Biological Psychology
L5 - HOMEOSTASIS
Homeostasis
Maintaining a relatively stable internal environment despite a changing external environment
body temperature
glucose levels in the blood
oxygen in the blood
blood pressure
can also involve neurotransmitters, hormones, and immune system
careful regulation and balance of bodily processes
requires detection, action and feedback systems
Why Do We Eat?
maintain homeostasis
pleasant
social aspect
keep us warm
build our body, and recycle
stock and release energy
use for muscle power
needed for thinking
energy required for metabolic processes
Digestion in Gastrointestinal (GI) Tract
GI tract is the site of digestion in which food is broken does and absorbed so that the nutrients can be mobilized and delivered as sources of energy
Steps:
starts before eating
mouth: saliva contains enzymes that facilitate breakdown
→ start digestion starch (carbohydrate)
→ bolus: moist ball of chewed food
swallowed → enters oesophagus → food transportation [also says “digestion carbohydrates → into small sugars” but that is duodenum]
stomach:
→ low pH (basic) kills bacteria
→ grinds food
→ ★ start digestion of proteins into amino acids★
→ pepsin: breaks down proteins into amino acids
→ hydrochloric acid: breaks down food into smaller particles
pyloric sphincter → duodenum:
→ enzymes from the pancreas and gallbladder (safra kesesi) continue the metabolic degradation of proteins, and starch as well as complex sugar molecules into simple sugar molecules (glucose)
→ small enough to mix into the bloodstream → processed by the liver
→ fats are broken down (emulsified) by bile acids (made by the liver and stored in the gallbladder and then released into the duodenum)
→ fat molecules can’t pas through the wall of duodenum and are therefore carried via small ducts into the lymphatic system.
small intestine absorption
large intestine absorption
rectum: water and electrolytes (e.g. sodium and potassium) are absorbed from the remaining waste material that is in the large intestine → fluid absorption
anus: remain waste
SUM:
mouth → saliva enzymes
oesophagus → food transport (carbohydrates → simple sugars (glucose) [?]
stomach → low pH (basic) bacteria, (protein → amino acids)
duodenum → juices pancreas neutralizes, bile acids for gallbladder emulsify fats (digestion and absorption of fats)
small intestine absorption
large intestine absorption
rectum (fluid absorption)
Digestion
provides three forms of energy:
lipids (fats)
amino acids (proteins)
glucose (carbohydrates)
NOT all of the energy is used immediately, some of it is stored (most to least) as:
fats (main storage system, accounts for increased body fat)
glycogen (which is converted into glucose)
proteins
→ fat is a physiologically economical way to store energy compared to glycogen
three phases in energy metabolism:
cephalic / reflex phase
gastric / absorptive phase
post-absorptive / intestinal / fasting phase
Cephalic / Reflex Phase
preparatory processes for feeding
sensory stimulus of food activates digestive systems
stops when nutrients are being absorbed into the bloodstream
Absorptive / Gastric Phase
immediate needs of the body are being attended to
nutrients are being absorbed into the bloodstream
nutrients are broken down, absorbed from the gastro-intestinal (GI) tract into the blood, distributed and metabolized for use and storage
lasts 3-4 hours
[Note: whereas in this lecture we contrast ‘Absorptive’ from ‘Post-absorptive’ state, the term ‘postprandially’ (=after a meal) can be used to describe the state of having just eaten. So the absorptive state is postprandially…]
Q: is there much or little food available in your stomach in the absorptive / gastric phase?
→ Much food - just eaten
physical distension created by food in the stomach activates stretch receptors →which then stimulates the parasympathetic release of acetylcholine (ACh)
ACh → increases the secretion of gastric juices
a rising pH (more alkaline) stimulates the release of gastrin (a peptide hormone that stimulates hydrochloric acid (HCI))
gastrin also activates smooth muscle contractions and the movement of food
HCI creates an acidic (low pH) environment for protein digestion
low pH increases firing rate of the vagus nerve
during the gastric (and cephalic) phase, insulin is released rom the pancreas for:
conversion of glucose to glycogen and for fat storage
conversion of amino acids to proteins for storage
storage of glycogen in liver and muscle
storage of fat in adipose tissue
storage of protein in muscles
→ insulin regulates the amount of blood-borne (carried or transmitted by the blood) during different phases
Biomolecules: break it down
Q: can you name the units of the most relevant biomolecules in your body?
→ protein / peptides
→ fat (lipids)
→ carbohydrates
→ nucleic acid
protein / peptides → amino acids
fat (lipids) → triglycerids
carbohydrates (carbs) → glucose
Proteins
> UNIT OF A PROTEIN / PEPTIDE = AMINO ACID
amino acids are used to make new proteins
Q: where do amino acids come from?
→ eaten protein - stomach + pancreas enzymes like pepsin break proteins into peptides - then they are further broken does to amino acids
→ absorbed in the small intestine, carried in the bloodstream
Q: what is an “essential” amino acid?
→ amino acids that our body can’t make on it’s own, we get it from diet (e.g. Histidine, Isoleucine, Leucine, Lysine, Methionine, Phenylalanine, Threonine, Tryptophan, Valine)
Q: what is the difference between a peptide and a protein?
→ size: protein > peptide
→ protein consists of multiple polypeptides
Carbohydrates
> CATABOLISM
break down of complex molecules to release its energy
for example: sucrose (table sugar) → glucose + fructose
mono | = single |
di (mono + mono) | = two |
tri | = three |
poly | = many |
Q: what form of carbs is the most important blood sugar of our body?
→ glucose
> ANABOLISM
generating complex molecules from simple ones to store it’s energy
for example: glycogen (storage of carbs in animals) = multiple glucose molecules bonded together (polysaccharide)
[Fact: experiencing “hitting the wall ” in sports is due to glycogen depletion during long periods of exercise]
Lipids (fats)
> LIPIDS: UNITS, TRIGLYCERIDES & PHOSPHOLIPIDS
catabolized (broken down) units: glycerol and fatty acids (long chains)
analogized (generating) units: triglycerides (body fat) and phospholipids (membrane)
Q: what units are needed to create triglycerides?
→ glycerol + 3 fatty acids
> LIPIDS: STEROIDS
cholesterol promotes cell membrane fluidity and can be synthesizes (metabolized) into steroid hormones (all of them)
> TRANSPORT OF FATTY ACIDS IN THE BLOOD
fatty acids are lipids (cholesterol, specifically), thus water insoluble (lipophilic /fat-loving: dissolves in fat, not water → hydrophobic, avoids water)
lipoproteins:
transport unit for lipids, secreted by the liver
a combination of protein, triglycerides, cholesterol in a phospholipid membrane
low density lipoprotein (LDL): deposits excess cholesterol on the artery walls, promoting plaque formation → “bad” cholesterol
high density lipoprotein (HDL): scrapes away necessary LDL from artery walls, preventing plaque formation → “good” cholesterol
HDL < LDL
Absorptive phase: glucose
glucose is:
used for energy (all cells)
stored as glycogen (muscle and liver)
transformed into fat (liver and fat cells)
→ Q: during the absorptive state what three things can happen to glucose?
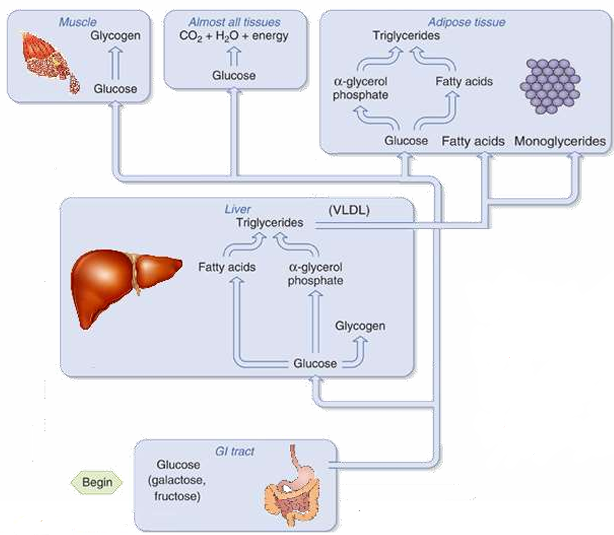
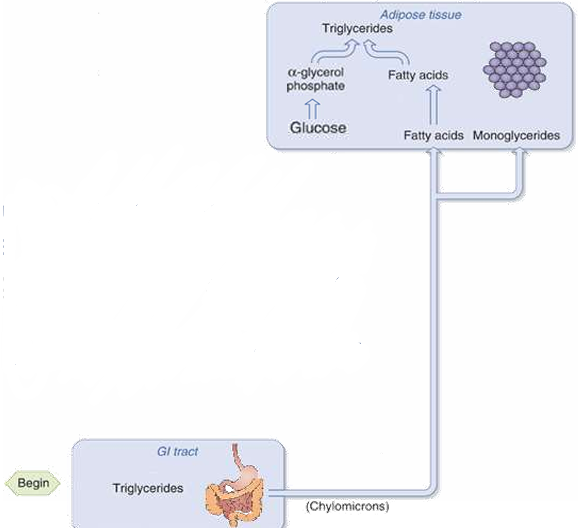
Absorptive phase: lipids
lipogenesis: fatty acids are taken up by adipose (fat) tissue, combined with a-glycerol phosphate to form triglycerides
[Note: glucose in the form of glycerol is needed for triglyceride synthesis]
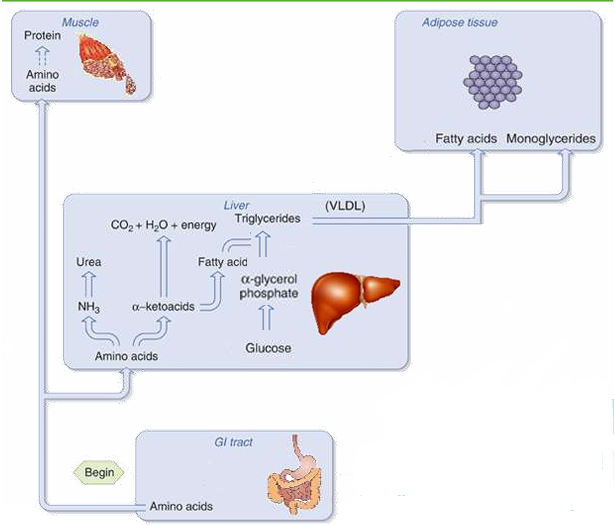
Absorptive phase: amino acids
analogized into new proteins (protein synthesis)
metabolized into a-ketoacids for energy
metabolized into fatty acids for storage (lipogenesis)
→ Q: what three things happen to amino acids during the absorptive phase?
Body composition
daily food intake compromises 44-65% carbs (body comprises of only 1% carbs)
Q: where do all the carbs that you eat go?
→ stored as fat
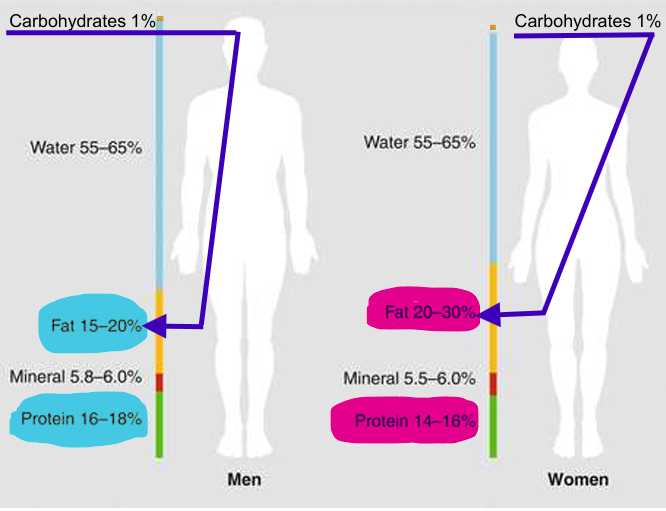
Q: what are the main differences in body composition between women and men?
→ women have more fat
→ man have more protein, therefore muscle
Post-absorptive / Intestinal / Fasting Phase
occurs when nutrients no longer provide immediate energy and the boy has to mobilize previously stored nutrients, e.g. fats.
begins after about 4 hours of fasting
stored nutrients are mobilized, maintaining a stable blood glucose supply
→ glycogenolyse = glucose is released from stored glycogen (limited supply)
→ gluconeogenesis = new glucose made from amino acids (a-ketoacids)
→ triglycerides are converted into ketones for fuel
[Note: “lysis” → breakdown —&— “(neo)genesis” → new formation]
high glucagon levels and low insulin levels
Glucagon: a peptide hormone released by the pancreas when glucose levels fall
→ promotes release of fatty acids and stimulates the conversion of these fatty acids into ketones (used as energy sources by muscles)
→ it coverts stored glycogen into glucose → mobilizes glucose
insulin: performs tasks that are opposite of glucagon, insulin stores glucose
Energy: Cellular Respiration → ATP
metabolic process of converting biomolecules (glucose, a-ketoacids, ketones) into energy (ATP)
requires oxygen (O2 ) and water (H2O)
produces ATP + CO2 + heat
> CAN YOU DO SOMETHING TO INCREASE THE EFFICIENCY OF MITHOCONDRIA?
→ YES, high intensity exercise!
why:
more oxygen (O2)
triggers mitochondrial genesis
Control of the Absorptive & Post-absorptive States
1. What controls uptake and breakdown of protein, glycogen, and triglycerides?
What controls the cells to use glucose during absorptive phase and fat during postabsorptive phase?
What stimulates glucose uptake by the liver during the absorptive phase, but glucogenesis and glucose release during the postabsorptive phase?
→ INSULIN & GLUCAGON
[Note: many other factors contribute]
[Remember:
» insulin → glucose uptake by cells
» glucagon → glucose release to the blood]
Homeostasis: Glucose in Blood
blood glucose optimal levels:
hypoglycemia [<0.04] → low blood sugar, excess insulin
excellent [0.05-0.06]
hyperglycemia [0.07] → high blood sugar, insufficient insulin
diabetes [>0.08] → no insulin production or insulin resistance
Insulin: storage
Insulin is a polypeptide hormone produced and secreted
(by \beta-cells)in the pancreas → lecture 2: hormones\beta-cellsin the pancreas detect glucose in the blood
→ when glucose is high: cells secrete insulin
→ low glucose: stop insulin production
Q: do you expect insulin during absorptive or post-absorptive state?
→ absorptive
insulin stimulates:
uptake of glucose by cells
conversion of glucose to glycogen and fat
conversion of amino acids to proteins
storage of glycogen, fat and proteins
Q: describe how insulin and glucose are related?
→ high glucose stimulates insulin secretion
→ low glucose: stops insulin production
→ insulin-sensitive cells respond to insulin binding by increasing the rate of glucose entry !!!
When glucose levels are low…
glucagon:
peptide hormone secreted by pancreatic
\alpha-cellsstimulates conversion of glycogen into glucose (to use for energy) → stimulates glucogenesis
promotes release of fatty acids and stimulates conversion into ketones → lipolysis
low glucose: stimulate release of glucagon
Glucose and insulin during the day [some questions]
❓a food, rich in starch and fibers?
→ carbs: potato, bread, fruits, vegetables…
❓a food, rich in sucrose?
→ sugar: fruits…
compare starch-rich vs sucrose-rich food:
❓difference in glucose blood level?
→ starch-rich: slower glucose increase (better sustained energy)
→ sucrose-rich: faster glucose spike (overshoot → sugar crush/dip)
❓difference in insulin blood level?
→ starch-rich: either high or low insulin increase
→ sucrose-rich: insulin overshoot and extreme dip
»»» why?
→ digestion speed
❓what is meant by “hyperglycaemia”?
→ high blood sugar, insufficient insulin
❓which food source (starch or sucrse) is more likely to be related to hyperglycaemia?
→ sucrose-rich
Low blood sugar: alert!
abnormally low glucose levels (hypoglycemia) is detected by chemosensory neurons in the CNS → CNS activates the sympathetic nervous system
result: adrenaline secretion → blood adrenalin levels rise
adrenaline → increases release of glucose and new assembly of glucose → increases glucose in blood
Factors Influencing Hunger
multiple and divers factors → obesity hard to treat
Body Mass Index [It’s Relative]
BMI = weight in kg / (length in cm)²
was designed for European men based on Scottish highland soldiers and French gendarmery
→ bias for women and non-European people
Obesity
problem treating obesity → lack of understanding of the aetiology and pathogenesis of this behavior
→ many reasons why someone can be obese, ranging from hormonal through genetic and behavioral
target neural systems are noradrenergic and serotonergic
!!! obesity as an addiction !!!
Obesity as an addiction
addiction → reduced dopamine
discrepancy between an enhanced expectation and reduced response to the food → might trigger drive to eat more to compensate
however, food addiction is not a withdrawal symptom from discontinuation of treatment drug
Obesity & stress
(chronic) stress is a risk factor
can both increase and reduce consumption
stress → seeking pleasure → eating high calorie foods
→ if this continues for too long, dopaminergic systems invoke compensatory downregulation
downregulation of dopamine may lead to anhedonia (inability to derive pleasure from life)
Obesity & Education in the NL
obese women have lower education levels than normal weight women and obese man
→ they earn less
obesity in women → less education
!!! correlation, NOT CAUSATION
On the Side: Ozempic - Semaglutide
not exam material!
ozempic:
mimics (because its an agonist) action of glucagon-like peptide (GLP1)
→ longer duration than produced GLP1
GLP1:
hormone released from the gut in response to food intake
stimulates insulin release (only when glucose levels are high) and reduces glucagon secretion → lowers blood glucose level
slows down gastric emptying and gut motility → improves absorptive state (less “spikes” in glucose levels)
suppresses appetite
beneficial for diabetes and reduces obesity (but has side effects!)
how to stimulate GLP1 release naturally:
fiber-rich foods, “lean” protein and non-saturated fat
regular exercise, good sleep and reduce stress
Anorexia nervous [AN]
BMI < 85% of expected BMI
adults (20+):
→ BMI < 18.5 = underweight
→ BMI < 16 = severe underweight
eating disorder
extreme fear of weight gain
distorted body image
excessive exercise
amenorrhea: absence of periods
starvation-dependent syndrome
eating less is initially perceived as rewarding
maintained through conditioning to the situations providing reward
different insula (disgust) and cingulate cortex (motivation)
self-loathing
overactive prefrontal cortex → increased inhibition
low serotonin and dopamine →SSRIs and Prozac helps
“AN has been conceptualized as a starvation-dependent syndrome that develops because eating less food is perceived as rewarding initially, and is then maintained through conditioning to the situations providing reward”
bulimia nervosa:
ingestion of food my reduce stress induced negative emotions → binging
they usually have depression
AN vs cachexia
anorexia → symptom of poor appetite whatever the cause
cachexia: progressive depletion of muscle and fat mass, reduced food intake, abnormal metabolism, reduced quality of life, increased physical impairement → seen in serious/lethal illnesses
AN: physiological consequences
fatigue, memory problems, mood
hair loss
dental decay → purging type
low BMI
low/high heart rate
low body temperature
loss of bone mass density (osteoporosis)
muscle weakness
dehydration
amenorrhea (no period)
gastrointestinal problems
Are these symptoms part of a biological dysregulation
symptoms of anorexia
symptoms of hormonal changes throughout development affecting metabolic rate and appetite
are these connected?
if so, can they explain symptoms in anorexia?
can they be treated?
Step Back…Metabolic Rate
metabolic rate = rate at which your body burns calories
1 calorie = the energy needed to increase the temperature of 1g of water by 1 degree
1000 calories = 1kcal or 1C
average need: women 2000 kcal, men 2500 kcal per day
of which 60-75% required for the basal metabolic rate (BMR)
Basal metabolic rate [BMR] → metabolic cost of living
BMR is the amount of energy used daily by animals at rest → includes breathing, blood circulation, maintaining body temperature, cell growth, brain and nerve function, and contraction of muscles
requires 60-75 % of total kcal intake
does NOT include activity (20%) or digesting food (10%)
estimated 1200-1500 kcal for women and 1500-1875 kcal for men → for doing absolutely nothing
Factors affecting metabolic rate
diet / starvation → slows down metabolic rate
age → decreases with age
gender → women lower
MORE height, weight and body surface the MORE energy needed
body temperature
physical activity
food intake → digestion requires energy
sleep → decreases during sleep
pregnancy, menstruation, lactation
emotional stress
hormone levels → adrenaline, thyroid hormone, and leptin
Hormones which affect metabolic rate and food intake [eating behavior & energy homeostasis]
HORMONE | SOURCE | METABOLIC RATE | FOOD INTAKE |
leptin | adipose (fat) cells | long term (+) | long term (-) |
thyroid hormone | thyroid gland | (+) | (+) |
adrenaline | adrenal medulla | short term (+) | short term (-) |
leptin: “the hormone of energy expenditure” a hormone predominantly made by adipose cells that helps to regulate energy balance by inhibiting hunger
AN & Hormones that Affect BMR and Food Intake
Leptin hormone in AN?
leptin (full!) = hunger suppressant hormone → anorexigenic
stimulates anorexigenic neurons & inhibits orexigenic (hunger) pathways
thought to reduce incentives of rewards
underweight AN patients:
more sensitive to leptin
levels recover when body weight recovers
Thyroid hormone & AN symptoms
Hypo-thyroidism | Hyper-thyroidism |
tiredness | hyperactivity |
sensitiveness to cold | anxiety, irritability, nervousness |
weight gain | insomnia |
depression | fatigue |
slow movements / thoughts | muscle weakness |
irregular or heavy periods | amenorrhea |
loss of libido | loss of libido |
reduced metabolic rate | increased metabolic rate |
slow heart rate (Bradycardia) | fast heart rate (Tachycardia) |
AN: regular functioning of thyroid hormone disturbed → hypothyroidism
because it down regulates metabolic rate → slowed heart rate…)
Adrenalin & AN symptoms
acute increase in adrenalin (prepare for action!):
increases heart rate
increases breathing rate
vasoconstriction (tight blood vessels → high blood pressure, conserves heat) and vasodilation (dilated blood vessels → low blood pressure, heat loss)
muscle contraction
stimulates release of energy from glycogen (liver) and fat
not immediately related to AN, however… ⇲
Adrenalin & thyroid hormone
adrenaline and thyroid hormone have an additive effect (1+1 → 2)
thus in conditions with low thyroid hormone, adrenaline cannot function properly
Summary
homeostasis: maintaining balance
eating and digestion
biomolecules: carbohydrates, lipids, proteins
absorptive state and storage
post-absorptive state and release
ATP as energy molecule
insulin and glucose storage
glucagon and glucose release
adrenaline ad glucose
hunger: more than lack of food
obesity: more than overeating
eating disorder and starvation
hormones involved in metabolic rate and appetite become dysregulated
can recover when body weight is restored
Additional Information from Book
Brain mechanisms for eating behavior
digestive system is connected to neural systems in the brain via the vagus nerve, therefore the focus of feeding behavior can be redirected towards the brain
brain is in control of eating behavior but it responds to the general environment of the body
the brain itself requires enormous amounts of energy in the form of glucose
> HYPOTHALAMUS
» lateral hypothalamus (LH)
hunger center
lesion → aphagia (stop eating)
aphagia followed adipsia (stop drinking)
LH is under inhibitory control of the VMH
» ventromedial hypothalamus (VMH)
satiety center
lesion → hyperphagia (overeating)
glucoreceptors (glucose receptors) → glucose is a simple sugar that gives energy to cells
→ high glucose: VMH inhibits LH
→ low glucose: VMH releases LH from control
SUM:
a complex network controls feeding, mediated by the hypothalamus in order to maintain homeostatic balance of energy supplies, and connected to the mesolimbic pathway that guides motivational behavior
Evolutionary explanations of eating disorders
obesity:
mismatch between evolutionary requirements of the past and modern-day resource excess
scarce food → high incentive value → reinforcing / rewarding
AN / BN:
reproductive suppression when conditions aren’t suitable
late sexual maturation → more time t focus on improving yourself (but men and postmenopausal women can also have these eating disorder)
escape famine
Psychological factors which influence eating
shape and color: same shaped pasta over and over again led to a decline in pleasantness
Drinking & thirst
extracellular fluid:
intravascular fluid: blood plasma
interstitial fluid: between the cells
cerebrospinal fluid (CSF)
there are movement / transaction between extracellular and intracellular fluids that allow cells to survive
extracellular fluid supports the cells and is controlled by the brain by promoting thirst
two types of thirst:
OSMOTIC THIRST
→ when solute concentration of extracellular fluid increases (it becomes more salty) and takes water from the intracellular cells which can damage the cells
→ osmoreceptors, located in the anterior hypothalamus, detect changes in he concentration of the interstitial fluid
HYOVOLAEIMIC THIRST
→ when the intravascular fluid decreases, a loss of blood volume is detected by baroreceptors (detects blood pressure) and receptors in kidneys
→ kidney secretes renin » production of angiotensin (increases drinking)
→ angiotensin » activates aldosterone (retains salt and water, also constricts blood vessels) and vasopressin (reduces fluid going to the bladder)
→ vasopressin conserves water, whereas aldosterone conserves salt
median preoptic nucleus (MPN) integrates hypovolaeimic and osmotic signals
L6 - PSYCHOPHARMACOLOGY
Depression Intro
Prevalence of depression globally
women > men
Q: is there a sex difference in depression / antidepressant use
→ YES
Dutch depression facts
one in 10 people report feeling depressed in the post four weeks
depression declines with older age
women about 1.5 - 2 times more likely
inverse / negative relation with income, work, and education level
ethnicity: Moroccan, Turkish, Surinam more
→ Dutch people with Turkish descendant receive more antidepressants
→ Antillean / Aruban descent receive less antidepressants
CONCLUSION:
→ “normative” group (old white educated men) are better off?
But: death by suicide is twice as prevalent in men than in women
one in ten people reported depression in the past year
→ 1.5 million people (NL population: 18 million)
about half of these people receive treatment
over 1.200.000 people use antidepressants
→ also used for other conditions such as anxiety disorders
in 2021: 4% (396.000) of men, 7% (667.000) of women use antidepressant
in the past years: increase in use of antidepressants in children and young adults
N06? = ATC classification
Anatomical Therapeutic Chemical (ATC)
N06 AA: NSRI* | Non-Selective Monoamine Reuptake Inhibitors |
N06 AB: SSRI | Serotonin Selective Reuptake Inhibitors |
N06 AF: MAOI | MonoAmine Oxidase Inhibitors |
N06 AX: Other | other antidepressants |
[*also known as SNRI’s = serotonin and norepinephrine uptake inhibitors, of which many are tricyclic antidepressants (TCA’s)]
Did you ever take…
Brand names: Acephen, Alagesic, Bupap, Butapap, Capacet, Doliprane, Endocet, Excedrin, Fioricet, Goody’s, Lortab, Mexalen, Midol, Norco, Ofirmev, Panadol, Pamprin, Percocet, Percogesic, Phrenilin, Premsyn , Primlev, Roxicet, Trezix, Tylenol, Ultracet, Vanquish, Vicodin, Zolben …
description: synthetic nonopiate derivative of p-aminophenol; produces analgesia and antipyretics
class: analgesics and antipyretics
ATC code: N02BE01
DDD: 3g O
DDD = defined daily dose
“O” stands for oral (taken orally)
active ingredient: acetaminophen
generic name: paracetamol
ATC classification system
active substances divided into groups according to the organ or system on which they act and their therapeutic, pharmacological and chemical properties
drugs are classified in groups at five different levels
Are antidepressants drugs? - definition of drugs
A) often an illegal substance that causes addiction, habituation, or a marked change in consciousness
B) a substance used as a medication or in the preparation of medication
C) formal definition according to the Food, Drug, and Cosmetic Act (FTC)
Psychopharmacology & psychopharmaca
pharmaceutical drug / medication / medicine = a substance used to treat, cure, prevent, or diagnose a disease or to promote well-being
psychopharmaca / psychoactive drug / psychopharmaceutical, psychotropic = a chemical substance that crosses the blood-brain barrier and acts primarily upon the central nervous system where it affects brain function, resulting in changes in perception, mood, consciousness, cognition, and behavior
psychopharmacology = the scientific study of the actions of drugs and their effects on mood, sensation, thinking, and behavior
Q: what about caffeine?
