WK5A: Care of the Mother during the Perinatal Period
PRENATAL CARE
OBSTETRIC DATA
Gravida - Number of pregnancy regardless of duration as long as the mother becomes pregnant even abnormal.
Para/Parity - number of viable pregnancy or the total number of pregnancies in which the fetus has reached the age of viability and subsequently delivered whether dead or alive at birth.
Viability - Ability of the fetus to live outside the uterus at the earliest possible gestational age.
Primigravida - Woman who is pregnant for the first time
Primipara - Woman who has given birth to one child past age of viability; woman who has completed one pregnancy to age of viability and subsequently delivered the fetus, whether alive or dead at birth.
Multigravida - Woman who has been pregnant previously; 2 or more pregnancy
Grand multigravida - woman who has had six or more pregnancies
Multipara - Woman who has carried two or more pregnancies to viability; woman who has carried two or more pregnancies of stage of viability and subsequently born alive or dead.
Nulligravida - Woman who has never been and is not currently pregnant
Nullipara - woman who has not carried a pregnancy beyond 20 weeks
Grand multipara - woman who has had 6 or more viable deliveries, whether, the fetuses were alive or dead.
PRINCIPLES IN IDENTIFYING PARITY
Number of pregnancies is counted and not the number of fetuses.
Abortion is not included in parity count
Live birth or stillbirth is counted in parity count.
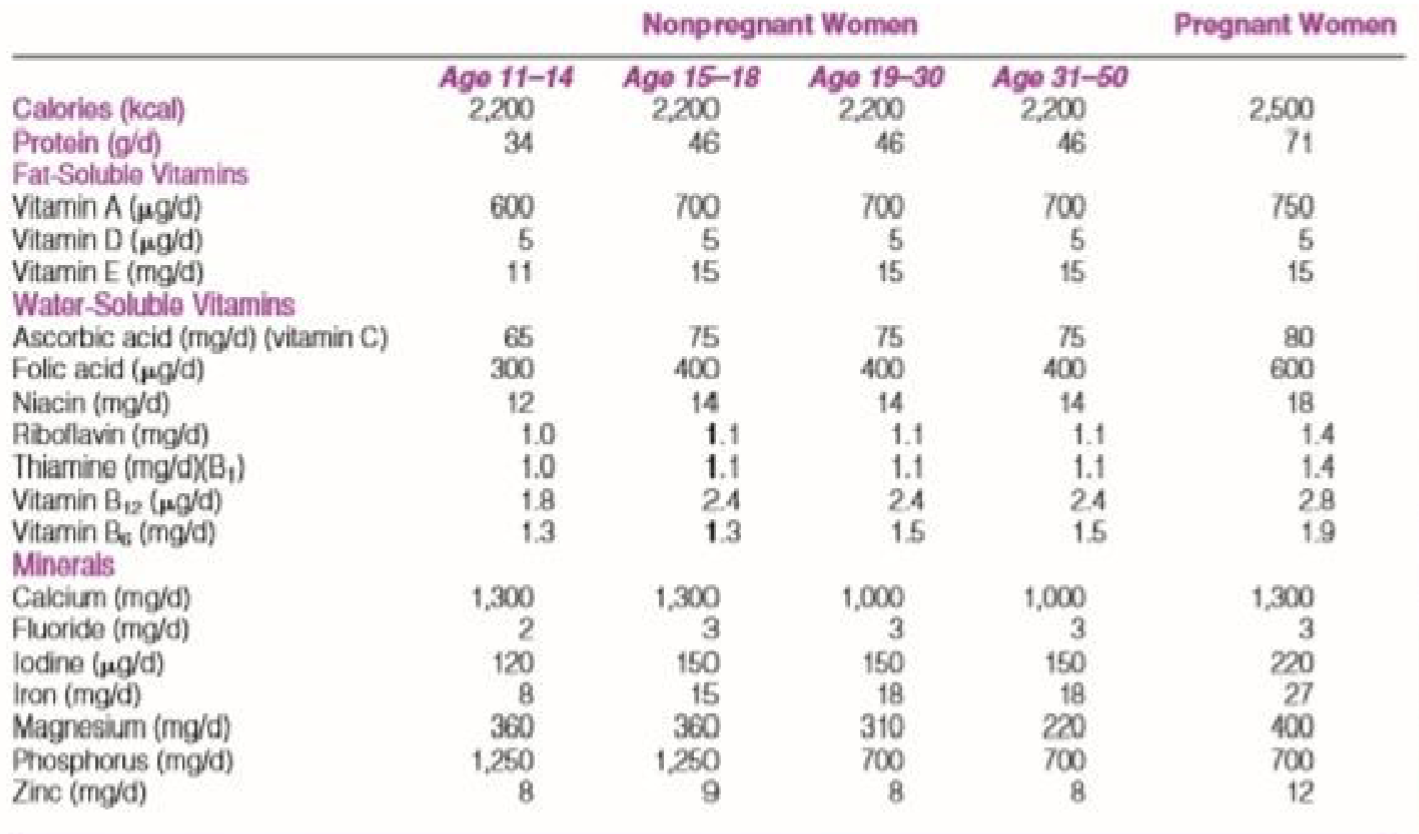
OB SCORING
T - Term: Number of full-term infants born 37 weeks
P - Pre-term: Number of preterm infants born 20 – 36 weeks
A - Abortion: termination of pregnancy before the age of viability (less than 20 weeks)
L – Number of Currently Living Children
M – Multiple Pregnancy
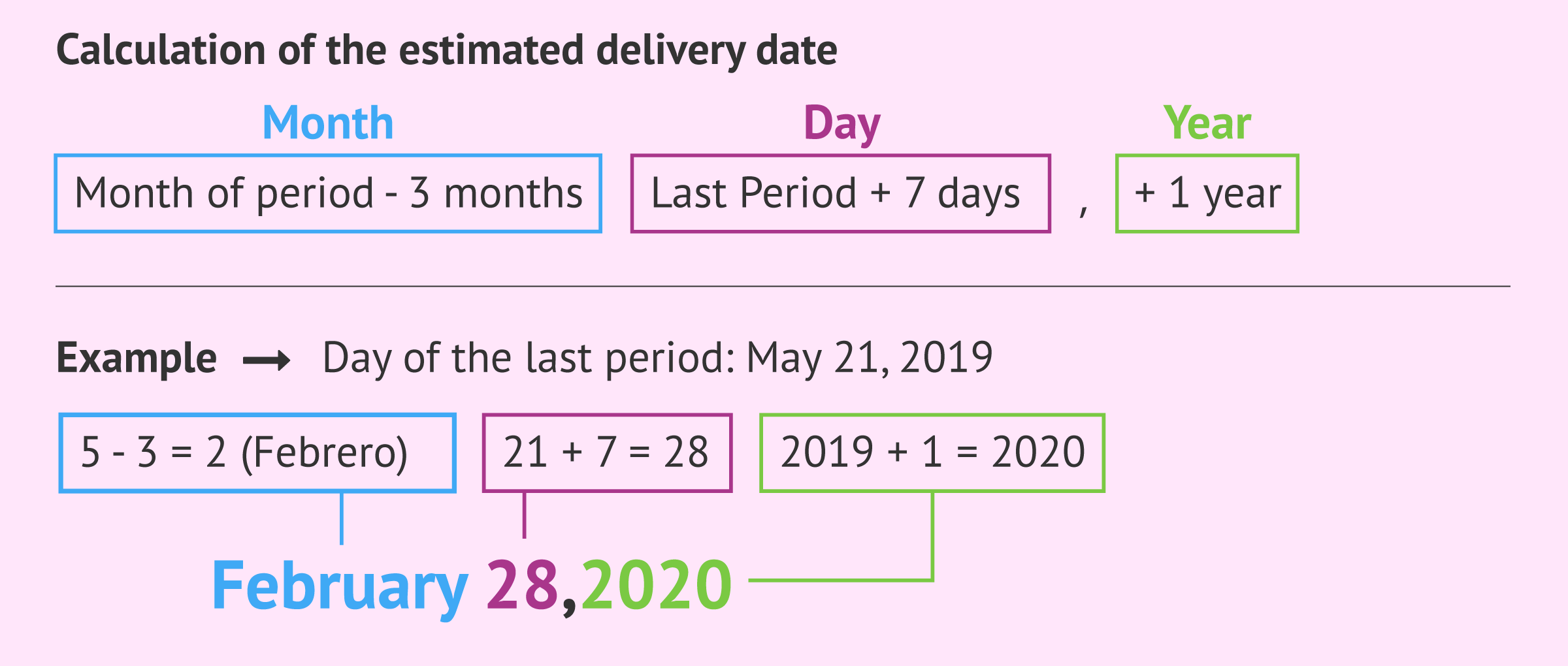
NAGELE’S RULE
Use to determine expected date of delivery (EDD or EDB). It is important to determine the mother’s LMP.
If Jan – March = +9 +7

If Apr – Dec = -3 +7 +1
MC DONALD’S RULE
Use to determine age of gestation in weeks using FUNDIC HEIGHT
FORMULA:
AOG in WKS = FUNDIC HEIGHT (cm) x 8/7
FORMULA:
AOG in MONTHS = FUNDIC HEIGHT (cm) x 2/7
![maternal & child nursing care [autosaved] | PPT](https://image.slidesharecdn.com/healthforce1maternalchildnursingcareautosaved-120524213553-phpapp01/85/maternal-child-nursing-care-autosaved-57-320.jpg)
BARTHOLOMEW’S RULE
Use to determine age of gestation by proper location of fundus at abdominal cavity
< 12 weeks = not palpable/pelvic cavity
