Respiratory Failure and VQ Mismatch
Normal Arterial Values
PaO2 → 11-15kPa
Hypoxia = Low PaO2
PaCO2 → 4.6-6.4kPa
Hypercapnia = High PaCO2
Pulmonary Circulation
Lung has two circulations
High pressure, low-flow circulation - Structural parts of the lung
Supplies arterial blood to trachea, bronchial tree, terminal bronchioles etc.
Low pressure, High-flow circulation - To the rest of the body
Venous blood from all parts of the body to alveolar capillaries for gas exchange.
Under normal conditions, right side of heart is a low pressure system pumping against low resistance.
Blood flow and distribution through the lungs
Blood flow through lungs = cardiac output
In pulmonary circulation, low PaO2 causes vasoconstriction in the adjacent vessels and reduces alveolar blood flow.
Systemic vessels dilate in response to low oxygen.
This helps distribute blood flow to the alveoli that are better ventilated.
Low O2 →DILATION → SYSTEMIC → More blood reaches O2 deprived muscle (low resistance)
Low O2 → VASOCONSTRICTION → PULMONARY → Less blood reaches O2 deprived alveoli, blood moves to alveoli with higher O2 (increased resistance).
Pulmonary Vs Systemic Circulation
Characteristic | Pulmonary | Systemic |
Pressure and Resistance | Low-pressure, low -resistance | High pressure, High resistance |
Vessel structure | Thin walled, compliant arteries | Thick-walled, muscular arteries |
Response to Hypoxia | Hypoxic Pulmonary Vasoconstriction (HPV) | Vasodilation and increase blood flow |
Capillary dynamics | Thin walls, low hydrostatic pressure, prevents pulmonary edema | Higher pressure to promote tissue perfusion |
Ventilation (V), Perfusion (Q) and Gravity
V(A) | Q | V/Q | |
Top | 1.2L/min | 0.4L/min | 3.0 |
Middle | 1.8L/min | 2.0L/min | 0.9 |
Bottom | 2.1L/min | 3.4L/min | 0.6 |
Top - Least amount of blood (due to gravity)
Bottom - Blood pools the most here due to gravity.
When lying down there will be minimal difference in the V/Q between the different areas.
Both blood flow and ventilation may vary from bottom to top of the lung.
The result is that the average arterial and alveolar partial pressures of O2 are not exactly the same.
Significant in disease.
Pulmonary ventilation and gravity
The intrapleural pressure is more negative at apex than the base.
The alveoli at the base are highly compliant (expand more) so can accommodate more air.
Hydrostatic Pressure Gradient
Hydrostatic Pressure Gradient → Pressure caused by the weight of the blood itself in the blood vessels.
Variance in upper and lower parts of the lung has implications for blood flow.
In the standing position, there is little flow in the top of the lungs.
Flow at the bottom is about 5 times as much.
The lung is divided into 3 flow zones
Zone 1: No blood flow, alveolar air pressure remains greater than the alveolar capillary pressure.
Zone 2: Intermittent blood flow, only during peaks or pulmonary arterial pressure.
Zone 3: Continuous blood flow, alveolar air pressure remains lower than the capillary pressure.
