BIO 202 Respiratory Final Exam Review Guide
Absolutely, Sarah! Here's a comprehensive and structured review guide tailored to your BIO 202 Respiratory Final. I’ve organized it into digestible sections with bullet points and key terms to help you master each concept.
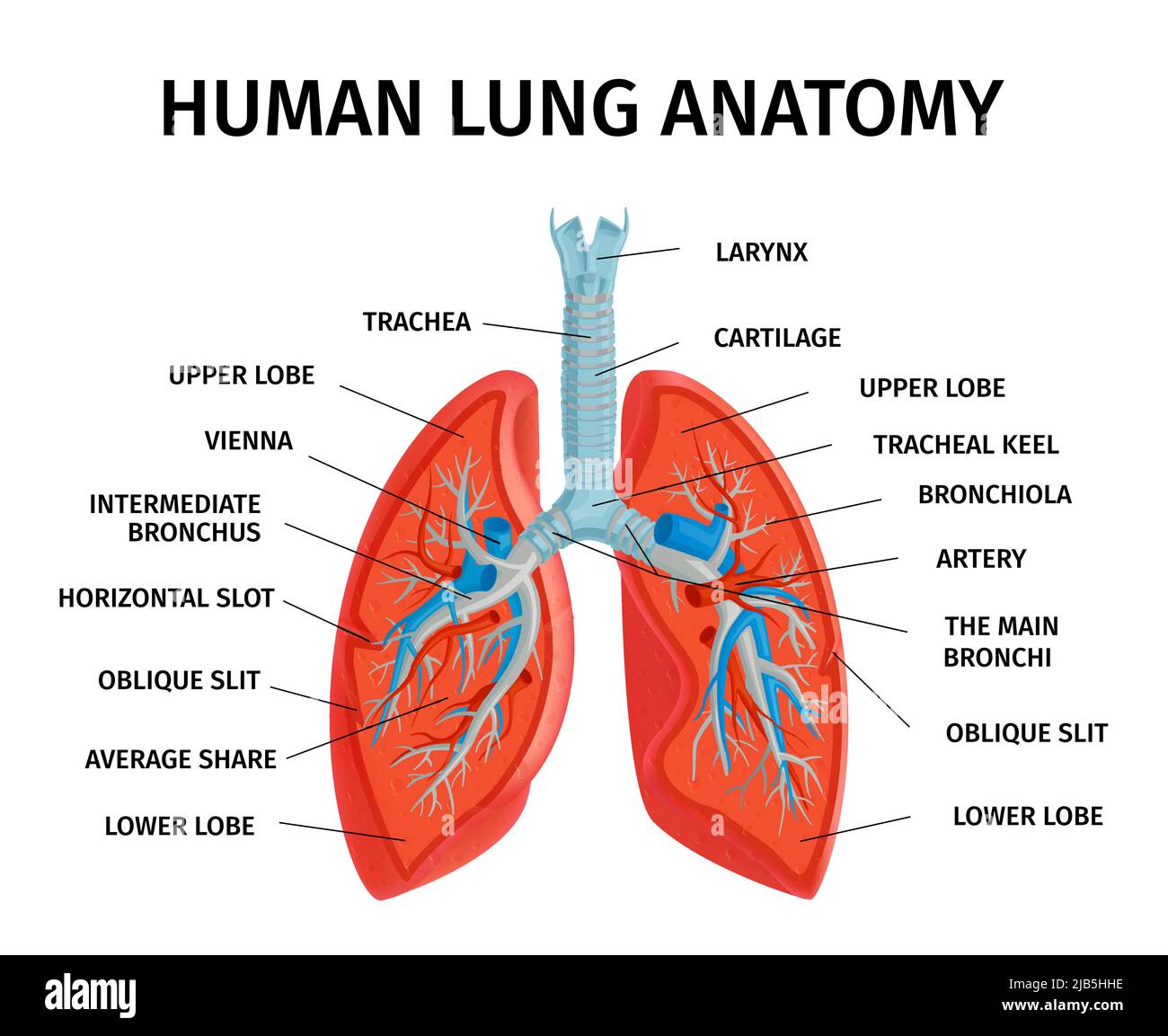
🫁 1. Structures & Functions of the Respiratory System
Upper Respiratory Tract
Nose & Nasal Cavity: Filters, warms, humidifies air
Pharynx: Passageway for air and food
Larynx: Voice production; protects lower tract during swallowing
Lower Respiratory Tract
Trachea: Windpipe; conducts air to bronchi
Bronchi & Bronchioles: Branching airways; regulate airflow
Alveoli: Site of gas exchange
Lungs: House alveoli; facilitate ventilation
🫧 2. Alveolar Structure & Gas Exchange
Alveoli: Thin-walled sacs surrounded by capillaries
Type I cells: Gas exchange
Type II cells: Secrete surfactant to reduce surface tension
Gas exchange: Driven by partial pressure gradients (O₂ in, CO₂ out)
🌬 3. Respiratory Tract Structures & Pressures
Airflow: Moves from high to low pressure
Intrapulmonary pressure: Pressure inside alveoli
Intrapleural pressure: Always negative to keep lungs inflated
Transpulmonary pressure: Difference between the two; drives lung expansion
🧠 4. Pons & Medulla Oblongata Functions
Medulla:
Dorsal respiratory group (DRG): Controls inspiration
Ventral respiratory group (VRG): Controls forced expiration
Pons:
Apneustic center: Stimulates inspiration
Pneumotaxic center: Inhibits inspiration for rhythm control
⚗ 5. Gas Laws in Breathing & Exchange
Law | Application |
|---|---|
Boyle’s Law | ↑ Volume = ↓ Pressure (inhalation) |
Dalton’s Law | Total pressure = sum of partial pressures |
Henry’s Law | Gas dissolves in liquid based on partial pressure & solubility |
Fick’s Law | Rate of diffusion ∝ surface area & pressure gradient |
📊 6. Lung Volumes & Capacities
Term | Definition |
|---|---|
TV (Tidal Volume) | Air in/out during normal breath |
IRV | Extra air inhaled after normal inspiration |
ERV | Extra air exhaled after normal expiration |
RV | Air remaining after full exhalation |
VC | TV + IRV + ERV |
TLC | VC + RV |