3 months = above symphysis
5 months = level of umbilicus
7 months = bet. Umbilicus and xyphoid
9 months = touching/below xyphoid
10 months = level of 9 months due to lightening; about 4 cm
LEOPOLD’S MANEUVER
1st MANEUVER: Purpose: to determine the fetal presentation/lie through fundal palpation
If palpated a round, hard and movable – BREECH presentation
If palpated round, soft and immovable - HEAD/CEPHALIC presentation
2nd MANEUVER: Purpose: to determine the back of fetus to hear the fetal heart sound
If smooth hard and resistant surface - FETAL BACK
If angular nodulations - KNEES AND ELBOWS
3rd MANEUVER: Purpose: to determine the degree of engagement by palpating the lower uterine segment
If the presenting part is movable: NOT ENGAGED
If the presenting part is immovable: ENGAGED
HARD: HEAD
SOFT, GLOBULAR, LARGE: BUTTOCKS
4th MANEUVER: Purpose: to determine the fetal attitude –relationship of fetus to each part or degree of flexion by grasping the lower quadrant of abdomen. It is done only if the fetus is in cephalic presentation.
Full Flexion if the fetal chin touches chest
Psychological Changes of pregnancy
Pregnancy is such a huge change in a woman’s life and brings about more psychological changes than any other life event beside puberty.