Respiratory Blood flow zones
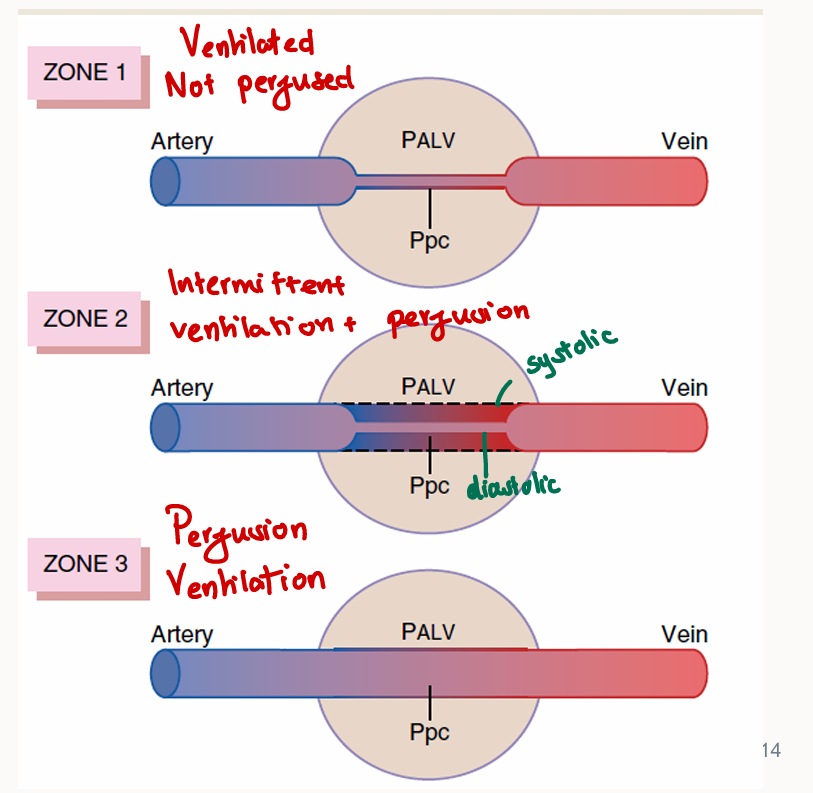
Zone 1: No flow, Alveolar air pressure (PALV) is greater than arterial pressure.
Zone 2: intermittent flow - systolic pressure (heart pump) rises higher than alveolar air pressure, but diastolic arterial pressure (heart relax) falls before alveolar air pressure.
Zone 3: continuous flow - arterial pressure and pulmonary capillary pressure (Ppc) remain greater than alveolar air pressure at all times.
Normally lungs have only zones 2 and 3 blood flow.
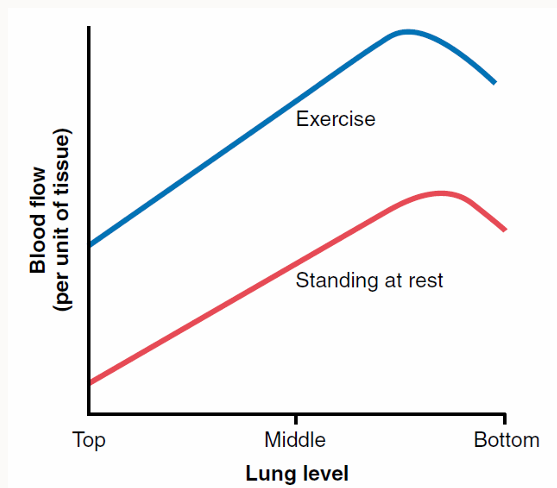
Upright person at rest - blood flow is very low at the top of the lungs, high at the bottom.
During exercise - Pulmonary vascular pressure rise to convert the lung apices from a zone 2 pattern into a zone 3 pattern of flow.
increased cardiac output = increased pulmonary pressure
Ventilation Perfusion Ration (V/Q)
V/Q → Ratio of the amount of air reaching the alveoli to the amount of blood reaching the alveoli.
Ratio of alveolar ventilation to pulmonary blood flow per minute.
Alveolar ventilation at rest = 4.2L/min
VA = Respiratory rate (RR) x (Tidal volume - physiologic dead space)
Physiological dead space = Anatomic dead space + functional dead space.
Pulmonary blood flow = 5L/min
V/Q = 4.2/5 = 0.84.
Abnormal V/Q Ratio: Pathophysiological causes
Alveolar Hypoventilation
Reduction in minute ventilation characteristically shows an increase in PaCO2.
