and systems that perform specific functions necessary for survival.
Examples of Integration:
Epithelial tissues form barriers; connective tissues provide structural support; muscle tissues enable movement; and nervous tissues facilitate communication, demonstrating the interdependence and specialization of tissue types in body systems.
5.5 Processes in Tissue Health
5.5A: Development
Overview: Tissues develop from specific germ layers during embryogenesis, leading to the formation of various organ systems.
Key Stages:
Fertilization and cleavage, blastulation, and gastrulation; shape the early development of tissues and organs.
5.5B: Change and Aging
Overview: As the body ages, changes occur at the tissue level, affecting function and structure.
Key Aspects:
Cell metabolism slows, regeneration capacity decreases, elastic tissues lose elasticity, and cellular components may undergo degeneration, leading to overall tissue deterioration and health issues.
5.6 Tissue Death
5.6A: Causes of Tissue Death
Overview: Tissue death, or necrosis, can result from lack of blood supply (ischemia), infections, toxins, or physical damage.
Implications: Leads to loss of function and potential complications, making understanding the cause critical for treatment.
5.6B: Apoptosis
Overview: Programmed cell death, a vital process for growth and maintaining homeostasis by eliminating unnecessary or damaged cells without causing inflammation.
Significance: Essential in processes such as embryonic development and tissue remodeling in adult organisms.
5.6C: Repair Mechanisms
Overview: Tissue repair mechanisms activate in response to injury, involving inflammation, regeneration, and fibrous repair.
Phases of Repair:
Inflammation: Immediate response to injury; blood vessels become permeable, allowing immune cells to enter the damaged area.
Regeneration: Replacement of lost or damaged cells with new cells of the same type where possible.
Fibrous Repair: Formation of scar tissue when regeneration is incomplete, restoring some functionality, but may lead to permanent changes in tissue structure.
 Knowt
Knowt