A woman’s attitude towards a pregnancy depends a great deal on psychological aspects: such as:
The environment in which she was raised
The messages about pregnancy her family communicated to her as a child
The society and culture in which she lives as an adult
Whether the pregnancy has come at a good time in her life
Psychological Changes of Pregnancy
Social Influences
Cultural Influences
Family Influences
Individual Differences
Partners Adaptation
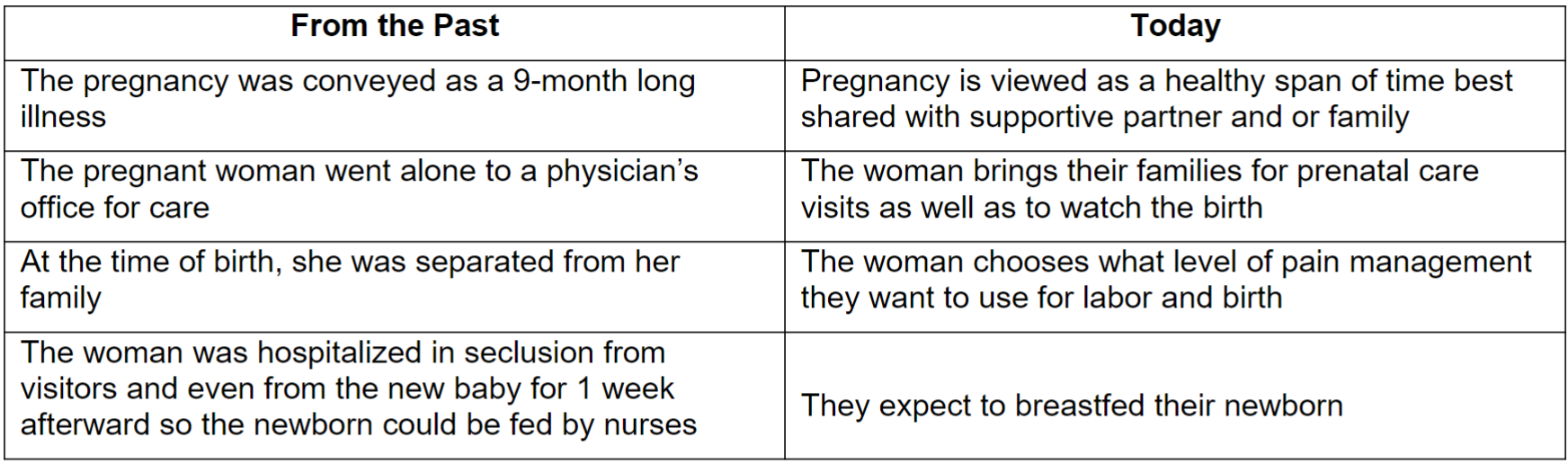
Social Influences
The woman and her partner feel during pregnancy and prepared to meet the challenges are related to them:
a. Cultural background
b. Personal beliefs
c. Experiences reported by friends and relatives
d. Current plethora of information available
Nurse’s Role
1. Teaching the woman about their health care option
2. Continue to work with other health care provider to “demedicalize” childbirth
the process by which a condition or behavior is no longer considered a medical issue, removing it from clinical diagnosis and treatment.
Cultural influences
Cultural beliefs and taboos can place restrictions on a woman’s behavior and activities regarding her pregnancy
During prenatal visits, ask the woman and her partner if there is anything, they believe that should or should not be done to make the pregnancy successful and keep the fetus healthy.
Examples: Beliefs
Lifting the arms over the head during pregnancy will cause the cord to twist
Watching a lunar eclipse will cause a birth deformity
Nurse’s Role:
1. Supporting these beliefs shows respect for the individuality of a woman and her knowledge of good health.
2. Find a compromise that will assure a woman that these are not really harmful to a fetus but that still respects these beliefs
Family Influences
The family in which woman raised can be influential to her beliefs about pregnancy
Woman and her siblings were loved and seen as a pleasant outcome is more likely to have a positive attitude towards her pregnancy
A woman who views mothering a positive activity is more likely to be pleased when she becomes pregnant than one who does not value mothering
Negative Influences - woman and her siblings were blamed for the breakup of a marriage or a relationship.