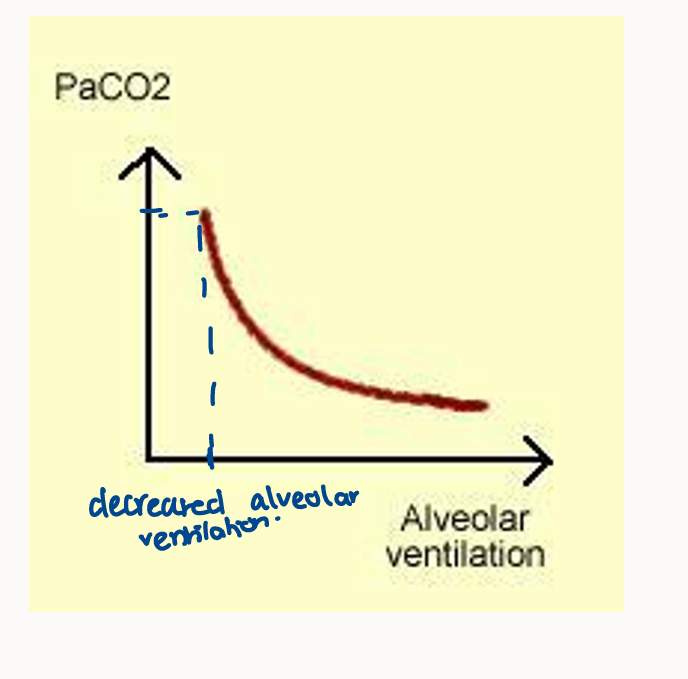
Results in CO2 retention.
Reduction in minute ventilation.
Increase in proportion of dead space → less alveoli being used.
Causes TYPE II RESPIRATORY FAILURE:
COPD
Respiratory Muscle Fatigue.
Certain medications
Correctable with oxygen (careful)
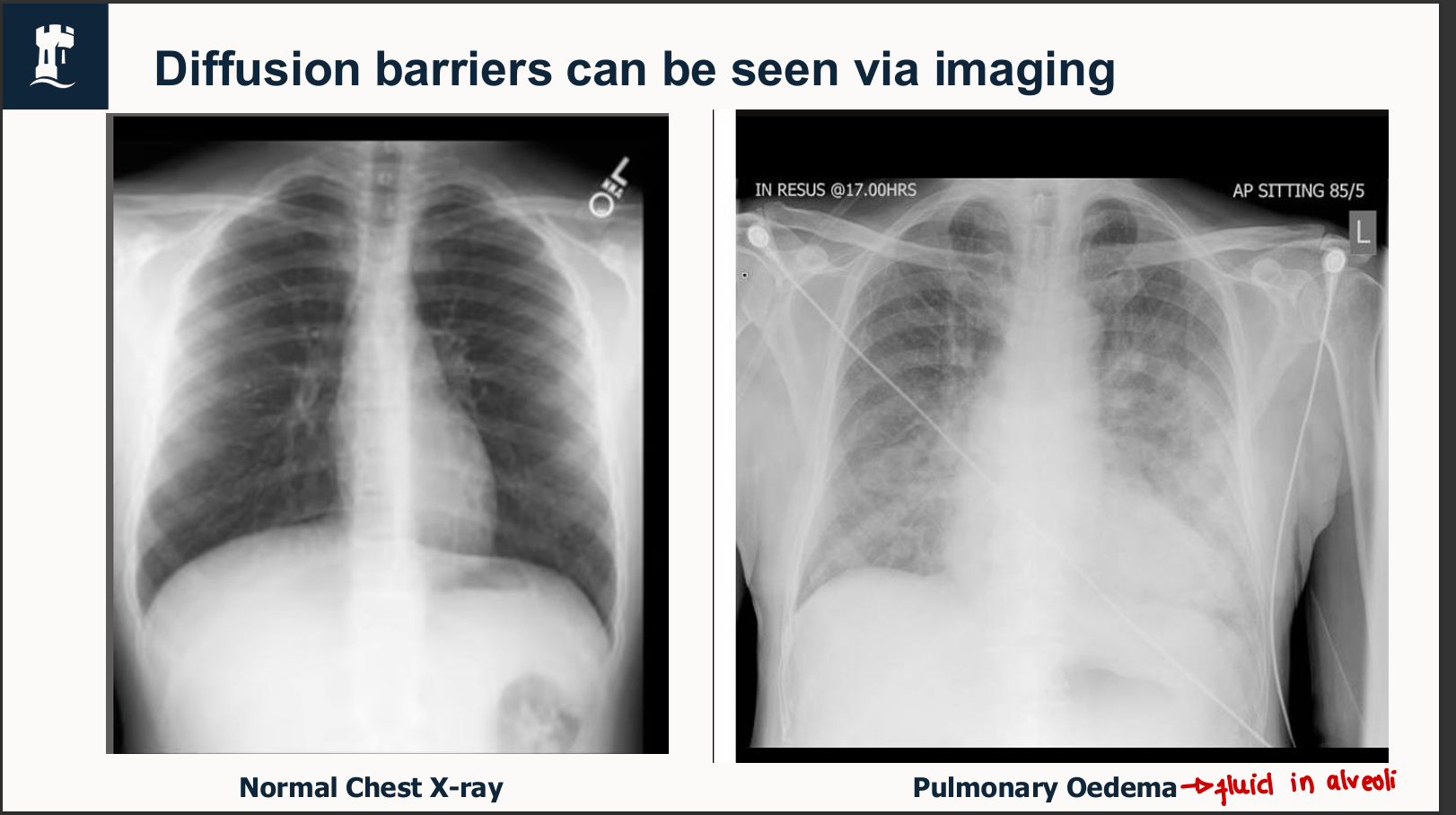
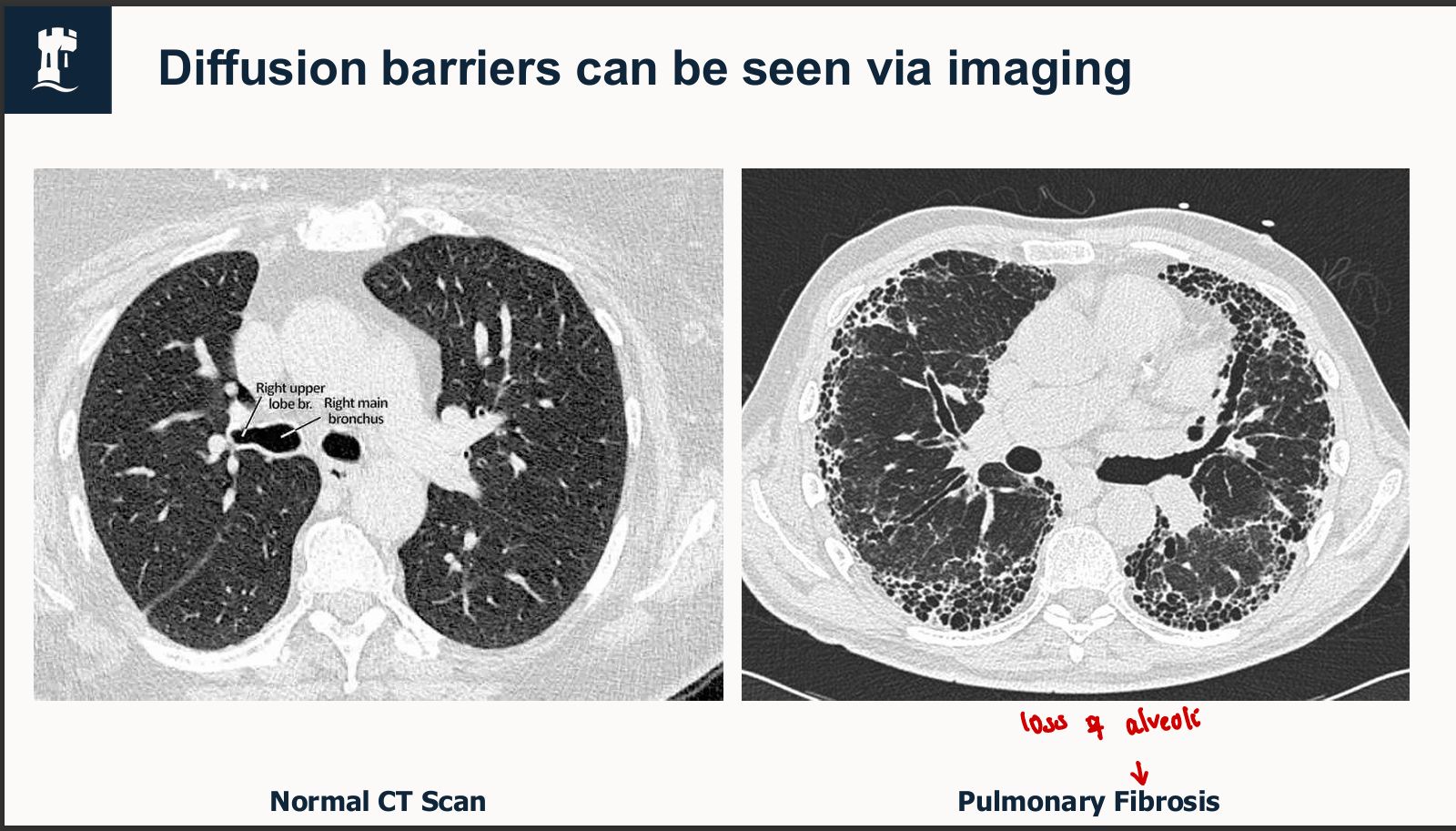
Diffusion Deficit
Fick’s law describes the rate of diffusion across the alveoli into the blood.
Rate of diffusion is proportional to both the surface are and concentration difference and is inversely proportional to the thickness of the membrane.
EFFECTS OF DIFFERENT FACTORS ON DIFFUSION
Influences | Examples | Notes |
Partial Pressure Gradient | Increased metabolism or 100% O2 Increases rate of diffusion → Steeper gradient. Altitude decreases rate of diffusion | 100% O2 increases the gradient about 5x so speeds up the delivery of O2 and so helps relieve breathing demand. |
