WK2B: Male and Female Reproductive System
The major function of the reproductive system is to ensure survival of the species. An individual may live a long, healthy, and happy life without producing offspring, but if the species is to continue, at least some individuals must produce offspring.
Within the context of producing offspring, the reproductive system has four functions:
To produce egg and sperm cells
To transport and sustain these cells
To nurture the developing offspring
To produce hormones
REPRODUCTIVE DEVELOPMENT
Intrauterine Development - The sex of an individual is determined at the moment of conception by the chromosome information supplied by the particular ovum and sperm that joined to create the new life.
A gonad is a body organ that produces the sex cells necessary for reproduction (the ovary in females, the testis in males). At approximately week 5 of intrauterine life, primitive gonadal tissue is already formed.
In both sexes, two undifferentiated ducts, the mesonephric (wolffian) and paramesonephric (müllerian) ducts, are present.
By week 7 or 8, in chromosomal males, this early gonadal tissue differentiates into primitive testes and begins formation of testosterone. Under the influence of testosterone, the mesonephric duct begins to develop into the male reproductive organs, and the paramesonephric duct regresses. If testosterone is not present by week 10, the gonadal tissue differentiates into ovaries, and the paramesonephric duct develops into female reproductive organs
Mesonephric in males = Paramesonephric in females
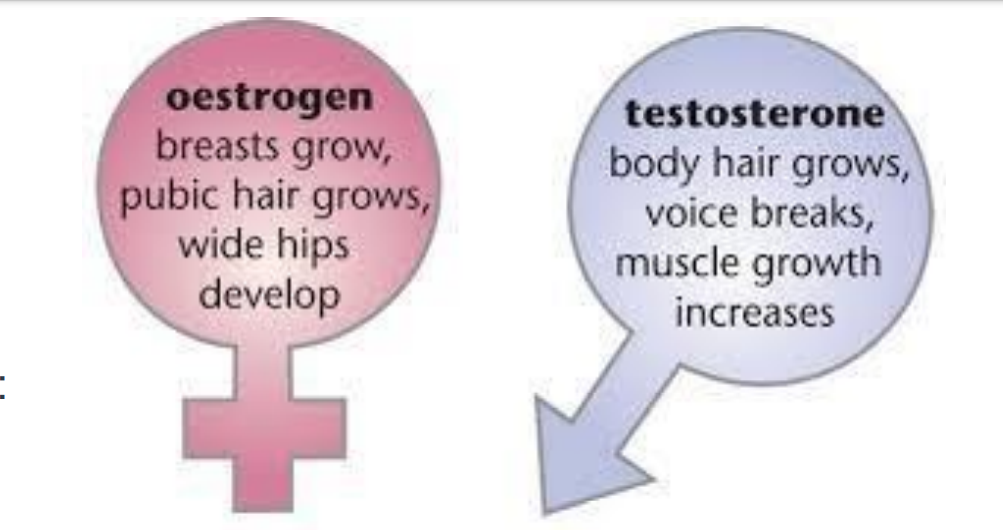
Pubertal Development - Puberty is the stage of life at which secondary sex changes begin. These changes are stimulated when the hypothalamus synthesizes and releases gonadotropin-releasing hormone (GnRH), which in turn triggers the anterior pituitary to begin the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH initiate the production of androgen and estrogen, which in turn initiate secondary sex characteristics, the visible signs of maturity.
Puberty is initiated by hypothalamicpituitary – gonad complex.
Puberty usually starts in Girls at 10-13 years old and Boys starts at 12-14 years old.
Role of Androgen - Androgenic hormones are the hormones responsible for muscular development, physical growth, and the increase in sebaceous gland secretions that cause typical acne in both boys and girls. In males, androgenic hormones are produced by the adrenal cortex and the testes; in females, by the adrenal cortex and the ovaries.
Role of Estrogen – When triggered at puberty by FSH, ovarian follicles in females begin to excrete a high level of the hormone estrogen.This hormone is actually not one substance but three compounds (estrone [E1], estradiol [E2], and estriol [E3]).