Individual Differences
A woman’s ability to cope with or adapt to stress plays a major role in how she can resolve any conflict and adapt:
a. To being a mother without needing mothering, to loving a child as well as partner
b. To becoming a mother for each new child depends on her basic temperament on whether she adapts to new situations quickly or slowly, whether she face them with intensity or maintain a low-key approach, and whether she had experience coping with change and stress
c. The extent to which a woman feels secure in her relationship with the people around her
d. Past experiences influence on how woman perceive pregnancy as a positive or negative experience
e. To being concerned about her appearance
f. To being worry that pregnancy will rob her financially and ruin her chances of job promotion
Nurse’s Role:
1. Assessing and counselling pregnant woman
2. Fill the role of an attentive listener
Partner’s Adaptation
The more emotionally attached a partner is to a pregnant woman, the closer the partner’s attachment is apt to be to the child.
Factors that affect the pregnant woman’s decision making:
a. Cultural
b. Past experience
c. Relationships with the family members
Psychological Tasks of Pregnancy
1. First Trimester: Accepting the Pregnancy
● Task: Accepting the pregnancy - woman and partner both spend time recovering from shock of learning they are pregnant and concentrate on what it feels like to be pregnant. A common reaction is ambivalence, or feeling both pleased and not pleased about the pregnancy.
The Woman
● Accept the reality of the pregnancy, later will come the task of accepting the baby, following their initial surprise women often experience the feeling of ambivalence
● Ambivalence – refers to the interwoven feelings of wanting and not wanting feelings which can be confusing to an ordinarily organized woman
● Most women who were not happy about being pregnant at the beginning are able to change their attitude towards their pregnancy by the time they feel the child move inside
● Woman often comment after such visit they feel “more pregnant” or it makes a first visit more than an ordinary one
● Early diagnosis is important because the earlier a woman realizes she is pregnant, the sooner she can begin to safeguard fetal health by discontinuing all drugs not prescribed or approved by her health care provider.
Health care plan:
1. Routine sonogram – to assess for growth anomalies and can be a major step in promoting acceptance because women can see a beating heart or fetal outline or can learn the sex of their fetus.
2. First prenatal visits - hearing their pregnancy officially diagnosed at a first prenatal visit is another step toward accepting a pregnancy
The Partner
● All partners are important and should be encouraged to play a continuing emotional and supportive role in pregnancy
● Accepting the pregnancy for a partner means not only accepting the certainty of the pregnancy and the reality of the child to come but also accepting the woman in her changed state
● Partner may also experience feeling of ambivalence
● Partner may feel proud and happy at the beginning of pregnancy
● Soon begin to feel both overwhelmed with what the loss of salary will mean to the family if the woman has to quit work
● Feeling close to jealousy of the growing baby who although not yet physically apparent, seems to be taking up a great deal of the woman’s time and thought
Health care plan:
o Prenatal visit or fetal testing – provide an outlet for both male and female partners to discuss concerns and offer parenting information.
2. Second Trimester: Accepting the Baby
● Task: Accepting the baby - Woman and partner move through emotions such as narcissism and introversion as they concentrate on what it will feel like to be a parent. Roleplaying and increased dreaming are common
The Woman
● Psychological task of a woman is to accept she is having a baby, a step up from accepting the pregnancy
● The change usually happens at quickening or the first moment a woman feels fetal movement.
● Woman who carefully planned the pregnancy, this moment of awareness may occur soon as she recovers from the surprise of learning she has actually conceived
● She announces the news to her parents and hear them express their excitement and see a look of pride on her partner’s face
● A good way to measure the level of a woman’s acceptance is to measure how well she follows prenatal instructions
The Partner
● A partner may become overly absorbed in work, striving to produce something concrete on the job that may limit the amount of time a partner spends with family
● Some men have difficulty enjoying the pregnancy because they have been misinformed about sexuality, pregnancy, and women’s health.
