Lecture 10: Alteration in pulmonary function
alterations of pulmonary function:
pulmonary disease is often classified as
acute or chronic
obstructive or restrictive
infectious or noninfectious
signs and symptoms of pulmonary disease:
pulmonary disease have many signs and symptoms (the most common symptoms are cough and dyspnea)
dyspnea
subjective sensation of uncomfortable breathing and feeling of unable to get enough air
orthopnea
dyspnea when a person is lying down
orthopnea is generally relieved by sitting up in a forward leaning position
paroxysmal nocturnal dyspnea is caused by fluid in the lungs
dyspnea causes
decreased ph, increased PaCO2, an decreased PaO2
decreased blood flow to the medulla oblongata
causes alternating periods of deep and shallow breathing
fatigue of the intercostal muscles and diaphragm
abnormal breathing patterns
kussmaul respirations (hyperpnea)- characterized as a slightly increased ventilatory rate; large, tidal volumes; and no expiratory pause
cheyne-stokes respirations- characterized by alternating deep and shallow breathing
hypoventilation- inadequate alveolar ventilation in relation to metabolic demand
hyperventilation- alveolar ventilation exceeds metabolic demand - lungs remove co2 faster - respiratory alkalosis can result
hyperventilation causes hypocapnia (reduced co2 in blood, not necessarily bad in short term)
cough- important reflex
acute cough
chronic cough
hemoptysis- coughing blood
cyanosis is bluish discoloration of the skin and mucous membrane caused by
