Clinical Interviews, Behavioral Observations, and Self-Monitoring
clinical interview: overview
clinician directed conversation to gain information relevant to
problem definition
diagnosis
case formulation
goal specification
differs from normal conversation
different goals
focus on client
respectful and non-judgmental
confidential (to an extent)
safety exceptions
central role for attending/listening skills
silence, clarification, paraphrasing, summarization
2 types of interviews
UNSTRUCTURED
no standard set of questions or structures method for integrating and summarizing obtained information
STRUCTURED
very specific format for asking questions, determining follow-up questions, integrating and summarizing obtained information
can be semi-structured
follows a script that allows for some divergence if needed to obtain more information
unstructured interview: open questions
ask client why they have come in
follow client’s response
focus on what the client presents, not necessarily psychopathological symptoms
generally use open notebook to take notes on
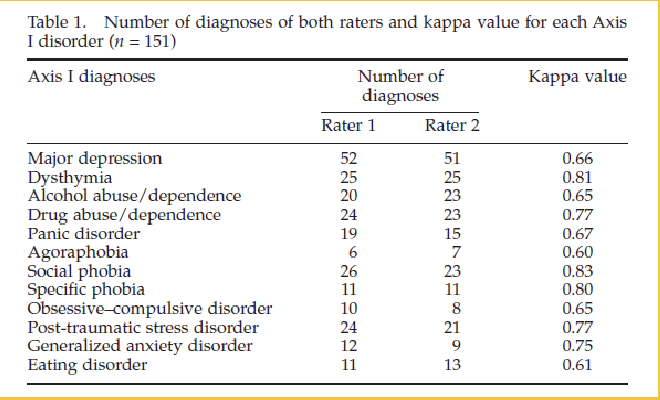
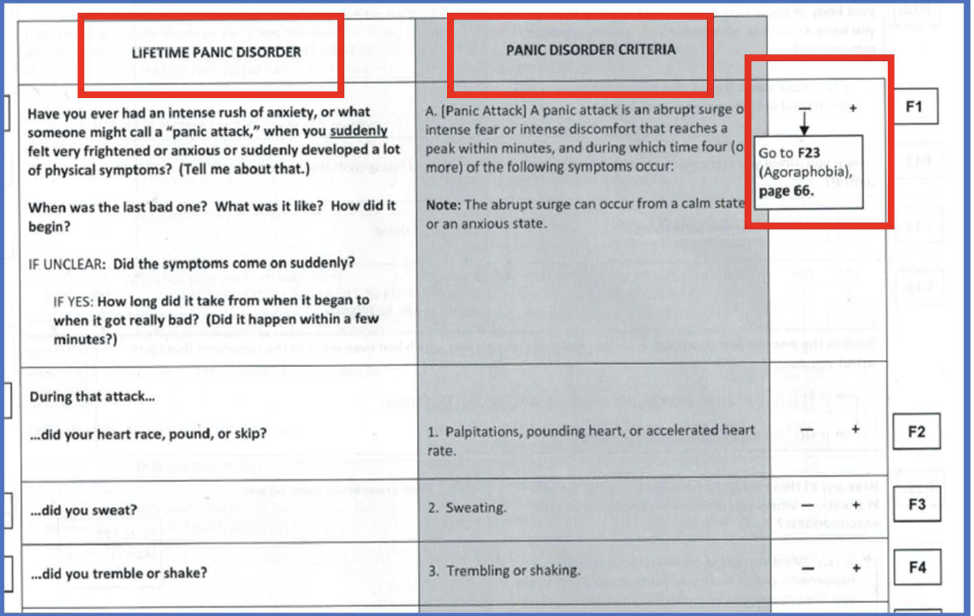
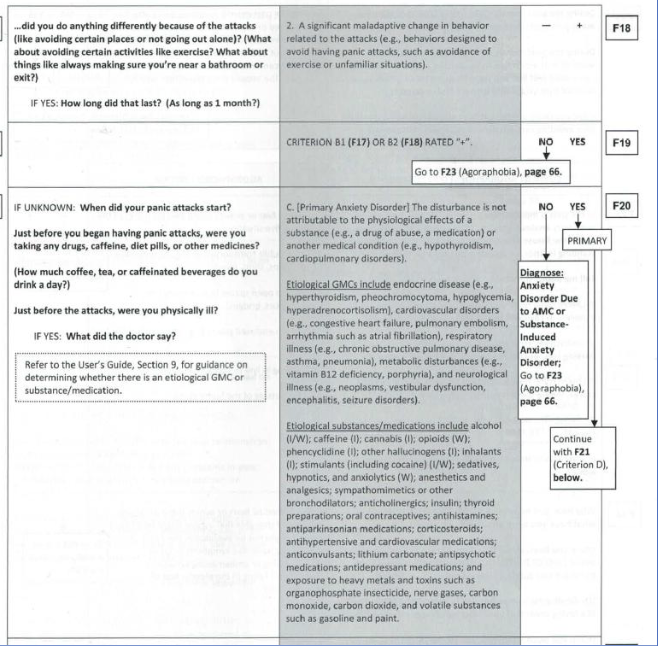
structured interview: SCID
structured clinical interview for mental disorders
SCID
First et al. (2016)
gold standard diagnostic instrument for DSM-5 disorders
training and supervision usually extensive
has moderate to high interrater reliability