Secondary Sex Characteristics
Adolescent sexual development is categorized into stages (Tanner, 1990). There is wide variation in the time required for adolescents to move through these developmental stages; however, the sequential order is fairly constant. In girls, pubertal changes typically are manifest as:
Growth spurt
Increase in the transverse diameter of the pelvis
Breast development
Growth of pubic hair
Onset of menstruation
Growth of axillary hair
Vaginal secretions
Secondary sex characteristics of boys usually occur in the order of:
Increase in weight
Growth of testes
Growth of face, axillary, and pubic hair
Voice changes
Penile growth
Increase in height
Spermatogenesis (production of sperm)
Female and Male Reproductive System Homologues
Female = Male
Clitoral glans = Penile glans
Clitoral shaft = Penile Shaft
Labia major = Scrotum
Ovaries = Testtes
Skene’s glands = Prostate
Bartholin’s glands = Cowper’s glands
I. Male Reproductive System
Functions of the Male Reproductive System:
Production of gametes
Male sex cells, i.e., sperm, Synthesis of androgens
Male sex hormones, e.g. testosterone
Delivery of sperm into the female reproductive tract
A. Male External Structures
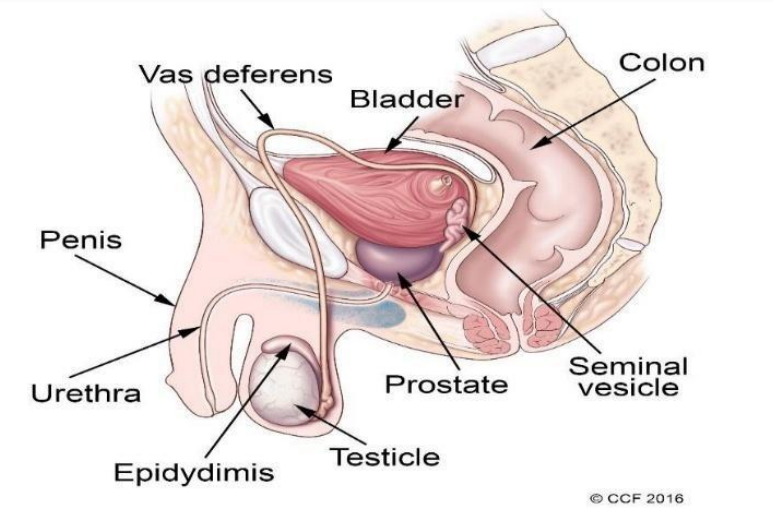
Scrotum - is a rugated, skin-covered, muscular pouch suspended from the perineum. Its functions are to support the testes and to help regulate the temperature of sperm through contraction and relaxation and moving closer to and further away from the perineum. Loose pouch-like sac of skin that hangs behind the penis. Contains the testes/male gonads, epididymis, and the lower portion of the spermatic cord
the looseness of the scrotum is intentional to provide expansion and contraction
lowers Temperature by 3*C
In very cold weather, the scrotal muscle contracts to bring the testes closer to the body; for warmth
in very hot weather, or in the presence of fever, the muscle relaxes, allowing the testes to fall away from the body. High temperature can cause delicate sperm cell to die.
Warm Temperature = Scrotum becomes very loose and allow the testes to hand further away from the near of the body.
Testes - are two ovoid glands, 2 to 3 cm wide, that lie in the scrotum (walnut size). Each testis is encased by a protective white fibrous capsule and is composed of several lobules, with each lobule containing interstitial cells (Leydig’s cells) and a seminiferous tubule.
The main reproductive organs of the male body are the testes, which produce sperm and also male hormones, in the form of testosterone.
Seminiferous tubules produce spermatozoa.
Leydig’s cells are responsible for the production of testosterone.
Testes in a fetus first form in the pelvic cavity. They descend, late in intrauterine life (about the 34th to 38th week), into the scrotal sac. Because this descent occurs so late in pregnancy, many male preterm infants are born with undescended testes.
In most males, one testis is slightly larger than the other and is suspended slightly lower in the scrotum than the other (usually the left one). Because of this, testes tend to slide past each other more readily on sitting or muscular activity, and there is less possibility of trauma to them.