3. Third trimester: Preparing for parenthood
● Task: Preparing for the baby and end of pregnancy - Woman and partner prepare clothing and sleeping arrangements for the baby but also grow impatient with pregnancy as they ready themselves for birth
The Woman and Partner
● Couples begin “nest building” activities (Planning the infant’s sleeping arrangements, choosing a name for the infant, ensuring safe passage) by learning about birth
● Couples are usually interested in attending prenatal classes and or classes on preparing for childbirth.
● Childbirth education class and or preparing for parenthood can not only help a couple accept but also expose them to other parents as a role models who can provide practical information about pregnancy a concern child care.
Assessing events that could contribute to difficulty accepting Pregnancy:
Pregnancy is unintended
Learning the pregnancy is a multiple, not a single one
Learning the fetus has developmental abnormality
Pregnancy is less than 1 year after the previous one
Family has to relocate during pregnancy (Involves a need to find new support people
The main family support person suffers a job loss
The woman’s relationships end because of partner’s infidelity
There is a major illness in self, partner, or a relative
Complications of pregnancy occur (Hypertension)
The woman has a series of developing experiences (failure in school work)
Emotional responses that can cause concern in Pregnancy
Emotional responses and common reactions helpful to caution a pregnant woman and her partners that the common changes may occur so they’re not alarmed if they appear:
Grief
Narcissism
Introversion versus Extroversion
Body image and Boundary
Stress
Depression
The Confirmation of Pregnancy
A medical diagnosis of pregnancy serves to date when the birth will occur and helps predict the existence of a high-risk status
Pregnancy was diagnosed on symptoms reported by a woman and the signs elicited by a health care provider
Signs and symptoms of Pregnancy
1. Presumptive Signs (Subjective Symptoms) - are findings in connection with the body system in which they occur and are experienced by the woman but cannot be documented by an examiner
a. Breast changes – feelings of tenderness, fullness, tingling, enlargement and darkening of areola
b. Nausea and vomiting – on arising or when fatigue
c. Amenorrhea – absence of menstruation
d. Frequent urination – sense of having to void more often than usual
e. Fatigue - general feeling of tiredness
f. Uterine enlargement – uterus can be palpated over symphysis pubis
g. Quickening - fetal movement felt by woman
h. Linea Nigra – line of dark pigment forms on the abdomen
i. Melasma – dark pigmentation forms on face
j. Striae Gravidarum) - red streaks forms on abdomen
2. Probable Signs (Objective Symptoms) – are findings and can verified by an examiner
Chadwick’s sign - color change of the vagina from pink to violet
Goodell’s sign – softening of the cervix
Hegar’s sign - softening of the lower uterine segment
Sonographic evidence of gestational sac
Braxton Hick’s contraction – periodic uterine tightening
Fetal outline felt by examiner through palpation
Ballottement – the fetus can feel through bimanual examination
Laboratory Tests – blood serum and urine specimen to detect the presence of human chorionic gonadotrophin (hCG)
a. Serum pregnancy test – hCG appear as early as 24 – 48 hrs. after implantation and reach a measurable level about 50 unit/ml 7-9 days after conception
b. Urine sample – concentrated such as a first urine in the morning
c. Home Pregnancy Test -it takes 2-3 mins. to complete and have a high degree of accuracy
d. Early prenatal care – is the best safeguard to ensure successful pregnancy.
