Healing, Repair & Regeneration
The Only Time is Now
Healing, Repair & Regeneration
Course: MDP10208 Man in the Environment 2024/2025
Instructor: Prof. Dr. Dayangku Norlida A.O
Specific Instructional Objectives
At the end of the teaching session, students should be able to:
Define regeneration.
Describe the differences between various cell types in terms of their regeneration potential and provide examples.
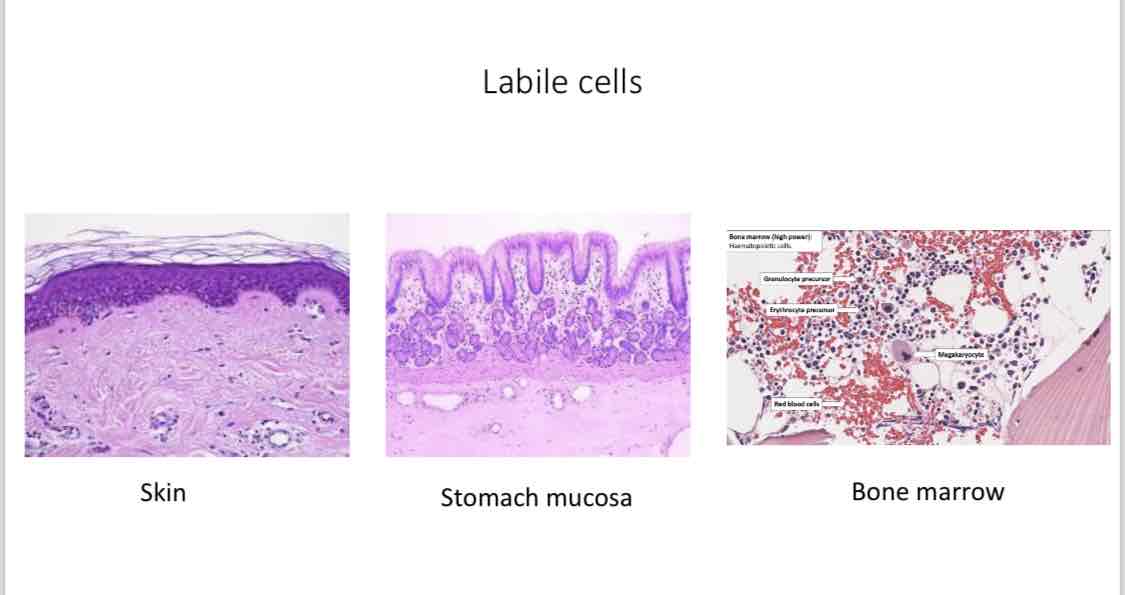
Labile cells: continuously dividing cells.
Stable cells: quiescent and can divide when prompted.
Permanent cells: terminally differentiated and nonproliferative postnatally.
List and differentiate the two types of wound healing.
Primary (first intention)
Secondary (second intention)
Describe the process involved in cutaneous wound healing.
Describe the complications in cutaneous wound healing.
Describe granulation tissue formation, scar formation, and the role of fibrosis in healing and repair.
Discuss factors that influence wound healing.
Overview of Tissue Repair
Definition: Repair (or healing) refers to the restoration of tissue architecture and function after injury.
Terminology:
"Repair" is used for parenchymal and connective tissues.
"Healing" applies to surface epithelia.
Importance: Critical for the survival of an organism, repair restores damage caused by toxic insults and inflammation.
Inflammatory Response: Eliminates dangers while initiating repair processes.
