Lecture 4: Alteration of Immune System
Hypersensitivity:
hypersensitivity- the inappropriate or altered immunologic response to an antigen that results in disease or damage to the host
allergy- a collection of conditions caused by inappropriate or exaggerated reactions of the immune system to a variety of substances
many common diseases such as asthma and hay fever are caused by allergic reactions to substances
the most common allergens:
airborne: pollens, spores from molds, dust mites, animal dander
foods: dairy products, eggs, fish, cereals, some fruits
autoimmunity- disturbance in the immunologic tolerance of self-antigens
numerous disorders such as rheumatoid arthritis and insulin dependent diabetes mellitus are caused by a reaction of the individuals immune system against the organ or tissue of their own body
alloimmunity- immune reaction to tissues of another individual
hypersensitivity can have any of 4 dif immune mechanisms:
type 1- aka anaphylactic or immediate hypersensitivity, IgE mediated
type 2- tissue specific reactions
type 3- immune complex mediated
type 4- cell mediated
immediate hypersensitivity reactions
anaphylaxis
delayed hypersensitivity reactions
type 1 hypersensitivity:
allergens (from the environment) provoke the immune system to produce specific antibody (ige that present in the surface of the skin and lining of respiratory and digestive systems)
when the allergen is encountered for the second time, it binds to ige and causes mast cells to release chemicals (ex. histamine) that causes:
blood vessels to widen
fluid to leak into tissue
muscles to go into spasm
manifestations:
itching
urticaria- aka hives
conjunctivitis- inflammation of conjunctiva, causing redness, discomfort, and discharge from the affected eye
rhinitis- inflammation of the mucus membrane of the nasal cavity
hypotension
bronchospasm- temporary narrowing of bronchi
dysrhythmias- disturbance of heart rhythms
gi cramps and malabsorption
genetic predisposition:
ppl w a family history of allergies tend to have:
elevated levels of ige
inherited general hyper responsiveness
inherited antigen specific response
lower number of t suppressor cells also play a role
tests:
food challenges
skin tests
laboratory tests
treatment:
avoid allergen
avoid exposure to environmental pollutant
desensitization
injection of allergen in low and increasing doses can reduce sensitivity
injection of allergens tend to increase igg which acts as blocking antibody and remove antigen before it can interact with mast cells
desensitization sometimes may trigger generalized or system anaphylaxis
(there’s a picture here that shows what happens but its super unclear, check textbook)
type 2 hypersensitivity:
tissue specific
antibodies bind to antigens on cell surface (ex. surface of rbcs) and lead to possible destruction of the cell
it is tissue specific bc specific cells or tissues (tissue specific antigens) are the target of the immune response
can be responsible for certain autoimmune disorders and hemolysis
5 mechanisms
cell is destroyed by antibodies and complement (complement??)
cell destruction through phagocytosis
soluble antigen may enter the circulation and deposit on tissues
antibody dependent cell mediated cytotoxicity
causes target cell malfunction
(there’s a picture here that shows what happens but its super unclear, check textbook) DISREGARD ^ CHECK NOTABILITY
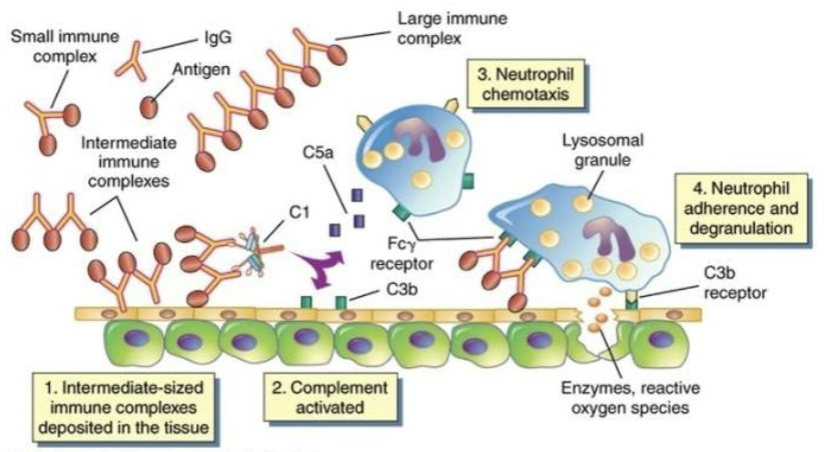
type 3 hypersensitivity:
immune complex (antibody bound to antigen) lodge in various tissues and activate further immune system response therefore it is known as immune complex mediated
antigen-antibody complexes are formed in the circulation and are later deposited in vessel walls (mediate the formation (of?) microthrombi and cause endothelial damage) or extravascular tissues
not organ specific
immune complex clearance
immune complex clearance is a process directed at removing immune complexes from the body (im assuming next part is how theyre cleared based on size; maybe not, research seems to say maybe not?)