Spermatozoa do not survive at a temperature as high as that of the body, however, so the location of the testes outside the body, where the temperature is approximately 1° F lower than body temperature, provides protection for sperm survival (McCance & Huether, 2007).
Surrounded by 2 tunics:
Tunica vaginalis: Derived from the parietal peritoneum.
Tunica albuginea
Feel smooth and are freely movable within the scrotum.
Penis = The penis is composed of three cylindrical masses of erectile tissue in the penis shaft: two termed the corpus cavernosa, and a third termed the corpus spongiosum. The urethra passes through these layers of erectile tissue, making the penis serve as the outlet for both the urinary and the reproductive tracts in men. At the distal end of the organ is a bulging, sensitive ridge of tissue, the glans. A retractable casing of skin, the prepuce, protects the nerve-sensitive glans at birth.
Tubular structure located above the scrotum, composed of shaft and glans.
Half of it is an internal root and half is the external visible shaft.
Soft and flaccid (2.5 to 4 inches).
Erection - blood vessels in the shaft become congested, penis become hard and erect (5.5 to 7 inches)
Glans = The distal end of the organ is bulging sensitive ridge of tissue which has the external urinary meatus at its tip.
Corona = The proximal margin of the glans.
Prepuce = Also called the foreskin. Loose skin attached to the shaft, allowing for expansion during erection. Retractable casing of skin that protects the nerve sensitive glans at birth
Frenulum = Ventral fold of tissue attaches the skin to the glans. Contains the urethra as well as 3 erectile bodies:
2 dorsal erectile tissues known as the corpora cavernosa
1 midventral tissue known as the corpus spongiosum
Surrounds penile urethra
Expands distally to form the glans penis
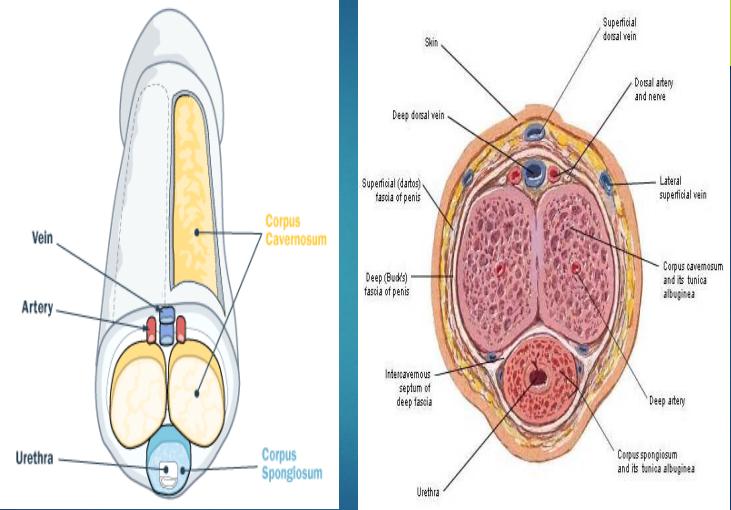
Sexual excitement → Nitric acid is released from the endothelium of blood vessels → Result in engorgement or an increase in the blood flow to the arteries of the penis → The Ischiocavernosus muscle at the penis base then contracts → Trapping both venous and arterial blood in the 3 sections of erectile tissue → Leading to distention and erection of the penis
B. Male Internal Sructures
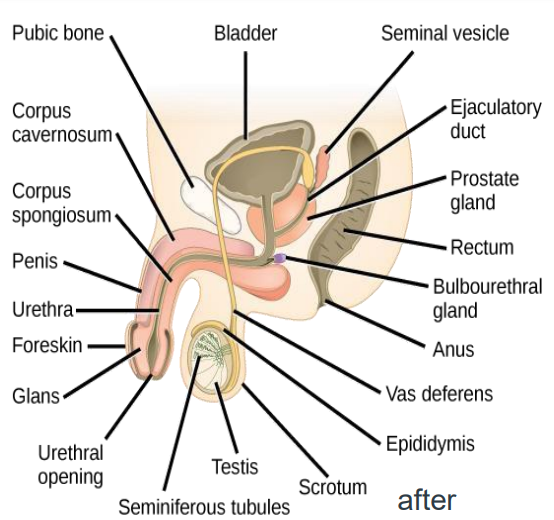
Epididymis - the seminiferous tubule of each testis leads to a tightly coiled tube, the epididymis, which is responsible for conducting sperm from the tubule to the vas deferens, the next step in the passage to the outside.