Lobbestael et al. (2010)
151 patients and controls
Kappa 0.41-0.75= “fair”
Kappa >0.75= “excellent”
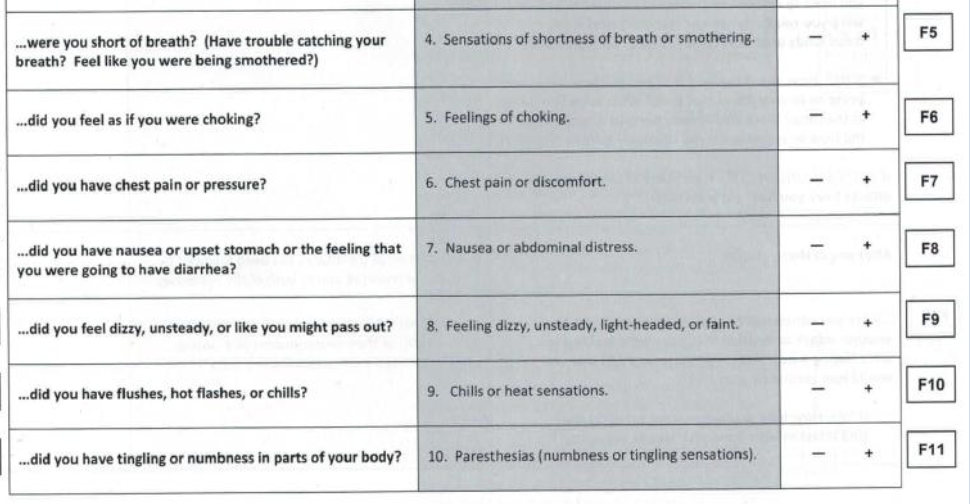
criteria for panic attack (DSM-5)
a discrete period of intense fear or discomfort, in which four (or more) of the following symptoms developed abruptly and reached a peak within 10 minutes
palpitations, pounding heart, or accelerated heart rate
sweating
trembling or shaking
sensations of shortness of breath or smothering
feeling of choking
chest pain or discomfort
nausea or abdominal distress
feeling dizzy, unsteady, lightheaded, or faint
derealization (feelings of unreality) or depersonalization (being detached from oneself)
fear of losing control or going crazy
fear of dying
paresthesias (numbness or tingling sensations)
chills or hot flushes
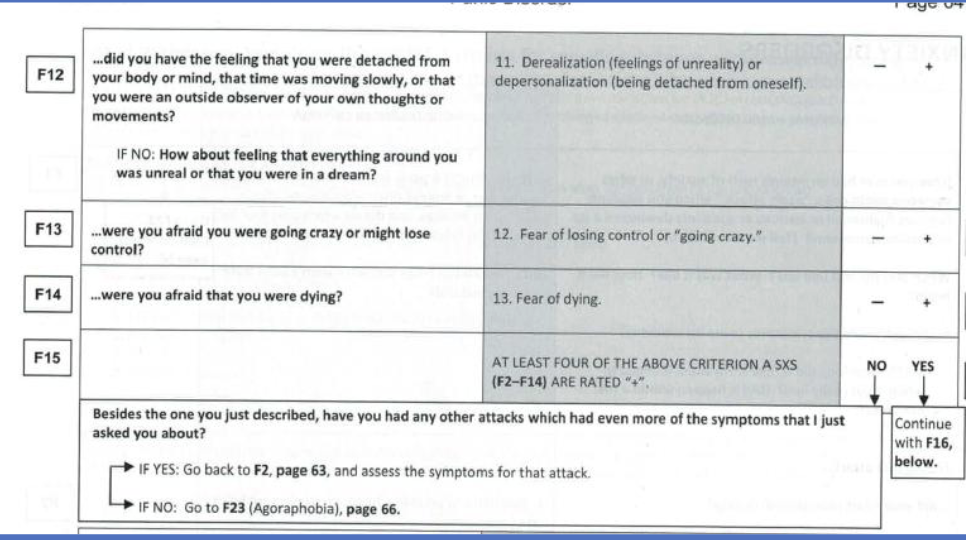
recurrent unexpected panic attacks
at leas one of the attacks has been followed by 1 month (or more) of one or both of the following-
persistent concern or worry about additional panic attacks or their consequences (losing control, having a heart attack, “going crazy”)
a significant maladaptive change in behavior related ro the attacks (behaviors designed to avoid having panic attacks, such as avoidance of exercise or unfamiliar situations)
the disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hyperthyroidism, cardiopulmonary disorders)