increasing amount or desaturated or reduced hemoglobin in blood
usually develops when 5g of Hb is desaturated
pain- caused by pulmonary disorders
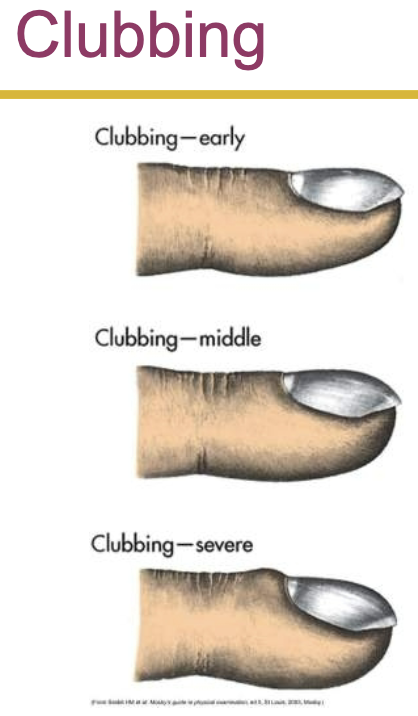
clubbing- the selective bulbous enlargement of the distal segment of a digit and is commonly associated w diseases that interfere with oxygenation of the blood
abnormal sputum- color, consistency, odor, and amount
conditions caused by pulmonary disease or injury:
hypercapnia- increased co2 in arterial blood caused by hypoventilation
hypoxemia- reduced oxygenation of arterial blood
high altitudes may produce hypoxemia through decreased inspired oxygen
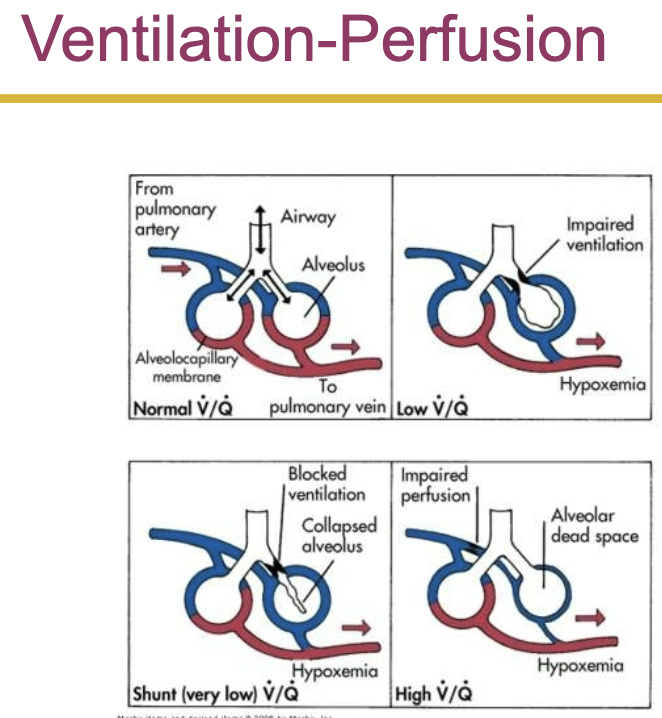
hypoxemia is most commonly caused by abnormal ventilation-perfusion ratio
pulmonary emboli causes alveolar dead space- alveolar is ventilated but not perfused
acute respiratory failure- inadequate gas exchange (hypoxemia or hypercapnia)
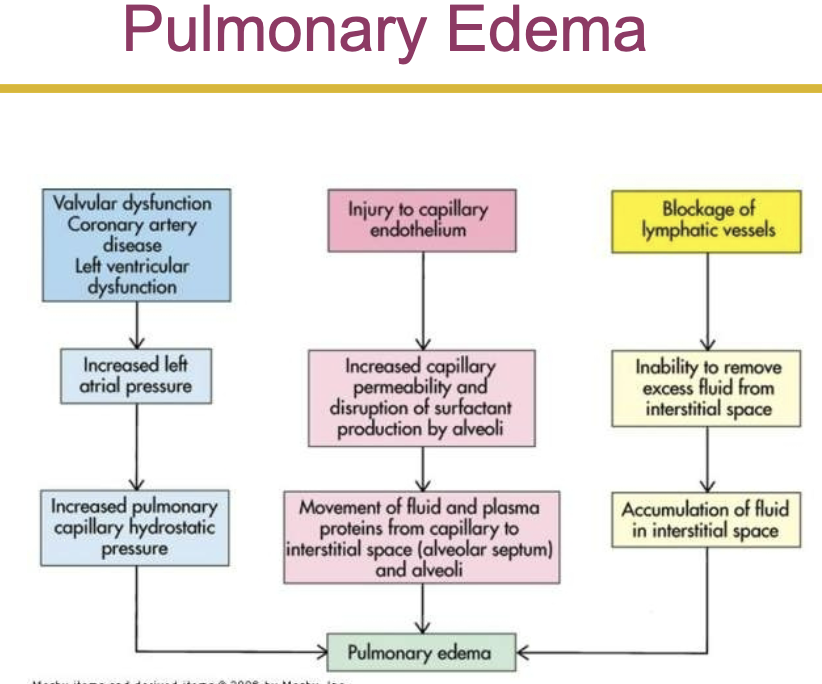
pulmonary edema
excess water in the lungs
edema and pulmonary fibrosis cause hypoxemia by impairing diffusion through the alveolocapillary membrane
the most common cause of edema is left sided heart failure
pulmonary edema usually begins when pulmonary capillary wedge pressure or left atrial pressure is 20mmhg
aspiration
passage of fluid and solid particles into the lungs due to impaired swallowing mechanism and cough reflex
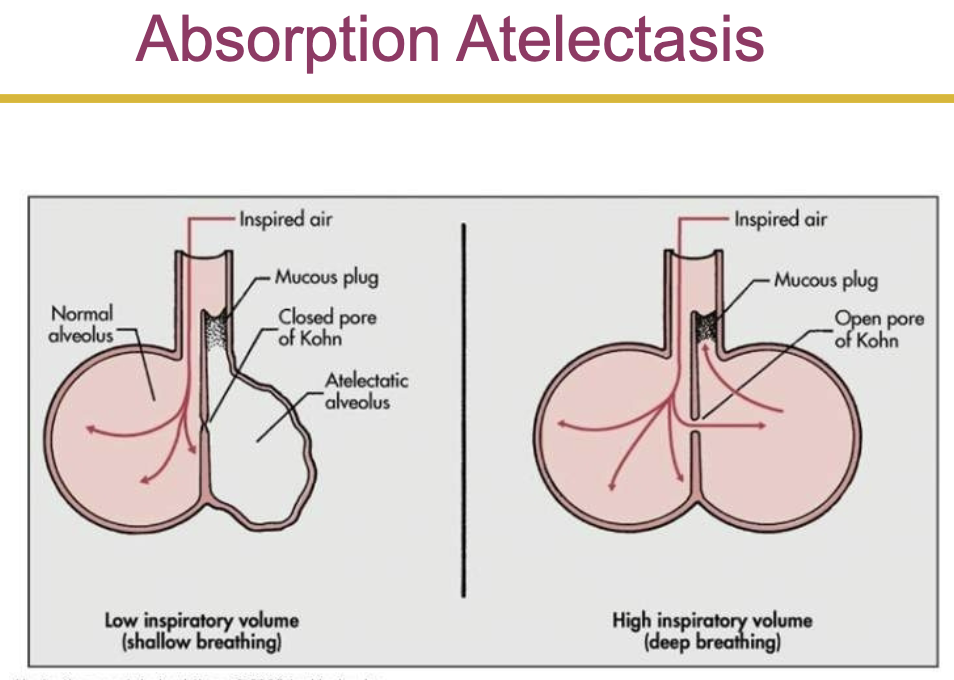
atelectasis- collapse of lung tissue
compression atelectasis- caused by external pressure
