Special Care Dentistry
special care dentistry provides preventative treatment oral care services for people who are unable to accept routine dental care because of some physical, intellectual, medical, emotional, sensory, mental or social impairment or a combination of these factors. Special care Dentistry is concerned with the improvement or oral health of individuals and groups in society who fall within these categories. it requires a holistic approach that is specialist led in order to meet the complex requirements of people with impairments. It pertains to adolescents and adults, as the care of children with disabilities and additional needs sits within the domain of the specialty of paediatric dentistry.
SCD
Medical complexity
neurological conditions
Respiratory conditions
Cardiac disease
Renal/hepatic disease
Cancer
Care of the elderly
polypharmacy
Multiple comorbidities
Dementia
Learning disabilities
mild, moderate, severe
Associated with other diagnoses
Physical disability
cerebral palsy
Spina bifida
Post stroke
Arthritis
Dental anxiety
IHS/IVS
Tier 1
General dental practice
UG training
DF training
No further formal enhanced skils
Experience of treating SCD patients beneficial
Tier 2
clinical team with enhanced Skills
+/- specialist register
May involve additional equipment
May be part of continuing care or require referral
Tier 2 providers must have established link with a specialist
Tier 3
3a - care that requires management by a specialist in SCD
3b - care that requires management by a specialist in SC who is also a consultant.
Assessment
varies
Dependant on:
which tier the service is
experience/knowledge/ skills of team
services you are able to provide
standard:
NDAS
IOSN
BDA CDS Case mix
Assessment tools:
Pros:
widely used
easy to use
transferabie into different
clinical settingsassess the patientineeds
can compare the patient
within a populationQuantitative data
Cons:
subject to bias (staff and patient)
reliable?
accurate?
enough evidence?
must be used in the context of the patient
modified Dental anxiety scale
Patient reported anxiety scale
Patient completes form prior to referral for treatment
Five questions regarding dental procedures and associated anxiety
Answers score 1-5 from not anxious to extremely anxious
5-11 is minimal
12-18 is moderate
19-25 is high
Index of Sedation Need
There is a high demand for dental treatment to be carried out with the support of Iv sedation
IOSN developed to:
- support clinicians with decision making
- gives valuable information to commissioners with regard to the population so that services con be planned appropriately
- allows need for sedation to be ranked
considers 3 factors:
- Patient anxiety (MDAS)
- Medical history (conditions relevant to dental treatment)
- Treatment need (S+P/I-2 simple XLA's, MOS compIex)
Medical History
• Does not repiace full medical mistory
• Asks information relevant to proposed treatment
• scores 1-4 with 1 meaning no medical/behavioural indicators
• Then relies on clinician to score 2-4, severity of systematic disorders/conditions that compromise cooperation, gag reflex or behavioural difficulties
Treatment Complexity
Routine (1) - Scale, single quadrant requiring restorations
Intermediate (2) - multi-rooted tooth XLA, 2 quadrants requiring restorations
Complex (3) - surgical XLA with bone removal, multiple quadrants requiring restorations, endodontics
Highly complex (4) - any treatment more complex than above, or multiples
IOSN
Anxiety (1-3) - MDAS if 5-11 scores 1, 12-18 scores 2 and 19-25 scores 3
MH (1-4) - a range of medical and behavioural indicators indicators are provided including gag reflex, fainting, hypertension, angina, asthma, epilepsy, arthritis and Parkinson’s