the disturbance is not better explained by another medical disorder (e.g., the panic attacks do not occur only in response to feared social situations, as in social anxiety disorder; in response to circumscribed phobic objects or situations, as in specific phobia; in response to obsessions, as in obsessive-compulsive disorder; in response to reminders of traumatic events, as in posttraumatic stress disorder; or in response to separation from attachment figures, as in separation anxiety disorder)
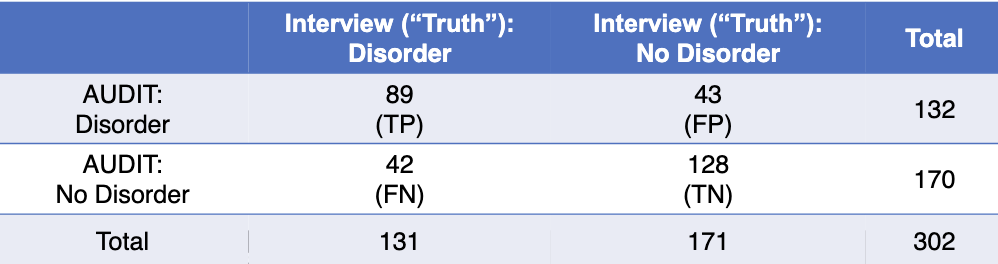
interview vs. questionnaire
diagnostic assessment via questionnaire
evaluate in studies examining diagnostic agreement between interview and questionnaire
treat interview classification of diagnosis or not as “gold standard” against which compare accuracy of questionnaire classification
helps determine whether questionnaire can be used in place of interviews
prior example- AUDIT vs. structured interview
behavioral observations
goal
maladaptive behavior is key aspect of many mental health problems
every behavior has a function/purpose/reason
observation used to identify behavior patterns and generate hypotheses about causal/maintaining factors (reasons for behavior)
always observing in clinical interviews
observation of verbal and nonverbal behavior plays central role
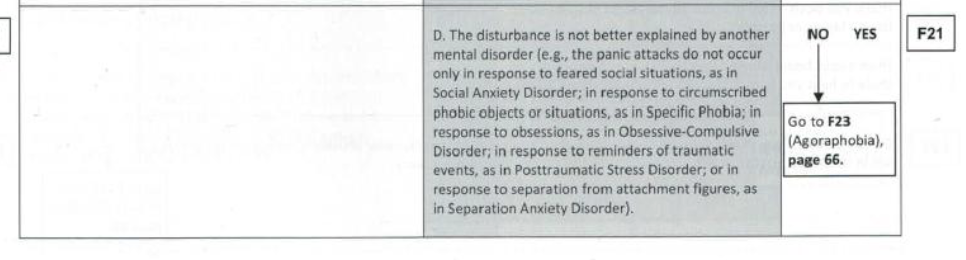
clinician usually observes specific areas
appearance and behavior