Because each epididymis is so tightly coiled, its length is extremely deceptive: it is actually over 20 ft long.
Some sperm are stored in the epididymis, and a portion of the alkaline fluid that will surround sperm at maturity (semen, or seminal fluid that contains a basic sugar and mucin, a form of protein) is produced by the cells lining the epididymis.
Sperm are immobile and incapable of fertilization as they pass or are stored at the epididymis level.
It takes at least 12 to 20 days for them to travel the length of the epididymis and a total of 64 days for them to reach maturity.
This is one reason that aspermia (absence of sperm) and oligospermia (20 million sperm/mL) are problems that do not appear to respond immediately to therapy but rather only 2 months.
Site of sperm maturation and storage
Contains smooth muscle to propel sperm during ejaculation
Vas Deferens (Ductus Deferens) - is an additional hollow tube surrounded by arteries and veins and protected by a thick fibrous coating. It carries sperm from the epididymis through the inguinal canal into the abdominal cavity, where it ends at the seminal vesicles and the ejaculatory ducts. Sperm mature as they pass through the vas deferens.
Vasectomy (severing of the vas deferens to prevent passage of sperm) is a popular means of male birth control (Cook et al., 2009).
It is about 40cm long
The vas deferens serves a transport function and the area of the ampulla serves as astorage reservoir of sperm for release at ejaculation.
Seminal Vesicles - are two convoluted pouches that lie along the lower portion of the posterior surface of the bladder and empty into the urethra by way of the ejaculatory ducts.
These glands secrete a viscous alkaline liquid that has a high sugar, protein, and prostaglandin content. Sperm become increasingly motile with this added fluid, because it surrounds them with nutrients and a more favorable pH.
Ejaculatory Ducts - The two ejaculatory ducts pass through the prostate gland and join the seminal vesicles to the urethra.
These are formed by the fusion of the vas deferens and the seminal vesicles. The ejaculatory ducts empty into the urethra
The ejaculatory ducts are part of the human male anatomy, which cause the reflex action of ejaculation. Each male has two of them.
They begin at the vas deferens, pass through the prostate, and empty into the urethra at the Colliculus seminalis. During ejaculation, semen passes through the ducts and exits the body via the penis.
Prostate Gland - is a chestnut-sized gland that lies just below the bladder. The urethra passes through the center of it, like the hole in a doughnut.
The prostate gland secretes a thin, alkaline fluid. When added to the secretion from the seminal vesicles and the accompanying sperm from the epididymis, this alkaline fluid further protects sperm from being immobilized by the naturally low pH level of the urethra.
Bulbourethral Glands - two bulbourethral or Cowper’s glands lie beside the prostate gland and empty via short ducts into the urethra. Like the prostate gland and seminal vesicles, they secrete an alkaline fluid that helps counteract the acid secretion of the urethra and ensure the safe passage of spermatozoa.
Produce small droplets of fluid during sexual activity that neutralizes the acidity of the male urethra and aid in the transport of sperm
5% semen
Urethra - is a hollow tube leading from the base of the bladder, which, after passing through the prostate gland, continues to the outside through the shaft and glans of the penis. It is approximately 8 in (18 to 20 cm) long.
3 sections
Prostatic
Within the prostate
Membranous
Within the urogenital diaphragm
Penile (spongy)
Within the penis
The seminal vesicles, prostate gland and Cowper’s gland produce a liquid called a seminal plasma.
Seminal Plasma = Aids in the transport of sperm
Provides energizing nutrients for the sperm
Contains form of sugar – fructose, mucous, salts, water, base buffers and coagulators to aid the sperm in their journey.
The sperm collectively make up the semen.
Semen / seminal fluid
Thick, creamy white fluid with the consistency of mucus or egg whites
Normal amount is 2 mL – 6 mL per ejeculation
Fertile man will dispel 20-160 million sperm per ejaculate.