→ YES, psychoactive stimulant
Summary
depression prevalence
gender differences
diversity differences (SES, ethnicity, age)
antidepressant use
coming of medication names
(psycho)pharmaca and drugs definitions
Pharmacokinetics
it is about factors that influence a drug as it travels → what body does to the drug
what the body does to the drug can be summarized as ADME
Absorption / Administration
Distribution
Metabolism*
Elimination / Excertion
*something is either added to it or it’s changed in some way
Routes of administration
process by which the drug enters the bloodstream (absorption), either via:
passing through cell membranes
or by direct administration to the bloodstream
[Note: concentration of drug measured in blood is reference level]
> PARENTERAL ADMINISTRATION
bypasses the gastrointestinal tract (GI)
injections
epidermis → dermis → subcutaneous tissue → subcutaneous adipose tissue → muscle and vein
(slide ones are also underlined):
epidural: nerve block to relieve pain
intradermal (ID): into the skin, usually for diagnostic tests (don’t confuse with TRANSdermal)
subcutaneous (SC): just below the skin
intravenous (IV): directly to the bloodstream
intramuscular (IM): through the muscle, slower than IV
intraperitoneal (IP): predominantly used in animals, through the abdominal wall
intrathecal (IT): to the arachnoid space of the spinal canals that it reaches csc → spinal anesthesia (nerve block)
intracerebroventricular (ICV): to ventricles of the brain, done to animals
> ENTERAL ADMINISTRATION
via gastrointestinal tract (GI)
(slide ones are underlined):
oral (PO): have to be lipid soluble, absorbed across intestinal mucosa via passive diffusion
rectal (PR): reserved for people who are vomiting, unconscious, or have difficulty swallowing (e.g. suppository → fitil)
> OTHER ROUTES OF ADMINSTRATION
inhaled: fast, large surface area where the drug can enter the bloodstream and capillaries of the lung carry the drug directly to the heart → faster the route more addictive (smoking)
transdermal: via skin (patches) → nicotine replacement theory (NRT), hormone replacement therapy (HRT)
transmucosal: across mucous membranes → intranasal, sublingual / buccal (under the lounge e.g. nitroglycerine for chest pain)
Distribution of drugs
> DISTRIBUTION IN THE BODY
need to be taken up via cells lining the stomach or intestines for oral drugs
mostly active transport
all blood vessels lining stomach and intestines first go to the liver (except for oral and rectum)
liver can transform drugs
thus a smaller amount than ingested is measurable in the blood
blood transports drugs to target organs / cells
needs active transport from blood to target cells (unless lipophilic / lipid soluble)
Q: what does the portal vein do?
→ instead of sending that blood straight to your heart, it first goes through the portal vein → liver.
> DISTRIBUTION IN THE BRAIN
two arteries supply oxygenated blood to the brain:
internal carotid artery
vertebral artery
HOWEVER, the drug still has to overcome some obstacles → body membranes:
cell membrane: lipid-soluble (lipophilic) drugs readily pass but many drugs aren’t, the drugs ability to pass is also determined by the environmental acidity and the drug’s acidity (pH → 7 neutral)
the small blood vessel (capillaries): capillary walls are thin and single layered, small holes that allow small molecule to be exchanged
blood-brain barrier: composed of high-density glial-cells restricting passage of substances from the bloodstream much more than endothelial cells in capillaries in the body
placental barrier:connectable mother and the foetus and is a point of exchange of nutrients and drugs consumed by the mother
> DISTRIBUTION: WHERE IS THE DRUG?
transfer of a drug from one location to another within the body
measurement of a drug is usually in blood plasma
but drugs can be distributed among other bodily fluids → intracellular did (ICF), interstitial fluid (IF)…
Q: can drugs distribute non-fluid compartments as well?
→ YES, skin, organs, bone, fat …
> DISTRIBUTION: BODY FLUIDS
intracellular fluid (cytoplasm)
extracellular fluid:
→ interstitial
→ intramuscular / blood plasma
→ cerebrospinal
> DISTRIBUTION: BODY COMPARTMENTS
metabolic tissue → muscle, connective tissue, brain, nervous system cells
body fluids (intracellular water and extracellular water)
bone tissue
fat
> BODY FAT MASS: SEX DIFFERENCES
sex differences in body fat mass (women consist of more solids than fluids when compared to men) matter considering the dosage of the medication
Metabolism & excertion
> METABOLATION: THANK YOUR LIVER (and to a lesser extent kidney, lung, brain, intestine, skin and more)
most common excretion is via kidney and intestines but liver is the one metabolizes
circulating blood with drugs, keeps “losing” drugs via the liver, kidneys and uptake by tissues
metabolism involves enzymes in the liver changing the drug to increase solubility
→ sometimes leads to harmful substances: paracetamol
liver metabolizes (both active or inactive) drugs so that they become water-soluble, and therefore can be excreted via kidney (urine) or via liver-excreted bile to the intestines (feces)
liver does this in two biotransformation phases (hepatic metabolism)
→ phase 1, oxidation: oxygen is incorporated in to the drug
→ phase 2, conjugation: combining the drug with a small molecule
> EXCRETION / ELIMINATION
kidney - urine
liver - bile and feces
skin - perspiration (sweat)
lungs - respiration
glands - tears, saliva, sweat, milk
hair
nails
Q: name an example of a drug which can be detected in respiration and hair respectively?
→ alcohol and cocaine
Measuring drugs in the body
usually blood plasma without red blood cells, but other ways to detect substances are e.g. CSF, saliva, urine, breath
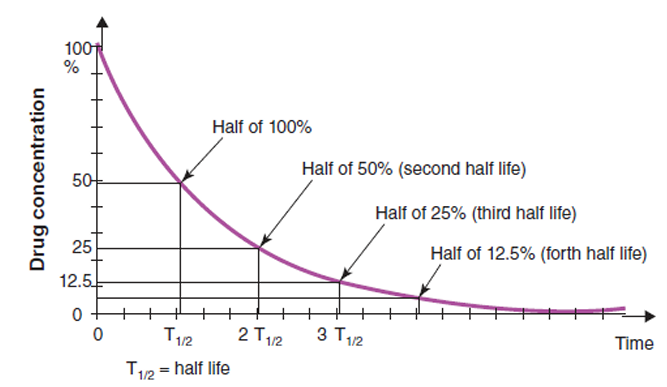
T1/2 or half-life of a drug in the body: time required for the drug concentration to fall by 50%
Q: what route of administration was most likely used here?
→ intramuscular (IV), because the drug concentration starts immediately at its peak (100%) — meaning it entered the bloodstream instantly
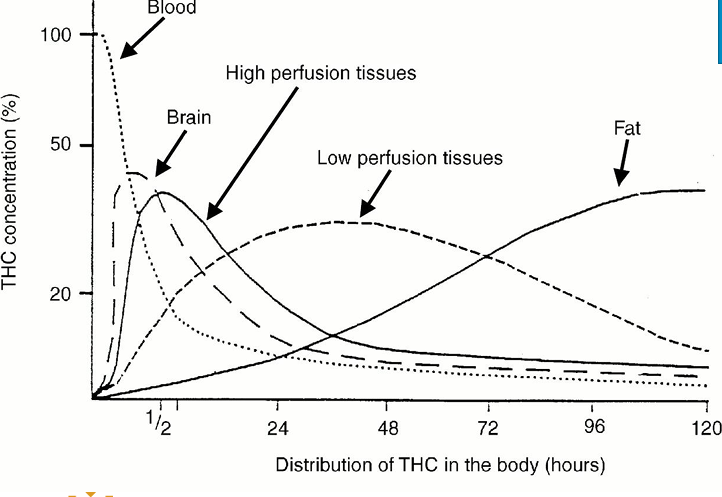
(Complex) Example: distribution of the [cannabinoid] in the body
Summary
Pharmacokinetics = What the body does to the drug Can be summarized as ADME
• Absorption / Administration
• Distribution
• Metabolism
• Elimination / Excretion
Pharmacodynamics
what drugs does to the body, what happens when it reaches its destination
→ involves ability of a drug act upon cells or cellular components
Pharmacodynamic examples - modulation of neurotransmission by drugs
drugs can influence neurotransmission at a number of different points that can ultimately influence behavior
> PRECURSOR PRELOADING DRUGS
enhances synthesis and increases the turnover of a neurotransmitter by acting as a precursor in the neurotransmitter's synthesis
Parkinson’s disease therapy → provide patients with precursor to dopamine: L - DOPA
> SYNTHESIS INHIBITION
drugs can prevent neurotransmitters from being made
treating depression with metyrapone: a cortisol synthesis inhibitor → blocks the recall of emotional memories in healthy participants
> STORAGE PREVENTION
drugs can prevent the neurotransmitter from being stored in the vesicles
reserpine makes monoamine vesicles “leaky”
> ENHANCE NEUROTRANSMITTER RELEASE
drugs can promote neurotransmitter release from synaptic terminals
amphetamine mimics DA and enters the synaptic terminals via the dopamine transporter (DAT → uptake receptor!), therefore it has two effects:
→ 1. competes with DA for reuptake, thus less DA can be removed from the synapse
→ 2. this causes extra release of DA that is independent from action potentials ( this release of DA is via reversing the uptake processes)
amphetamine induces symptoms similar to those seen in paranoid schizophrenia
> POSTSYNAPTIC RECEPTOR STIMULATION
drugs can mimic the endogenous neurotransmitters, e.g. nicotine as acetylcholine (ACh)
> POSTSYNAPTIC ANTAGONISM
drugs can block the postsynaptic receptors by binding to them, therefore preventing the endogenous neurotransmitters to bind to them
antipsychotic haloperidol blocks DA D2 receptors and stops DA from binding to those receptors
> AUTO-RECEPTOR STIMULATION & ANTAGONISM
autoreceptor: receptors at the synaptic neuron that gives feedback
drugs can act at the autoreceptors to provide false feedback on synaptic activity
dopamine receptor agonist apomorphine:
→ at already low doses stimulates the DA autoreceptor to reduce the release of DA
→ at high doses stimulates DA photoreceptor to increase the release of DA
= selective stimulation, happens because dopaminergic autoreceptors are 10 times more sensitive than postsynaptic receptors therefore at low doses provides a negative feedback
conversely, DA antagonist haloperidol increases DA at already low doses → appears counterintuitive since it’s used to treat schizophrenia
> DRUGS THAT BLOCK REUPTAKE
drugs can prevent the neurotransmitter being removed from the synapse (blocking metabolic escape route)
cocaine and methylphendiate (Ritalin) block the DA transporter
SSRI’s like prozac block 5-HT transporters
> INHIBITION OF METABOLISM / BREAKDOWN OF A SUBSTANCE
prevents the neurotransmitter from being metabolized
MAOI: increases the monoamines by inhibiting the enzymes that degrade them.
donezpil for Alzheimer’s blocks the metabolism of ACh
Substances need to bind…
in order to have a certain effect
same for psychopharmaca
psychopharmaca act on the same sites as the bodies own substance
usually have a stronger effect, or rather, block the effect of a bodies own substances
a number of terms are associated with these binding properties that affect the outcome of a treatment
Drugs acting upon a receptor
where does it bind to the receptor?
what is the effect on the receptor?
how does it affect the usual functioning of the receptor?
what happens in the long run?
→ number of receptors can be downregulated or upregulated
ligand: anything that binds to a receptor
the shape and distribution of a binding protein determine which ligands it will bind
the amino acid sequence of a protein determines both shape and the distribution of charge
shape and charge work together in matching up ligands with their receptors
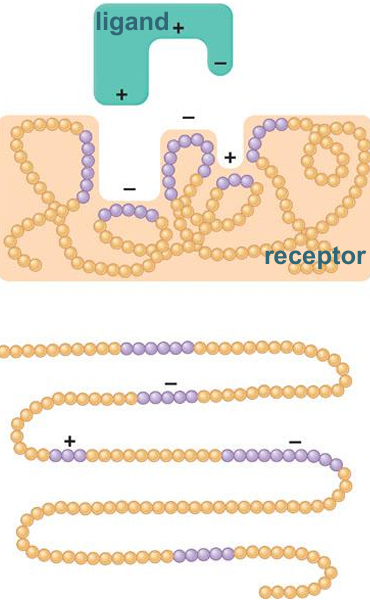
Specificity: only cell… has the matching receptors for a specific chemical messenger, so it is the only one that responds
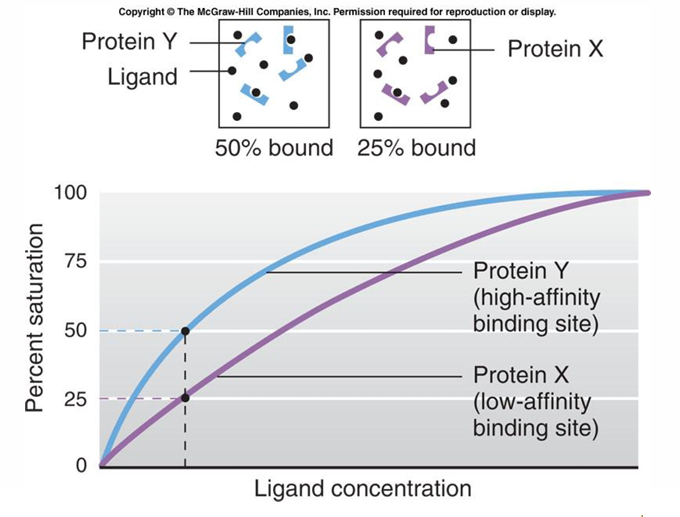
Affinity (Kd): how well the ligand fits in a binding cite (high affinity binding site: best fit for the ligand and low… vice versa)
Bmax (binding maximum): maximum amount of binding sites available for a ligand
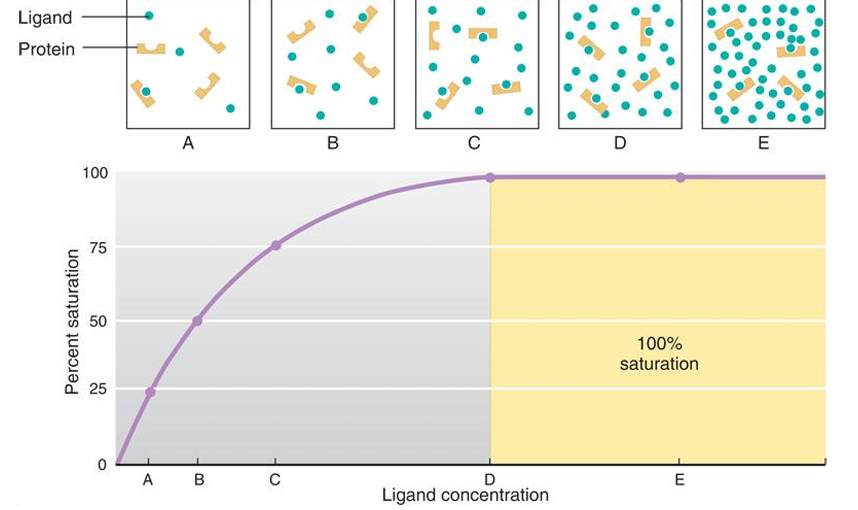
affinity (Kd) of a drug can be measured as the percentage amount of drug that binds to the receptor (Bmax) according to a concentration (steeper the curve the higher the affinity)
strong binding needs less concentration and vice versa
saturation: occurs when ligands become so abundant that every binding site is occupied (B)
when two proteins can bind the same ligand, saturation occurs more readily for the protein that has a higher affinity for the ligand (A)
Drug-Ligand competition
non-competitive drugs (allosteric): binds to a different site rather that the active site
competitive drugs (orthosterically): binds to the same active site as a natural ligand
Evaluation of the drug effect
to evaluate the effect of a drug, psychopharmacologists will administer different doses and a dose-response curve will be generated which describes the biological or behavioral effect of the drug
dose-response curves permit the identification of the following:
potency: amount of drug needed to get the effect (compare ED50)
efficacy: maximum effect (ED100)
ED50: dose that produce half the maximum effect (Effective Dose - effective in half of the population)
TD50: dose that is toxic in 50%
LD50: dose that is lethal in 50%
Biology: antagonist vs agonist
drugs can be divided into four groups depending on what they do at the synapse:
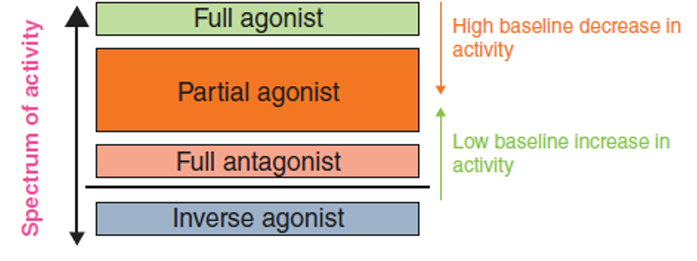
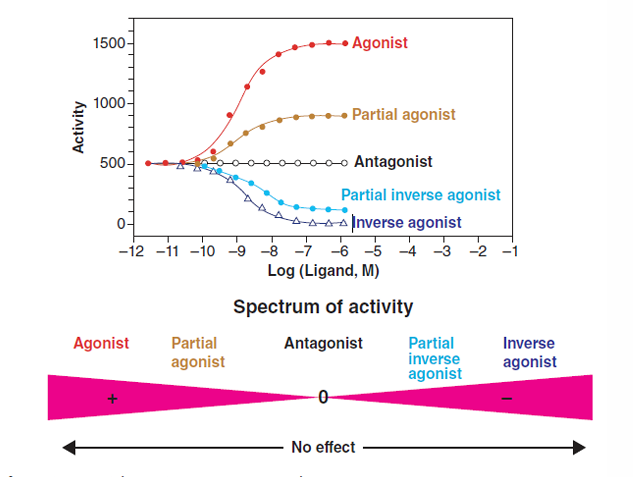
agonists (full efficacy → lights on): produces a response as an endogenous neurotransmitter at maximum capacity
many effects “downstream” in the cell = cellular cascade = stepwise processes → chain of reactions
some examples of effects:
→ release of hormone
→ DNA transcription and creation of protein
→ opening or closing of an ion channel
→ activating or inhibiting an enzyme
→ many possibilities
partial agonist (dimmed lights): somewhere between an agonist and and an antagonist, binds to the receptor and prevents other ligands to bind, but it only has reduced efficacy → effects are different depending on the endogenous neurotransmitter's behavior (causes agonist at low doses when there is no full agonist but antagonism when a full agonist is present)
antagonist (zero efficacy → lights off): inhibits activity, doesn’t make a physiological change but just stops the receptor from being activated. It can do this by either binding to the same site as the agonist (orthosterically) or by binding to a separate site and changing the conformation of the receptor (allosterically)
beta-blocker is drug that acts as an antagonist on the beta-adrenergic receptor
thus preventing (nor)adrenaline to bind to the beta-adrenergic receptors
causing the heart to bat slower and with less force, and lowering blood pressure
inverse agonist: response that is in the opposite direction to that of an agonist (don’t confuse it with antagonist, antagonists inhibit a response) → if agonist has a positive effect, an antagonist will have no effect, but an inverse agonist will have a zero effect
Summary
pharmacodynamics
ligand and receptor binding
affinity; specificity; drug-ligand competition
agonist - antagonist
partial - agonist
Antidepressants: An Introduction on SSRI and MAOI
Psychiatric medications
antidepressants: used to treat disparate disorders such as depression , dysthymia (persistent depressive disorder), anxiety, eating disorders, and BPD
stimulants: treat disorders such as ADHD and narcolepsy and to suppress appetite
antipsychotics: which are used to treat psychosis, schizophrenia and mania
mood stabilizers: to treat bipolar and schizoaffective disorders
anxiolytics: to treat anxiety disorders
relaxants: used as hypnotics, sedatives, and anesthetics
Serotonin pathway
trypthophan (amino acid)
⬇ENZYME 1
5-Hydroxy-L-tryptophan (5-HTP)
⬇️ENZYME 2
serotonin (5-HT)
⬇️ENZYME 3 → MAO Monoamine Oxidase: an enzyme which inactivates serotonin
5 - HIAA (no longer serotonin)
Q: where does tryptophan come from?
→ diet
Monoamine-oxidase (MAO)
monoamine-oxidase = an enzyme that breaks down monoamines
a drug called Monoamine-Oxidase INHIBITOR (MAOI) blocks this step…resulting in less breakdown of monoamines (e.g. serotonin)
MAOIs
inhibit breakdown of monoamines such as serotonin, but also (nor)epinephrine, and dopamine
used to be irreversible - takes a few weeks to wear off
nowadays reversible
not first OR second choice of treatment
Serotonin pathway in the cell
5 - HT = serotonin
SERT = serotonin transporter → reuptake of serotonin!
Reuptake transporters: reuptake of monoamines
serotonin transporter: SERT
norepinephrine transporter: NET
dopamine transporter: DAT
Drug class: selective serotonin uptake inhibitor (SSRI)
inhibit the reuptake of serotonin from the synaptic cleft
selectively serotonin
presynaptic transporters
acts as antagonists for the reuptake transporters
immediate effect: less reuptake, more serotonin in synaptic cleft
antidepressants take long to work
Reuptake inhibitors
SSRI’s
TCA’s (non-selective reuptake inhibitors set and NET)
SNRI’s (selective serotonin-norephinephrine reuptake inhibitor)
Summary
one in 10
over 1 million antidepressant users
mostly SSRI’s
monoamine oxidase inhibitors
reuptake inhibitors
Additional Info From the Book
off-label prescribing: when drugs are used for purposes for which they were not originally intended → can be useful for understanding the pathways
Drug classification
A to C: most harmful to least
1 - 4: no therapeutic value to therapeutic value
sequence number: | Lilly 110140 (LY110140) |
chemical name: | 3-(p-trifluoromethylphenoxy)-N-methyl-3-phenylpropylamine |
generic name: | Fluoxetine |
brand name: | Prozac |
Disulfiram
to treat alcoholism by main it unbearable
Nerve agents and bioterrorism
sarin: prevents metabolization of ACh → excess ACh
Clinical trials
divided into four phases:
small number of paid volunteers
small number of the target pop. → efficacy in target pop.
random assignment, large n → important for licensing the drug
after the product is in the market
L7 - EMOTIONS
Learning Goals
being able to understand what emotions are
being able to distinguish emotions from other affective phenomena
understand what the main characteristics of emotions and their functions are
insight into five major theoretical approaches of emotional the specific role of the physiology of emotions
understand the links between emotions and psychopathology
What is Emotion?
❌emotional is nonrational ❌
❌it is better to not have negative emotions ❌
❌shame is not an emotion ❌
→ it is an self-conscious emotion
emotional responses have at least three components:
subjective (the feeling)
behavioral (e.g. facial expression)
physiological (heart rate)
❗any emotion can be adaptive or maladaptive depending on contextual factors and the employed emotion regulation strategies ❗
facial feedback theory: smiling → happy
Functions of emotions
Affective phenomena
feelings are involved but these are NOT emotions:
preferences
attitudes
moods: no clear stimulus/reason, lasts longer (emotions → clear reason and lasts short)
affects predispositions: tendency to act in a certain way (grumpy)
interpersonal stances: shyness, friendliness, anxiety
emotions:
aesthetic emotions → no evolutionary benefit / unclear why we show it (looking at art)
utilitarian emotions: evolutionary/survival benefits
Characteristics of emotions
reaction to a stimulus
appraisal: assessment of the situation (importance)
experiental and expression component: may or may not show when angry
limited duration of a state
motivates us to display certain specific behaviors: tendency to show certain behaviors
capacity to regulate emotions: we are not defenseless victims of our emotions
effect on self and others: seeing someone’s emotional section gives us information about them
Evolution
Reacting to our emotions
man causes a car accident and then threatens the other driver and tries to flee - not adaptive, body reacts to emotions
Instinctive behavior (NOT emotion)
pulling your hand away from a candle:
reflex - instinctive behavior, not an emotion
people who don’t experience pain live less because they don’t retract their hands from the flames - adaptive
taxis: moths are attracted to light:
survival value
instinctive emotion (not an emotion!)
fixed action pattern: when eggs fall out of the nests swans pulls them back with their beaks, and she continues doing that movement even if you remove the egg
imprinting: baby ducks immediately start following their mother
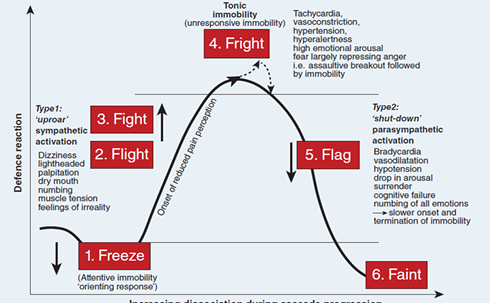
How to cope with external threats?
our central and peripheral nervous system and our immune system have these functions:
perception → five senses
evaluation → brain / memory !!!
action → muscles, autonomic nervous system , endocrine system, immune system
[NOTE: the functioning of the immune system is influenced by the central and peripheral nervous system!]
Benefits of emotions
we have infinite possible situation - if we fail to recognize a threat, we might choose to react in an incorrect way - infinite possible reactions
⬇️
optimal tuning: picking the best fitting reactions by using our emotions as a guide
behavioral immunity: we get disgusted from rotten food
Five Theoretical Approaches
Evolutionary Emotion Theories (Darwin / Ekman)
→ emotions are universal and have adaptive value
James-Lange Theory / Canon-Bard Theory / Schachter’s Cognitive Labelling Theory
→ emotions are essentially the perception of bodily responses to stimuli
Cognitive Emotion Model (Arnold / Lazarus)
→ emotions are based on appraisals (cognitive point of view)
Emotions & Our Brain (Ledoux / Damasio / Roll)
→ brain and emotions - the link between emotion and cognition
New Approaches (Barrett)
Evolutionary Emotion Theories (Darwin / Ekman)
Darwin
emotional expression evolved in order to signal what behavior an animal might engage in
expression of emotions serves as an effective means of communication about intention and possible behavior
also provides additional information to verbal communication (supported by the six primary emotions)
being unable to recognize facial expressions, and therefore understand other people, → leads to difficulties in prosocial behavior (autism and alcoholism)
Paul Ekman
default face: everyone has different resting faces
he measured facial expressions to identify emotions
> BASIC EMOTIONS
6/8 primary (innate) emotions: happiness, sadness, fear, disgust, anger, surprise (contempt and embarrassment / shame)
these primary emotions can make up the core of other more subtle emotions
located in a specific, innately determined neural substrate
a characteristic facial expression or neuro-muscular expressive pattern
a distinct subjective or phenomenological quality → we know the difference between being anxious or sad
independent of language and culture → universal
also displayed by blind and deaf children
> UPDATE
expansion of his theory to a neuro-cultural theory of emotion
the neuro-part: keeping the original idea that each (basic) emotion is associated with a fixed facial expression and peripheral physiological reaction pattern
the cultural addition: acknowledged that culture might impose rules and guidelines as to when and how an emotion is expressed → display rules
> SELF-CONSCIOUS EMOTIONS
shame, guilt, regret, pride…
occur at a later stage in development
more doubt about the universal character; greater influence of culture
occur first when an organism has the capacity to recognize itself in the mirror
James-Lange Theory / Canon-Bard Theory / Schachter’s cognitive Labelling Theory
James-Lange theory
emotion is the result of your physiological response, not the cause of it.