mood and affect
perception
comprehension
orientation
insight
memory
content of communication
mental status exam
commonly used system of behavioral observation in psychiatric contexts
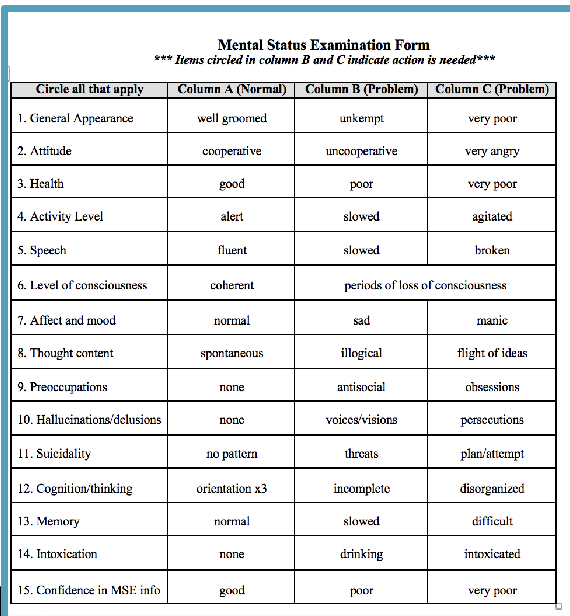
naturalistic behavioral observation
observation within normal situational contexts and under natural occurring reinforcements and consequences
validity and reliability and cost
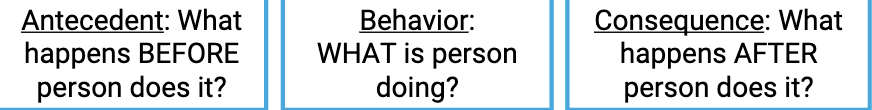
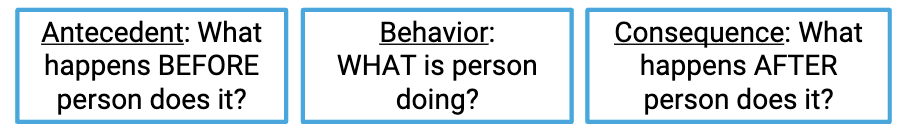
FUNCTIONAL BEHAVIORAL ASSESSMENT
observe behavior
classify behavior into ABCs
3 ideas here-
problematic behavior may be more likely under some conditions (antecedents)
problematic behavior may be reinforced by positive consequences
may be able to modify problematic behavior by changing antecedents and/or
consequences
ex-
structured behavioral observation
observation in role played scenarios in which person engages in one or more simulated social interactions
validity and reliability and cost
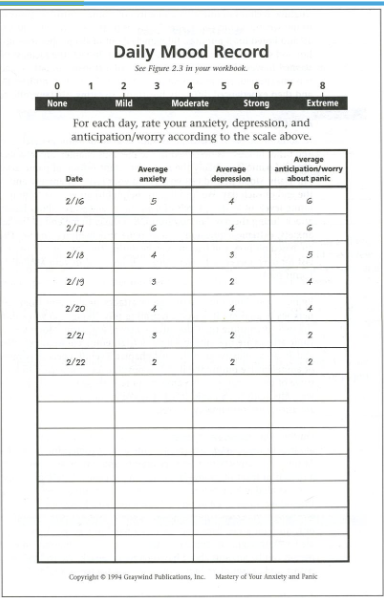
self monitoring
observing and recording own behaviors, thoughts, emotions, bodily sensations, events, etc
provides great deal of info at low cost
characterize problem and presumed causal/maintaining factors
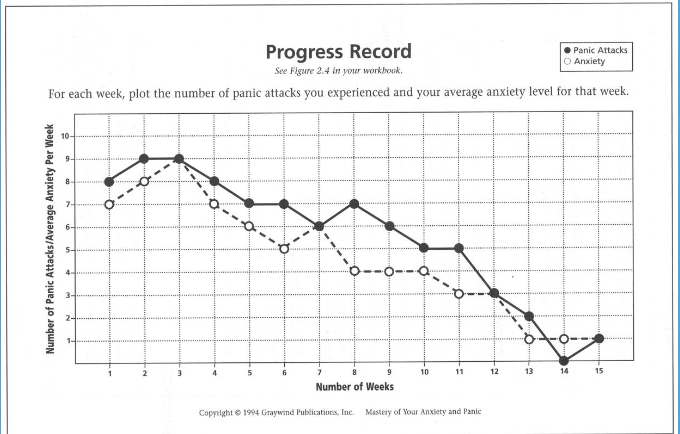
can be used to track treatment progress
can be used to highlight connections btw thoughts, behaviors, feelings, physical sensations, etc.