Treatment complexity (1-4) - see above
IOSN
3-4 - minimal need (No)
5-6 - moderate need (No)
7-9 - high need (Yes)
10-11 - very high need (Yes)
BDA SCD Case Mix Model
first developed in 2008
Aid clinical team to ‘score’ Complexity of patients requiring SCD
Used in:
Commissioning/contracts
Epidemiology
Suitable for all clinical areas (GDP, Hospital, CDS)
Uses six criteria, four point scalE
BDA SDC Case Mix Model
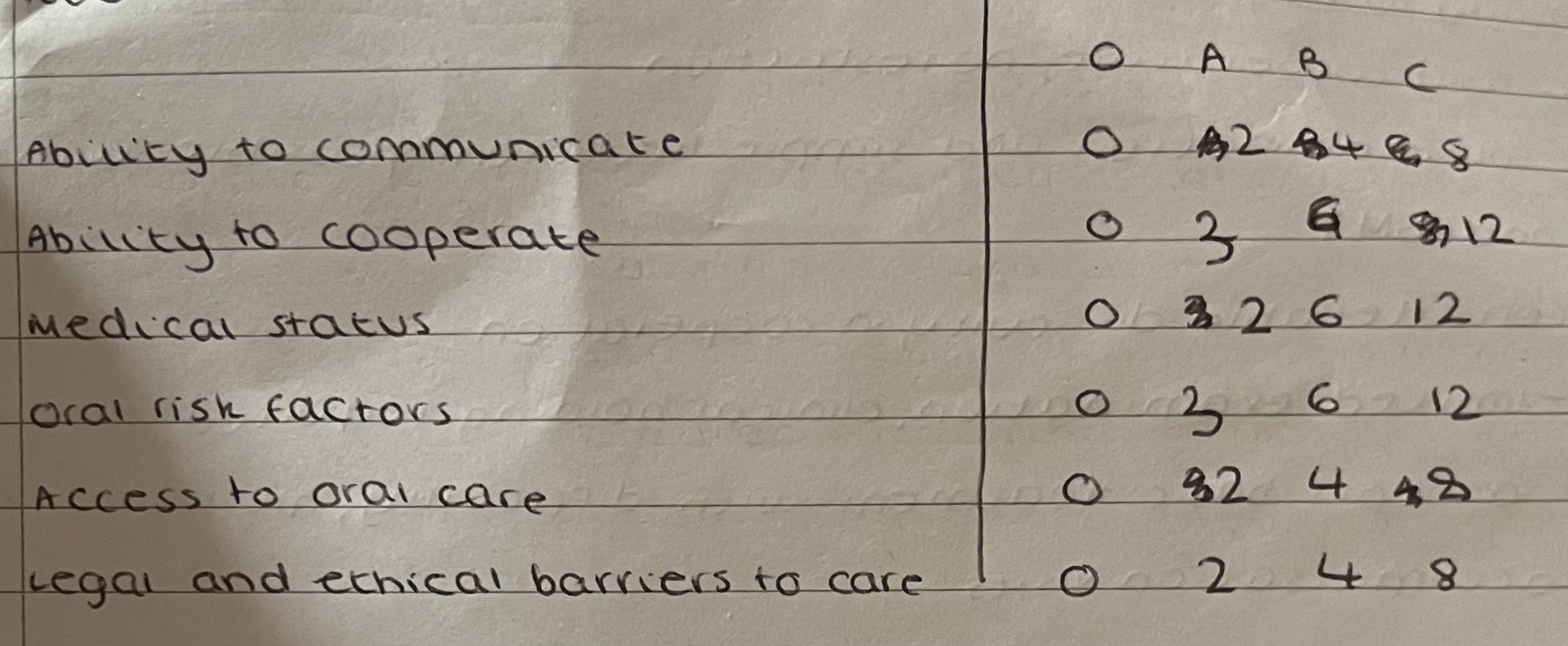
O-C Represent increasing complexity
Completed for each episode of treatment
Assesses complexity of the patient, but not the dental treatment required
Has been validated as a useful method of assessment
Ability to communicate
O - Free communication, no restriction
A - Mild restriction
Mild learning disability, difficulty overcome easily, young child with limited verbal communication
B - Moderate restriction
Non-verbal, limited communication, moderate learning disability
C- Severe
Unable to communicate, profound learning disability, third-party discussions
Ability to cooperate
O - Fully cooperative, no restriction
A - Full examination and simple treatment possible with support and BMT
B - Considerable difficulty in cooperation
Limited examination, clinical holding required, patient accepts basic treatment with difficulty, multiple acclimatisation visits
C - Serious difficult difficulty in cooperation
Unable to examine/treat Without sedation
Medical status
O - Adequate medical history obtained, no impact on the plan treatment, no further investigations required
A - Some treatment modification required
MH Unable to be obtained on first appointment and further info required
B - Moderate impact of medical/psychiatric Condition on provision of care
Medical/psychiatric Status complex/unstable, Treatment affected and child in need
C - Severe impact of medical/psychiatric Condition on provision of care
Complex medical history, requires multidisciplinary review to decide whether to treat and precautions required
Oral risk factors
O - Minimal risk, low caries/periodontal risk
A - Moderate risk
Can comply with most DBOH, good OH Reduced due to malocclusion/dexterity issues
B - Severe risk
Extensive support for DBOH, third-party responsibility, reduced slavery flow and access to oral cavity severely restricted
C - Extreme risk
Unable to comply with DBOH, unable to comply with toothbrushing, regular sugar containing medication, severe xerostomia and PEG fed
Access to Oral Care
O - unrestricted, can access surgery without intervention
A - Moderate restriction
Multiple FTA/UTA Within a course of treatment, require support to access dental surgery
B - Severe restriction
Specialised equipment required to get their appointment
C - Domiciliary care
Patient unable to leave place of residence
Legal and ethical Barriers
O - No legal or ethical responsibilities affecting care e.g. No issues with consent or PR
A - Some difficulties
Best interests decision not requiring additional correspondence, children in need
B - Moderate difficulties
Fluctuating capacity, best interest decision needing additional correspondence, looked after children
C - Severe difficulties
Multi professional consultation in order to overcome legal/ethical Issues, IMCA/Safeguarding referral required
Case mix score
0 - No patient complexity
1-9 - Mild
10-19 - Moderate
20-29 - Severe
30+ - Extreme
Summary
SCD provides dental care for a wide spectrum of patients with broad and diverse needs
Assessment of SCD patient is a vital importance and ensure patients have their treatment:
At the right time
In the right place
By the appropriately trained team
All members of the dental team will provide care for patients with SCD requirements - it’s important that you know what to do and when to refer
 Knowt
Knowt