3. Positive Signs of Pregnancy
a. Sonographic evidence of fetal outline. – fetal outline can be seen and measure by sonogram
b. Fetal movement felt by examiner
c. Fetal heart audible – doppler ultrasound reveal heartbeat (10th – 12th week of gestation
Physiologic Changes of Pregnancy
They can categorize as local (confined to the reproductive organs) or systemic (affecting the entire body)
1. Reproductive System Changes
a. Uterine Changes – increase the size of the uterus to accommodate the growing fetus. The uterus increases in length, depth, width, weight, wall thickness and volume
Length – from 6.5 - 32 cm;
Width – from 4cm to 24 cm;
Weight - increases from 50g to 1000g;
Depth- increases from 2.5 cm to 22 cm
Uterine wall thickens from 1cm to 2cms
Volume – increases from 2 ml. to more than1,000 ml. can hold a total of 4000g at term (7-lb (3.175 g.) fetus, 1,000 ml. amniotic fluid
Fundus height at various week of pregnancy
20-22nd week – reaches the level of the umbilicus
36th week – touches the xiphoid process
38th week – fetal head settles into the pelvis
Hegar’s signs – extreme softening of the lower uterine segment
Ballottement – the fetus can be felt to bounce or rise in the amniotic fluid
Braxton Hick’s contraction
Amenorrhea
b. Cervical changes – becomes more vascular and edematous
Goodell’s sign - softening of the cervix
c. Vaginal Changes – increase vascularity of the vagina
Chadwick’s sign - changes in color from light pink to a deep violet
d. Ovarian Changes – active production of estrogen and progesterone
e. Breast changes
Feeling of fullness, tingling or tenderness because of increased estrogen level
Breast size increase because of the growth in mammary alveoli and in fat deposit
Areola of the nipple darkens and the diameter increases from about 3.5 cm (1.5 inches) to 5cm or 7 cm (2 or 3 inches)
2. Endocrine changes
● Increased thyroid and parathyroid hormone production
● Palmar erythema
● Insulin production is decreased early during pregnancy and increases after the 1st trimester
● Prolactin, Melanocyte-stimulating hormone, and human growth hormone of the pituitary gland increase,
ESTOGEN AND PROGESTERONE produced
● Placenta as a transient endocrine organ
● Colostrum can be expelled as early as 16 weeks
● Increase vascularity
● Enlarge and protuberant nipples
3. Respiratory system
● Shortness of breathing is common
● Marked congestion or stuffiness – due to increase estrogen
6.Cardiovascular system
● 30-50% increase in the total cardiac volume
● Physiologic Anemia of pregnancy may occur
● Increases heart rate
● Palpitations is common
● Edema and varicosities of the lower extremities
7. Gastrointestinal system
● Slow emptying time of the stomach
● Nausea and vomiting
● Decreased pH of the saliva
● Hemorrhoids is common due to constipation, pressure of the uterus, slow peristalsis
8. Urinary System
● Glomerular Filtration rate increases
● BUN and Plasma Creatinine decreases
● Renal threshold for sugar decreases
● Frequent urination in 1st trimester, normalizes in 2nd trimester, frequent urination in 3rd trimester
9. Muscular system
● Calcium and Phosphorus needs are increased
● Gradual softening of the pelvic ligaments
● Wide separation of the symphysis pubis
10. Immune system
● IgG production decreases
● WBC simultaneously increases
RECOMMENDED WEIGHT GAIN DURING PREGNANCY
A weight gain of 11.2 to 15.9 kg (25 to 35 lb) is recommended as an average weight gain in pregnancy.
Weight gain in pregnancy occurs from both fetal growth and accumulation of maternal stores and occurs at approximately 0.4 kg (1 lb) per month during the first trimester and then 0.4 kg (1 lb) per week during the last two trimesters (a trimester pattern of 3-12-12).
As a general rule, in the average woman, weight gain is considered excessive if it is more than 3 kg (6.6 lb) a month during the second and third trimesters; it is less than usual if it is less than 1 kg (2.2 lb) per month during the second and third trimesters.
Women can be assured that most of the weight gained with pregnancy will be lost afterward
To ensure adequate fetal nutrition, advise women not to diet to lose weight during pregnancy. Weight gain will be higher for a multiple pregnancy than for a single pregnancy. You can encourage women pregnant with multiple fetuses to gain at least 1 lb per week for a total of 40 to 45 lb
Sudden increases in weight that suggest fluid retention or polyhydramnios (excessive Amniotic fluid) or a loss of weight that suggests illness should be carefully evaluated at prenatal visits.