Processes of Tissue Repair
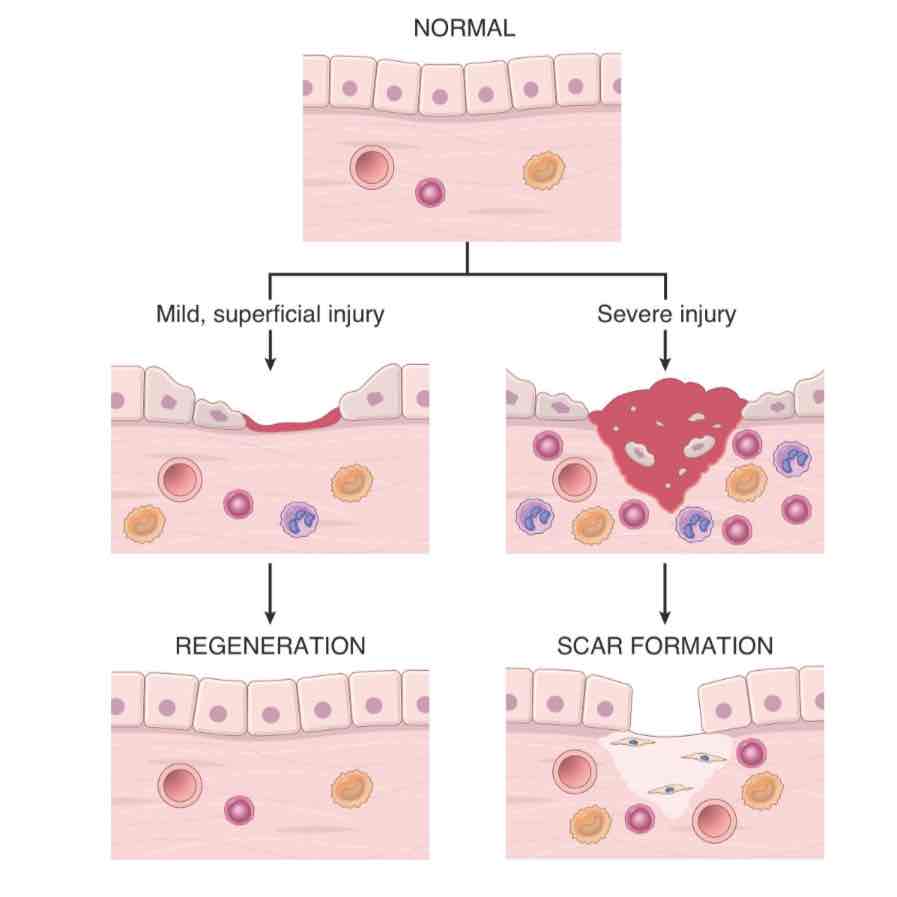
Regeneration:
Some tissues can return to a normal state by replacing damaged components.
Occurs via:
Proliferation of surviving differentiated cells (e.g., liver hepatocytes).
Collaboration of stem cells and progenitors (skin and intestine epithelia).
Mammals have a limited capacity to regenerate; not all tissues restore fully.
Scarring (Connective Tissue Deposition):
If tissues cannot regenerate, connective tissue lays down (produce/deposits its ECM component; collagen, elastin & fibronectin) causing scar formation.
Fibrous scars provide structural stability, but do not restore normal functionality.
Excessive collagen deposition is identified as fibrosis (replacement of functional tissue architecture with excess fibrous connective tissue. lead to reduced in organ f(x) & ultimately organ failure and death)seen in lungs, liver, and kidneys.
Mechanisms of Tissue Repair
Tissue repair mechanisms include cellular proliferation, growth factors, ECM integrity, and stem cell development.
Cell Proliferation: Involves various cell types including:
Remnants of injured tissue (restoration).
Vascular endothelial cells (new vessel formation).
Fibroblasts (fibrous tissue formation).
Categories Based on Proliferative Capacity:
Labile Tissues: Continuously dividing cells (hematopoietic cells, epidermal cells).
Stable Tissues: Minimal activity under normal conditions but can proliferate especially under demand (liver, kidneys).
Permanent Tissues: Terminally differentiated; injury leads to scarring (neurons, cardiac muscle).
Healing Process Overview
Healing is influenced by a balance between growth factor activity and ECM integrity.
Tissue repair types include resolution, regeneration, and scar formation based on injury severity and tissue type.
Factors Influencing Tissue Repair
Factors affecting the healing process can be extrinsic (e.g., infection) or intrinsic (systemic conditions).
Key factors:
Infection: Prolongs inflammation and contributes to local tissue damage.
Diabetes: Impairs tissue repair mechanisms.
Nutritional Status: Protein and vitamin deficiencies retard healing.
Mechanical factors: Local pressure or torsion can disrupt healing.