ABCs
contributes to objective self awareness
problems
inaccuracy and distortion, reliability and validity
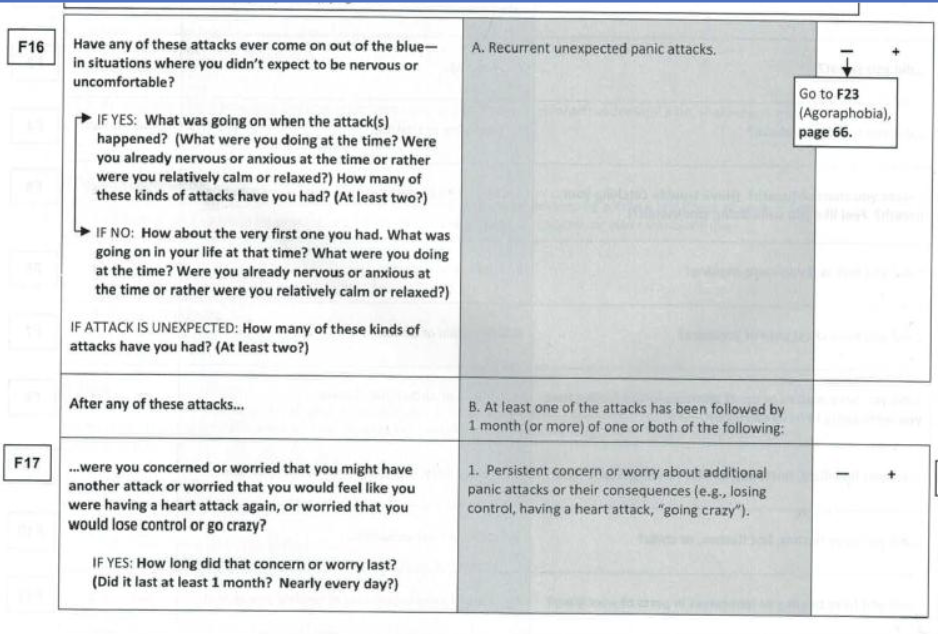
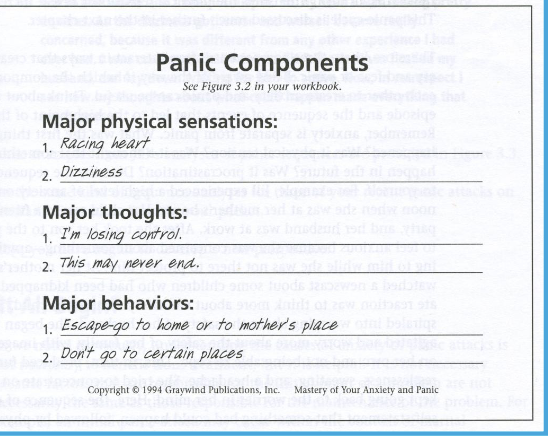
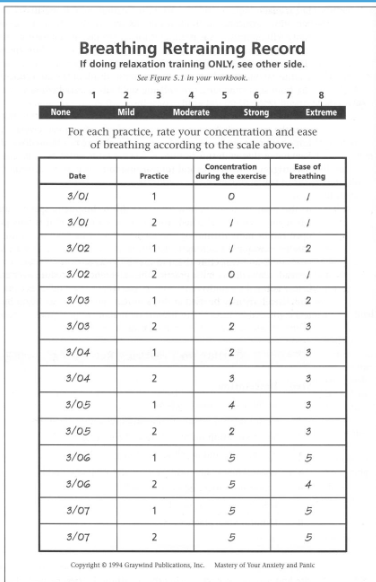
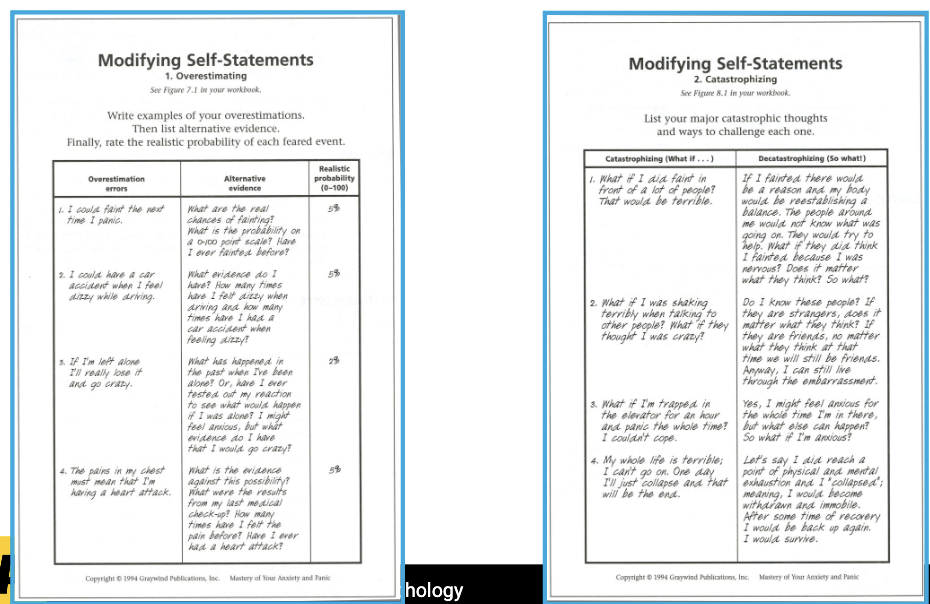
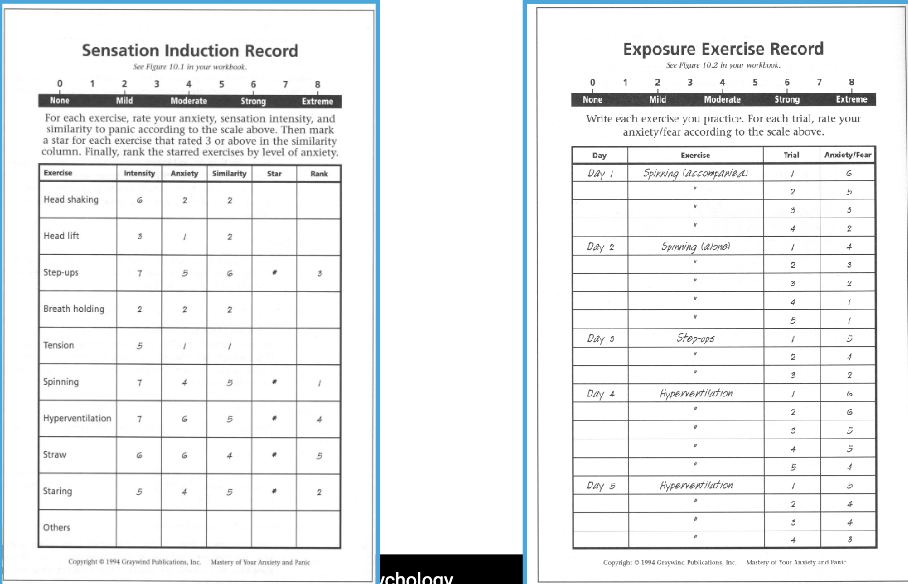
role of monitoring in cognitve-behavior therapy for panic disorder
evidence of effectiveness
70-80% panic free
50-70% within normal range of functioning
gains largely maintained over 2 year follow up
treatment components
education about nature and causes of panic and anxiety, how perpetuated by feedback loops among physical / cognitive / behavioral systems