absorption atelectasis- the collapse of lung tissue caused from the lack of collateral ventilation through the pores of Kohn
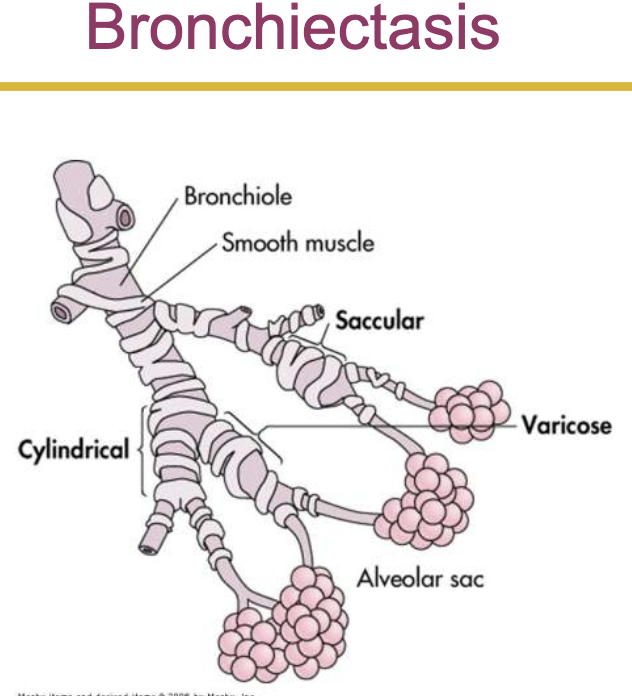
bronchiectasis
persistent abnormal dilation of the bronchi
in varicose bronchiectasis, constrictions and dilations deform the bronchi
bronchiolitis
inflammatory obstruction of the small airways
most common in children
occurs in adults w chronic bronchitis, in association with a viral infection, or with inhalation of toxic gasses
bronchiolitis obliterans
late stage fibrotic disease of the airways
can occur w all causes of bronchiolitis
pleural abnormalities:
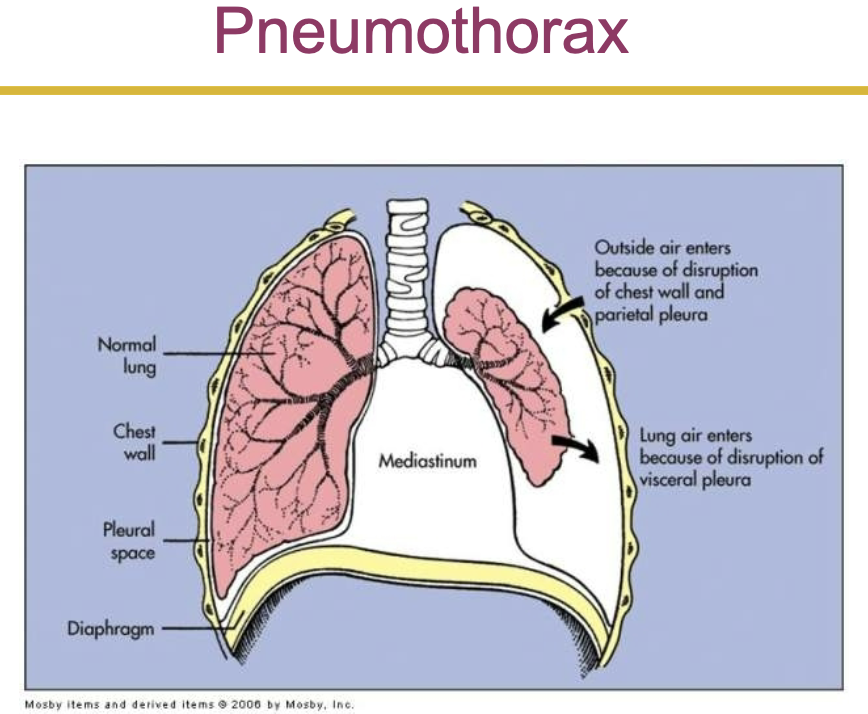
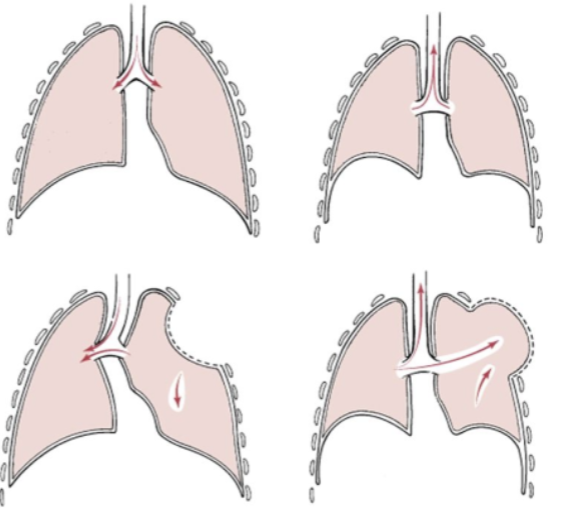
pneumothorax- the presence of gas or air in the pleural caused by rapture in visceral pleura
open pneumothorax- air pressure in pleural space equals barometric pressure
the lung no longer has the negative pressure environment it uses in order to expand
tension pneumothorax- involves a site of pleural rupture that acts as a one way valve, permitting air to enter on inspiration, but preventing its escape by closing during expiration
air builds up, putting pressure on the lung and compressing it
pleural effusion- the presence of fluid in the pleural space
transudative effusion- the fluid is watery and diffuses out of the capillaries as a result of increased blood pressure or decreased capillary oncotic pressure
exudative effusion- is less watery and contains high concentration of wbcs
empyema
involves an infected pleural effusion, the presence of pus in the pleural space, and a complication of respiratory infection, usually pneumonia