🌀 7. Resistance & Airflow
Airflow ∝ Pressure / Resistance
Resistance ↑ with:
Bronchoconstriction
Mucus/inflammation
Airflow ↓ with:
Narrow airways
High resistance
🔄 8. Internal vs External Respiration
External: Gas exchange between alveoli & blood
Influenced by partial pressures, membrane thickness, surface area
Internal: Gas exchange between blood & tissues
Driven by cellular metabolism and pressure gradients
🩸 9. CO₂ Transport in Blood
Dissolved in plasma (~7%)
Bound to hemoglobin as carbaminohemoglobin (~23%)
As bicarbonate (HCO₃⁻) via carbonic anhydrase (~70%)
🌎 10. Atmospheric Gases
Gas | % Composition |
|---|---|
Nitrogen (N₂) | ~78% |
Oxygen (O₂) | ~21% |
CO₂, H₂O, others | ~1% |
📈 11. Oxygen Dissociation Curve, Carbonic Anhydrase, Carbaminohemoglobin
O₂ Dissociation Curve: Sigmoidal; shows hemoglobin’s affinity for O₂
Shift right: ↓ affinity (↑ CO₂, ↑ temp, ↓ pH)
Shift left: ↑ affinity
Carbonic Anhydrase: Enzyme converting CO₂ + H₂O ↔ H₂CO₃ ↔ H⁺ + HCO₃⁻
Carbaminohemoglobin: CO₂ bound to hemoglobin (not at O₂ binding site)
🧪 12. Bohr & Haldane Effects
Bohr Effect: ↑ CO₂ or ↓ pH → ↓ hemoglobin affinity for O₂
Haldane Effect: Deoxygenated hemoglobin binds CO₂ more readily
😮💨 13. Hyperventilation vs Hypoventilation
Condition | Effect |
|---|---|
Hyperventilation | ↓ CO₂ → respiratory alkalosis |
Hypoventilation | ↑ CO₂ → respiratory acidosis |
🧬 14. Neuronal Control of Breathing
Central chemoreceptors: Detect CO₂ & pH in CSF
Peripheral chemoreceptors: Detect O₂, CO₂, pH in blood (carotid/aortic bodies)
Stretch receptors: Prevent overinflation (Hering-Breuer reflex)
💪 15. Muscles of Ventilation & Thoracic Pressure
Primary Muscles
Diaphragm: Contracts → ↑ thoracic volume
External intercostals: Elevate ribs
Accessory Muscles
Inspiration: Sternocleidomastoid, scalenes
Expiration (forced): Internal intercostals, abdominal muscles

Absolutely, Sarah! Here’s your BIO 202 Respiratory System Lecture Notes, written in simple language, organized like classroom-style slides, and ready to be turned into flashcards or study sheets. I’ll keep the explanations clear, conversational, and include emoji cues to make it easier to visualize.