breathing retraining to address Sx of chronic hyperventilation that are similar to PA Sx
cognitive restructuring to identify, challenge, and replace distorted thoughts and beliefs
exposure to physical sensations of PA, to activities that provoke PA sensations, to situations avoided b/c of concern couldn’t escape / get help (agoraphobia)
evidence based symptom record
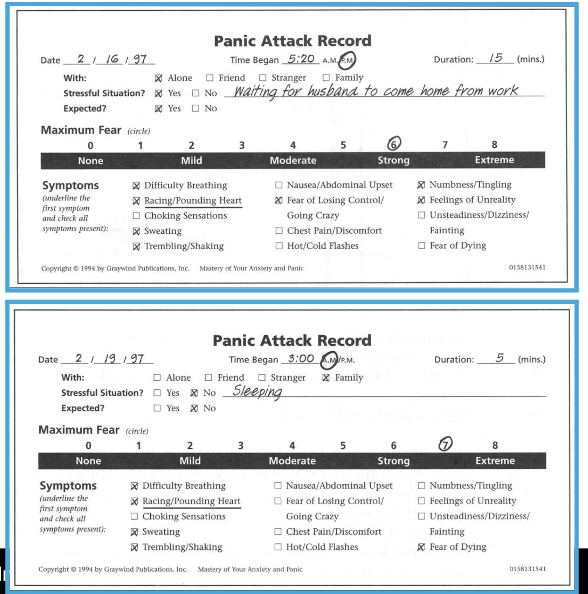
daily/weekly symptom record
education: linking sensations, thoughts, and behaviors
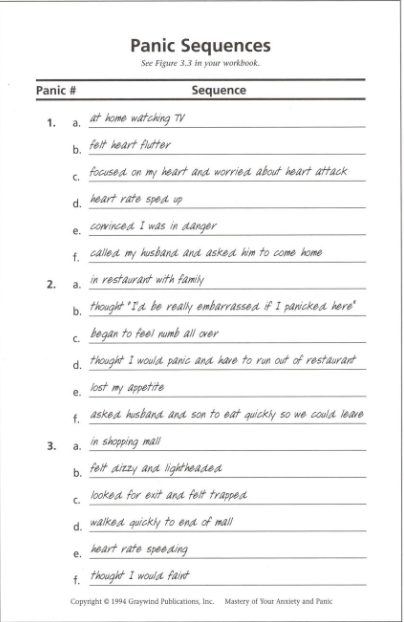
physiology: breathing retraining
cognitive restructuring: challenging thoughts
behavior: gradual exposure
reactivity to self monitoring