conditions caused by pulmonary disease or injury:
pulmonary fibrosis
excessive amount of fibrous or connective tissue in the lung
chest wall restriction
compromised chest wall
caused by neuromuscular disease, gross obesity, severe kyphoscoliosis (lateral bending and rotation of the spinal column, w distortion of thoracic cage)
(flail chest- when multiple adjacent ribs are fractured in 2+ places which causes a section of the chest to lose stability causing it to move in the opposite direction that it should during breathing (it follows the lungs with pressure, inhalation = negative pressure in flail chest so goes in (instead of forcing air in bc the chest cant move) and vice versa)
inhalation disorders
exposure to toxic gasses
pneumoconiosis- any change in the lungs caused by inhalation or inorganic dust particle
silicosis and asbestosis
caused by inhalation of inorganic dust particles (ex. silicon)
cause inflammation and cellular apoptosis of lung cells
pulmonary disorders:
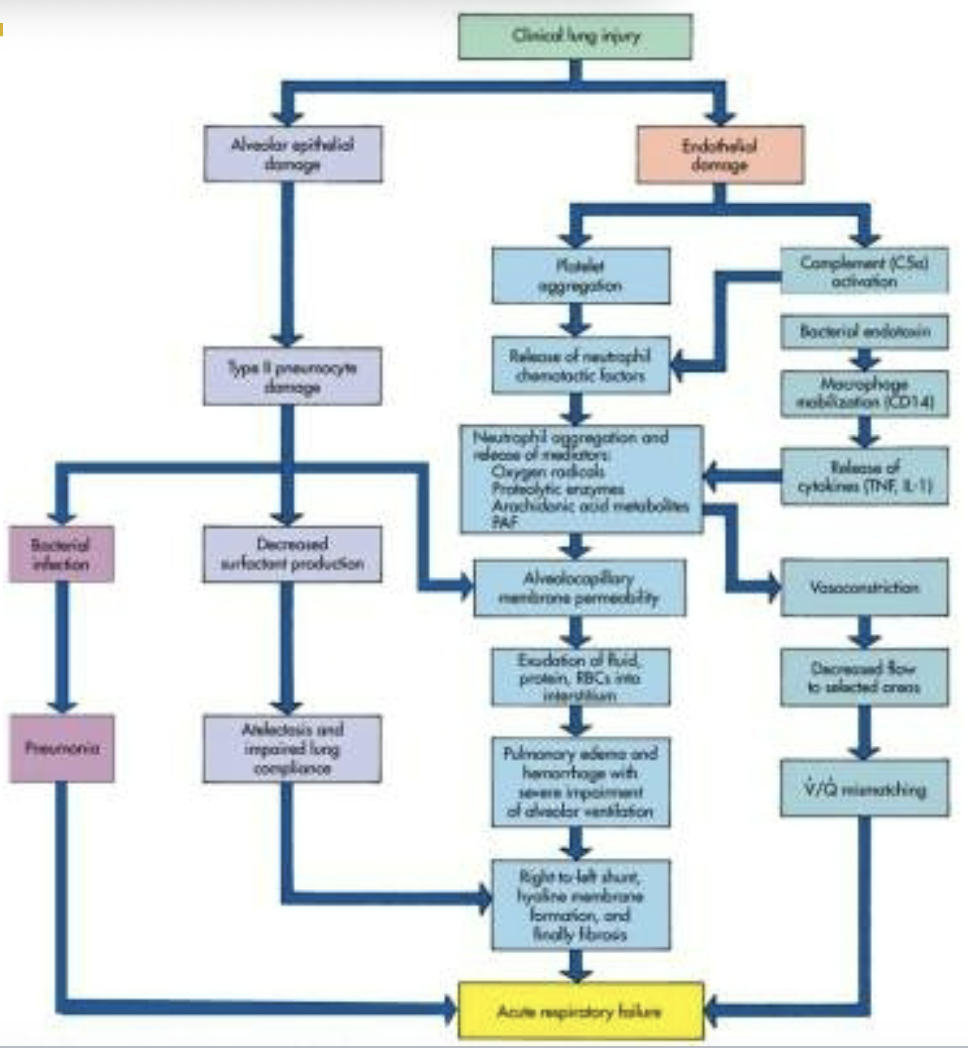
acute respiratory distress syndrome (ards)
is a fulminant (sudden development or rapid progression) form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury
injury to the pulmonary capillary endothelium
inflammation leads to complement cascade and platelet activation
complement cascade releases inflammatory mediators such as proteolytic enzymes, oxygen free radicals, prostaglandins, leukotrienes, and platelet activating factor
increased capillary permeability causes pulmonary edema