“We don’t cry because we’re sad — we’re sad because we cry.” 😭➡😢
emotionally salient stimulus is perceived (bear)
this leads to a set of physiological responses (increased heart rate)
⭐ there are different / specific physiological responses for every different emotion⭐
that then determines the emotion experienced (fear)
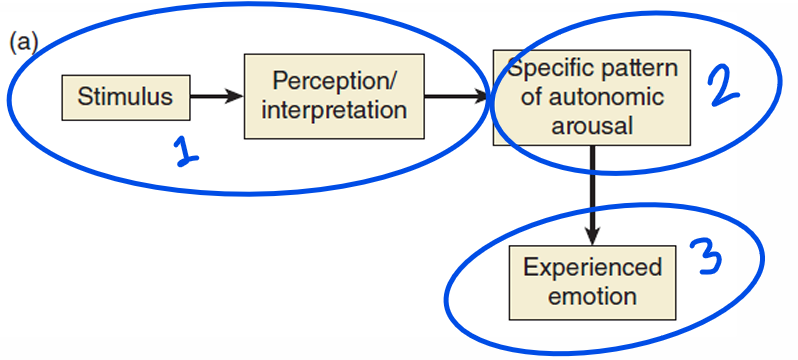
→ eat bad food - stomach upset - feel disgust
Canon-Bard theory
emotionally salient stimulus is perceived by THALAMUS → site of sensory integration
both physiological reaction and an emotional reaction occur instantly and SIMULTANEOUSLY
⭐evolutionary advantage - faster response⭐
⭐physiological responses have NO INFLUENCE on the emotion being expressed (unlike James-Lange)⭐
physiological change can ADJUST THE INTENSITY of emotion felt (but not the affect)
criticized James-Lange because:
interruption of physiological feedback (e.g. spinal injury) does not prevent emotions being expressed
different emotions can have the same physiological reactions
this theory is too slow, dos not make evolutionary sense
artificial induction of physiological changes does not produce emotions
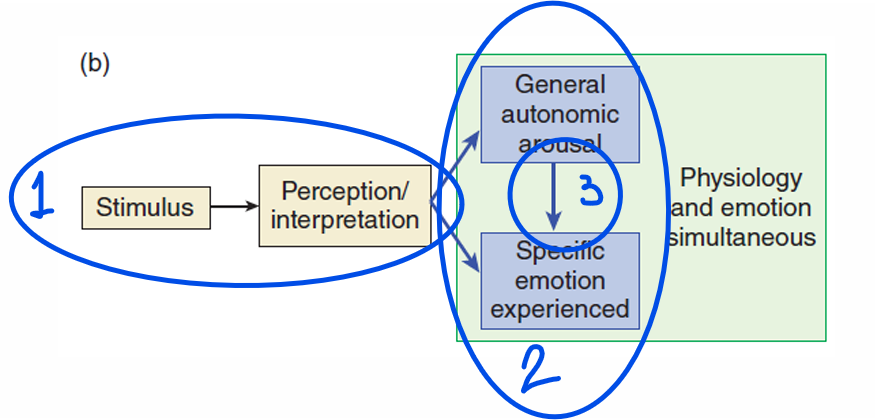
Schacter’s cognitive labelling theory
stimulus is perceived
stimulus causes a physiological reaction + COGNITIVE INTERPRETATION of CONTEXT determines the emotion felt ⭐increased heart rate because of spider → fear / increased heart rate before a date → excitation⭐
feedback is sent to use in the future
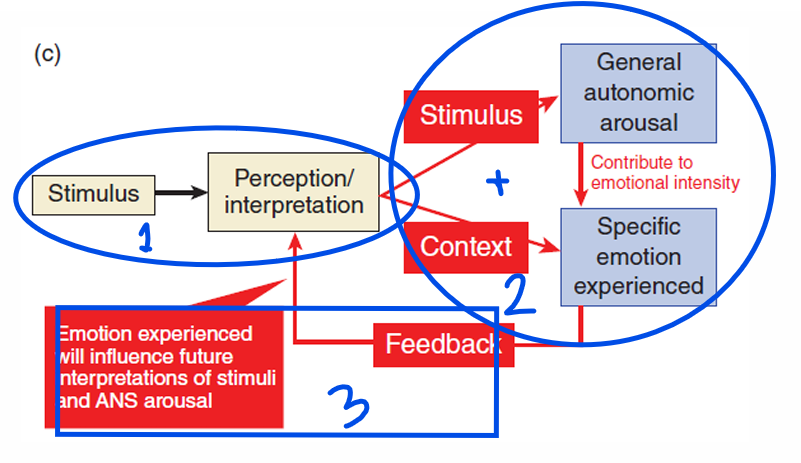
> EXPERIMENT: ARTIFICAL PHYSIOLOGICAL AROUSAL
groups who were informed about the drug → attributed their reactions to treatment
those who were NOT informed → attributed their reactions to the collaborator who acted like an asshole
placebo conditions → intensity of emotion was related to physiological reaction
! emotion experienced is a product of the interpretation of the environment
! there is a cognitive attribution of emotion in which the context is critical and physiological arousal increased the intensity of the emotion experienced
> EXPERIMENT: BRIDGE
arousal from the bridge were misattributed to the female
> EXPERIMENT: WHETHER THE LABELLING OF EMOTIONAL STIMULI WOULD BE AFFECTED BY BIOFEEDBACK?
participants viewed naked women whilst hearing their own heart beat. However, the experiment manipulated heart rates to provide false feedback
false feedback (increased heart rate): rated the females as more attractive
false arousal can also be attributed
Cognitive Emotion Model (Arnold / Lazarus)
appraisal: evaluation, how some one interprets the situation
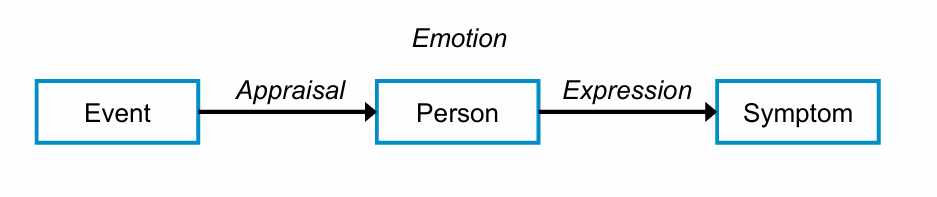
basis of cognitive therapies - you can’t change the event but you can change how the person how a person thinks about the situation
Emotions & Our Brain (Ledoux / Damasio / Roll)
Ledoux
> PAPEZ NEURAL CIRCUIT
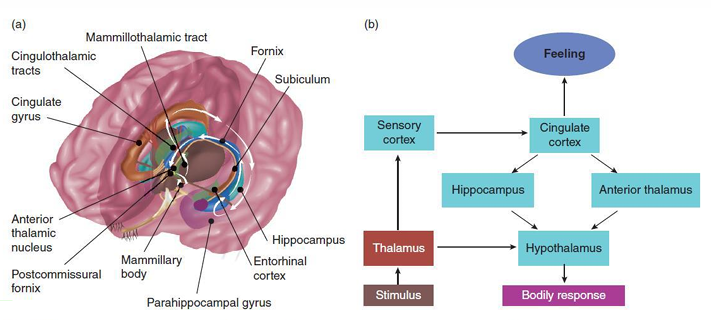
two routes of information flow:
cortical circuit: represents the thinking or perception of the emotion
thalamic circuit: feeling
Klüver-Bucy syndrome: medial temporal lobe lesion (Papez circuit) → monkeys showed hypersexuality, coprophagia, unresponsive to humans
visceral brain (striatal regions and basal ganglia): enhances primitive emotions → limbic system = emotional brain
> AMYGDALA
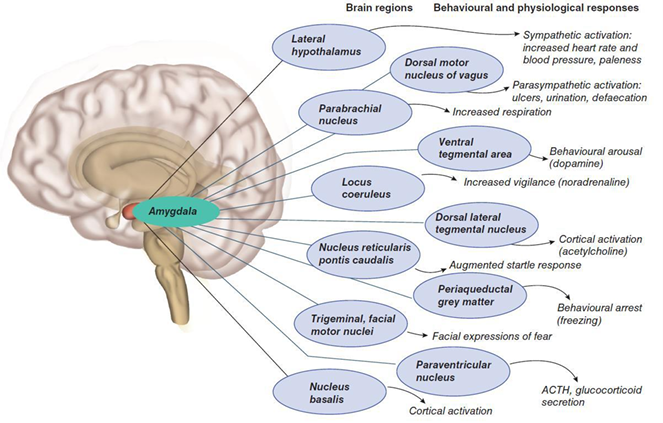
unconscious emotional responses
integrates cortical and subcortical info
also involved in the preparation of the fight / flight mode
two pathways:
unconscious subcortical pathway - directly activate body systems based on sensory info from thalamus
conscious cortical pathway - slower - thalamus to cortex to amygdala
> HIPPOCAMPUS
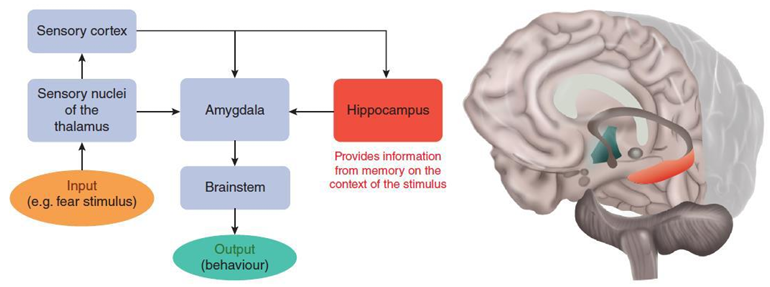
hippocampus is responsible for the conditioning of contextual fear
lesions prevent conditioning
learning principle that something evokes fear
info from memory of the stimulus
Damasio: somatic marker hypothesis
! physiological responses directly affect areas of the brain involved in decision-making !
decision making: not an entirely cognitive process, emotions play a role too
distinguishes between emotions and feeling of emotions:
feelings: should only be used for subjective experiences of emotions → introspective
emotion: should refer to all the processes involved such as physiological state → measurable
→ thus, emotional decision making is influenced by peripheral feedback from the body (re-emergence of James-Lange theory)
Roll’s emotional model
emotion as a product of reinforcement / punishment
different emotions will arise from different primary reinforces (effects of sex is different from the effects of food)
environmental conditions can determine the emotion experienced (losing → anger if allowed, sadness, if anger is not allowed)
orbitofrontal cortex, amygdala, and cingulate cortex
orbitofrontal cortex: permits flexibility of emotional behavior and is sensitive to changes in reinforcement
cingulate cortex: receives input about reward expectations from the orbitofrontal cortex and amygdala
amygdala: less prioritized
New Approaches - Conceptual Act Model of Emotion (Barrett)
evolution produced multipurpose set of mechanisms that work together to produce a variety of emotional responses that are tailored to each situation
moves away from the Darwinian evolutionary account of specific emotions…
… to a view that says emotions as defined by words such as “anger” correspond to mental events emerging from the interaction of basic psychological constructs
emotions are mental events constructed, instantaneously, from psychological processes producing variations in “core effect”
core effect: feeling of positive or negative affective states (pleasant / unpleasant)
→ mental representations of bodily sensations that inform the organism that something in the environment is important
primitive psychological processes are not specific to emotion but are rather general processes for mental life
non-emotional factors such as concepts and languages have an important role in determining emotion
categorizing emotions provides meaning
adaptive because understanding how other people see the world gives rise to our understanding of their intentions
emotions are not discrete but are collection of concepts for the emotion that can be combined in a number of diverse and flexible ways (different types of anger)
Short version it is 👇
Your brain doesn’t receive emotions — it creates them. It’s constantly regulating your body and summarizing all that information into basic feelings like calm or tense. Then, using your past experiences, it predicts what those feelings mean and constructs an emotion — fear, anger, joy, etc. Since emotions are built from predictions, not just reactions, changing your present experiences can literally reshape how you feel in the future.
⭐Barrett therefore sees emotion as the physiological changes brought about by stimuli along a dimension of pleasantness that are subsequently conceptualized as specific categorical emotions⭐
> HER CRITICISM ON THE EVOLUTIONARY EKMAN
not all instances of an emotion referred to by the same (e.g. anger) look alike, feel alike, or have the same neurophysiological signature (angry at the world and angry at your partner can be experienced differently)
cross-cultural variation in the recognition of emotional expression is greater than Ekman asserts (doubt about universality)
how an emotion is experienced differs from culture to culture, even from person to person (sadness for some is fatigue for another)
the “typical” posed emotional expressions are rather symbols than real expressions (real life has more variation)
→ fear can be experienced differently (inconsistent with Ekman)
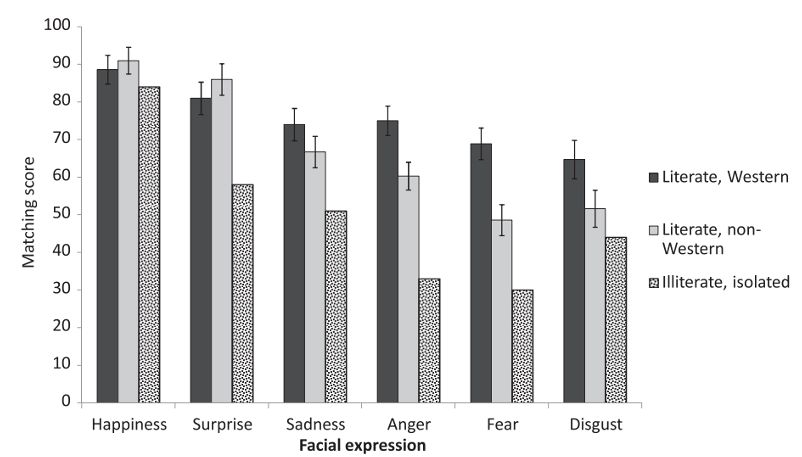
→ Ekman was too optimistic some emotions aren’t well recognized as he thought it was in non-western cultures
Emotions & Psychopathology
one single emotion can become very prominent, e.g. fear or sadness
anxiety disorders
one reacts to events with deviant emotional responses
agression
emotions are not properly regulated - emotions are more intense, last longer or interfere strongly with daily activities
antisocial p.d., bipolar, borderline
deviant behavior is used to regulate emotions
OCD
a more general incapacity to experience (and express) emotions
depersonalization-derealization disorder
incapacity to experience certain very specific emotions (e.g., empathy, love, guilt, remorse)
emotions of others are not recognized
autism
Summary
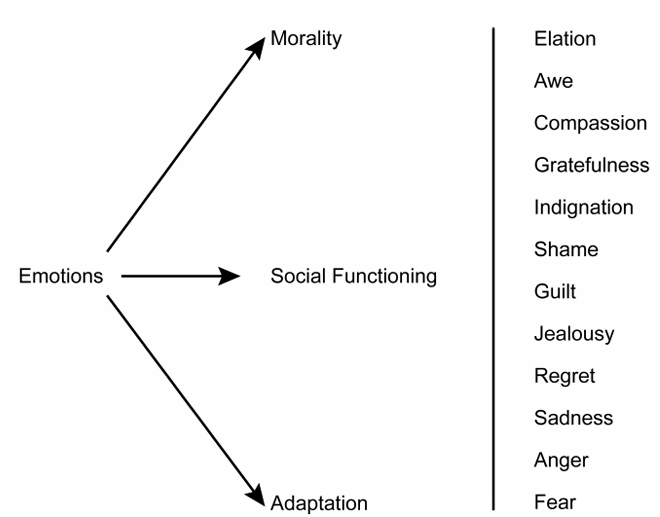
emotions have evolved to solve important adaptational problems (survival / reproduction, social, and moral functioning)
a distinction is made between basic emotions and self-conscious emotions
emotions can be defined based on some specific criteria
there are different theoretical approaches
there is currently much discussion about emotions
Additional Information from the Book
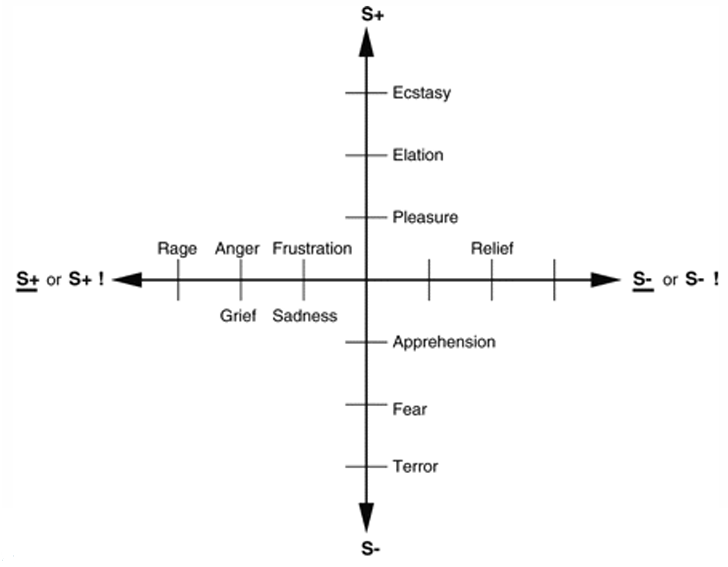
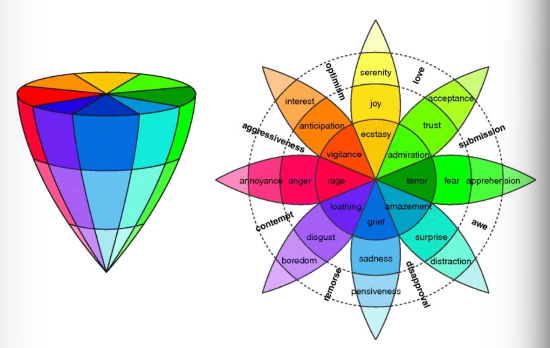
Emotions as dimensions
The view of emotions as a dimension stems from early work by Wundt, who suggested that emotional experience could be described along an effective continuum (e.g. pleasantness/unpleasantness, subdued/excited and relaxation/strain)
In a similar manner, Russell's circumplex model of affect viewed emotion on dimensions of pleasant/unpleasant and aroused/not aroused

Plutchik provides a similar account but this view is one of emotions being on a continuum with extremes at either end
→ eight basic emotions that represent opposite-paired dimensions (e.g. joy being the opposite of sadness)
Physiology of facial expressions
there are two types of facial muscles:
deep facial muscles: attach to bone to enable large movements like chewing
superficial facial muscles: attach only to skin and provide emotional expressions
muscles of the face are innervated by two cranial nerves:
facial nerve: innervates the superficial muscles
trigeminal nerve: innervates the deep facial muscles such as the temporalis
Emotion: what’s love got to do with it?
when looking at their loved ones:
increased activity in the anterior cingulate cortex and the striatum
reduction of activity in amygdala
→ amygdala is associated with negative emotions
activation of brain reward mechanisms like ventral tegmental area and the nucleus accumbens
cortisol levels rise → oxytocin and vasopressin are released
testosterone in males decrease and increase in females → reduce polarity of sexes
endorphins and enkephalins are also involved in the love response, as is dopamine
> LOVE IS THE DRUG
similarities between addiction and love:
people in love feel protective of the one they love and will do anything for them. Addicts will do anything to get a drug
motivation is centered around that person at the expense of other responsibilities
obsessive thoughts concerning the loved one are common
the lover becomes salient in everyday occurrences
stimuli that one ordinarily would not attend to suddenly make one think of the loved one (e.g. a scent). Stimuli associated with the drug are powerful mediators of the addiction process
when one love is in love, the pleasure parts of the brain are activated → dopamine are seen within the mesolimbic system
the longer a couple are together, the more their brains become tolerant to the hormones being released, which causes the euphoric feeling not to be felt as strongly
breaking up with a loved one can lead to a withdrawal phase characterized by depression, anxiety, and possibly suicide
love and hate, common areas: putamen and insula
Neural mechanisms of aggression
amygdala and hypothalamus influence defence behaviors and attack behaviors
amygdala was activated in the brains of convicted murderers whose crime was impulsive and premediated, whereas those who were guilty of premediated murder exhibited greater prefrontal activity
research suggests that the job of the prefrontal cortex is inhibiting the amygdala’s response
Emotion and music: evolutionary adaptation
music activates large neural networks related to attention, semantic processing, memory, motor functions and emotional processing
⭐ somatosensory pathways that mediate the visceral feelings of the bass⭐
Increased activity levels in the ventral striatum have been recorded in response to music
inferior frontal gyrus, anterior superior insula, ventral striatum, Heschel's gyrus and rolandic operculum → PLEASANT MUSIC
activation of the amygdala, hippocampus, parahippocampal gyrus and temporal lobes was increased (all of which are areas associated with negative emotions) → UNPLEASANT MUSIC
⭐nucleus accumbens increased activity during the experience and the caudate nucleus was more active during anticipation⭐
reduced or increased cortisol depending on the style of music (relaxing versus stimulating)
reduced beta-endorphins
increased immunoglobulin A (an antibody enhancing immune response)
increased oxytocin when singing.
L8 - SEX
Why & Relevance
difference:
biological
sociocultural
issues:
biological issues
sociocultural / psychological issues
Reproduction
Definitions
sex refers to a set of biological attributes in humans and animals
it is primarily associated with physical and physiological features including chromosomes, gene expression, hormone levels and function, and reproductive anatomy
reproduction, ensuring survival of your DNA
sex as a pleasurable activity
Asexual reproduction
single parent cloning itself
(A)sexual reproduction
asexual reproduction: multiply as you are
sexual reproduction:
conjugation: exchange of genetic material
creates genetic diversity
increases chance of better adapted organism
Sex: chromosomes and genetic sex
x sperm + x egg = xx embryo (female)
y sperm + x egg = xy embryo (male)
→ more variations
Male and Female Genitals
Biology of sex
factors present at birth, including:
the number and type of sex chromosomes
the type of gonads - ovaries or testicles
the sex hormones
the internal reproductive anatomy (such as the uterus)
the external genitalia
(Sex) Hormones
Sex hormones
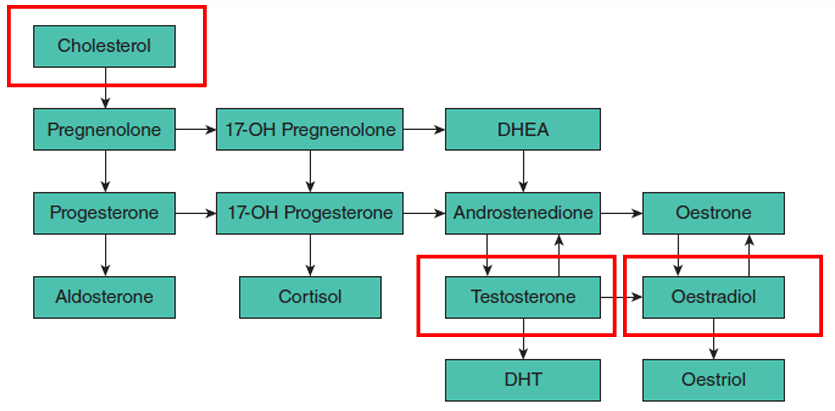
cholesterol at the basis:
synthesized to testosetrone by enzymes
which then synthesizes into oestradiol or oestrone by aromataste enzyme !!!!!!!!
⭐oestrogen is synthesized from testosterone⭐
Other relevant hormones
oxytocin (“cuddling hormone”, breastfeeding, orgasm, muscle contractions at giving birth)
prolactin
GnRH (FSH → sperm & egg /// LH → menstruation)
Menstruational Cycle & Ovulation
Uterus & endometrium
know: where the uterus, vagina, ovaries, uterine (fallopian) tube is, and what the uterus wall consists of
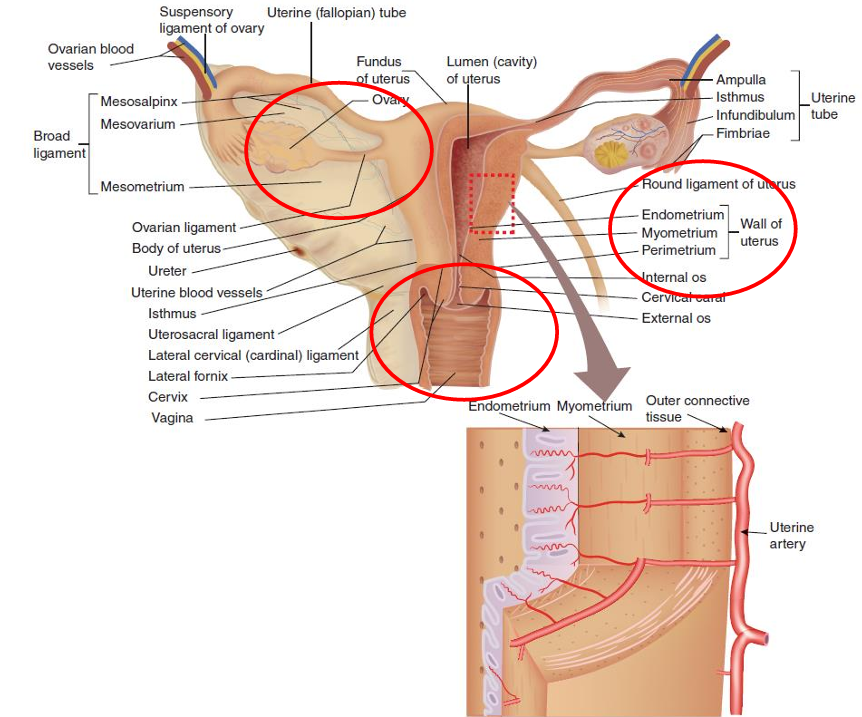
ovary: eggs
uterine tube: carries egg from ovaries into the uterus
uterus → cervix → vagina
uterus contains three layers and thickness of the endometrium is important for the nesting of an fertilized embryo
→endometrium gets broken down during menstruation !!!!
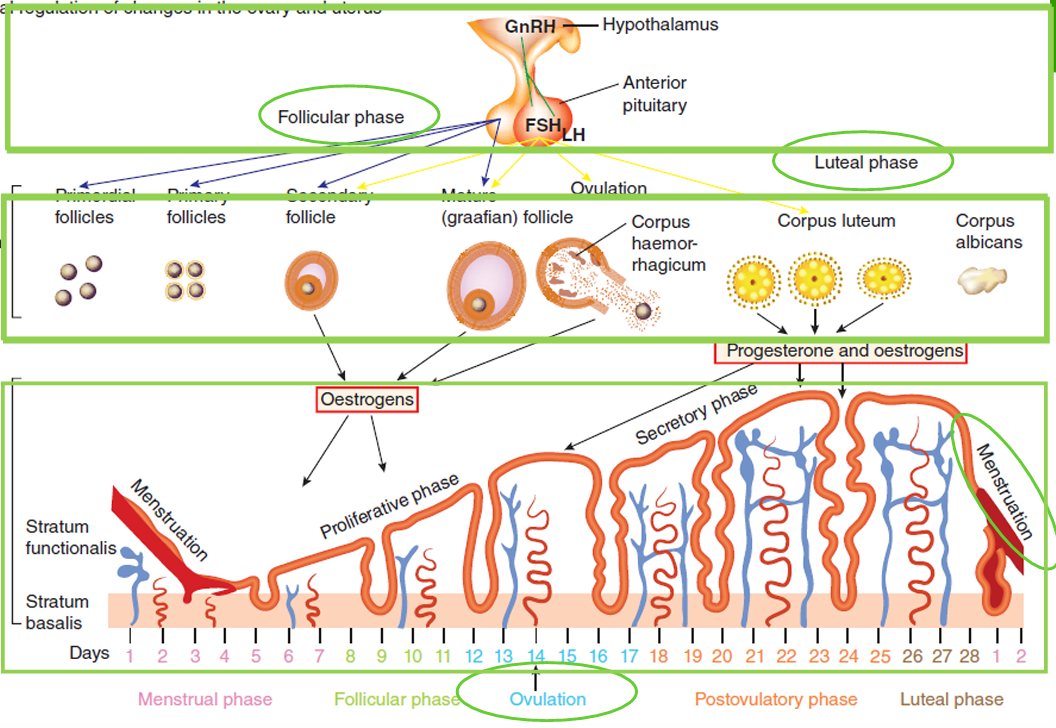
different phases driven by hormones
GNRH in hypothalamus
FSH and LH in anterior pituitary
follicle growth
14th day follicle pops and the egg is released which is the ovulation (caused by the steep peak of LH hormone)
the membrane that the egg was in shrinks to corpus luteum (yellow body)
follicle produces estrogen / estradiol → uterus starts to thicken
corpus luteum produces both estrogen and progesterone which impacts uterus (further thickness of endometrium to welcome the egg)
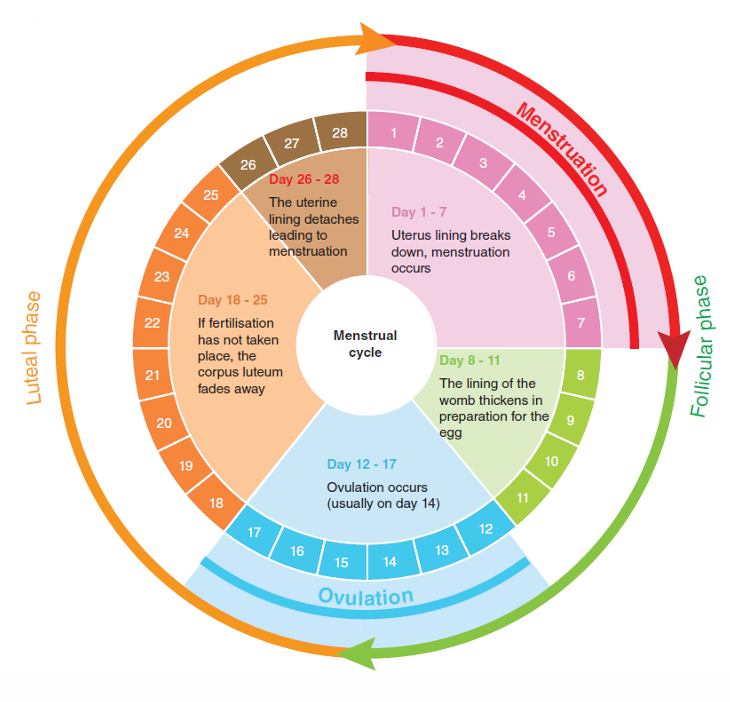
4 phases
follicular
ovulation
luteal
menstrual
Ovarian cycle
corpus luteum → progesterone → endometrium
determined number of follicles and eggs
one each month
two a month - heterozygotic twins
Hormonal control of the female reproductive cycle
the ovarian and menstrual cycles of female reproduction are regulated by hormones produced by the hypothalamus, pituitary, and ovaries
the pattern of activation and inhibition of these hormones varies between phases of the reproductive cycle
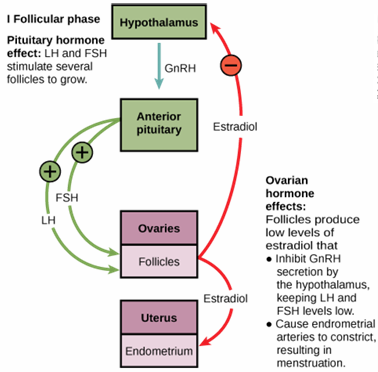
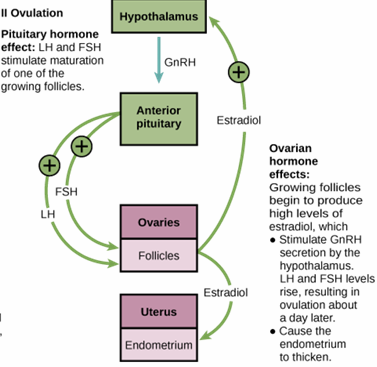
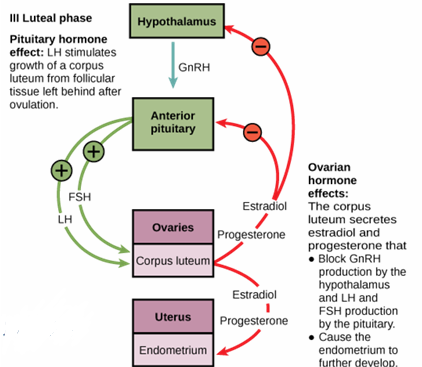
⭐3. luteal phase: double break (both hypothalamus AND anterior pituitary gland) → to further thicken the endometrium⭐
Menstrual cycle
follicular phase, starts with menstruation (photo: follicular covers menstruation)
gradual increase in estrogen
growth of follicles
peak LH at ovulation
luteal phase: progesterone level increases then decreases
repeat 28 days
Female issues
> PMS
slow increasing estrogen levels makes you feel relaxed, good, perfect (after menstruation)
ovulation and fertile phase
enter PMS: drop in estrogen and progesterone can induce irritability, anger or sadness (PMS)
pain sensitivity, acne, and cramps (PMS)
start of menstruation
repeat
⭐if abnormal: premenstrual dysphoric disorder (PMDD)⭐
> PCOS
slightly higher amount of testosterone:
irregular periods
more (facial) hair
large number of ovaries which look like cysts
often difficulties with reproduction
> MENOPAUSE
signs:
decreased estrogen production by the ovaries
low levels of testosterone
erratic levels of estrogen and progesterone
low levels of estrogen
thinner vaginal walls
common symptoms:
hot flashes
night sweats
decreased libido
irregular periods
mood swings
vaginal dryness
Sexual Development
virilization or masculinization is the biological development of sex differences
most of the changes of virilization are produced by androgens
⭐both sex differences are caused by male hormones⭐
Puberty
physiological changes:
fertility
breast development (thelarche)
pubic hair (pubarche)
ovulation and first menstruation (menarche)
growth spurt
enlargement of scrotum and penis
facial hair
Age of menarche
> DECREASE IN AGE OF MENARCHE IN WESTERN EUROPEAN & AMERICAN GIRLS
higher the education level earlier the menarche age, why?
women get their periods earlier each year, why?