REACTIVITY: changes in behavior being assessed due to process of self-monitoring
mechanisms- change in perceptions of behavior?
clients frequently admit not realizing how often behavior is occurring
clients recognize behavior somewhat predictable in ways that potentially can anticipate, control, better prepare for, etc
typically see improvement
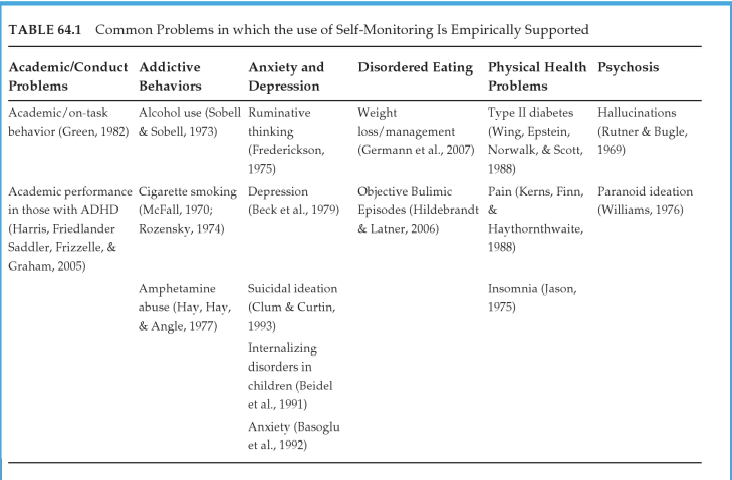
self-monitoring considered empirically supported treatment for number of conditions
self monitoring interventions
present rationale underlying self monitoring
select the target response
record the target response
chart/graph the target response
display the data collected
analyze the data collected