surfactant is inactivated and type 2 alveolar cells are impaired, this causes alveoli and respiratory bronchioles to fill w fluid
manifestations
rapid, shallow breathing
respiratory alkalosis
dyspnea
decreased lung compliance
unresponsive hypoxemia
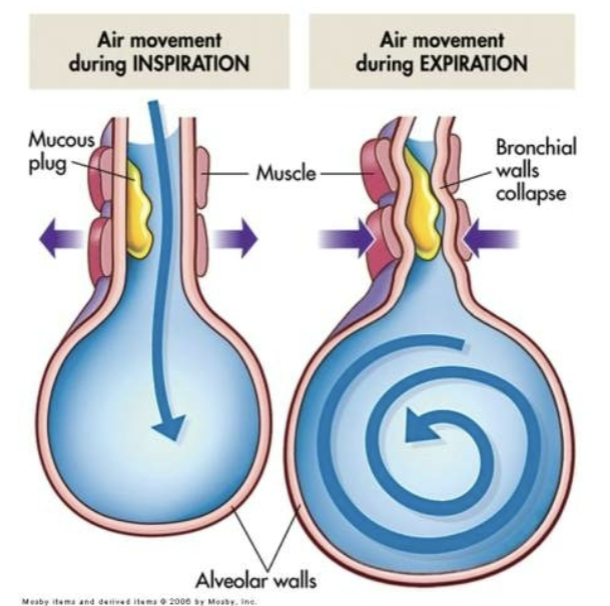
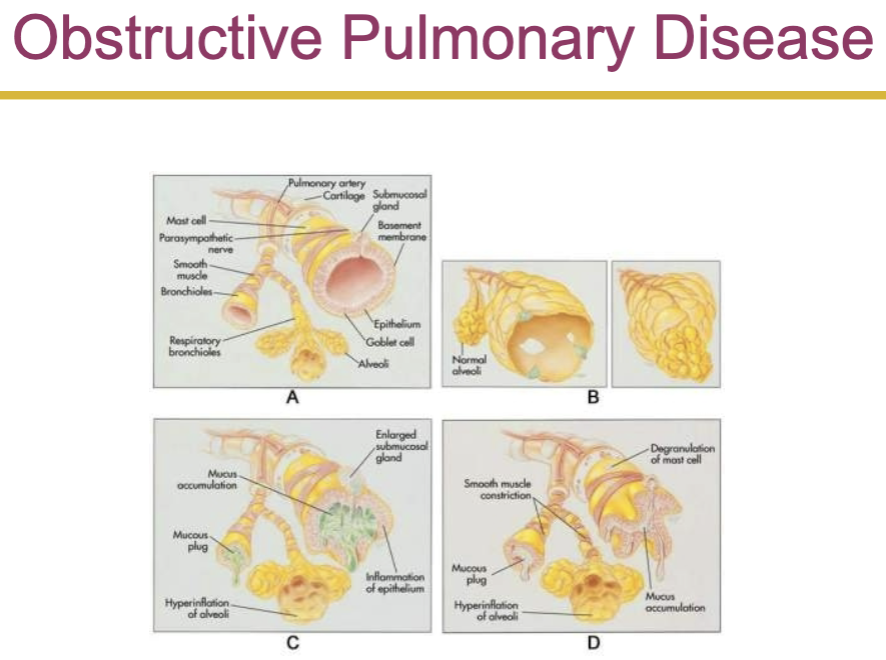
obstructive pulmonary disease:
in obstructive pulmonary disease either more force is required to expire a given volume of air, or emptying of the lungs is slowed, or both
airway obstruction that is worse w expiration
common signs and symptoms
dyspnea and wheezing
common obstructive disorders
asthma
emphysema
chronic bronchitis- caused when h influenzae and streptococcus pneumoniae bacteria become embedded in the airway secretions
manifestations: decreased exercise tolerance, wheezing, shortness of breath, and productive cough
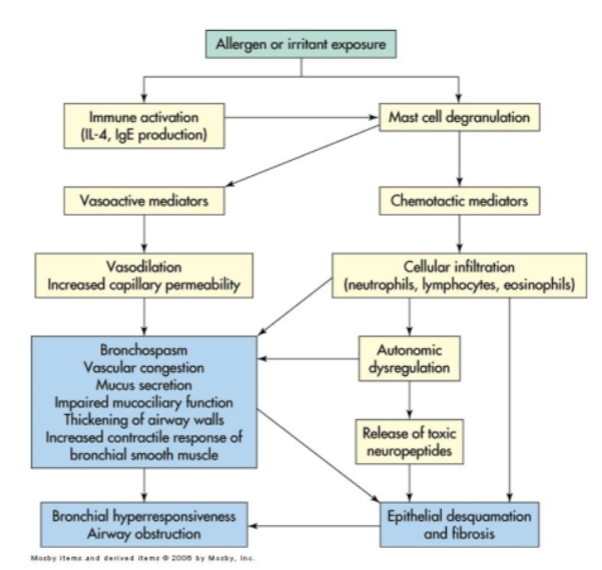
asthma
immunoglobulin e may contribute to the pathophysiology of asthma
inflammatory mediators such as histamine, prostaglandins, and leukotrienes are produced in asthma
manifestations: inspiratory and expiratory wheezing, dyspnea, nonproductive cough, and tachypnea
elimination of the causative agent is the most successful treatment for asthma
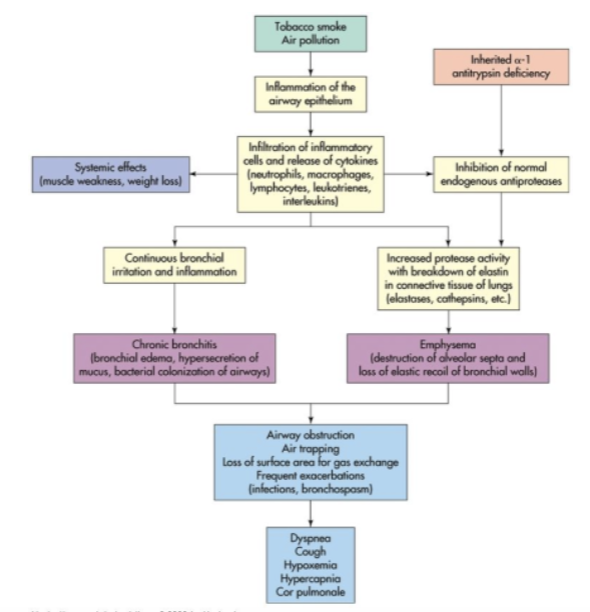
chronic obstructive pulmonary disease:
chronic bronchitis
hypersecretion of mucus and chronic productive cough that lasts for at least 3 months of the year and for at least 2 consecutive years