Spermatozoon – is made up of a head and a tail - the head carries the male’s haploid number of chromosomes (23)
the part that enters the ovum at fertilization
the tail specialize in motility
sperm maybe stored in the male genital system for 42 days
sperm can live only 2-3 days in the female genital tract once ejaculated.
II. Female Reproductive System
Functions of the Female Reproductive System:
It produces the female egg cells necessary for reproduction, called the ova or oocytes.
It is designed to transport the ova to the site of fertilization.
If fertilization does not take place, the system is designed to menstruate.
It produces female sex hormone that maintain the reproductive cycle.
A. Internal Structures
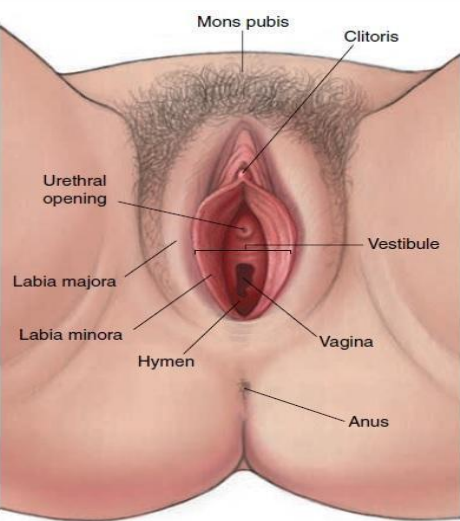
Mons Veneris/Pubis - is a pad of adipose tissue located over the symphysis pubis, the pubic bone joint. It is covered by a triangle of coarse, curly hairs. The purpose of the mons veneris is to protect the junction of the pubic bone from trauma. It contains many nerve ending that makes the mons pubis sensitive to touch and pressure.
Labia Minora - just posterior to the mons pubis veneris spread two hairless folds of connective tissue, the labia minora. Before menarche, these folds are fairly small; by childbearing age, they are firm and full; after menopause, they atrophy and again become much smaller.
It has 2 smaller lips located within the labia majora.
It appears thin pale pink in color. When stimulated, it turns to dark red or dark pink due to presence of blood vessels, no hair; smooth in texture.
The internal structure is covered with mucous membrane, and the external portion with skin
Labia Majora = The labia majora are two folds of adipose tissue covered by loose connective tissue and epithelium that are positioned lateral to the labia minora. Covered by pubic hair, the labia majora serve as protection for the external genitalia and the distal urethra and vagina. Analogous to the scrotum.
The outer lips separates downward from the mons and meet again below the vagina introitus.
It contains multitude of sebaceous and sweat glands.
It also serves as protection for the external genitalia and the distal urethra and vagina.
Vestibule - is the flattened, smooth surface inside the labia. The openings to the bladder (the urethra) and the uterus (the vagina) both arise from the vestibule
Clitoris - is a small (approximately 1 to 2 cm), rounded organ of erectile tissue at the forward junction of the labia minora. It is covered by a fold of skin, the prepuce.The clitoris is sensitive to touch and temperature and is the center of sexual arousal and orgasm in a woman.
It contains erectile tissue blood vessels and nerves.
It is made up of erectile tissue which many large and small venous channels surrounded by large amount of involuntary muscle tissue, the ischiocarvernosa facilitate erection of the organ.
The clitoris measures 5 – 6 mm. long and 6 – 8 mm. across.
It has very rich blood and nerve supplies.
Functions: Stimulate and elevate levels of sexual tension. Serve as a landmark in locating urethral opening during catheterization.
Skene’s glands (paraurethral glands) = are located just lateral to the urinary meatus, one on each side. Their ducts open into the urethra.
a pair of small glands lying on each side of the urethra
they produce a small amount of mucus and are especially susceptible to gonorrheal infection
it is homologous to male prostate
Secretions from both of these glands help to lubricate the external genitalia during coitus.
The alkaline pH of their secretions helps to improve sperm survival in the vagina.