large - macrophages
small - renal clearance
intermediate - deposit in tissues
disorders that result from type 3 hypersensitivity:
immune complex disease ex. immune complex glomerulonephritis (damage to glomerulus due to deposition of immune complexes)
serum sickness- damage from phagocytosis of immune complex deposited in capillaries following large transfusions of foreign serum (ex. horse antidiptheria serum)
arthus reaction- local production and deposition of antibodies against the synovial membrane
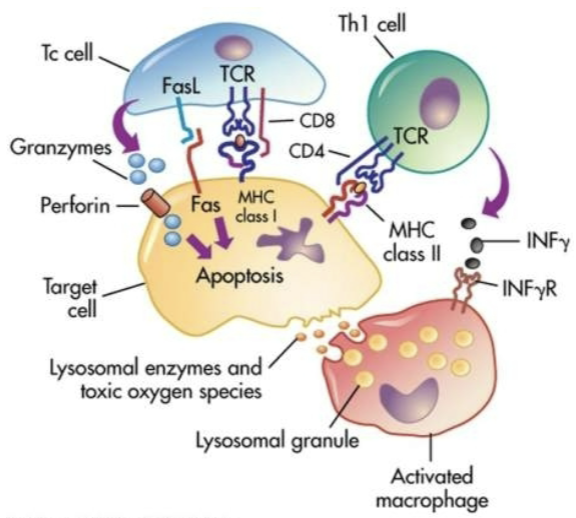
type 4 hypersensitivity:
aka delayed type hypersensitivity
does not involve antibodies
cytotoxic t lymphocytes or lymphokine producing th1 cells
direct killing by tc or recruitment of phagocytic cells by th1 cells (yeah theres too many abbreviations for me to make sense of this or to compare any research to this info)
th cells- t helper cells; tc- t cells
ex. acute graft reaction, skin test for tb, contact allergic reactions, and some autoimmune diseases
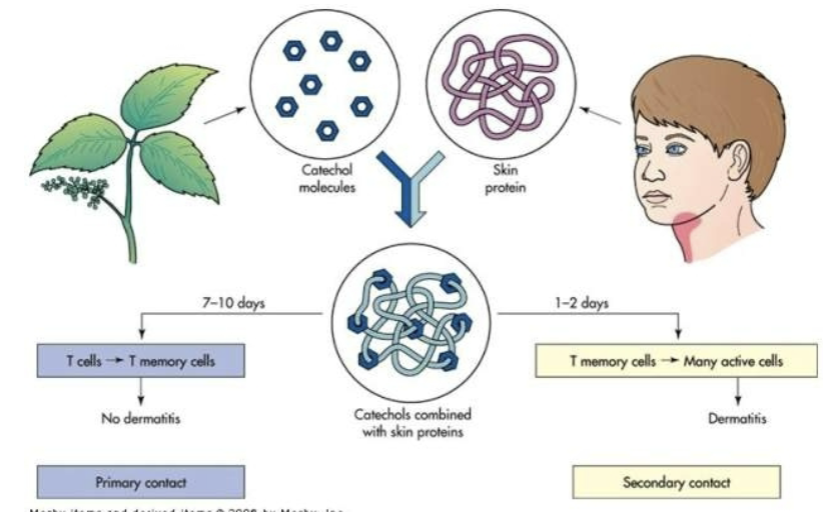
allergy:
environmental antigens that cause atypical immunologic responses in genetically predisposed individuals
pollens, molds and fungi, foods, animals, etc
allergen is contained within a particle too large to be phagocytosed or is protected by a nonallergenic coat
original insult is apparent (pretty sure this means the original instance or cause is clear but not sure/not sure whether instance or cause/if its cause, how is it known?)