inspired irritants increase mucous production and the size and number of mucous glands
the mucous is thicker than normal
emphysema
abnormal permanent enlargement of the gas exchange airways accompanied by destruction of alveolar walls without obvious fibrosis
loss of elastic recoil
centriacinar emphysema
panacinar emphysema
manifestations: dyspnea on exertion, use of accessory muscles, tachypnea, and prolonged expiration
respiratory tract infections:
the most common route of lower respiratory tract infection is aspiration of oropharyngeal secretions
tuberculosis
caused by mycobacterium tuberculosis
an acid fast bacillus that usually infects the lungs but may invade other organs
airborne transmission (highly contagious)
tubercle formation
in tuberculosis, the body wall off the bacilli in a tubercle by stimulating apoptotic infected macrophages that activate cytotoxic cells
caseous necrosis
positive tuberculin skin test (ppd)
treatment: antibiotic (type of drug and duration depends in individuals health history)
acute bronchitis
acute infection or inflammation of the airways or bronchi
commonly follows a viral illness
acute bronchitis causes similar symptoms to pneumonia but does not demonstrate pulmonary consolidation and chest infiltrates
chronic bronchitis
pathophysiology: increase in the number and size of mucous glands and goblet cells in airway epithelium
pulmonary vascular disease:
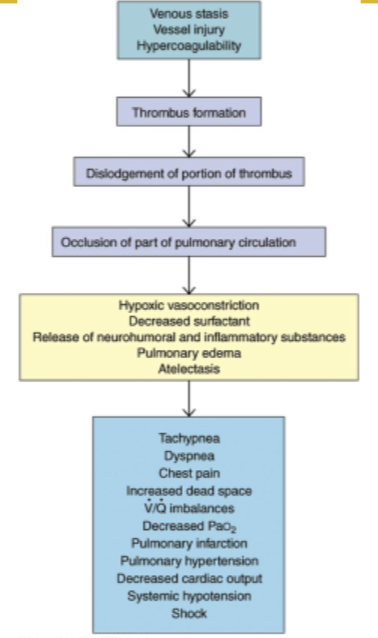
pulmonary embolism
occlusion of a portion of the pulmonary vascular bed by a thrombus, embolus, tissue fragment, lipids, or an air bubble