Bartholin’s glands (vulvovaginal glands) = are located just lateral to the vaginal opening on both sides. Their ducts open into the distal vagina.
pair of small, pea – sized glands located within the substances of the labia majora
they correspond to the bulbourethral or Cowper’s gland in male
the gland secretes a small amount of clear, viscid mucus during sexual excitement
Fourchette = is the ridge of tissue formed by the posterior joining of the two labia minora and the labia majora. This is the structure that is sometimes cut (episiotomy) during childbirth to enlarge the vaginal opening.
Hymen = is a tough but elastic semicircle of tissue that covers the opening to the vagina in childhood. It is often torn during the time of first sexual intercourse. However, because of the use of tampons and active sports participation, many girls who have not had sexual relations do not have intact hymens at the time of their first pelvic examination.
It is comprised mainly of connective tissue both elastic and collagen. Both surfaces are covered by stratified squamous epithelium.
The hymen can be broken through strenous physical activities or masturbation.
Urethral meatus / urethral orifice = although not a true part, it is considered as part of the reproductive system because of its closeness and relationship to the vulva
Vaginal orifice / introitus = occupies the lower portion of the vestibule and varies considerably in size and shape. The vagina has an abundantly vascular supply
Perineum = located just posterior to the fourchette. This is a muscular area, that’s easily stretched during childbirth to allow enlargement of the vagina and passage of the fetal head.
Many exercises (Kegel’s,squatting & tailorsitting) are aimed at making the perineal muscle more flexible to allow easier expansion during birth without tearing of this tissue.
B. Female Internal Structures
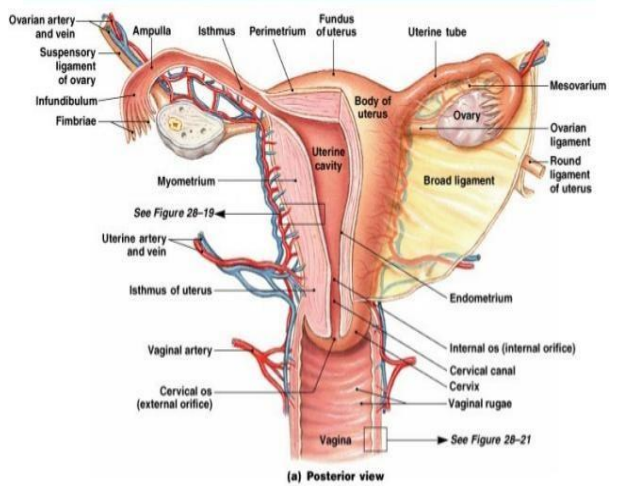
Ovaries = The ovaries are approximately 4 cm long by 2 cm in diameter and approximately 1.5 cm thick, or the size and shape of almonds. They are grayish white and appear pitted, or with minute indentations on the surface.
The function of the two ovaries (the female gonads) is to produce, mature, and discharge ova (the egg cells). In the process, the ovaries produce estrogen and progesterone and initiate and regulate menstrual cycles. Functions : ovulation and hormone production These also a counterpart to the testes of male organ. Maturation and maintenance of secondary sex characteristics in females.
At birth, each ovary contains approximately 2 million immature ova (oocytes), which were formed during the first 5 months of intrauterine life.
By age 7 years, only approximately 500,000 are present in each ovary; by 22 years, there are approximately 300,000; and by menopause, none are left (all have either matured or atrophied).
Each ovary contains approximately 200,000 to 400,000 follicles during female’s childbirth.
It secretes hormones ESTROGEN and PROGESTERONE which initiate and regulate menstrual process.
Ovaries have three principal divisions:
Tunica albuginea - dense and dull white and serves as protective layer of surface epithelium
Cortex, where the immature (primordial) oocytes mature into ova and large amounts of estrogen and progesterone are produced, main functional part because it contains ova, graafian follicles, corpora lutea, degenerated corpora lutea (corpora albicantia).
Central medulla, which contains the nerves, blood vessels, lymphatic tissue, and some smooth muscle tissue, or central portion of the ovary is composed of loose connective tissue.
Fallopian Tubes = The fallopian tubes arise from each upper corner of the uterine body and extend outward and backward until each opens at its distal end, next to an ovary. Fallopian tubes are approximately 10 cm long in a mature woman. Their function is to convey the ovum from the ovaries to the uterus and to provide a place for fertilization of the ovum by sperm.