Gas Physical Properties | Heavier gas or less soluble decreases rate of diffusion | Although heavier, CO2 is 20x more soluble than O2 and diffuses faster |
Alveolar-capillary membrane | Pathological - Pulmonary fibrosis (chronic RF), edema (acute RF), asbestosis, pneumonia. | Lung compliance reduces i.e stiff lungs (less expansion) |
Reduced Gas exchange area | Emphysema (permanent loss) Pneumonia (inflammatory consolidation) |
Shunts
Venous blood mixing with arterial blood.
Extra-pulmonary Shunt: Mainly pediatric cardiac causes e.g ductus arteriosus. This usually reverses.
Intra-pulmonary shunt
Blood is transported through the lungs without taking part in gas exchange.
Commonest causes are alveolar filling (Pus, edema, blood or tumor) and atelectasis (collapse of lung).
Oxygen does not correct pure shunt hypoxia.
Ventilation-Perfusion VQ matching
Gas exchange needs good ventilation and perfusion of alveolar capillaries.
Regulating alveolar ventilation AND perfusion maximizes gas exchange and efficiency. Ideally it should be 1:1. Regulation is needed to maximize gas exchange and maintain normal blood gas partial pressures.
Mismatch is the most common cause of hypoxia in respiratory diseases and of major significance in respiratory failure.
V/Q local Regulation
Airflow and blood flow are governed by the same principles of low, pressure and resistance (Poiseuille’s Law).
Resistance to flow is inversely proportional to the radius4
Bronchioles provide most resistance to airflow.
Arterioles provide most resistance to perfusion.
Continuous Local Changes
Altering respiratory bronchiolar and pulmonary arteriolar radius changes resistance and hence flow.
Bronchioles dilate in response to raised PaCO2 to improve airflow.
Pulmonary arterioles constrict to low PaO2 to reduce flow and redirect blood to better perfused areas.
Opposite to systemic circulation.
Mechanism uncertain.
VQ Mismatch
VQ mismatch increases the area that is not used for gas exchange (dead space).
PaO2 falls and the Pa-PaO2 gradient increases.
Breathing rate may increase.