→ SES status, well nourished = readiness
> DETERMINANTS OF MENARCHE ONSET
primary factors:
a girl’s age
weight - BMI - fat mass
SES status
age of menarche onset of the mother (in part genetic)
environmental factors / toxins
psychosocial stress (can postpone it)
> AGE OF MENARCHE DEPENDENT ON BMI
large BMI (overweight) = earlier onset !!!!
> FOOD & DIET
puberty onset and reproductive hormone axis activity require an adequate nutritional status
China: higher education > adequate nutrition available > earlier onset menarche
intake of animal foods has been associated with earlier sexual development, whereas vegetable protein intake is related to delayed maturation
childhood obesity is related to the earlier onset of puberty in girls
nowadays: abundance of nutrition, obesity related to lower SES
Cultural issues in sexual development
> FEMALE GENITAL MUTILATION
female genital mutilation comprises all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons
an attempt to control women’s sexuality, ideas about purity, modesty and beauty
usually initiated and carried out by women, who see it as a source of honor, and who fear that failing to have their daughters and granddaughters cut will expose the girls to social exclusion
more than 200 million girls and women alive today have been cut in 30 countries in Africa, the middle east and Asia
the procedure has no health benefits
procedures can cause severe bleeding and problems urinating, and later cysts, infections, as well as complications in childbirth and increased risk of newborn deaths
> AESTHETIC VAGINAL SURGERY: CULTURE AGAIN
gynoplasty: reparative or plastic surgery of the female genital organs
labiaplasty: is a plastic surgery procedure for altering the labia minora (inner labia) and the labia majora (outer labia), the folds of skin surrounding the human vulva
process:
pathologization of genital diversity: create a normal vs abnormal
portraying female genitals as important to wellbeing and sex life
portraying female body as degenerative and improvable through surgery
portraying surgery as safe, easy, and effective
Genotype vs phenotype
X0 - Turner’s syndrome | develop female sex organs and genitalia but often lack ovaries, they do not enter puberty and sexual maturation |
XXX | little emotion, impassive as children, late development in cognitive functioning and motor development (but normal physical development) |
XXY - Klinefelter’s syndrome | small testes, decreased facial hair, gynaecomastia (big male boobs), erectile dysfunction, infertility and cognitive deficits |
XYY | normal sexual development but tend to be more physically active as children and delayed in emotional maturity |
XY - Androgen insensitivity syndrome | lack of androgen receptors, female external genitalia but their internal female organs fail to develop |
XX | between external genitalia and male disposition |
persistent Mullerian duct syndrome | congenital lack of AMH or its receptors, causes both female and male internal sex organs (vagina and seminal vesicles) |
Male & Female Brain
Sex development in the brain
male:
testosterone converted into estradiol which masculinizes the neurons of the brain
female:
protected from masculinizing effects of estradiol
the protein “alpha-fetoprotein” binds to estrogens and stops it entering the brain
⭐estradiol masculinizes the brain ⭐
Gender
gender is usually conceptualized as a binary (woman or man) yet there is considerable diversity in how individuals and groups understand, experience, and express it
sex and gender differences can be used in research: examining biological (sex) vs sociocultural (gender) factors
gender refers to the socially constructed roles, behaviors, expressions and identities of girls, women, boys, men, and gender diverse people
it influences how people perceive themselves and each other, how they act and interact, and the distribution of power and resources in society
Nurture
parents
teachers
peers
the world in general - books, literature, movies, newspaper, social media
⭐gender roles are influenced by nurturing⭐
Make vs female
brain:
differences in volume
differences in connectivity - women have more connections
research:
cardiovascular studies on men doesn2t work on women
started to change
transgender brain?
transgender brain is more similar to the brain it is transferring to
L9 - PERSONALITY
Definition
Smith paper: Sullivan’s definition of personality “the relatively enduring pattern of interpersonal situations which characterize a human life”
Personality: particular combination of emotional, attitudinal, and behavioral response patterns of an individual
Personality Types
Type A
hostility
competitive
time urgent
Big Five
• neuroticism (emotionally unstable and easily anxious)
• extraversion (outgoing)
• conscientiousness (efficient and organized)
• agreeableness (friendly and compassioned)
• openness to experience (inventive and curious)
Questionnaire: Revised Neuroticism-Extroversion-Openness (NEO) Personality Inventory NEO-PI-R
Type D
negative affectivity
social inhibition
Personality & Health
Coronary heart disease (CHD)
hostility: tendency to experience anger, to be cynical or to have suspicious beliefs
→ related to atherosclerosis, incidence of CHD and mortality
Neuroticism
high neuroticism increased risk of mortality
high neuroticism is related to adverse cardiac events among cardiac patients and poorer cardiac functioning
high neuroticism is related to experiencing more somatic symptoms → students with high neuroticism had more somatic symptoms during exam period
Optimism
better health
less complications, less atherosclerosis
How do you know about these relations? (prevalence & incidence)
prevalence: how often does it occur?
examine whether a personality trait is more prevalent in persons with a disease compared to a group without a disease
case-control study: compare between group differences
incidence: how often will it occur in the future?
examine whether a personality trait is related to the incidence of people who will develop the disease
prospective cohort study: start with a group without the disease and examine the incidence over time
> PREVALENCE OF HOSTILITY
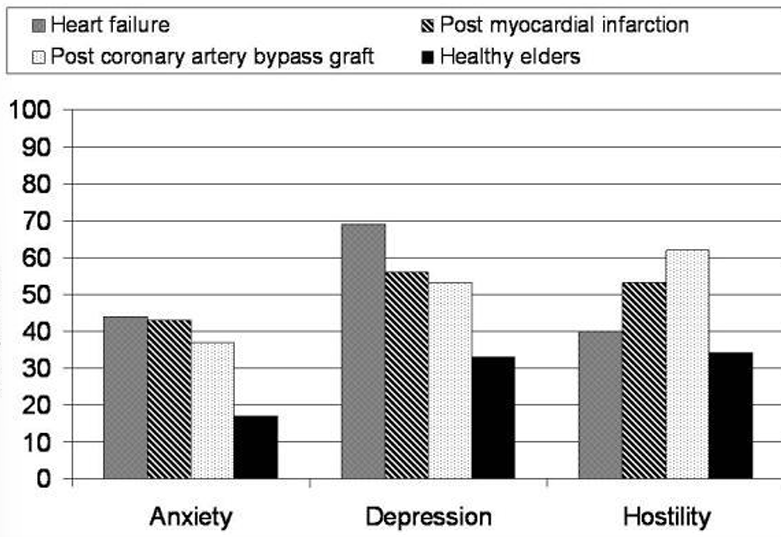
478 heart failure
298 post-infarction
131 post bypass
260 healthy elders
use cut-off score to detect percentage “high” hostility in each group
examine differences between groups
> HOSTILITY & INCIDENCE
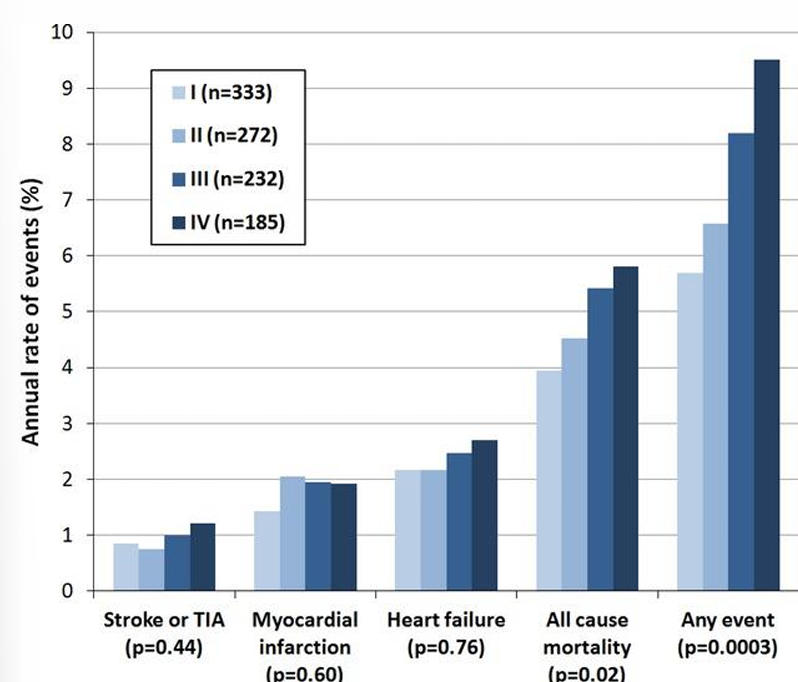
hostility in quartiles (1-4 → low to high)
highest hostile group related to more “all cause mortality” and “any event”
Summary
several personality types and constructs
topic of discussion
confirmed association with health outcomes (incidence, prevalence)
Type D Personality
Definition
combination of high scores on (have to have both)
negative affectivity (NA): tendency to experience negative emotions across time/situations
I am often in a bad mood
I often find myself worrying about something
I often make a fuss about unimportant things
social inhibition (SI): tendency to inhibit expression of emotions/behaviors in social interaction
I am a closed kind of person
I find it hard to start a conversation
I often feel inhibited in social interactions
Prevalence
general pop: 13-25%
cardiac pop: 25-30%
other patient pop: +-20%
⭐NOT PSYCHOPATHOLOGICAL TRAIT: normal variations among individuals⭐
Genetic basis
stable set of genes: type D personality is genetically determined and stable over time
variable set of environmental set of factors: different unique
Links with psychological constructs
> TYPE D & BIG FIVE
NA correlates with positively with neuroticism
SI correlates negatively with extraversion
→ related but similar
> TYPE D & SELF-ESEEM & ATTACHMENT
lower self esteem
inferior body image
diminished sense of personal accomplishment
type D’s more often have a preoccupied or fearful attachment style, while they are less likely to have a secure attachment style
> TYPE D & DEPRESSION
negative emotions | social inhibition | duration | |
depression | depressed affect in particular | not specified | < 2 years (episodic) |
type D | negative affect in general | elevated levels | > 2 years (chronic) |
Type D & CVD
Behavioral
> METABOLIC SYNDROME
a clustering of metabolic (biochemical) risk factors for CVD:
overweight, especially abdominally (large waistline)
high triglycerides and low HDL cholesterol
high blood pressure (or taking medication for hypertension)
high fasting glucose levels (or taking medication for diabetes)
type D individuals were twice as likely to have metabolic syndrome, irrespective of age, social situation presence of heart disease and other traditional risk factors (e.g. smoking)
conclusion: increased risk of incident CAD but not through traditional risk factors !!!!
> BEHAVIORAL MECHANISMS? (EXERCISE & DIET)
type D individuals adhered less often to the Dutch healthy activity norm (52% vs 62%) as well as to the Dutch fit norm (25% vs 35%)
> SO FAR…, ROLE OF BEHAVIORAL MECHANISMS
type D has been associated with future heart disease
metabolic syndrome may mediate this increased risk
type D’s unhealthy lifestyle did not completely explain the association with metabolic syndrome in our study (health behavior model)
this leaves room for other mechanisms, that still need to be elucidated (e.g. shared genes) → new research questions
Pathophysiological - possible pathophysiological mechanisms
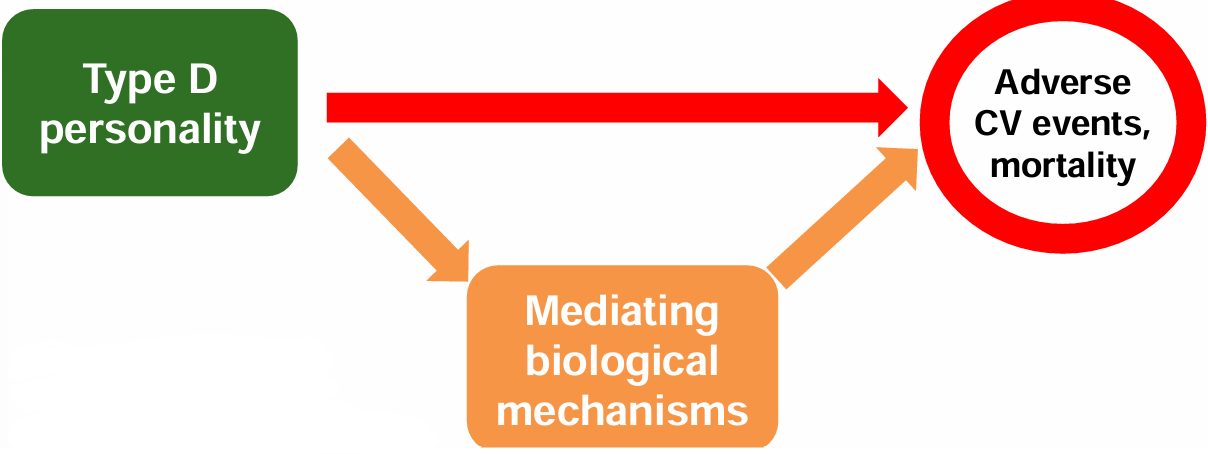
[Note: resembles the “interactional stress moderation model” by Smith, but does not include appraisal or coping]
mediating biological mechanisms, potential pathways:
cortisol (HPA axis)
immune system
norepinephrine (SAM axis)
oxidative stress
cellular aging
> CORTISOL (HPA - AXIS)
» HPA - axis
Hypothalamus Pituitary Adrenal axis
hypothalamus —(CRH)→ pituitary —(ACTH)→ adrenal cortex → cortisol ↺
example of a regulatory negative feedback loop
activated in stress situations
cortisol → many effects → energy balance
» Cortisol
hyper-activity: increased awakening response throughout the day
hypo-activity: decreased awakening response
» Cortisol as measure of stress reactivity
stress reactivity in response to trier social stress task (public speaking)
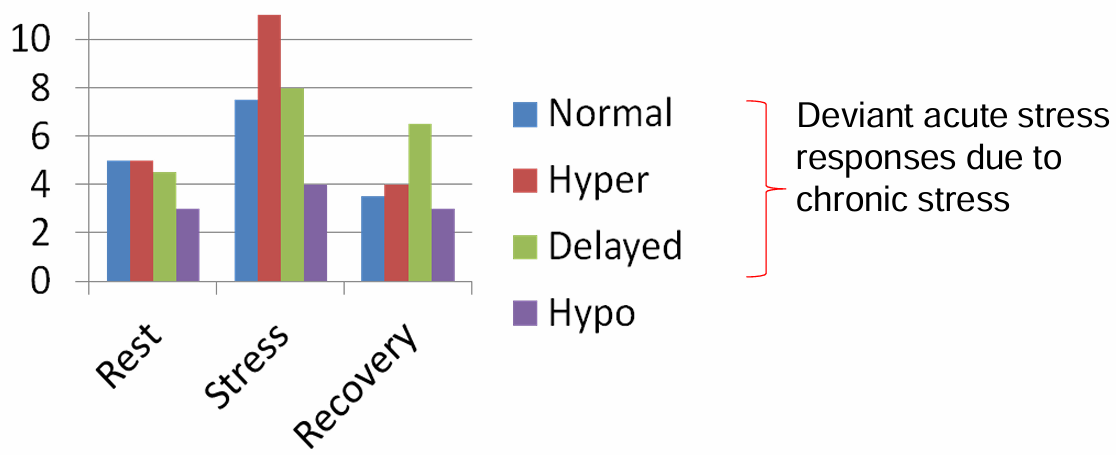
> IMMUNE SYSTEM
» Inflammation
cells (leukocytes = white blood cells):
nonspecific: macrophage, dendritic cell (eating cells), monocyte (undifferentiated macrophage)
specific: T-cells, B-cells
substances (messenger molecules):
nonspecific: C-reactive protein (CRP) = marker of inflammation
specific: cytokines such as interleukin 6 (IL-6), tumor necrosis factor a (TNF- \alpha), soluble TNF receptors (sTNFr1/'2)
⭐involved in atherosclerosis⭐
» Inflammation in atherosclerosis
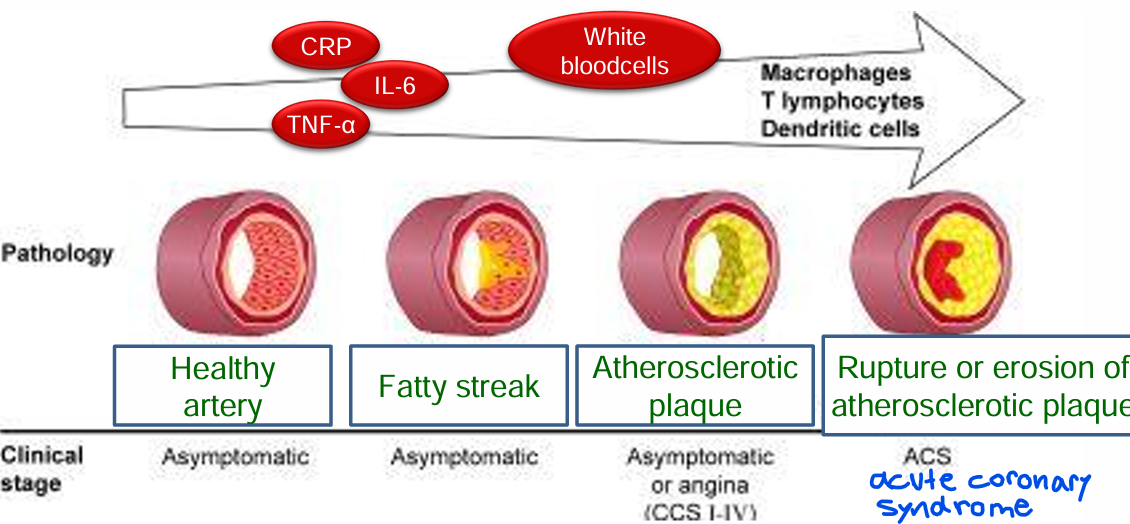
inflammation is involved in the gradual accumulation of cholesterol, fat and calcium in the walls of the coronary arteries
thrombi (blood clots) from ruptured plaques may cause a heart attack
asymptomatic (not necessarily related to symptoms)
» Inflammation predicts incident heart disease
analysis of 52 studies (246.669 patients)
CRP (a marker of inflammation) predicted the development of heart disease over a period of 10 years
same effect size as standard risk factors (BMI, family history)
especially obvious in men and patients who smoke
» Inflammation predicts long-term outcome
20 studies, total of 17.422 participants (2789 events)
patients with a higher CRP values after a heart attack had a larger chance of poor outcome (MACE major adverse cardiovascular events or death)
> NOREPINEPHRINE (SAM - AXIS)
» Heart rate control
intrinsic pacemaker capacity of the heart
sympathetic: activation of sympathetic nerves
increases heart rate (gas)
adrenaline and noradrenaline
parasympathetic: inhibitory, activation of vagus nerve decreases heart rate (brake)
acetylcholine
» Heart rate variability (HRV)
HRV is a measure of cardiac autonomic activity
measuring the time between to heartbeats = interbeat interval
HRV is the variation in these intervals
» Autonomic dysfunction in heart disease
altered cardiac autonomic activity, especially lower parasympathetic activity, is associated with the risk of developing a coronary heart disease
lower HRV after MI predicts both fatal and nonfatal cardiovascular events
⭐
high HRV: flexible and adaptive, balance between sympathetic and parasympathetic
low HRV: rigid and stressed out
⭐
» Type D & autonomic function
type D seems to be associated with an imbalance in the cardiac autonomic regulation
balance seems to tip towards higher activity (gas) during rest
decreased parasympathetic control
> OXIDATIVE STRESS
“rusting process”
occurs when there is an excess of free radicals (oxidants), a decrease in antioxidants, or both
damage to cell walls, DNA, cell contents, etc.
involved in artery and heart muscle damage
unhealthy lifestyle contributes to oxidative stress
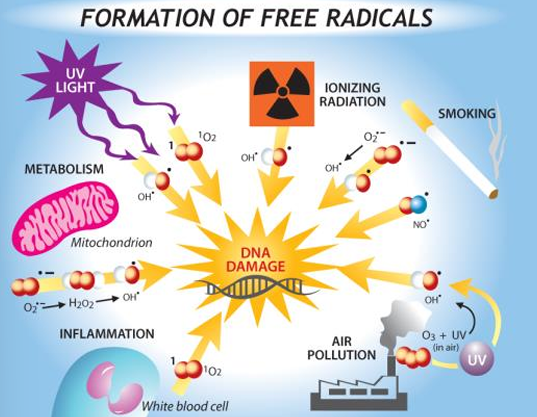
> CELLULAR AGING
telomere shortening: as cells divide over time telomeres shorten, and eventually cell division stops → biological age of cells
» Exposome paradigm
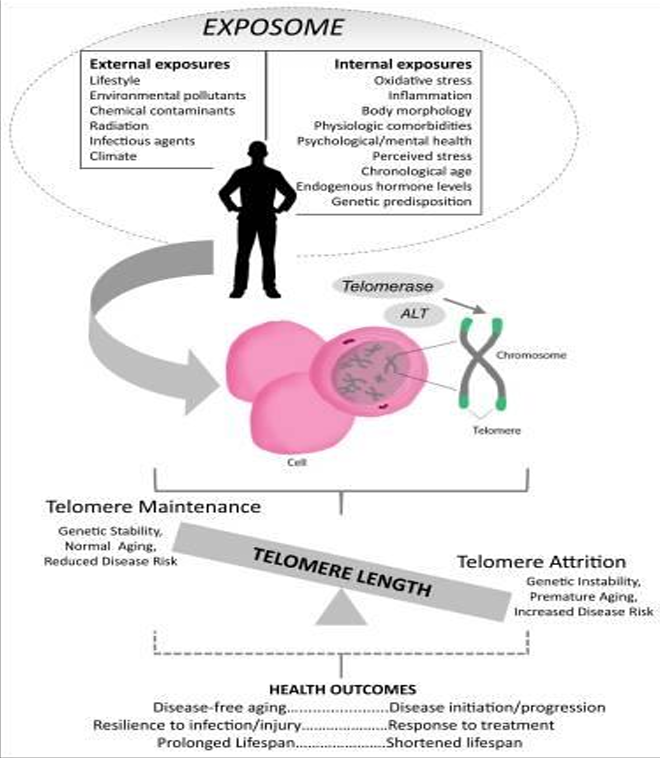
» Type D & cellular aging
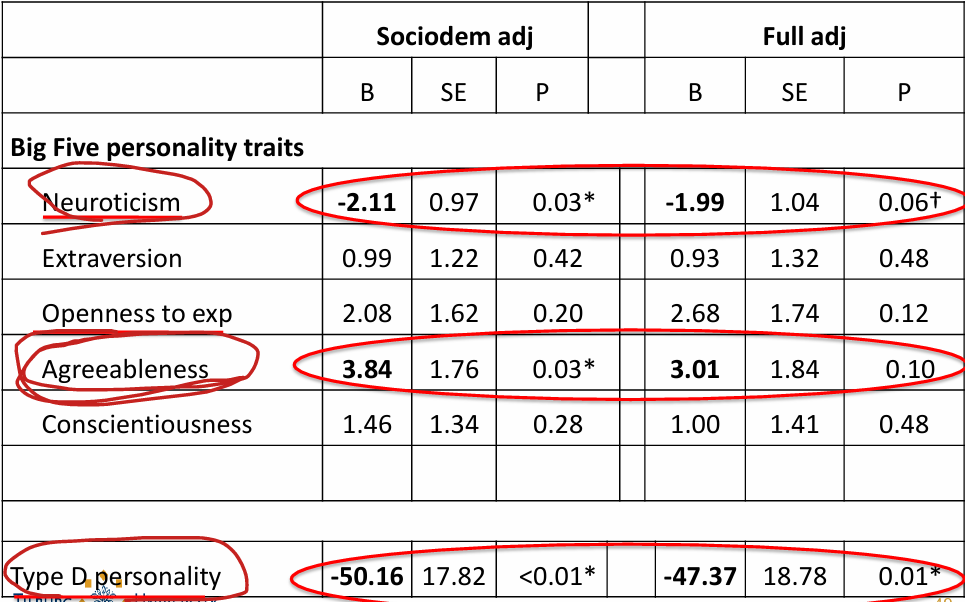
Summary
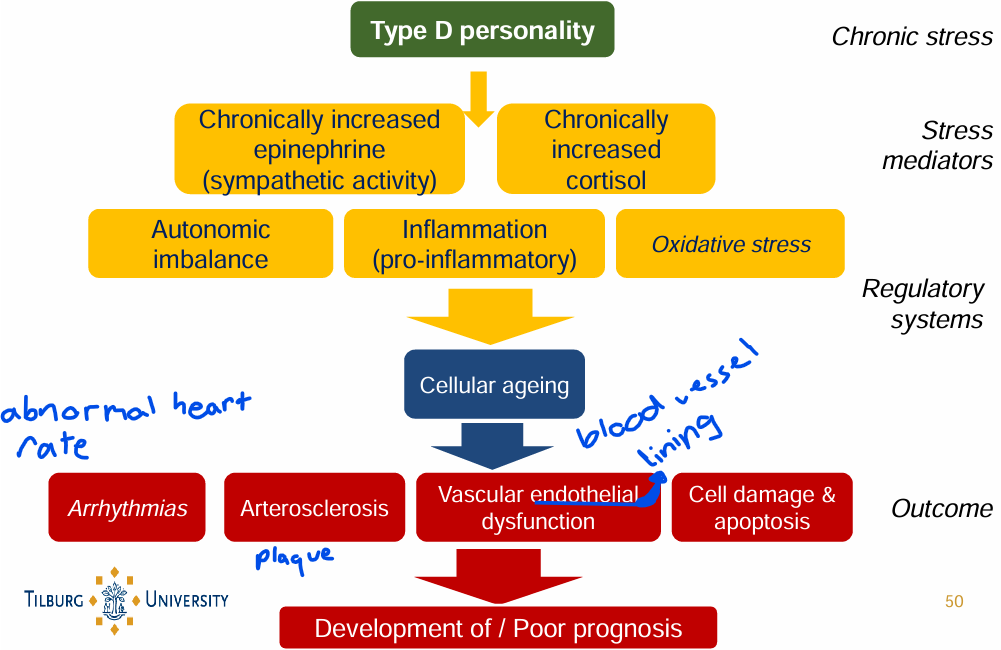
Clinical Implications
should we screen for type D personality in cardiologic (somatic) practice?
primary and secondary prevention are relevant (how?)