The most proximal division, the interstitial portion, is that part of the tube that lies within the uterine wall. This portion is only about 1 cm in length; the lumen of the tube is only 1 mm in diameter at this point. The isthmus is the next distal portion. It is approximately 2 cm in length and like the interstitial tube, is extremely narrow. This is the portion of the tube that is cut or sealed in a tubal ligation, or tubal sterilization procedure. The ampulla is the third and also the longest portion of the tube. It is approximately 5 cm in length. It is in this portion that fertilization of an ovum usually occurs. The infundibular portion is the most distal segment of the tube. It is approximately 2 cm long and is funnel shaped. The rim of the funnel is covered by fimbria (small hairs) that help to guide the ovum into the fallopian tube
Slender structure that extends from either side of the uterus and end in a fringed fashion near each ovary. It transports mature ovum from the ovary to the uterus and to provide place for fertilization of the ovum.
It takes about 3 days for an egg to travel the length, but unfertilized egg lives only 24 hours. If unfertilized it will die before it arrives in the uterus.
Functions : site of fertilization, provide transport for the ovum from the ovary to the uterus, serve as a warm, moist, nourishing environment for the ovum or zygote
The wall of the fallopian tube is made up of 4 layers:
Peritoneal (serous) – covers the tubes.
Subserous (adventitial) – contains the blood and nerve supply
Muscular - responsible for the peristaltic movement of the tube.
Mucosal – composed of ciliated and unciliated cells with the number of ciliated cells more abundant at the fimbria.
Uterus. The uterus is a hollow, muscular, pear-shaped organ located in the lower pelvis, posterior to the bladder and anterior to the rectum. During childhood, it is approximately the size of an olive. An adolescent is closer to 17 years old before the uterus reaches its adult size. With maturity, a uterus is approximately 5 to 7 cm long, 5 cm wide, and, in its widest upper part, 2.5 cm deep. In a nonpregnant state, it weighs approximately 60 g.
Its primary purpose is to house and nurture a pregnancy.
The function of the uterus is to receive the ovum from the fallopian tube; provide a place for implantation and nourishment; furnish protection to a growing fetus; and, at maturity of the fetus, expel it from a woman’s body.
Anatomically, the uterus consists of three divisions:
The body of the uterus is the uppermost part and forms the bulk of the organ. During pregnancy, the body of the uterus is the portion of the structure that expands to contain the growing fetus. The portion of the uterus between the points of attachment of the fallopian tubes is termed the fundus.
The isthmus of the uterus is a short segment between the body and the cervix. In the nonpregnant uterus, it is only 1 to 2 mm in length. It is the portion of the uterus that is most commonly cut when a fetus is born by a cesarean birth.
The cervix is the lowest portion of the uterus. It represents approximately one third of the total uterus size and is approximately 2 to 5 cm long. The opening of the canal at the junction of the cervix and isthmus is the internal cervical os; the distal opening to the vagina is the external cervical os. The level of the external os is at the level of the ischial spines (an important relationship in estimating the level of the fetus in the birth canal).
cervical canal – central cavity
internal cervical os – junction of the canal at the isthmus
external cervical os – distal opening to the vagina
Layers of uterus
Perimetrium – a part of visceral peritoneum
Myometrium – bulk of uterus – three layers of muscle that contract under influence of oxytocin during labor.
Endometrium – highly vascular mucosa
Stratum functionalis – shed during menstruation
Stratum basalis – deeper, permanent layer, gives rise to new stratum functionalis
Vagina = Passageway for sperm and menstrual flow Receptacle for penis during intercourse. Inferior portion of birth canal. Capable of considerable distention (stretching). Mucosa is continuous with that of uterus and consists of nonkeratinized stratified squamous epithelium
Contains large stores of glycogen which decomposes to organic acids – lower pH = less susceptible to infection & less hospitable to sperm
The cervical mucosa has 3 functions: provide lubrication for the vaginal canal, act as a bacteriostatic agent, provide an alkaline environment to shelter deposited sperm from the acidic vagina.