🫁 Lecture 1: Overview of the Respiratory System
🔹 Main Jobs:
Bring oxygen into your body 💨
Remove carbon dioxide 🫶
🔹 Two Main Zones:
Upper Tract: Nose, nasal cavity, pharynx, larynx – filters, warms, and moistens air
Lower Tract: Trachea, bronchi, lungs, alveoli – passes and exchanges gases
🫧 Lecture 2: Alveoli & Gas Exchange
🔹 Alveoli = tiny air sacs (like grapes)
Very thin walls
Surrounded by capillaries 🩸
🔹 Gas Exchange:
O₂ moves from alveoli → blood
CO₂ moves from blood → alveoli
Think of them as “swap stations” where oxygen and carbon dioxide trade places.
🌬 Lecture 3: Breathing Pressures
🔹 Air moves from high to low pressure
When chest expands → pressure drops → air rushes in
When chest shrinks → pressure rises → air goes out
🔹 Key Pressures:
Intrapulmonary (inside lungs)
Intrapleural (between lungs and chest wall) – always negative to keep lungs open
🧠 Lecture 4: Brain Control (Pons & Medulla)
🔹 Medulla:
Controls normal breathing rhythm
Turns breathing on and off like a switch
🔹 Pons:
Smooths breathing
Coordinates inhale & exhale timing
⚗ Lecture 5: Gas Laws Made Easy
Boyle’s Law: Bigger space = lower pressure
Dalton’s Law: Air is made of lots of gases
Henry’s Law: Gases dissolve based on pressure
Fick’s Law: More surface area = better gas exchange
📊 Lecture 6: Lung Volumes
Volume | What It Means |
|---|---|
TV | Regular breath in/out |
IRV | Deep breath in |
ERV | Forceful breath out |
RV | Air leftover in lungs |
VC | Full amount you can breathe |
TLC | Total lung capacity |
🌀 Lecture 7: Resistance & Airflow
🔹 Narrow tubes = harder to breathe
Conditions like asthma or mucus increase resistance
Air wants to flow freely, but blockages slow it down
🔄 Lecture 8: Internal vs External Respiration
External: Alveoli ↔ Blood (lungs)
Internal: Blood ↔ Cells (body tissues)
🩸 Lecture 9: CO₂ Transport
Dissolved in plasma: Small amount
Bicarbonate: Most common (70%)
Carbaminohemoglobin: Attached to hemoglobin
🌎 Lecture 10: Air Composition
Nitrogen: 78%
Oxygen: 21%
Others (CO₂, water vapor, etc.): 1%
📈 Lecture 11: Oxygen & CO₂ Exchange Helpers
Dissociation Curve: Shows how oxygen loads & unloads
Carbonic Anhydrase: Converts CO₂ into transportable form
Carbaminohemoglobin: CO₂ stuck to hemoglobin
🧪 Lecture 12: Haldene vs Bohr Effects
Effect | What It Does |
|---|---|
Bohr | CO₂/pH affects oxygen unloading |
Haldene | Less oxygen makes CO₂ bind easier |
😮💨 Lecture 13: Breathing Imbalances
Hyperventilation = breathing too fast → low CO₂
Hypoventilation = breathing too slow → high CO₂
🧬 Lecture 14: Nerve Control
Central sensors: Detect CO₂/pH in brain
Peripheral sensors: Detect gases in blood
Stretch receptors: Prevent lungs from overfilling
💪 Lecture 15: Breathing Muscles
Muscle Group | Function |
|---|---|
Primary (diaphragm, intercostals) | Normal breathing |
Accessory (sternocleidomastoid, abdominals) | Help during heavy breathing |
They change chest space to control pressure, letting air in or out.