tailored health care, taking into account type D characteristics
Hypercortisolemia & Coronary Arteries
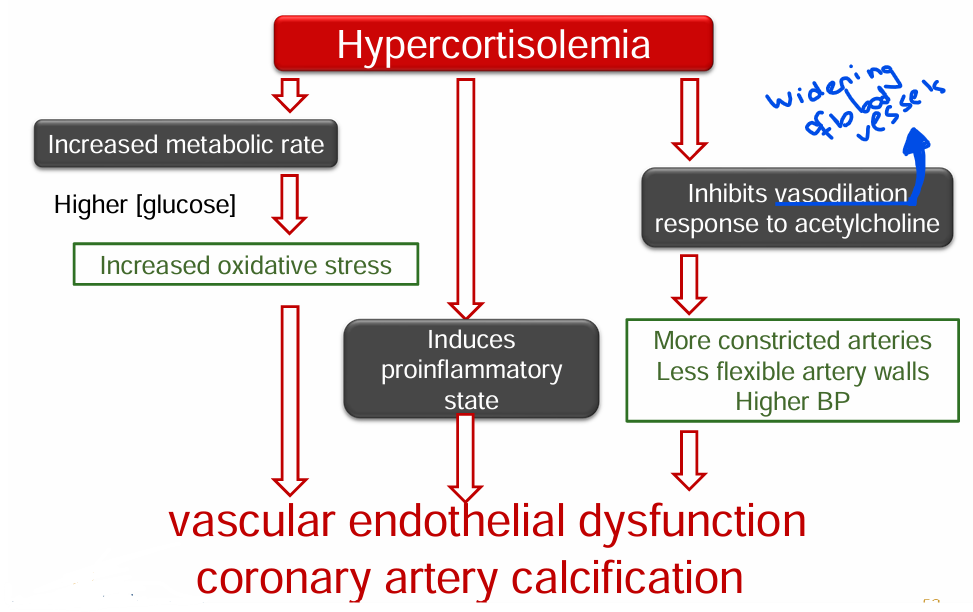
Theories
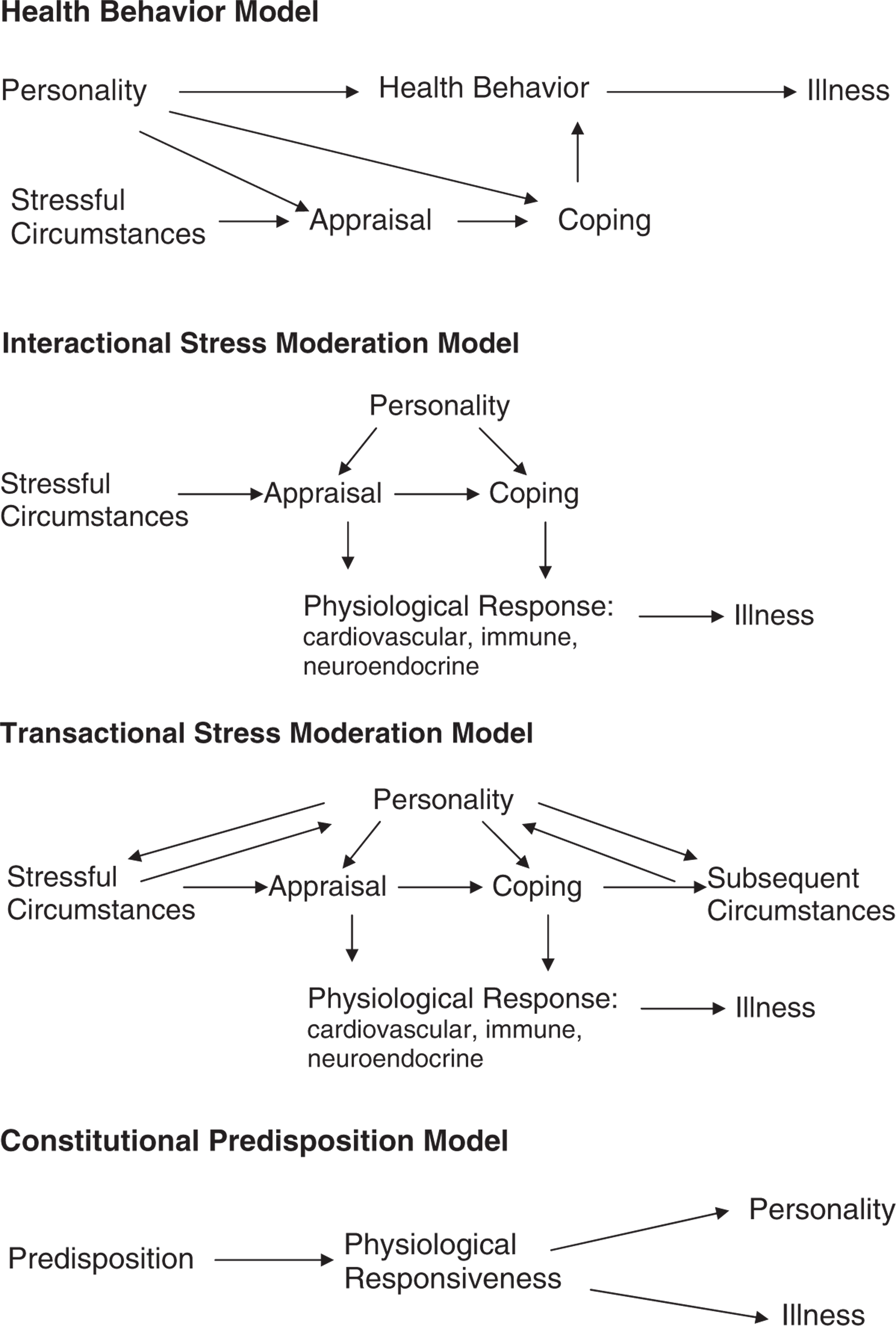
L10 - HEART & BRAIN
Terms
Cardiovascular diseases (CVDs): any diseases involving the heart or the blood vessels
Acute coronary syndrome (ACS): umbrella term for any situation where blood flow to the heart muscle is suddenly reduced or blocked
myocardial infarction (MI): heart attack - blood flow is blocked long enough to cause damage or death of heart muscle
Atrial Fibrillation (AF): atria start quivering or “fibrillating” instead of contracting properly
Cardiovascular Physiology is Important to Biological Psychology
cardiovascular diseases (CVDs):
are the leading cause of death globally
was responsible for 17.9 million deaths in 2019
that is 32% of all global deaths
in the NL:
cardiovascular disease is still the leading cause of death in women
cancer is the overall leading cause of death
in the USA:
CVDs are the leading cause of death
Anger as trigger of acute MI
Sir John Hunter: angry and rude, died of a heart attack after an argument
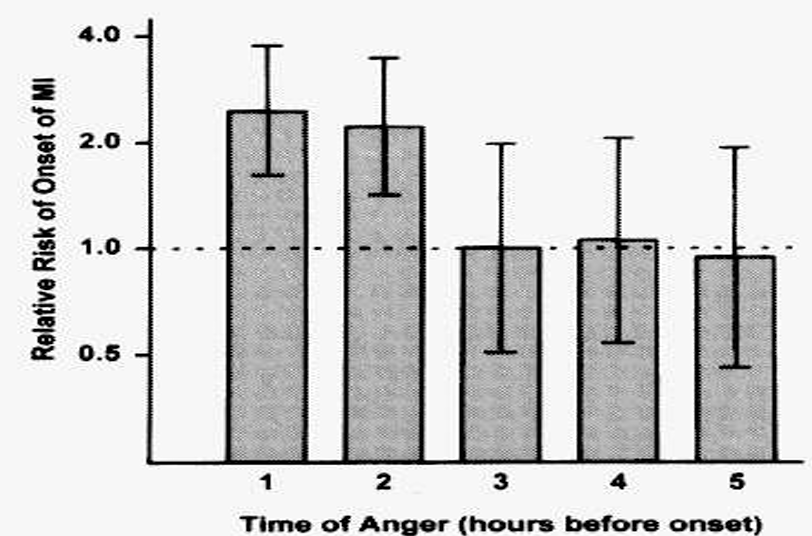
MI patients were interviewed at an average of 4 days after MI admission:
Anger occurred in 39 patients in the 2 hours preceding the MI
130 participants reported anger in 24 hours prior to MI
N = 1623, RR = 2.3 (95%CI = 1.7-3.2)
results may be influenced by retrospective bias (i.e. patients reporting emotional triggers as part of “seeking meaning” for their cardiac event)
Overview of Cardiovascular Disease
artery (red / oxygenated / fresh): away from heart, high pressure, narrow
vein (blue / deoxygenated / used): toward heart, low pressure, wide
the cardiovascular system consists of:
the heart (pump)
the blood vessels (to supply all tissues of the body with oxygen and nutrients)
systematic circulation: sends oxygenated blood to the whole body
pulmonary circulation: oxygen refill trip (just between heart and lungs)
coronary arteries: feed the heart muscle itself (myocardium)
Inside of the heart
the heart is a pump:
it pumps oxygenated blood out of the left ventricle (LV)
it pumps used blood through the lungs via the right ventricle (RV)
it needs blood supply from coronary arteries to function (contract) properly
Heart from the outside
coronary arteries lie on top of the heart muscle:
left coronari artery (LCA)
left anterior descending (LAD) artery
circumflex artery (LCx)
right coronari artery (RCA)
right marginal artery
posterior descending artery (PDA)
Main types of cardiovascular diseases (CVD)
coronary heart disease (CHD): a broad term for diseases that affect the heart itself due to the narrowing or blockage
coronary artery disease (CAD): the specific problem where the coronary arteries are narrowed are blocked by plaque build up (CAD is the main cause of CHD)
myocardial infarction (MI): the event - heart attack where part of the heart muscle actually dies due to complete blockage of a coronary artery
symptoms: chest pain (angina pectoris), shortness of breath, fatigue
Heart failure (HF): when the heart can’t pump blood effectively (still beating, just struggling)
caused by:
CAD / CHD
MI
valve diseases
valve disease
arrhythmias / sudden cardiac death (SCD): severe abnormal heart beats
stroke / CVA & TIA
other (e.g., endocarditis - inflammation of the inner lining of the heart)
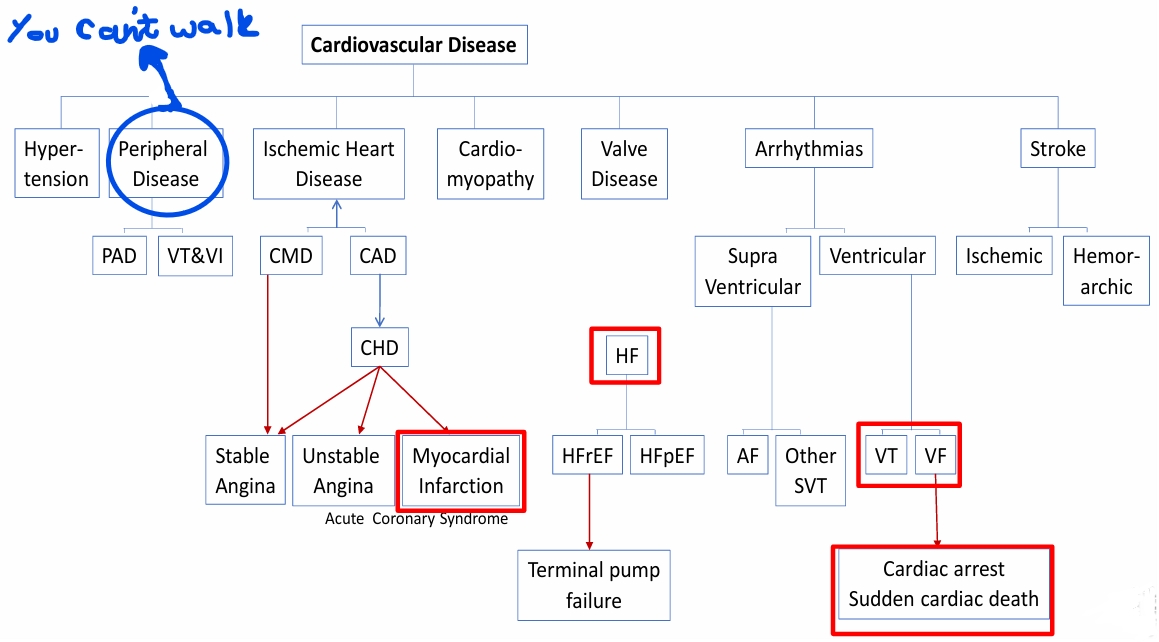
Coronary atherosclerosis & myocardial infarction
coronary atherosclerosis: build up of plaque inside the coronary arteries
tissue damage develops “behind” a complete narrowing
⭐non-atherosclerotic artery → healthy⭐
Atherosclerotic coronary heart disease: pathology, manifestations, and timeline
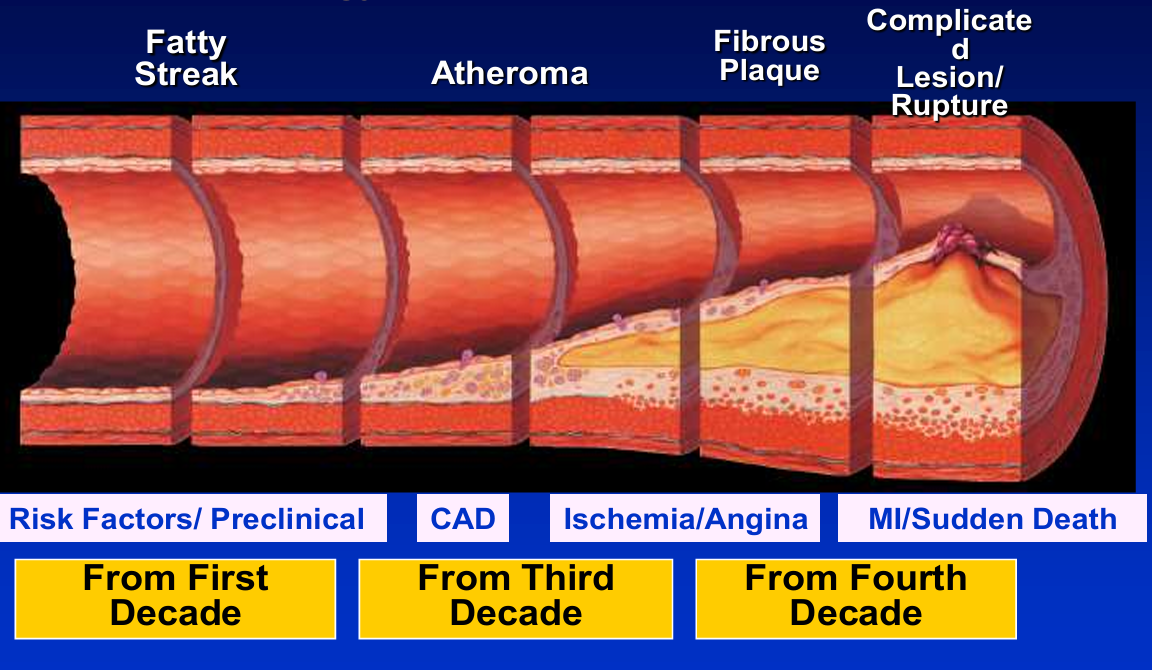
Risk factors for coronary artery disease
modifiable:
hypertension
diabetes mellitus
elevated lipid levels (cholesterol, LDL, low HDL)
smoke
overweight
psychological factors
non-modifiable:
age
sex (male)
genetic factors / family history of CVD
Myocardial ischemia
ischemia = insufficient blood supply to tissue or muscle
→ results in shortage of oxygen in places where it’s needed
myocardial ischemia is typically transient (temporary) in patients with stable coronary disease because:
there is reduced supply because of coronary narrowing, combined with
transient (temporary) increases in cardiac demand (e.g., by exercise, anger)
typical symptoms are chest pain / pressure and shortness of breath
if ischemia is severe and prolonged, permanent damage to the heart muscle can occur → myocardial INFARCTION (MI)
Treatment of coronary artery disease
percutaneous coronary intervention (PCI: coronary angioplasty: used to re-open narrowed coronary arteries) → stent
coronary artery bypass graft (CABG) surgery (used to “bypass” a narrowed segment(s) in one or more coronary arteries) → creates another road
thrombolysis (used to re-open a (nearly) completely blocked coronary artery in the setting of myocardial infarction)
Psychological Factors and Heart Disease
ACUTE FACTORS (triggers)
within an hour
anger, mental arousal, etc
EPISODIC FACTORS
transient (2 weeks - 2 years)
recurring
major depressive disorder, exhaustion
CHRONIC FACTORS (traits)
gradual
trait anxiety, hostility, type D / negative effectivity, low SES
⭐associations with disease progression depend on severity of underlying coronary disease⭐
⭐most psychological risk factors for CVD are “sub-threshold” → not meeting diagnostic criteria for psychological or psychiatric disorder⭐
Prevalence of depression in patients with medical conditions
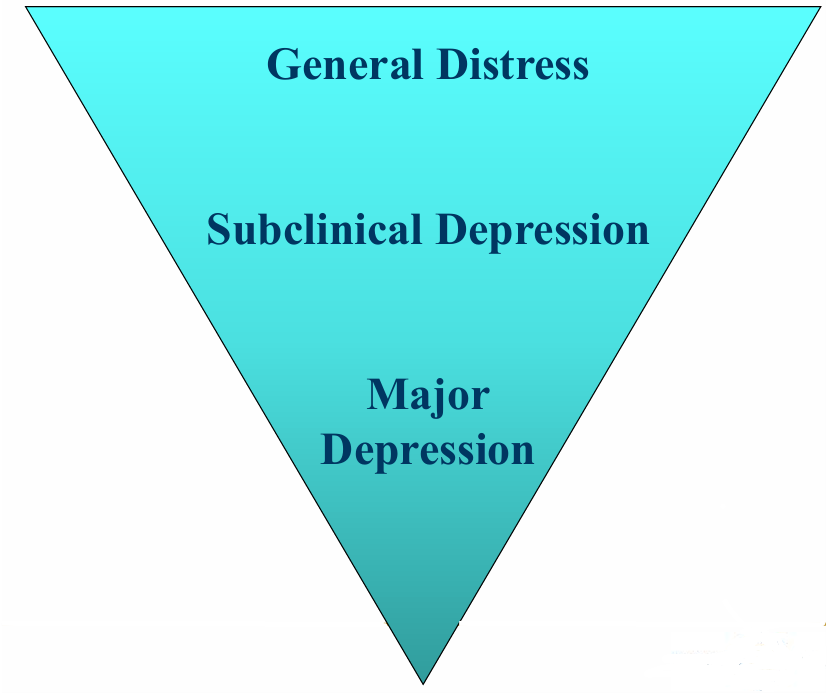
Stress
psychological distress: a negative internal state of the individual that is dependent on interpretation or appraisal of threat, harm, or demand
> WHAT IS STRESS?
there is a wide range of theories and models about stress
process that unfolds over time and involves the whole person
“stress” can refer to: a stressor, feeling, or consequence
distress response (what we typically mean by “stress”): how environmental events (stressors) threaten us, how they are interpreted, and how they make us feel
→ 2 types of distress response:
eustress: stress evoked by positive emotions or events (this term is not very common anymore)
distress: stress evoked by negative feelings or events
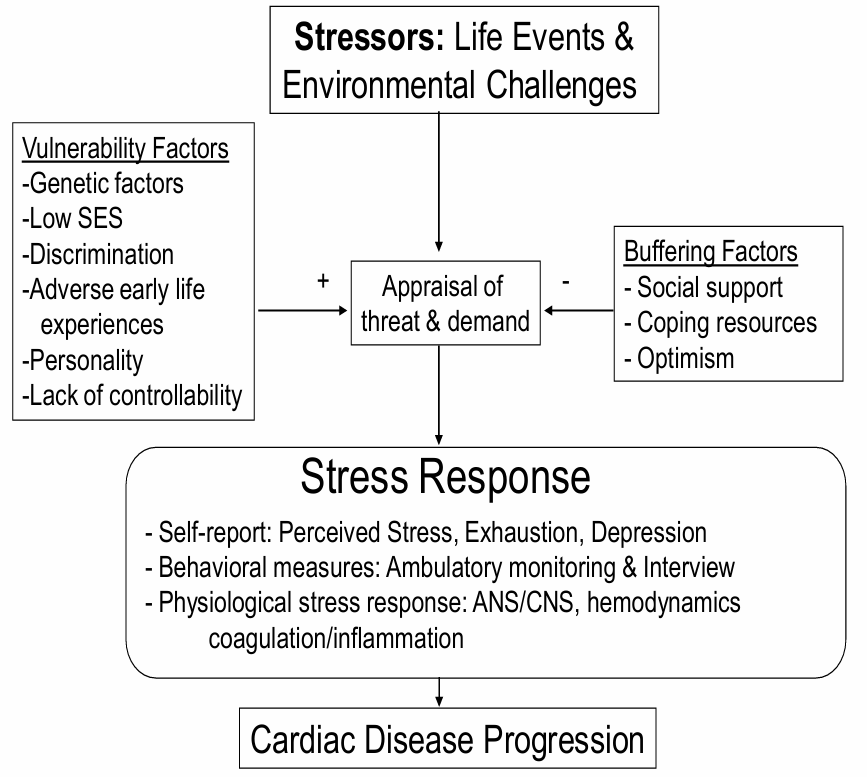
> VARIABLES AFFECTING STRESS RESPONSE
time
control
individual vulnerability
> YERKES - DODSON LAW
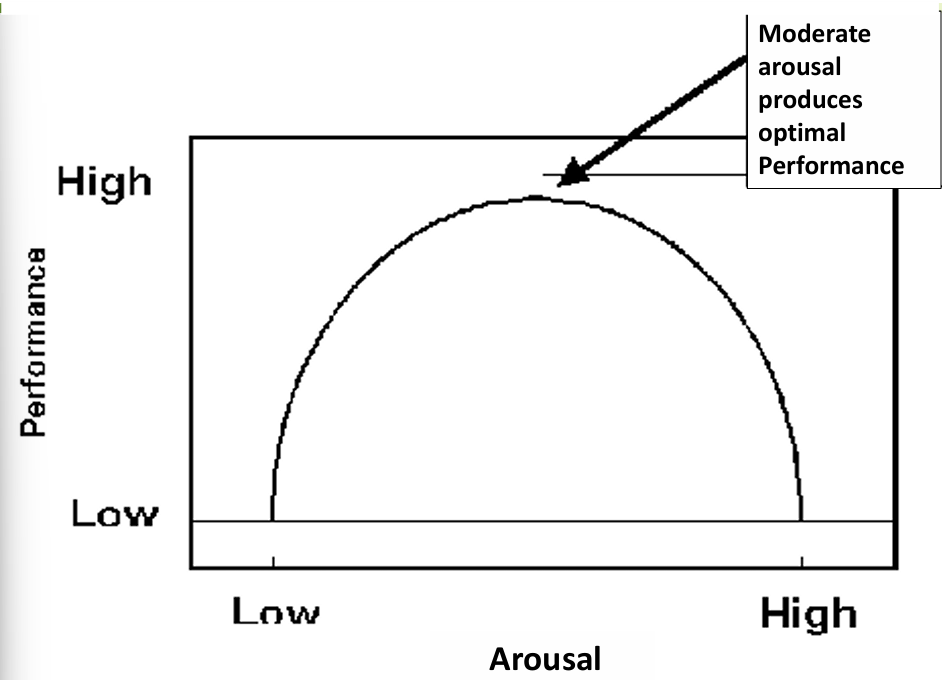
EXAM!
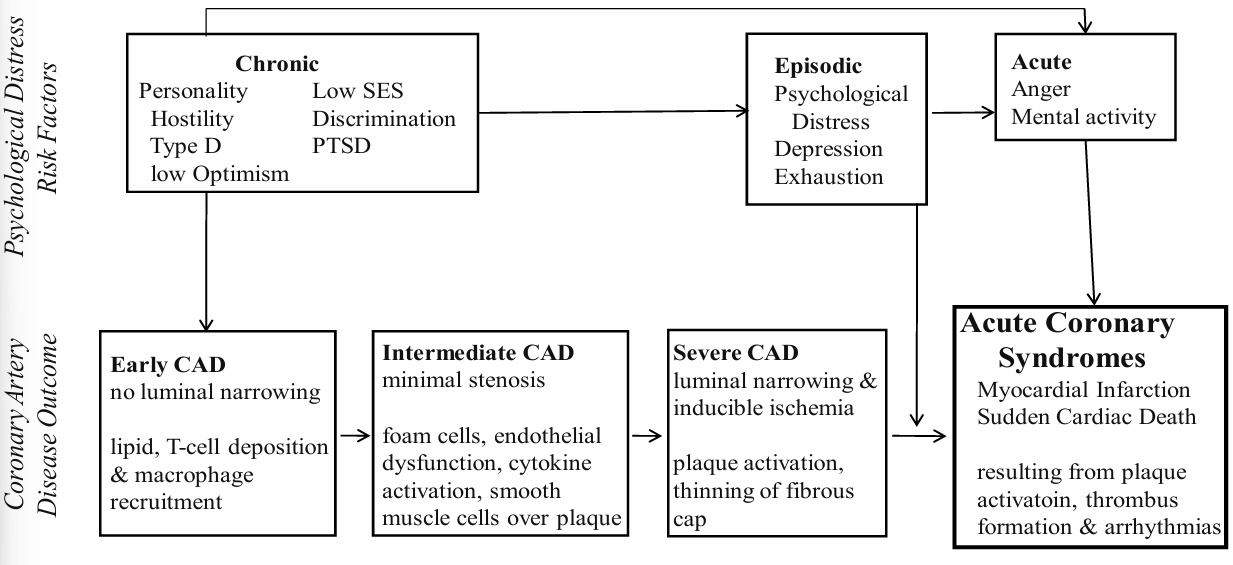
⭐chronic risk factors already play a role in early stages, but acute risk factors don’t ⭐
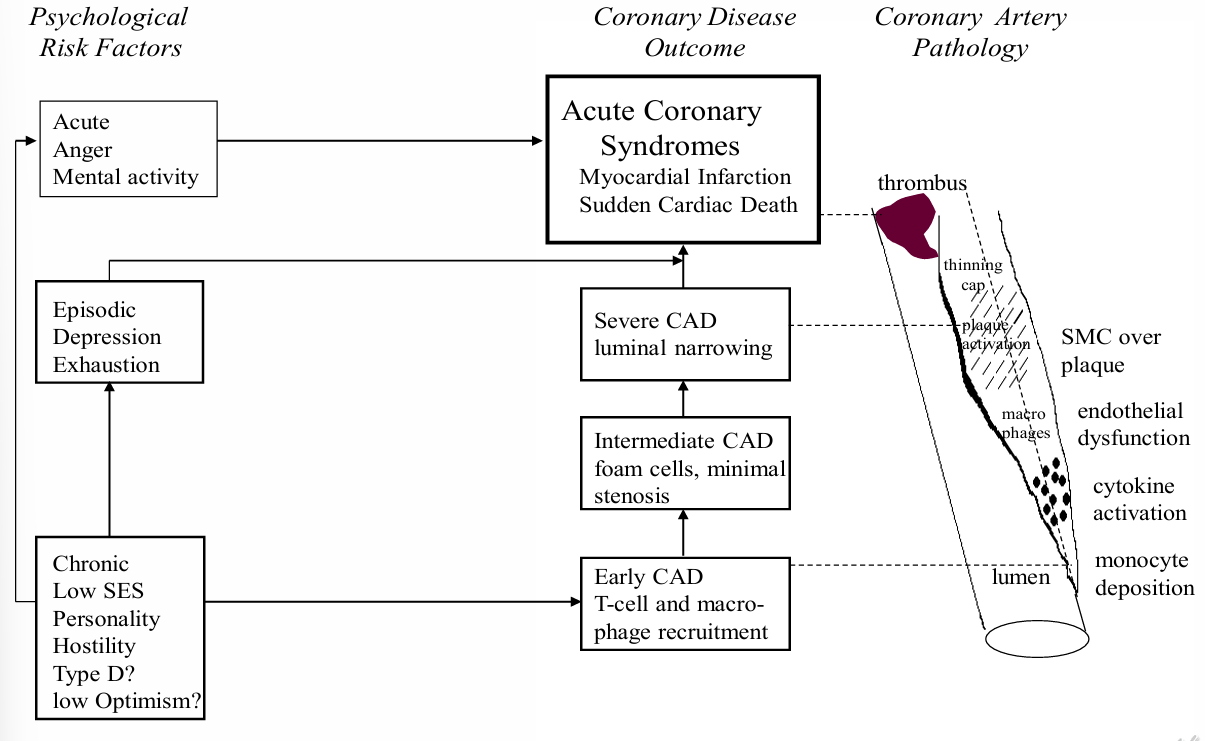
⭐REMEBER FOR EXAM⭐
Acute Psychological Risk Factors for Cardiac Events
anger - disaster (coronary patients increase after an eq)
anxiety - acts of war /violence / aggression
acute distress - major public events (sports, elections)
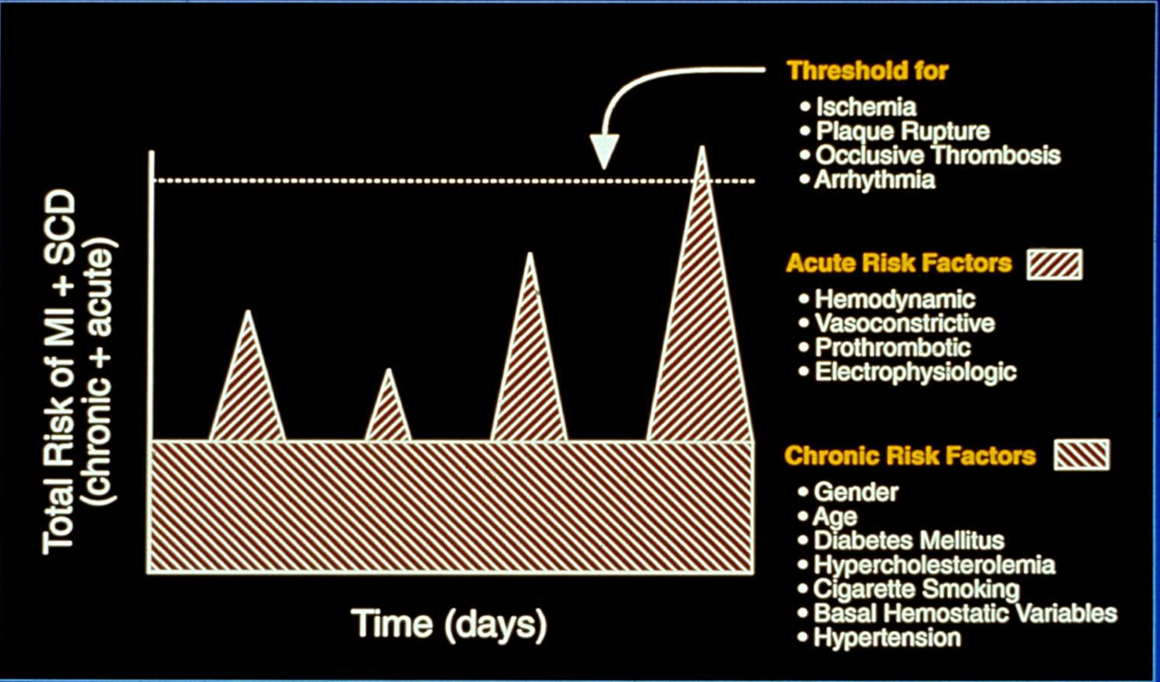
Going back - anger as trigger of acute MI
why there was only 39 people that scored 2h?