pulmonary emboli commonly arise from the deep veins in the thigh
the impact of embolus depends on the extend of pulmonary blood flow obstruction, the size of affected vessel, the nature of embolus, and the secondary effects
cancer:
lip cancer
most prevalent in men
the most common form of lip cancer is exophytic
laryngeal cancer
increased by the amount of tobacco smoked
combination of alcohol and smoking increases the risk of
lung cancer:
primary lung cancer arises from the bronchi within lungs, therefore called bronchogenic carcinomas
bronchogenic carcinomas
most common cause is cigarette smoking
heavy smokers have a 20 times greater chance of developing lung cancer than nonsmokers
smoking is related to cancers of the larynx, oral cavity, esophagus, and urinary bladder
environmental or occupational risk factors are also associated with lung cancer
other types of lung cancer are classified into small cell lung carcinoma and non small cell lung carcinoma
non small cell lung cancer
squamous cell carcinoma- slow growing tumor that produces a productive cough and airway obstruction in addition to pneumonia and atelectasis (partial or complete collapse of a lung or lobe of a lung due to the alveoli losing air (either bc they become deflated or filled w fluid))
adenocarcinoma
small cell carcinoma
secretion of antideuretic hormone is the most common paraneoplastic syndrome associated with small cell lung cancer
other lung cancers:
bronchial carcinoid tumors
adenocystic tumors (cylindromas)
mucoepidermoid carcinomas
mesotheliomas