Secretory cells of the cervix produce about 20 – 60 ml of mucus / day.
At time of ovulation, this mucus becomes thinner and more alkaline.
provide an alkaline environment to shelter deposited sperm from the acidic vagina.
Secretory cells of the cervix produce about 20 – 60 ml of mucus / day.
At time of ovulation, this mucus becomes thinner and more alkaline.
Mucus provides for the energy needs of the sperm, protects sperm from environment of the vagina,
Mucus provides for the energy needs of the sperm, protects sperm from environment of the vagina, and protects them from phagocytes.
At other times, mucus becomes thick and can form a cervical plug which impedes passage of pathogens.
C. Breasts
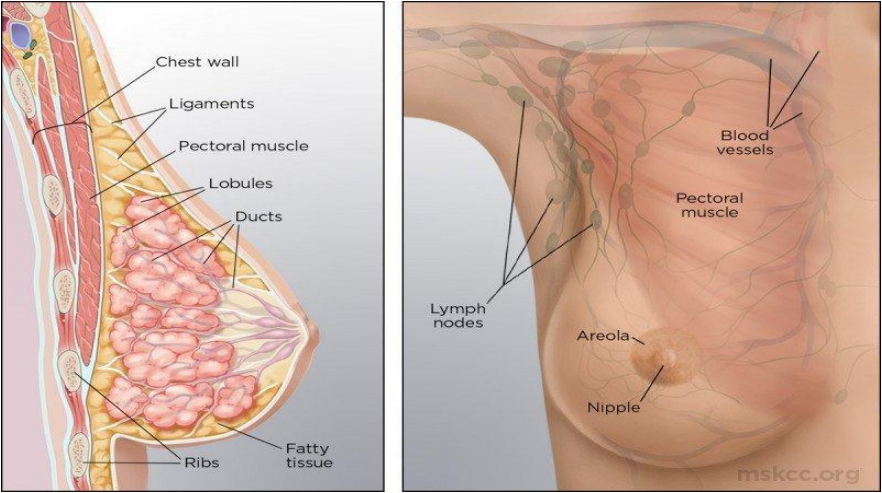
the mammary glands, or breasts, form from ectodermic tissue early in utero. They then remain in a halted stage of development until a rise in estrogen at puberty produces a marked increase in their size. The size increase occurs mainly because of an increase of connective tissue plus deposition of fat. The glandular tissue of the breasts, necessary for successful breastfeeding, remains undeveloped until a first pregnancy begins
Milk glands of the breasts are divided by connective tissue partitions into approximately 20 lobes. All of the glands in each lobe produce milk by acinar cells and deliver it to the nipple via a lactiferous duct. The nipple has approximately 20 small openings through which milk is secreted. An ampulla portion of the duct, located just posterior to the nipple, serves as a reservoir for milk before breastfeeding.
A nipple is composed of smooth muscle that is capable of erection on manual or sucking stimulation. On stimulation, it transmits sensations to the posterior pituitary gland to release oxytocin. Oxytocin acts to constrict milk gland cells and push milk forward into the ducts that lead to the nipple. The skin surrounding the nipples is darkly pigmented out to approximately 4 cm and is termed the areola. The area appears rough on the surface because it contains many sebaceous glands, called Montgomery’s tubercles. It contains the opening of sebaceous and sweat glands (Montgomery glands) that secrete lubricating substances for the nipple
Accessory organs of the female reproductive system Modified sweat glands Function is to synthesize, secrete and eject milk (lactation) Lie over the pectoralis major muscles Are attached to fascia by the suspensory ligaments (of Cooper) Breast size is determined more by fat than by glandular tissue.
Breasts or Mammary Glands Breasts are located anterior to the pectoral muscle. In many women, breast tissue extends well into the axilla. Each breast has 15-20 lobes made up of several lobules. Lobules are made of milksecreting cells arranged in alveoli.
All the glands in each lobe produce milk by acini cells & deliver it to the nipple by lactiferous duct Milk production is stimulated mostly by prolactin with some help from estrogen & progesterone.
Gynecomastia = Increase in male breast size Most evident in obese boys Normal change of puberty