anger scale:
calm
busy but not hassled
mildly angry, irritated, and hassled, but does not show
moderately angry - so hassled, it shows in your face
very angry, body tense, clenching fists or teeth
furious, almost out of control, very angry, pound table, slam door
enraged! lost control, throwing objects, hurting yourself or others
→ because these are rare
Myocardial ischemia
chest pain is the tip of the iceberg
cardiac event - clinical test:
chest pain — history
ST-T wave changes — ECG
systolic function: heart’s pumping ability — RVG, echo
diastolic function: amount of pressure in the arteries when the heart is at rest — RVG, echo
metabolic changes — PET scan
reduced perfusion — perfusion scintography, PET scan (contrast echo)
> MENTAL STRESS ISCHEMIA: MECHANISMS
decreased cardiac supply (narrowing coronary arteries)
increased cardiac demand ( hemodymanic reactivity)
→ blood pressure, heart rate, contractility
> THE ECG - THE RECORDING OF A MOVING CURRENT
measure of the changes in electrical loading of extracellular fluid due to electrical changes that occur in all cardiac muscle cells together
⭐the ECG represents all phases of the conduction pathway
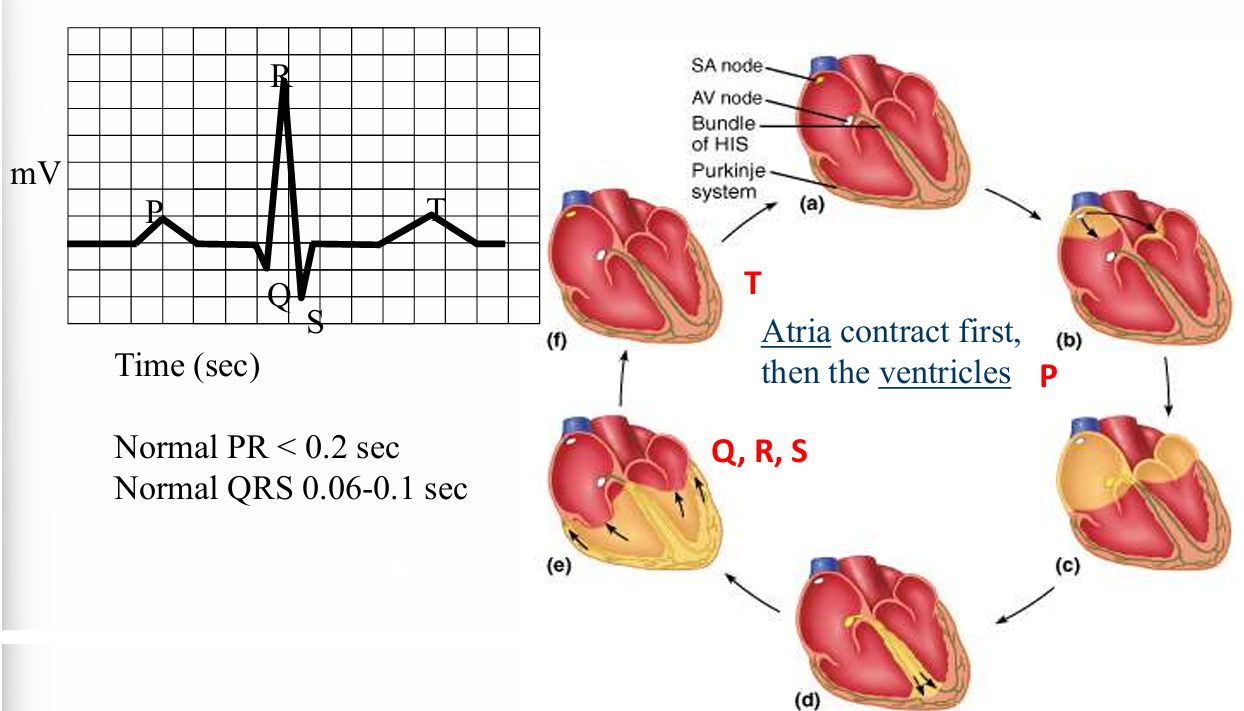
what does the ECG provide you with?
heart rate: net effect of cardiac parasympathetic and sympathetic NS activation
→ R-R interval = time between two beats
⭐60 / R-R = heart rate
< 60 beats per minute: bradycardia
> 100 betas per minute: tachycardia
ST - segment: depression / elevation
> FIELD STUDIES
patients with documented CAD → ambulatory ECG monitoring → detect ST depression → correlate with patient diaries
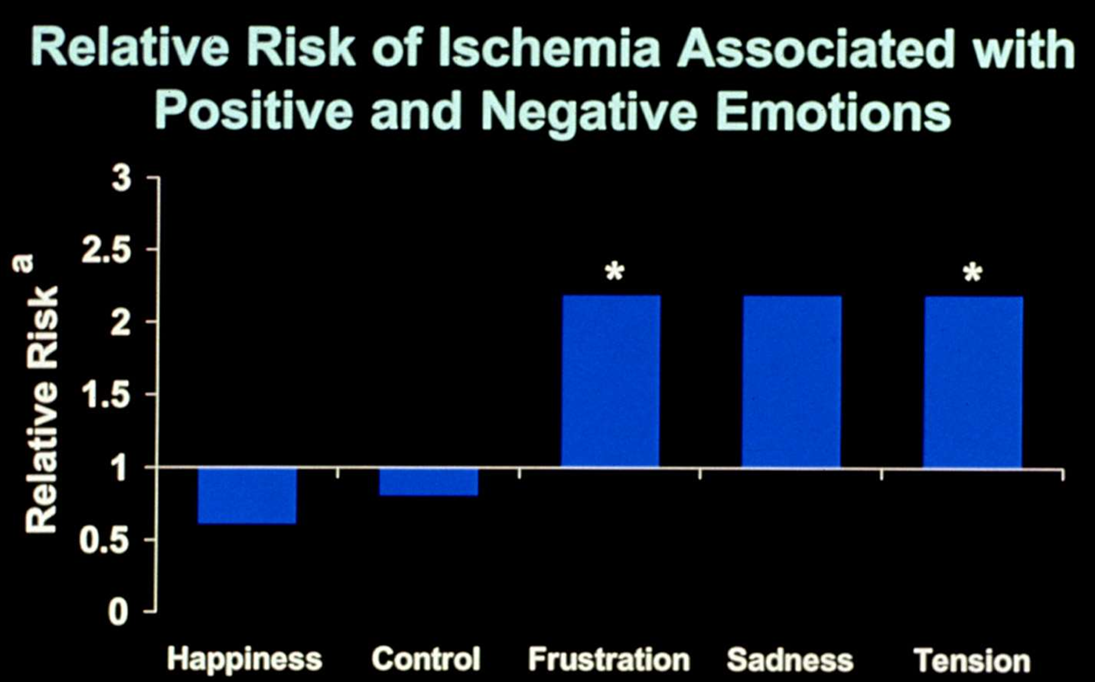
» DAILY LIFE ACTIVITIES AS TRIGGERS OF MYOCARDIAL ISCHEMIA
ambulatory ischemia: episodes of reduced blood flow to the heart that happens while a person is going on about their daily lives
examples of physical activity:
sleep
rest, reclining
eating, talking
washing, dressing
shopping
climbing stairs, heavy physical work
examples of mental activity:
sleep
rest, reading
talking, clerical work
waiting, driving
concentrating
anger or anxiety
»» CIRCADIAN VARIATION IN TRIGGERING AMBULATORY ISCHEMIA BY PHYSICAL ACTIVITY & MENTAL STRESS
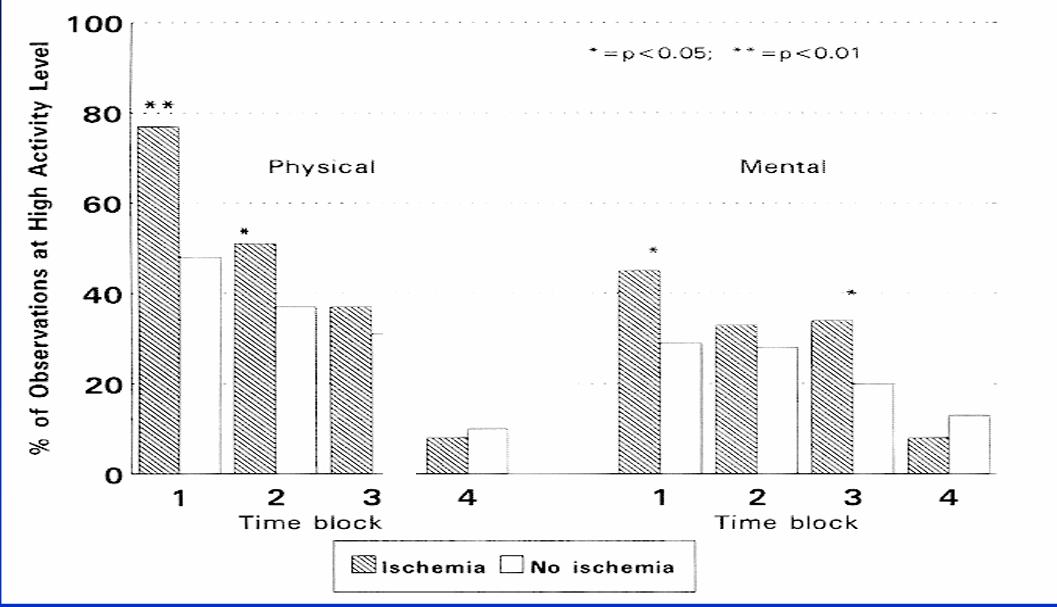
»» AMBULATORY MONITORING STUDY OF PRE-ISCHEMIC REDUCED PARASYPATHETIC ACIVITY
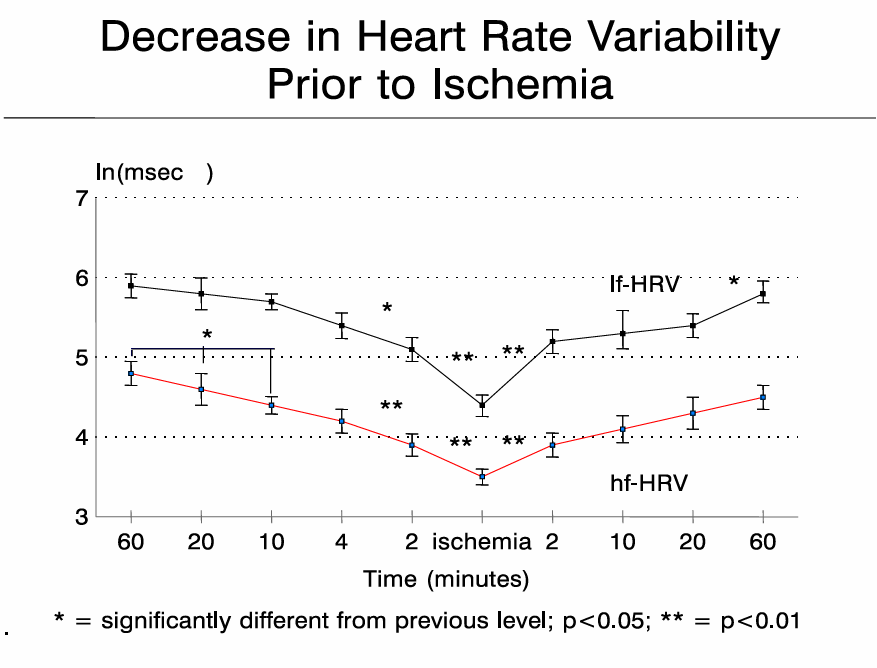
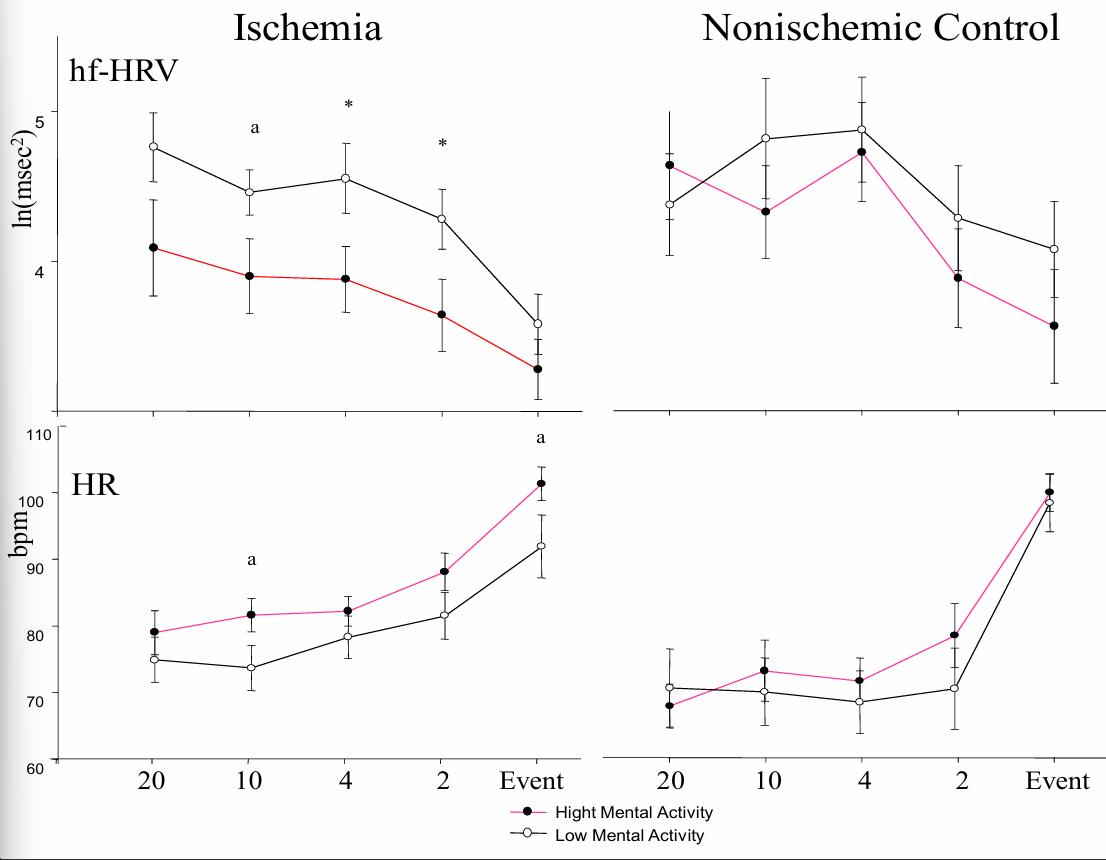
Summary
the heart is a muscle that pups oxygenated blood throughout the body (systematic circulation)
the heart also pumps “used” blood through the lungs for re-oxygenation
like any muscle, the heart muscle also needs supply of oxygenated blood, this occurs via the coronary arteries (this is a different process than the heart’s pump function)
myocardial infarction (MI) and sudden cardiac d. are the end-stage of progressive coronary artery disease
psychological stressors play a different role in the development of heart disease: acute, episodic, and chronic risk factors
acute mental stress can trigger MI and myocardial ischemia during daily life - partially mediated by changes in autonomic nervous system activity!!!!!!!
Need for the Study of Myocardial Ischemia (Lab Studies)
multiple mental stress stimuli + exercise = provocation
measure various markers of myocardial ischemia:
wall motion
perfusion
ECG
chest pain
Assessment of wall motion
> ECHOCARDIOGRAPY & RADIONUCLIDE VENTRICULOGRAPHY
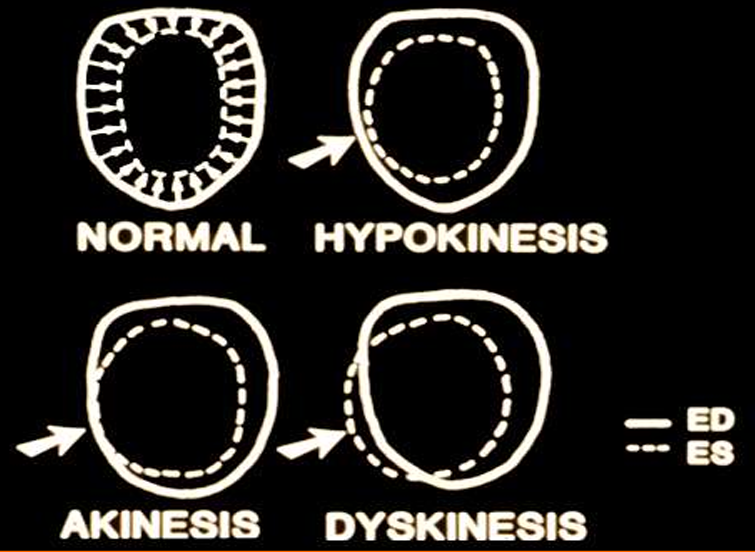
end diastole (ED): fully relaxed, filled with blood, largest
end systole (ES): contracted inward, pumping out blood, smallest
hypokinesis: moves less than normal
akinesis: doesn’t move
dyskinesis: moves outward instead of inward - very dangerous!
> CASE STUDY: EFFECT OF STRESSFUL IMAGERY ON ISCHEMIC LV WALL MOTION
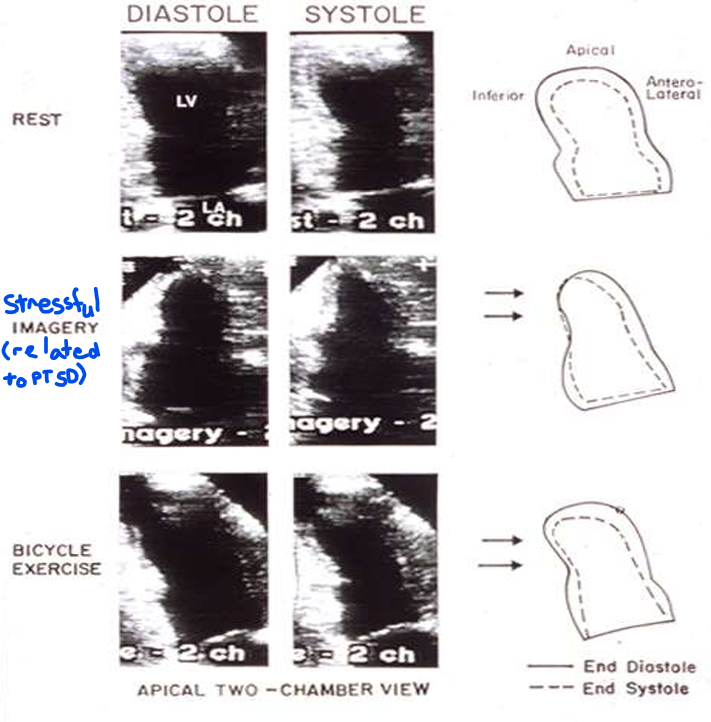
patient with PTSD and angina equivalent (cough) → thinking of trauma —→ ischemic
> ISCHEMIA WITH SPECT (moderate / severe)
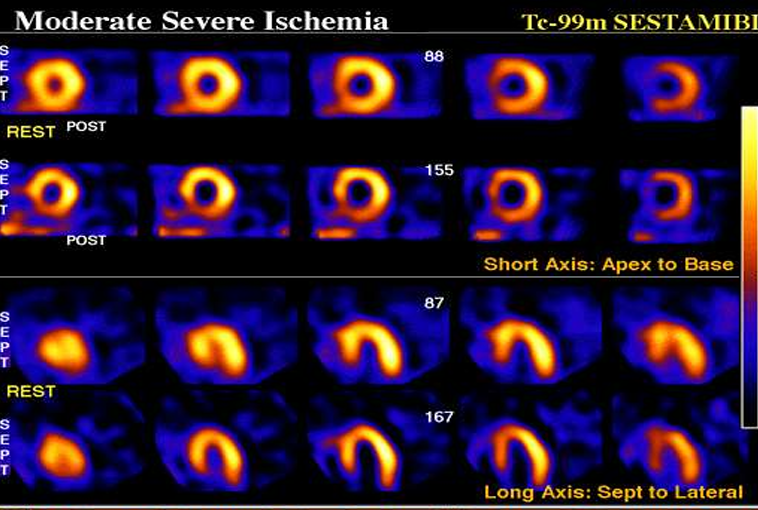
Clinical issues - panic disorder and inducible ischemia based on perfusion defects
1 vital capacity inhalation of a gas mixture containing 35% carbon dioxide and 65% oxygen
→ elicited panic in 26 / 35 participants who had CAD and panic disorder (PD)
→ and elicited panic in only 2 / 30 participants who had just CAD
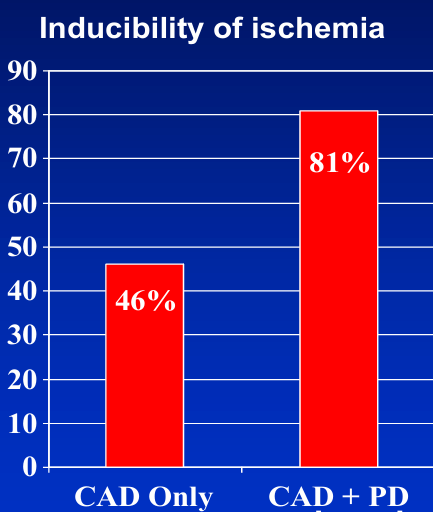
Transient coronary occlusion in response to acute mental arousal
coronary construction common with acute mental stress (reduced supply) - this is an extreme case (1 in 200)
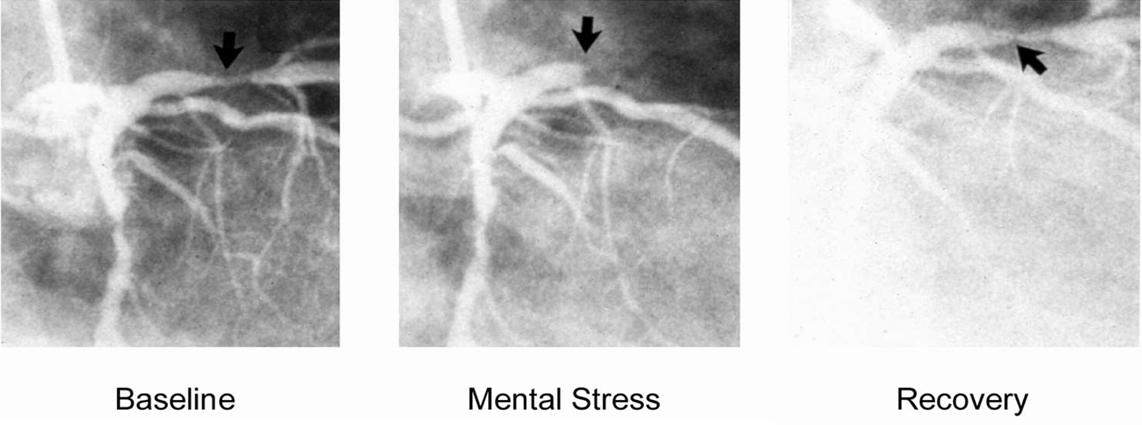
Relation between blood pressure response to mental stress and coronary constriction
59 CAD patients (age 60 to 80, only 8 women)
repeated angiograms
baseline control
3 minute mental arithmetic
200 micro g intracoronary NTG
18.6 % coronary constriction
blood pressure (BP) responses associated with constriction in diseased segments (not in nonstenotic / not-narrowed segments)
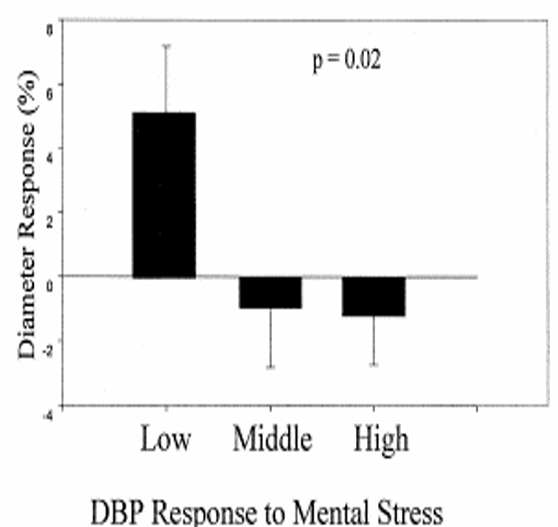
Mental stress-induced ischemia characteristic features
⭐observed in 30-70% of patients with coronary artery disease
rarely detectable with ECG in the lab
requires myocardial functional or perfusion imaging (echocardiography, SPECT, PET, cardiac MR)
often asymptomatic (silent ischemia)
more common in patients with exercise-inducible ischemia than in patients without
effects in the lab vary in reproducibility
associated with ambulatory ischemia
occurs at lower heart rate (i.e., lower cardiac demand than with exercise)
⭐reduced coronary supply plays an important role
⭐mental stress-induced ischemia is associated with poor prognosis and increased risk of mortality
Tako-tsubo cardiomyopathy (TTC)
also known as: Apical ballooning syndrome (ABS)
transient left ventricular (LV) apical ballooning
broken heart syndrome
stress cardiomyopathy
ampulla cardiomyopathy
neurogenic stunning
contrast enhanced ventriculography during diastole and systole
demonstrates apical and midventricular akinesis, with relative sparing of the base of the heart (arrow)
characteristic features:
ECG suggesting acute myocardial infarction
apical ballooning or other major ventricular dysfunction
chest pain/dyspnea, pulmonary edema, cardiogenic shock
short-term recovery of LV function typically fast
long-term prognosis similar to myocardial infarction
but also:
⭐minimal coronary artery disease
⭐often triggered by emotional or physical distress (50% each)
⭐high (supraphysiologic) circulating catecholamines on admission
⭐80% female, mostly post-menopausal
59 year old women - trigger: family member died in a car accident
coronary angiography ejection fraction 10-20% (anterolateral, apical, inferior, and posterobasal akinesia) but only moderate non-obstructive disease in the left anterior descending artery. peak (regulates cardiac muscle contraction) 29.9
history: MI, AF, mitral valve repair, restless leg syndrome, idiopathic joint disease
Episodic Factors: Depression and CVD (Epidemiological Studies)
examples:
major depressive disorder (vital) exhaustion
burnt-out
features:
transient (2 weeks - 2 years)
recurring
INTERHEART study
aim: examine psychosocial factors as risk indicators for non-fatal MI
design:
case-control 11,119 MI and 13,648 controls
52 countries, 262 sites
measures:
stress at work
stress at home
financial s.