Range of causes:
Lack of inspired oxygen.
Lack of circulation/blood flow (shunts).
Respiratory dysfunction.
Consequence of VQ mismatch
Blood leaving the relatively healthy alveoli will have an oxygen saturation of about 97% (normal) because of the flat upper portion of the oxyhemoglobin dissociation curve.
Blood leaving alveoli that do not have optimum V/Q ratios will have a much lower oxygen saturation and overall causes hypoxemia when they mix in the circulation.
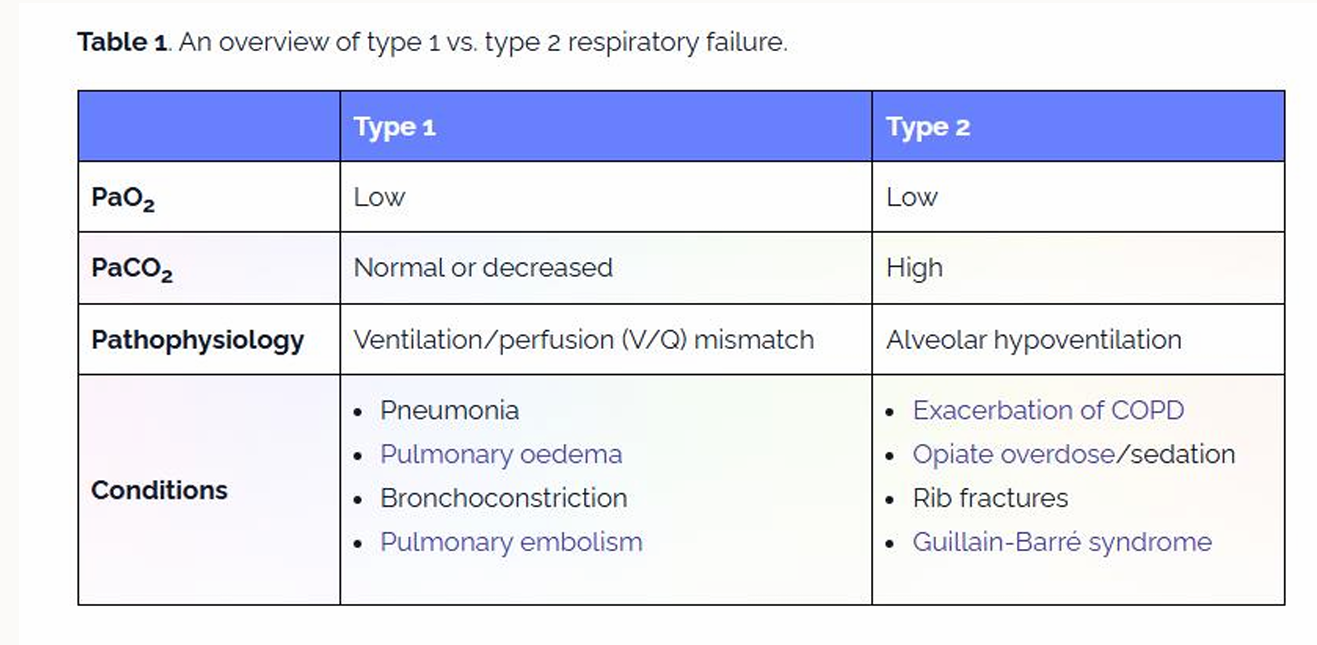
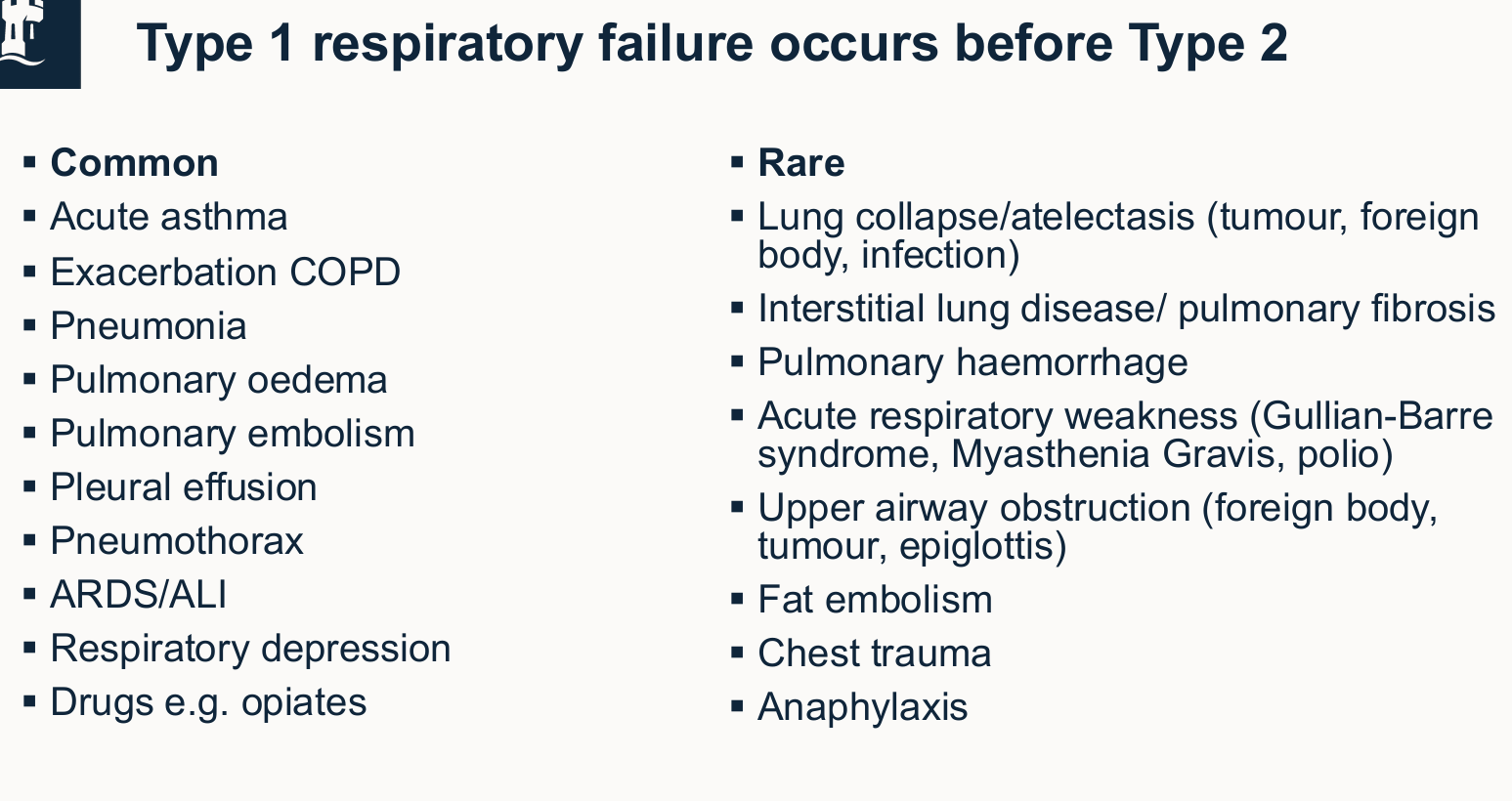
Respiratory Failure
Respiratory Failure: A failure to maintain adequate gas exchange and is characterized by abnormalities in arterial blood gas partial pressures.
Type 1: Hypoxemia (<8kPa/60mm Hg) with a normal or low Co2.
Type 2: Hypoxemia (<8kPa/60mm Hg) with a high CO2 (>6Kpa/45mm Hg).
Normally breathing rate cannot keep up.
They can co-exist.
Common respiratory dysfunctions causing VQ mismatched and reduced PaO2
Adult respiratory distress syndrome.
Pneumonia
Asthma
Pulmonary edema.
Chronic obstructive lung disease.
Interstitial fibrosis.
Pneumothorax
Pulmonary embolism.
Pulmonary hypertension.