Perfusion: Impaired blood flow due to various conditions affects healing.
Foreign Bodies: Disrupt normal repair processes leading to prolonged inflammation.
Type of Injury: Tissue composition (labile, stable, permanent) dictates recovery ability.
Location of Injury: Impacts the repair process, especially in vital spaces.
Examples of Tissue Repair and Fibrosis
Types of Repair: Healing of skin wounds and fibrosis in parenchymal organs.
Healing of Skin Wounds:
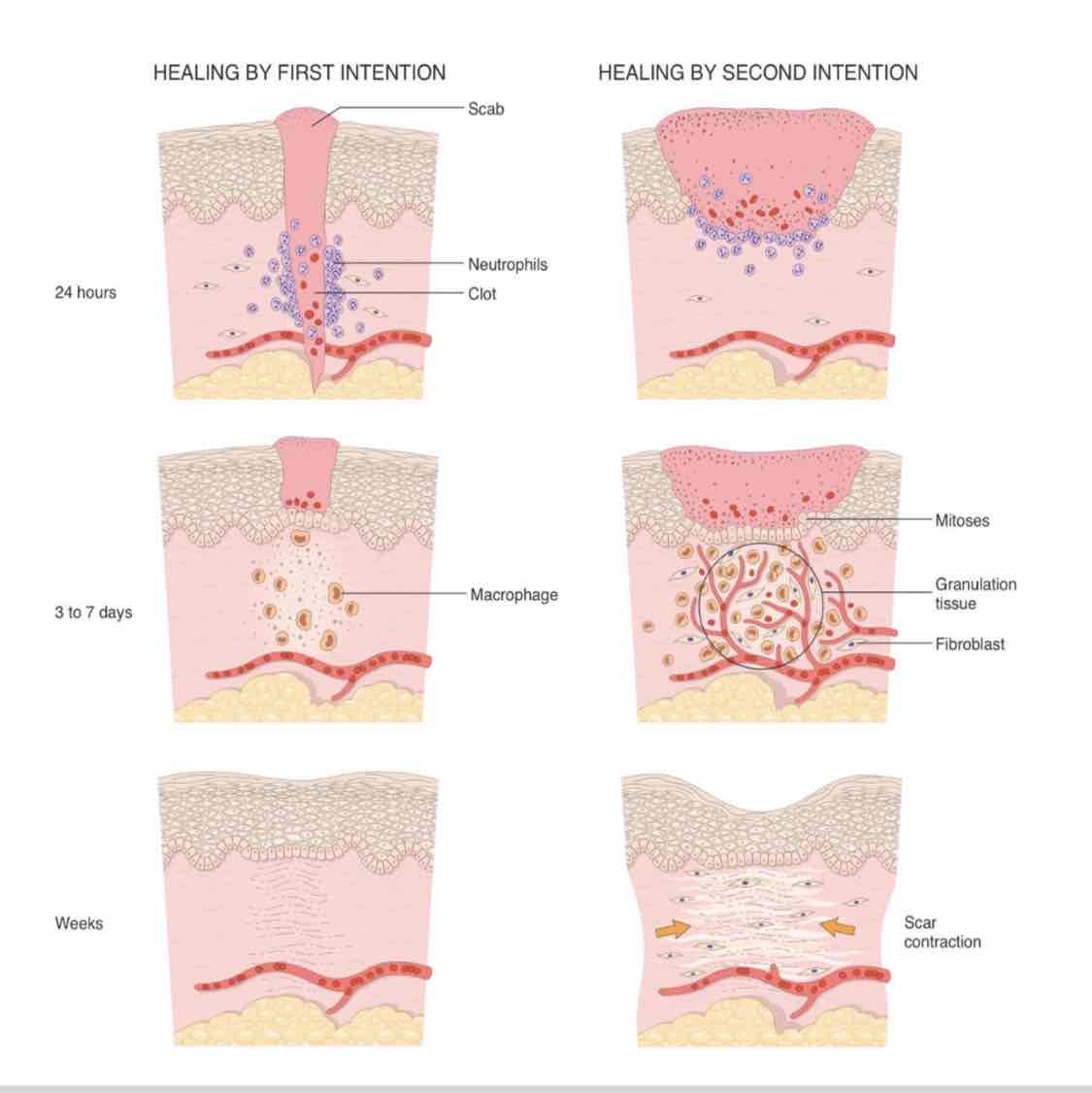
Healing types: First intention and second intention.