stressful life events
depression
loss of control
response options:
never, sometimes, several times, permanent
little to none, moderate, high severe
> REPORTED STRESS DURING THE LAST YEAR & RISK OF MI
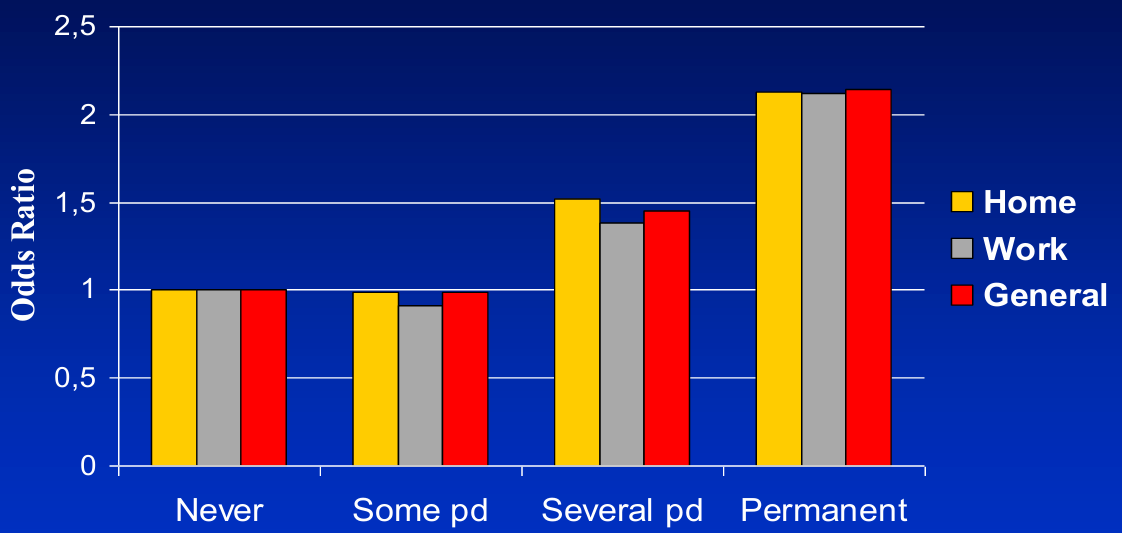
MI higher prevalence of all 4 stress factors
adjusted for age, sex, geographic region, and smoking
CVD ←→ depression (BIDIRECTIONAL)
factors associated with depression onset:
life stressors (particularly in mild-moderate depressive episodes)
negative cognitive bias
maladaptive response to loss (of a significant other or “object”)
genetic vulnerability
previous studies focused on depression as a risk factor for CVD
But, CVD can also increase the likelihood of developing depression:
symptoms (chest pain, shortness of breath, fatigue)
functional capacity (exercise tolerance)
biological consequences (inflammation, CNS changes)
existential questions related to a life-threatening disease (heart structure and function per se do not strongly predict depression)
> DEPRESSION IN PATIENTS WITH CVD
prevalence 15-40%
associated with biological risk factors (e.g., inflammation) and adverse health behaviors (e.g., physical inactivity, poor diet, smoking, alcohol overconsumption, medication non-adherence)
somatic depressive symptoms (fatigue, sleep problems) and irritability more common than typical depressive symptoms (depressed mood & anhedonia)
depression is not a direct byproduct of underlying coronary artery disease or poor heart function
> DEPRESSION & CARDIOVASCULAR EVENTS
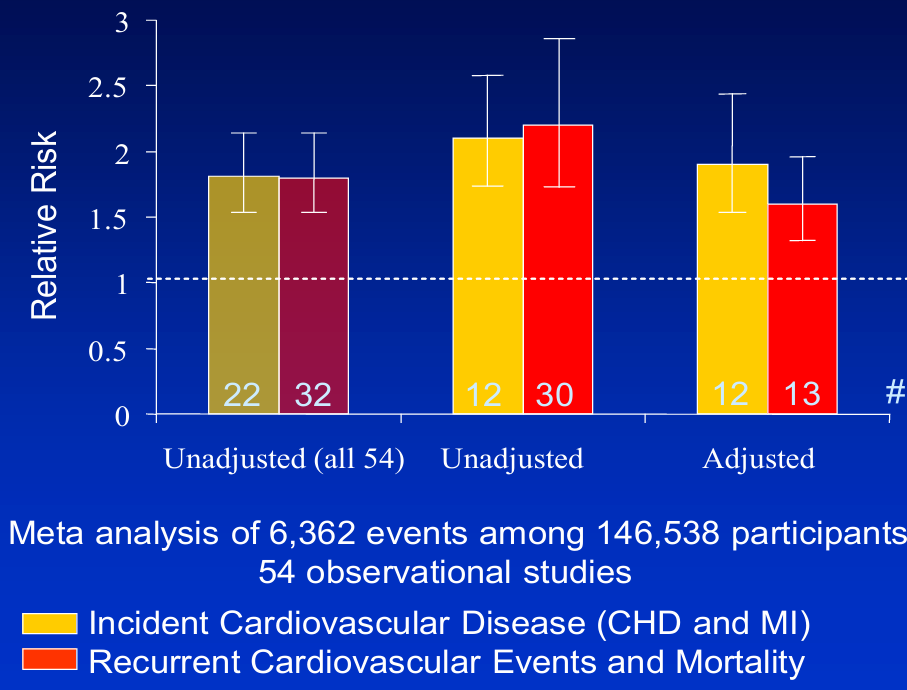
> META-ANALYSIS FOR PREDICTIVE VALUE OF DEPRESSION FOR INCIDENT CARDIOVASCULAR DISEASE (CHD & MI)
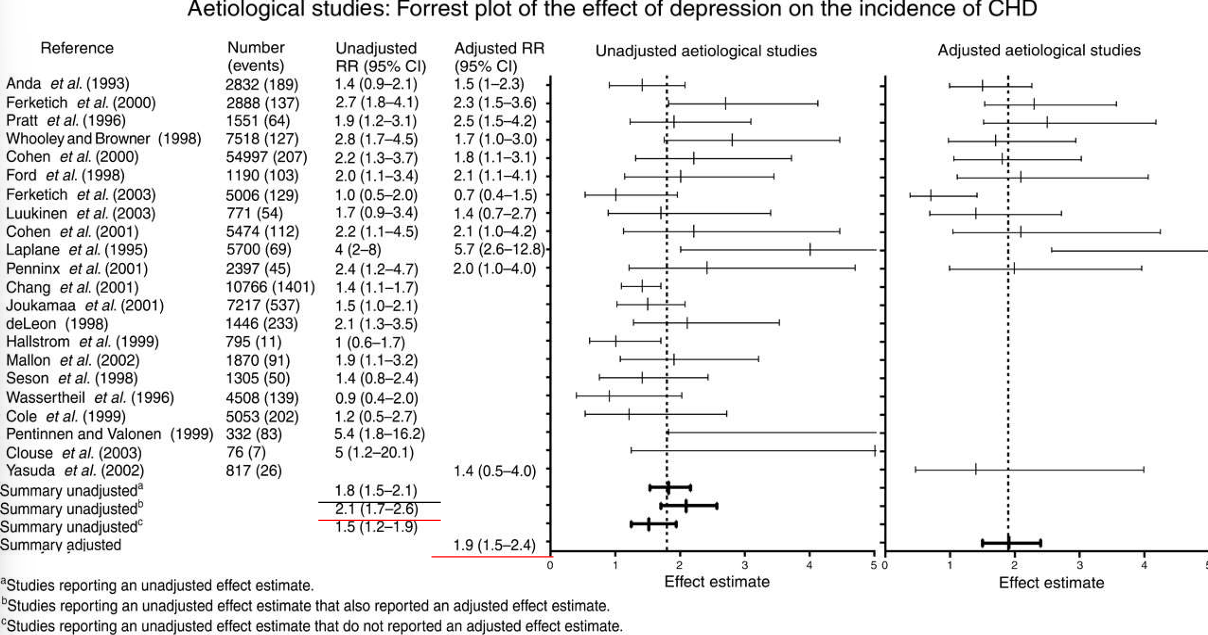
Mechanisms: Inflammation & ANS Dysregulation
central nervous system (SAM, HPA)
autonomic nervous system (parasympathetic & sympathetic)
blood clot formation (coagulation & reduced fibrinolysis)
inflammation and immune dysregulation
Multidisciplinary studies on PNI in cardiovascular disease
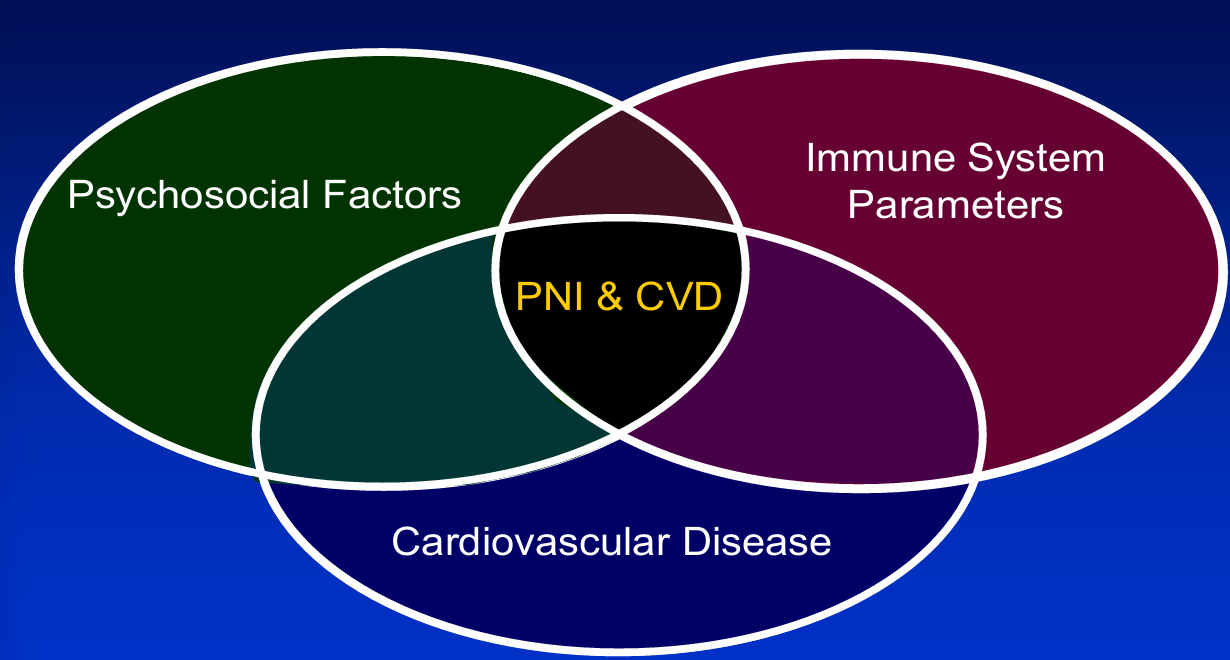
Atherosclerosis and infection: a first clue from Virchow
presence of leukocytes in artherosklerotic lesions → infectious agent?
The most common type of vulnerable plaque
thin-cap fibroatheroma:
lots of inflammatory cells (monocyte/macrophages, t-cells, etc.)
large lipid core
thin fibrous cap
Cardiovascular event-free survival among healthy individual according to baseline CRP
gradual
more CRP protein = more mortality risk
Elevated markers of chronic inflammation in depressive disorders
50 adults with depression
50 adults with clean mental health history
case-matched on age, gender, ethnicity
group differences significant
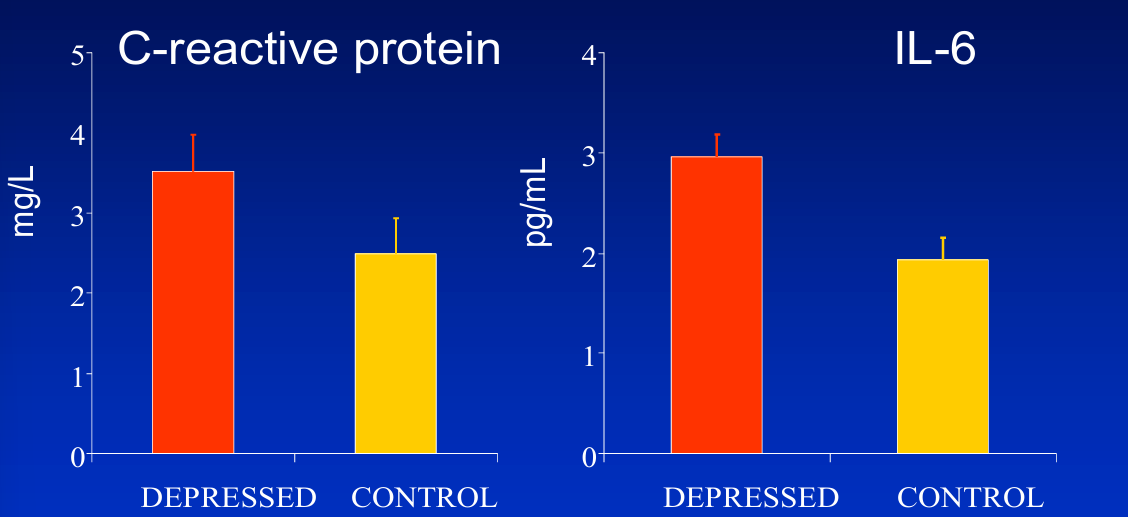
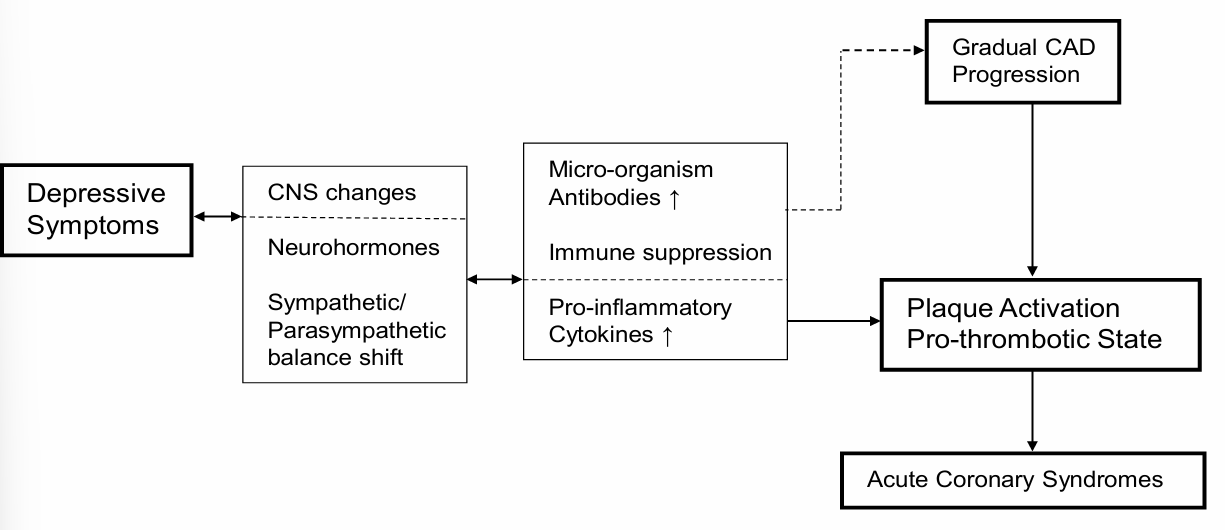
The Biopsychological Approach in Cardiovascular Health
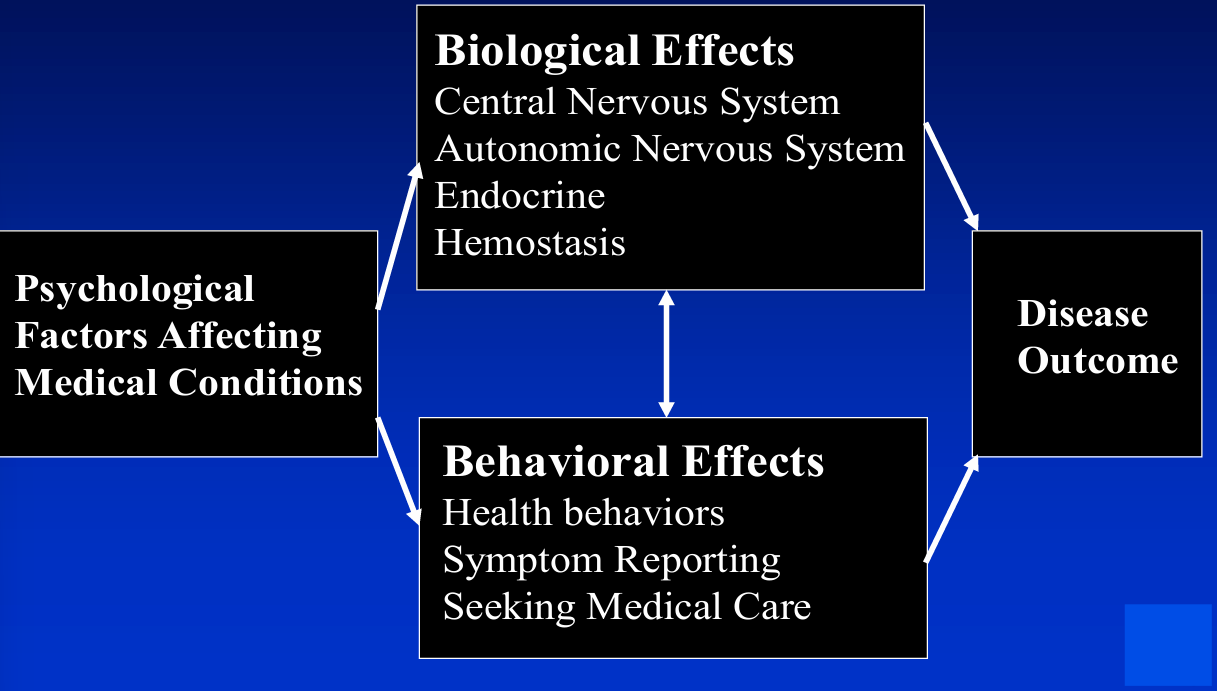
Conclusion
acute mental stress can induce myocardial ischemia in patients with CAD and is a significant precipitant (trigger?) of cardiac events
acute mental stress and depression are associated with elevated inflammation markers
acute stress reactivity elevated in CAD patients
results depression-inflammation inconsistent in CAD patients
effect sizes are small
depression is associated with increased cardiovascular risk
associations of depression with cardiovascular are bi-directional
pathways linking depression to adverse CVD outcomes may require inflammation and ANS dysregulation as co-factors
future studies are needed to:
develop models of mutually reinforcing risk factors: i.e., psychosocial, health behavior, biological processes and disease outcomes
identify high-risk subgroups and targeted interventions based on these dynamic models
L11 - DEPRESSION
Prevalence
mood disorders including MDD: 44 million in Europe
54% of patients recover from MDD within 6 months
81% of patients recover from MDD within 2 years
incidence is increasing over time
Definition & Subtypes
important is the distinction between
depressive symptoms (questionnaires)
depressive disorders (clinical assessment)
depressive disorder
unipolar
bipolar
endogenous: biological, internal, genetic
reactive: exogenous, event/situational related
Causes (Genetics & evolution)
94 possible genes related to depression
why is it taking so long to figure out?
different aspects of depression
Theory of Depression
Stress
disturbed HPA-axis regulation in:
depressive patients
those with latent vulnerability (such as childhood trauma)
those with treatment resistant depression
⭐if a mother experiences stress during pregnancy, it changes the babies HPA - axis which is related to stress⭐
Noradrenergic (monoamines)
two types of monoamines associated with depression:
catacholamines: variants of the amino acid tyrosine
dopamine
norepinephrine⭐
epinephrine
indoleamines/tryptamines: variants of the amino acid tryptophan
serotonin
melatonin
> MONOAMINE THEORY OF DEPRESSION: NORADRENERGIC HYPOTHESIS
» Point of Action 1
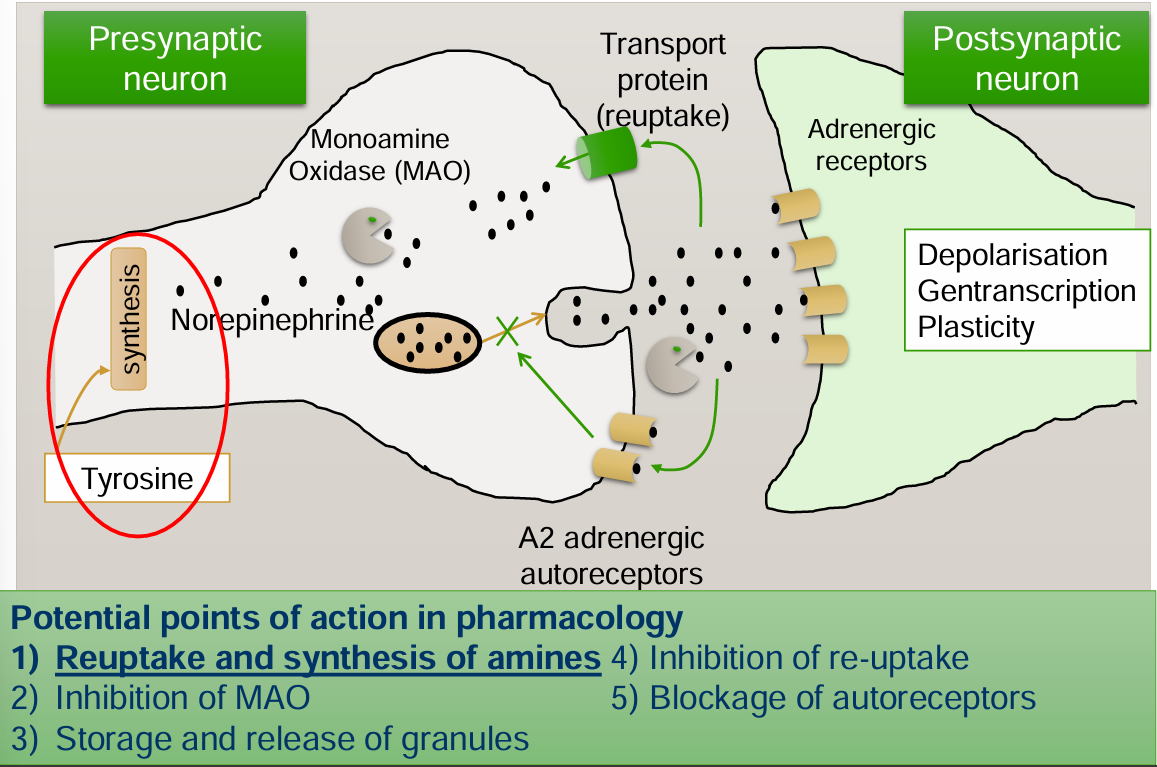
norepinephrine is synthesized from tyrosine
if there is enough norepinephrine they can attach to the adrenergic receptors
α-Methyl-Para-Tyrosine (AMPT): reduces norepinephrine and therefore is a short term depression inducer
» Point of Action 2
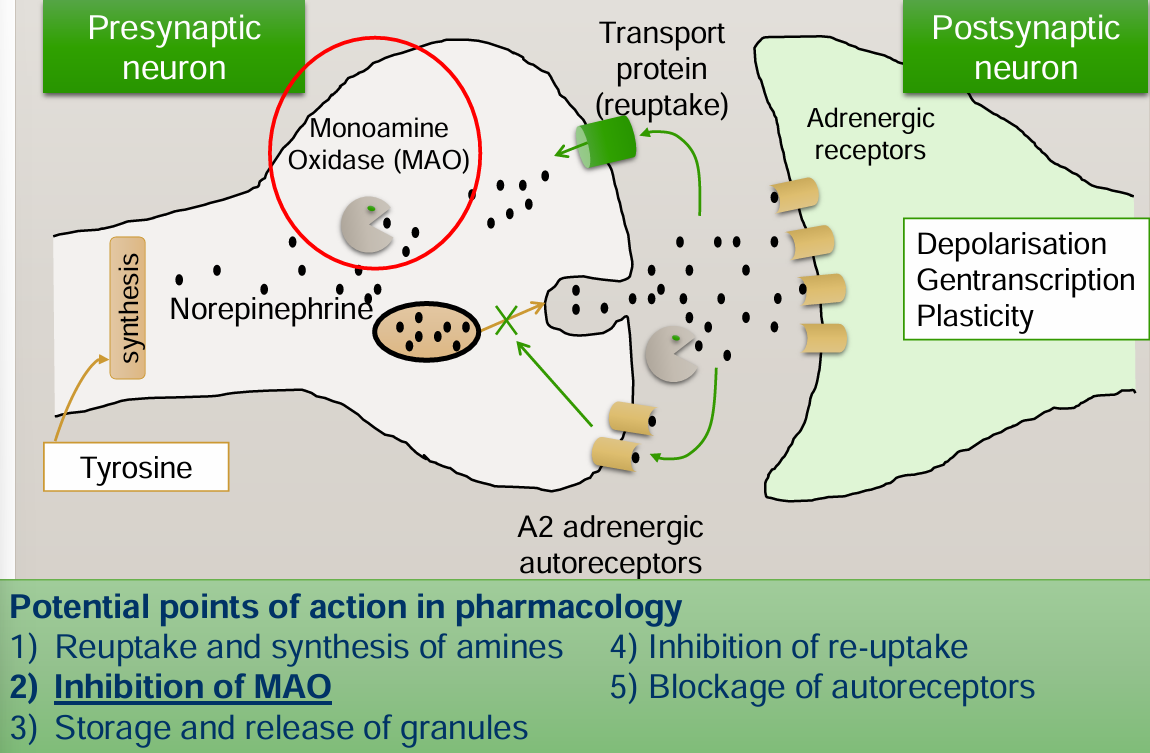
MonoAmine Oxidase (MAO): breaks down norepinephrine → induces depression (👎🏻)
MonoAmine Oxidase Inhibitor (MAOI): inhibits break down of norepinephrine → treatment for depression (👍🏻)
» Point of Action 3
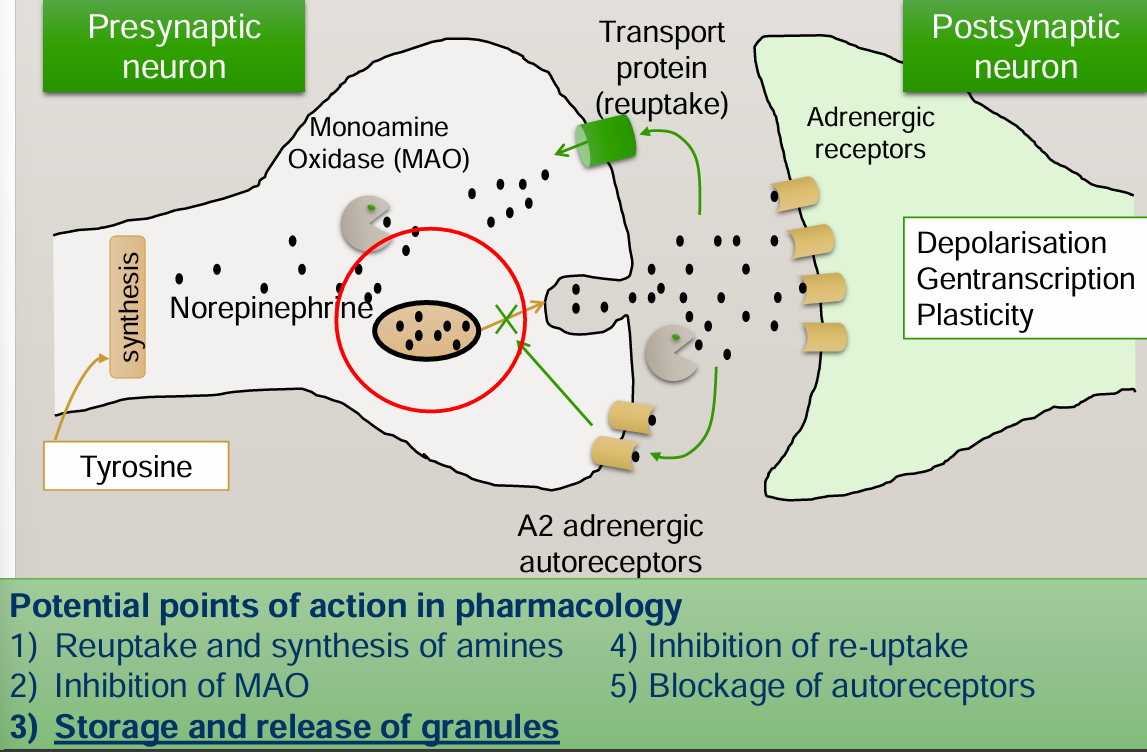
granules: vesicles that store and protect norepinephrine from MAO
reserpine drug: makes granules leaky → MAO eats more norepinephrine → less norepinephrine → depression
» Point of Action 4
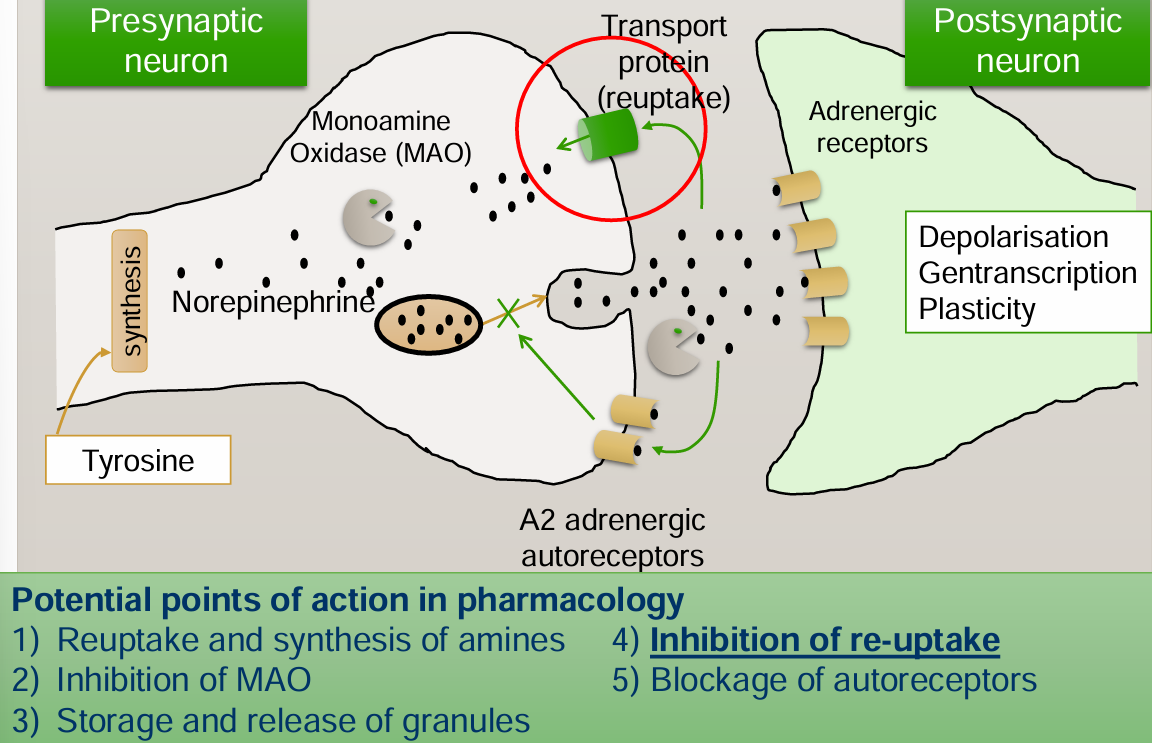
tricyclic antidepressants (TCA) → selective norepinephrine uptake inhibitor (SNRI)
» Point of Action 5
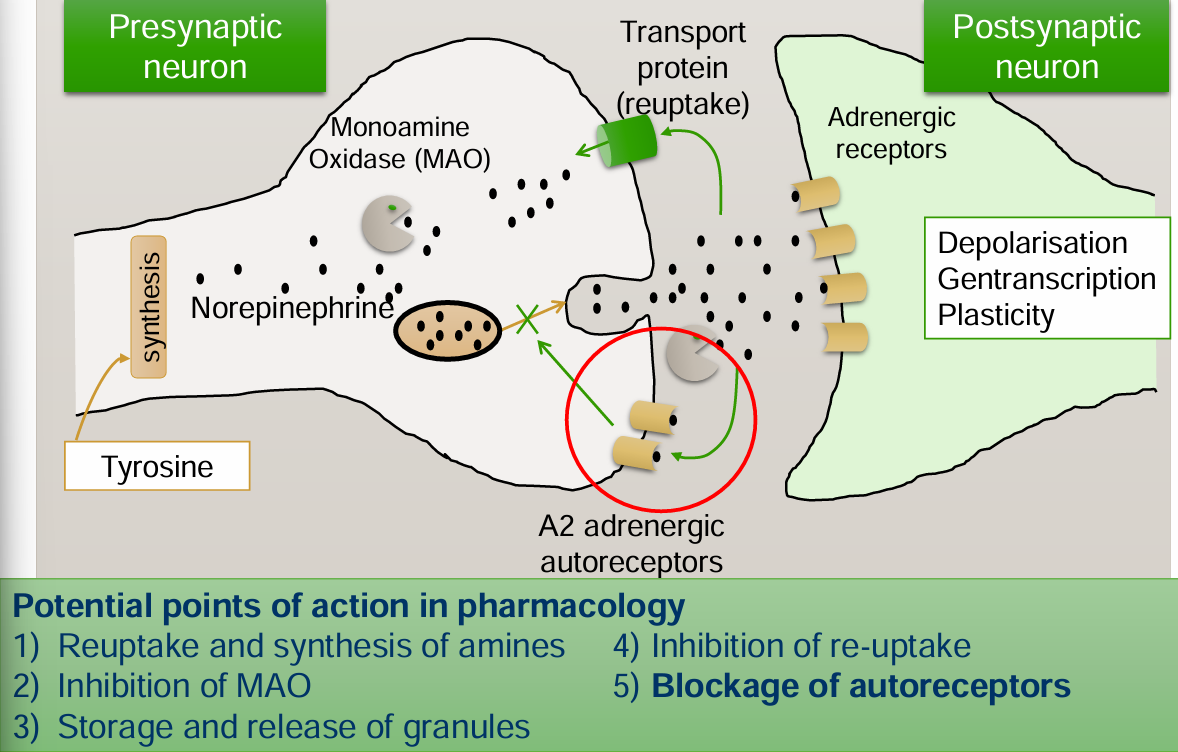
autoreceptors: signals that there should be less norepinephrine when norepinephrine attaches to them
Serotonin (monoamines)
two types of monoamines associated with depression:
catacholamines: variants of the amino acid tyrosine
dopamine
norepinephrine
epinephrine
indoleamines/tryptamines: variants of the amino acid tryptophan
serotonin⭐
melatonin
> SEROTONINE HYPOTHESIS
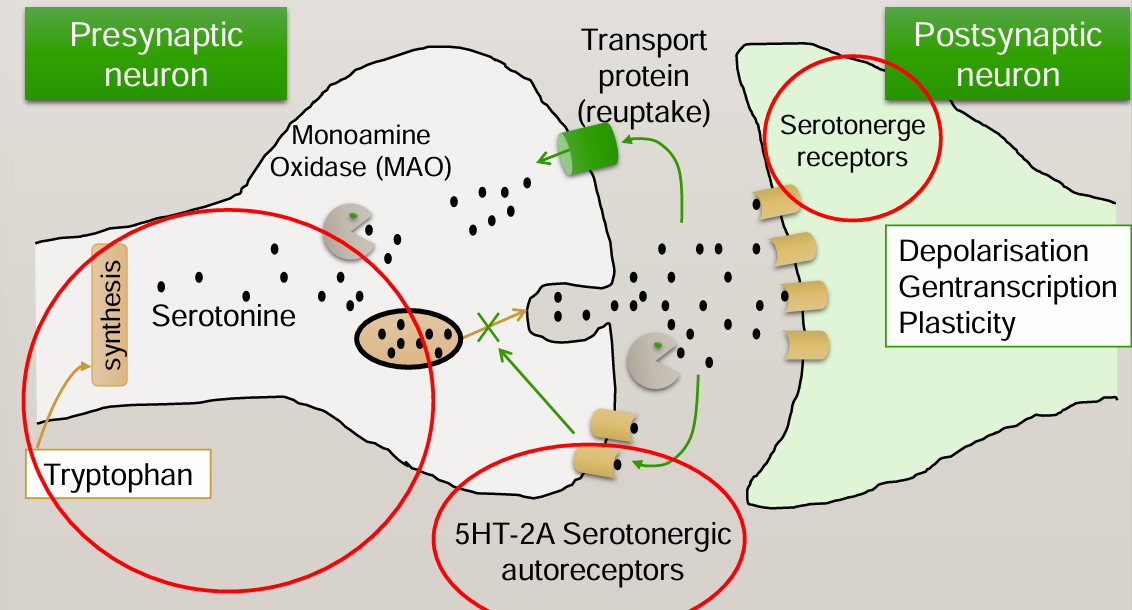
only differences with noradrenergic hypothesis are the red circles
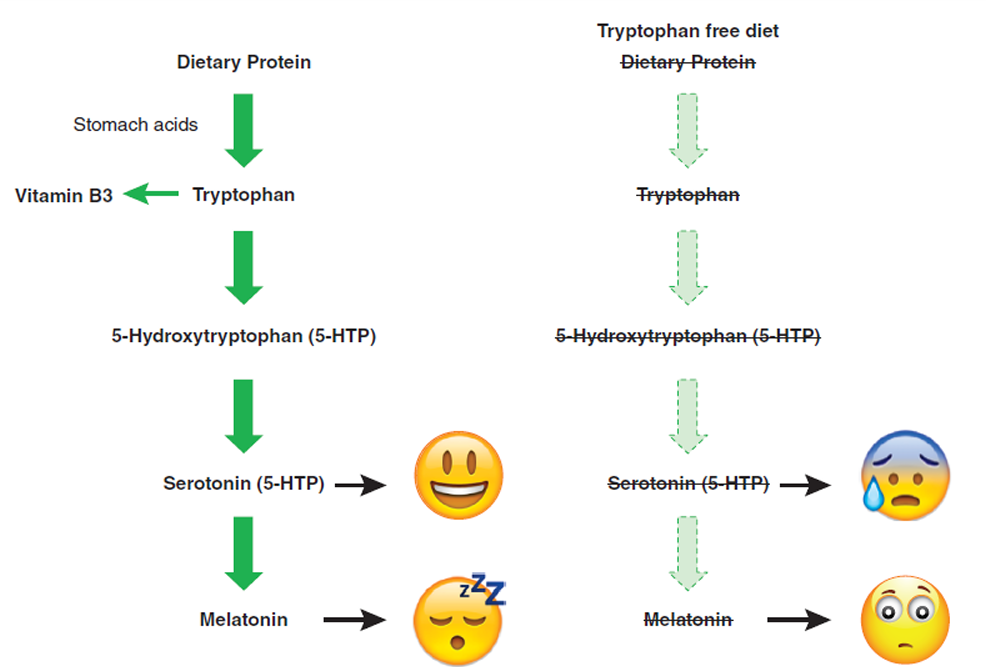
Inflammation
Cytokines: e.g. IL-1, IL-6, TNF-α, INF-α
The brain has cytokine-receptors and when pro inflammatory levels are elevated you develop ‘sickness behavior’: that is…
Apathy
Irritable
Fatigue and
disturbed sleep
Increased pain sensitivity
Social isolation
Anorexia
→ Sickness behavior has overlap with depression
> EVIDENCE
creating inflammation or administration of cytokines leads to symptoms of depression
cytokine-induced depression responds to anti-depressants
depressive patients show inflammatory activation
severity of symptoms is related to blood cytokine levels
Neuroplasticity
increases in monoamines:
leads to an increase in neuroplasticity
via the expression of growth factor (Brain-Derived Neurotrophic Factor BDNF → fertilizer for neurons)
> EVIDENCE
depression lowers BDNF in specific brain regions (humans and animals)
risk factors for depression (stress and somatic illness) also decrease BDNF
recovery from depression (by antidepressants, ECT, physical activity) increases BDNF
it is mechanically plausible, as decreases in BDNF levels cause:
neuroplasticity decrease
increased responsiveness of stress hormones
injection of BDNF into the brain improves depression
> OTHER MECHANISMS INVOLVED
gut-brain axis
contributor to immune dysregulation
HPA-axis, increases in cortisol
Kynurenine pathway
HPA-axis regulation (breaks down tryptophan)
reinforced by chronic inflammation
Treatments
Pharmaceutical
> TRYCICLIC ANTIDEPRESSANTS (TCAs)
“dirty drugs”: drugs with non-specific effects
besides reuptake inhibition of norepinephrine it also impacts unrelated processes because it binds to other receptors as well
higher number of side effects than SSRIs and in case of an overdose cardiac complications
> SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs)
are selective, but equally effective compared to TCAs
less side effects and lower risk in case of overdoses
better with other medications than TCAs
indication not only for depression: OCD, eating disorders, PMS
» Side effects
multifunctionality: has a selective effect on the same process, but this process has different functions in different cells
→ 5HT (serotonin) in the digestive system
Non-pharmaceutical
ECT (electroconvulsive therapy)
physical activity
light therapy
Saint John’s wort herb
Depression & Somatic
Co-occurrence
approximately 40-60% of depressed patients have a somatic condition
depression reduces medical treatment effectivity and increases mortality
a very high number (85% mild depression and 60% severe depression) depressed patients are not recognized by doctors
reversed: many somatic complaints of depressed patients are not taken seriously by their doctor
Depressogenic aspects of somatic conditions
psychosocial
dealing with loss and trauma
being limited with respect to self care, work, social and family life
the underpredictability or life threatening aspects of an illness
undergoing painful and intervening treatments
psychobiologic
neurological damage
effects of hormonal disturbance
effects of medications
> SOMATIC CONDITIONS WITH ELEVATED CYTOKINE LEVELS
autoimmune diseases:
rheumatoid arthritis (joints)
Crohn’s disease (inflammatory bowel disease)
multiple sclerosis (myelin)
systematic lupus erythematous (non-specific, all cells)
chronical viral and bacterial infections
being obese
diabetes mellitus
cardiovascular disease
Depression - medication
⭐25% of depression in the elderly is the effect of medication use⭐
pharmaceutical treatment for hypertension
beta blockers (e.g. propandol)
calcium receptor blockers
hormone treatment
glucocorticoids (reducing inflammation, e.g. prednisone)
alpha-interferon (INF-a ), for treating hepatitis C: 33% develops a depression <12 weeks
L12 - STRESS & ANXIETY
Cathy, 4 years:
mother of two
has rheumatoid arthritis (RA) since 31
RA has been stable, yet a few months ago she experienced more symptoms
currently getting a divorce
John, 24 years:
has eczema since he was 10
symptoms fluctuate over time
current outbreak
in a few days he has an exam
what do Cathy and John have in common?
→ STRESS
Why Stress Has Physiological Effects
the cognitive representation of a threat causes a “fight-or-flight” response
followed by a cascade of biological events:
starting in the brain
inducing peripheral stress responses such as increases in heart rate, blood pressure, and stress hormones (cortisol)
The reactivity hypothesis
classical theoretical understanding: stressful events are accompanied by physiological responses, which, if frequent and intense, may cause bodily harm
however, mostly weak and inconsistent support
does not account for prolonged physiological activity
From reactivity to prolonged activation model
prolonged activation model: physiological activity during stressful events (stress reactivity) will only become a critical health threat when it is sustained long after these events, or when physiological activity is already present in anticipation of these events, sometimes even far before them
Prolonged activation model
worry, rumination, perseverative thinking
= anticipation + slow recovery
The role of continuing stressful thoughts: perseverative cognition
to explain prolonged activity, the perseverative cognition hypothesis is formulated. Two core arguments:
recovery of the autonomic nervous system after a physical stressor (running upstairs) is much faster than from most psychological stressors
human brain looks backwards and forwards: ruminating about the past and worrying about the future
unique to humans
humans make mental representations of stressors long before, and long after these events occur or are believed to occur → perseverative cognition (PC)
Physiological & psychological profile of perseverative cognition
PHYSIOLOGICAL PROFILE | PSYCHOLOICAL PROFILE |
decreased heart rate variability | hyper vigilance to threat and failure to habituate to harmless stimuli |
decreased prefrontal cortex activity | impaired cognitive functioning, delayed responding |
increased amygdala activity | lack of inhibitory behavior |
altered immune function | denial and avoidant coping style |
increased blood pressure | increased neuroticism |
excess and prolonged cortisol responsivity | decreased conscientiousness |
pupil dilation | lack of perceived control |
greater levels of anxiety depression, and hostility |
Input of stress response
internal stressors (vagus nerve)
somatosensory stressors (skin and muscles)
painful stressors
emotional stressors
cognitive input
Complex Network of Signaling
Sympathetic nervous system (SNS)
flight or flight → via vagus nerve:
dilate pupil
inhibit salivation
increase heartbeat
relax airways
inhibit activity of stomach
stimulate release of glucose, inhibit gallbladder
inhibit activity of intestines
secrete epinephrine and norepinephrine
relax bladder
promote ejaculation and vaginal contraction
Endocrine system
> HPA - AXIS
hypothalamus —CRH→ anterior pituitary —ACTH→ adrenal cortex → CORTISOL!!!!
grow and appetite, metabolism, glucose storage, learning and memory
> SCHEMATIC HPA - AXIS
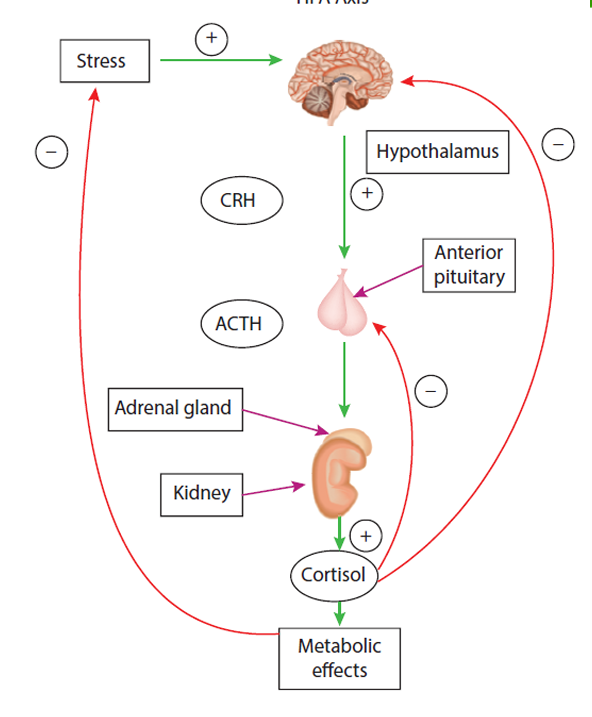
Immune system
> EFFECT OF STRESS HORMONES
cortisol:
stimulates lymphocyte maturation
regulates inflammatory responses
promotes catecholamine release
✅physiological response when life is actually in danger✅
❌when survival is not threatened it can lead to a poor immune functioning❌
Homeostasis vs Allostasis
homeostasis: if you are in north pole in a bikini your body has to work a little bit harder for maintaining 36C
allostasis: every thursday you drink, so your liver has to work harder in thursdays then it starts to remember that and your liver gets activated before u start drinking → anticipation, learning memory, prediction
Maladaptive or Adaptive
does stress has an effect on our health?
And if so, how?
Why is the duration of a stressor important when it comes to the effect of the stressor on one’s health?
real danger:
upregulates (+) natural immunity, rises in the number of neutrophils and NK cells → preparation for injury
chronic stress:
downregulates (-)
→ stress can negatively impact health through changes in immune functioning
Clinical relevance
> WOUND HEALING
a model for studying the immune function, as the immune system is involved in wound healing
» example
11 dental students
3.5mm biopsy wound was made inside their mouth
once wounds were made during vacation, once before exams
→ wounds took longer to heal during exams than summer
exam = prolonged stress (not acute)
how are positive psychological factors related to health?
→ social support and optimism!!!!
> SOCIAL SUPPORT
73 HIV seropositive gay men were assessed for concealment of being gay, social support, depression and CD4 amount
CD4 → predictor of HIV:
low CD4: bad
high CD4: good
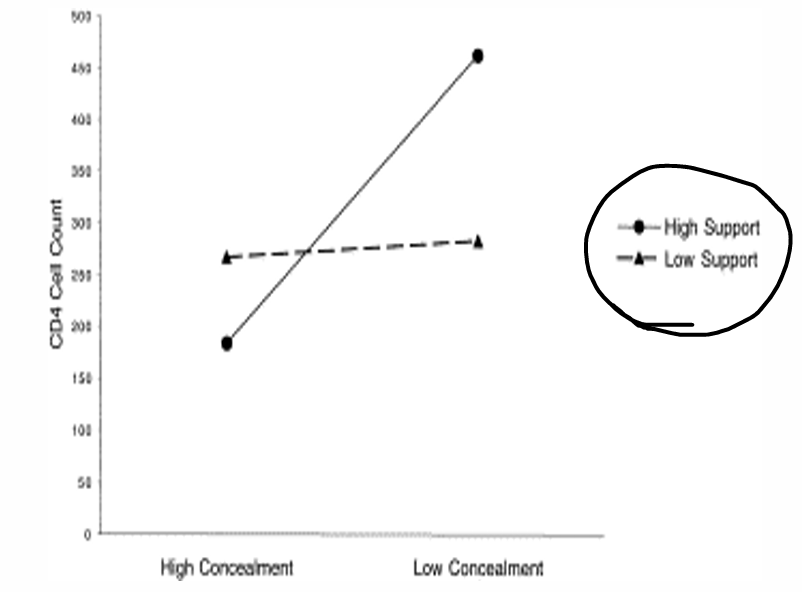
interaction effect:
low support: no effect
high support: matters if you are open or not
> OPTIMISM
positively correlated to cellular immunity in controllable, brief and straightforward situations
inversely correlated with cellular immunity in uncontrollable, chronic and complex aituations
the later may derive from optimists’ over-engagement in tasks, even if it’s complex, they cannot “give up”
> SUMMARY
studies show that stress can have negative effects on our health (wound healing, colds, infections)
studies show that some psychological factors can be protective (social support and optimism)
Anxiety - (mal)adaptive?
can be maladaptive and adaptive
can be evolutionarily useful - being alert
easily startled, hypersensitive to noise → response to threat easily evoked
insomnia → constant alertness
restlessness, increased heart rate → body prepared for action
attention diverted to cues related to threat → notice threats earlier
ambiguous information interpreted as threatening → reduced chance of making a false-negative assessment and missing a possible threat
ambiguity averse → avoidance of situations where threat is uncertain
GABA
GABA-A Receptor
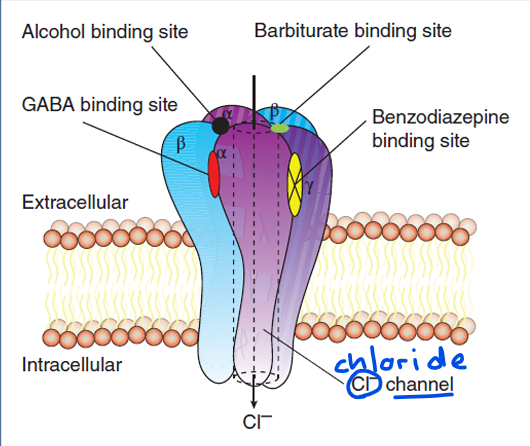
Anxiety and GABA
Anxiety = too much activity
GABA leads to:
CL- transportation into the cell
making the inside of the cell more negative or hyperpolarized
therefore less likely to fire an action potential
→ less activity = less anxiety
Indirect impact at the GABA receptor via the benzodiazepine binding site, by various drugs: effects can be positive (agonist) facilitating activity or negative (inverse agonist) inhibiting activity
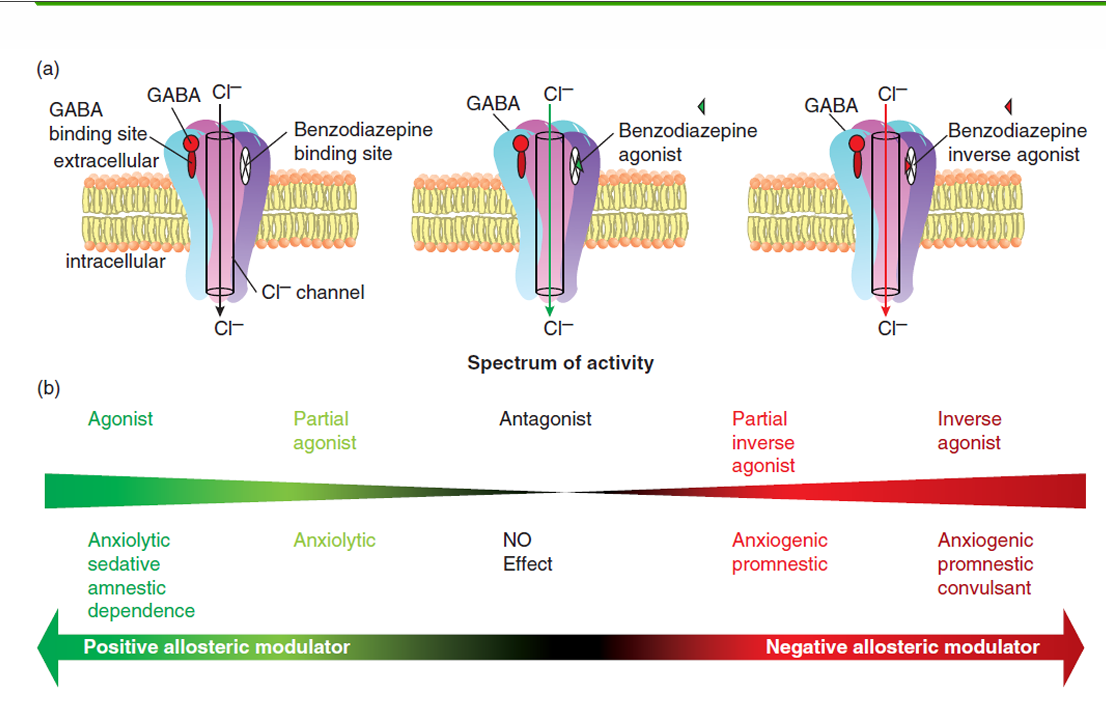
⭐barbiturates: don’t need GABA they can pretend to be GABA
→ on its own reduce the firing
⭐benzodiazepines : need GABA to be present in order to have an effect
Agonist: benzodiazepine + GABA
Benzodiazepine + GABA enhance inflow of CL
Cell is more negative, action potential is less likely
Inhibition of neuron, anxiety is reduced
→ agonist
Antagonist: flumazenil + GABA
Blocking the benzodiazepine binding site by flumazenil
Solely GABA binding will result in CL- induction (less then with benzodiazepines together)
There is no change in CL- inflow, no effect on anxiety
→ antagonist
⭐given for ODing → cancels out benzos⭐
Inverse agonist
Another drug attaches to the benzodiazepine binding site
GABA binding together with this inverse agonist results in a reduction in CL- induction
Cell is less negative, action potential is more likely
Less inhibition of neuron, anxiety is INDUCED
Response for each category
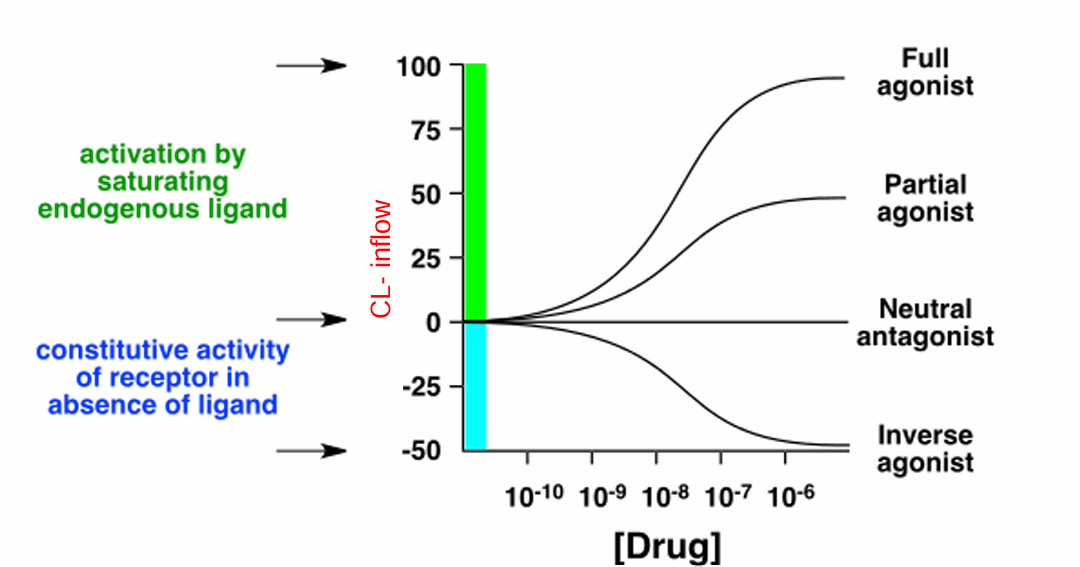
Barbiturates & benzodiazepines
⭐barbiturates are not given anymore because they do not have an antagonist (but benzos do)
Serotonin
(-) depression —— anxiety (+)
⭐given the involvement of serotonin in both disorders a partial agonist when treating anxiety is beneficial
Noradrenaline
Alpha-2 adrenoceptors:
blockage: increases release of noradrenaline (reduces depression)
stimulation: decreases release of noradrenaline (increases depression)
→ can do both