First Intention: Minimal tissue disruption, rapid healing with low granulation tissue.
Second Intention: Larger tissue deficits, extensive granulation tissue and inflammation.
Fibrosis: Excess collagen deposition in injured organs, can lead to dysfunction (e.g., liver cirrhosis).
Abnormalities in Tissue Repair
Defects in Healing: Common in chronic wounds like venous ulcers and diabetic ulcers.
Chronic inflammation and ischemia contribute to healing failures.
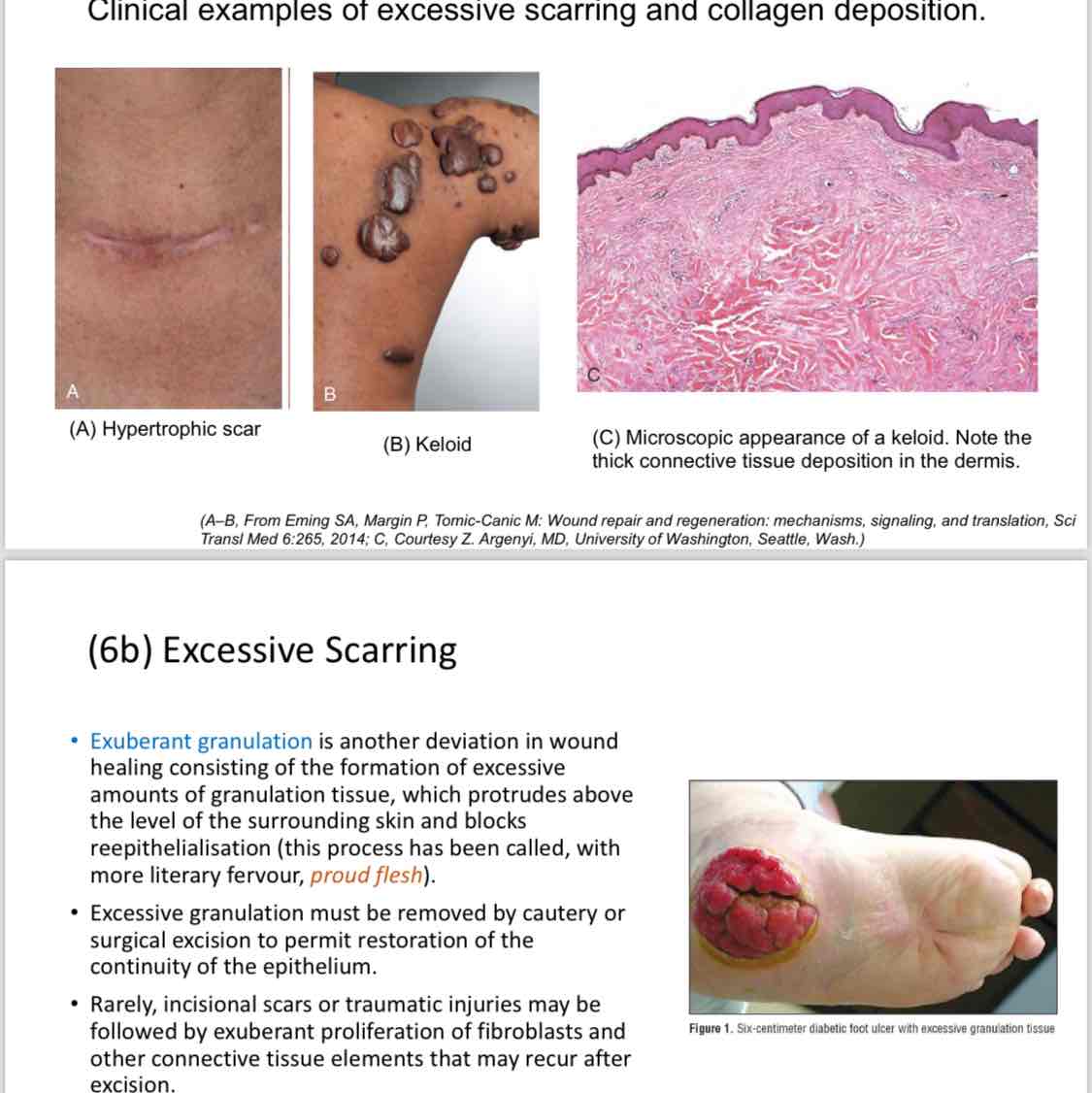
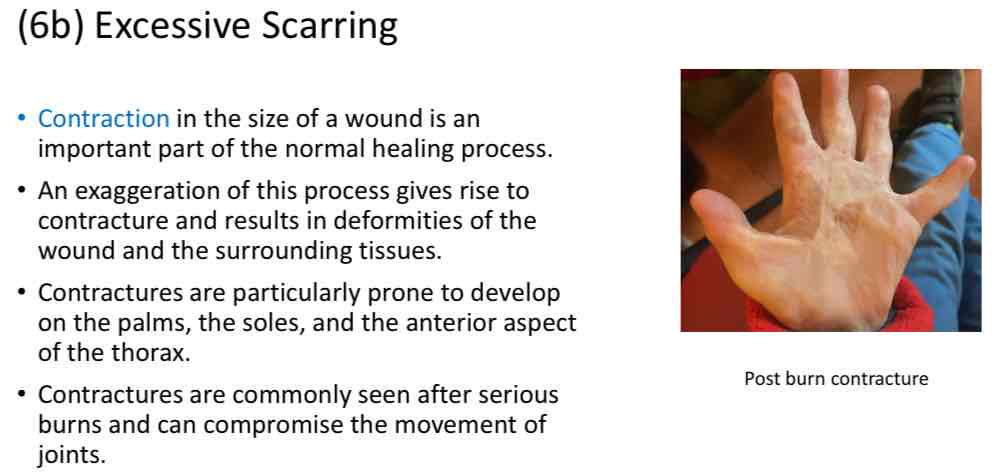
Excessive Scarring: Can lead to hypertrophic scars or keloids.
Hypertrophic Scars: Raised scars that tend to regress.
Keloids: Grow beyond wound boundaries; more common in certain demographics.
Exuberant Granulation: Excessive granulation may block epithelial restoration and may require surgical intervention.

References
Kumar, V., Abbas, A. K., Aster, J. C., Turner, J. R., & Perkins, J. A. (2021). Robbins & Cotran Pathologic Basis of Disease, 10th Ed. Elsevier.
Fibrosis and Metaplasia: Fibrosis is the process of excessive tissue scarring, where the normal tissue architecture is replaced with fibrous connective tissue, often due to chronic inflammation or injury. It does not undergo metaplasia.
Metaplasia, on the other hand, refers to the reversible transformation of one differentiated cell type to another, typically in response to chronic irritation or inflammation. While both processes are related to tissue response to injury, fibrosis results in permanent structural changes, whereas metaplasia involves changes in cell types that may revert back if the irritant is removed.
ECM Integrity and Growth Factor Activity in HealingECM (Extracellular Matrix) integrity and growth factor activity play crucial roles in the healing process.
ECM Integrity:
The ECM provides structural support and regulates various cellular functions.
It is composed of proteins such as collagen, elastin, and glycoproteins, which contribute to tissue strength and elasticity.
A well-structured ECM facilitates cellular migration, proliferation, and differentiation, which are vital for effective repair.
Disruption in ECM integrity can lead to poor healing outcomes and increased scarring.
Growth Factor Activity:
Growth factors are signaling molecules that promote cell proliferation, migration, and differentiation during tissue repair.
They are released at the site of injury and orchestrate the healing process by regulating stem cell activity, angiogenesis (formation of new blood vessels), and ECM synthesis.
Key growth factors include Vascular Endothelial Growth Factor (VEGF), Transforming Growth Factor-beta (TGF-β), and Platelet-Derived Growth Factor (PDGF).
A balanced interaction between growth factors and the ECM is essential for optimal healing; too much or too little can lead to inadequate repair or excessive scarring.