autoimmunity:
breakdown of tolerance
antibody or t cells against self antigens and recognizes self antigens as foreign
basically the breakdown is that the mechanisms that maintain the immune systems tolerance to self antigens fail (and so the immune system loses its tolerance to self antigens)
sequestered antigen
self antigen not normally seen by the immune system
infectious disease
molecular mimicry (self antigens are close enough to foreign antigens that an overactive immune system mistakes them)
neoantigen
haptens (a small molecule that when bound to a bigger one can produce an immune response) become immunogenic (able to produce an immune response) when they bind to host proteins
neoantigen- a new protein that forms on cancer cells when certain mutations occur in tumor dna. (cancer cells doesnt count for autoimmunity purposes)
forbidden clone
during differentiation, lymphocytes produce receptor(s?) that react with self antigens
these immune cells should have been destroyed (bc of their autoimmune properties) but they managed to survive (hence ‘forbidden’)
ineffective peripheral tolerance
defects in regulatory cells
the cells that are supposed to make sure the immune cells arent autoimmune cells dont work properly
original insult
genetic factors
alloimmunity:
immune system reacts w antigens on the tissue of other genetically dissimilar members of the same species
transient neonatal alloimmunity
fetus expresses parental antigens not found in the mother
transplant rejection and transfusion reactions
autoimmune examples:
systemic lupus erythematosus (sle)
chronic multisystem inflammatory disease
autoantibodies against nucleic acids, erythrocytes, coagulation proteins, phospholipids, lymphocytes, platelets, etc.
deposition of circulating immune complexes containing antibody against host dna
more common in females
clinical manifestations
arthralgias (general joint pain not from inflammation) or arthritis (joint pain from inflammation) (90% of individuals)
vasculitis (inflammation of blood vessels) and rash (70-80%)
renal disease (40-50%)
hematologic changes (50%)
cardiovascular disease (30-50%)
eleven common findings
serial or simultaneous presence of at least 4 indicates sle
facial rash (malar rash), discoid rash, photosensitivity, oral or nasopharyngeal ulcers, nonerosive arthritis, serositis (acute inflammation in pleurae or pericardium), renal disorder, neurological disorder, hematologic disorders, immunologic disorders, and presence of antinuclear antibodies (ana)
graft rejection:
transplant rejection is classified according to time
hyperacute
immediate and rare
preexisting antibody to the antigens of the graft
acute
cell mediated immune response against unmatched hla antigens
chronic
months or years
inflammatory damage to endothelial cells of vessels due to weak cell mediated reaction against minor hla antigens
transfusion reactions:
antibodies against blood groups antigens
abo system
2 major carbohydrate antigens
a and b (co dominant)
individuals have naturally occuring antibodies to the a and b antigens they lack
anti a and anti b antibody production is induced by similar antigens on naturally occurring bacteria in the intestinal tract
antibodies are usually of the igm class
o blood type is the universal donor
ab blood type is the universal recipient
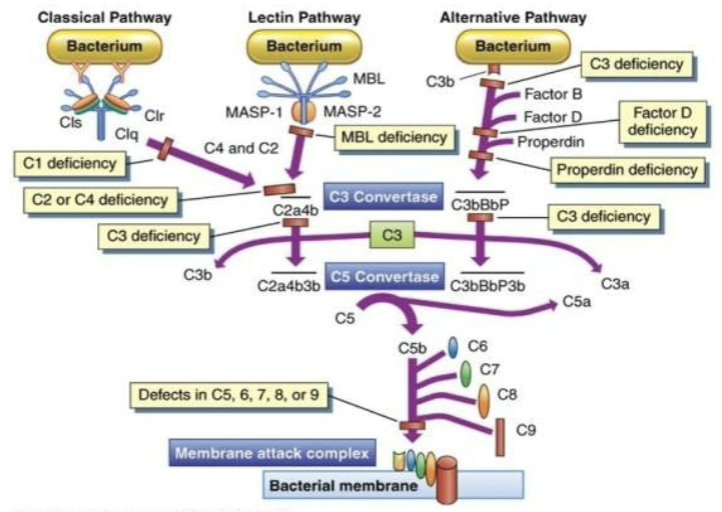
immune deficiencies:
failure of immune mechanisms of self defense
primary (congential) immunodeficiency
genetic anomaly
secondary (acquired) immunodeficiency
caused by another illness
more common
clinical presentation
development of unusual or recurrent, severe infections
t cell deficiencies
viral, fungal, yeast, and atypical microorganisms
b cell and phagocyte deficiencies
microorganisms requiring opsonization
complement deficiencies
primary immune deficiencies:
most are the result of a single gene defect
5 groups
b lymphocyte deficiencies
t lymphocyte deficiencies
combined t and b cell deficiencies
complement defects
phagocyte defects
secondary deficiencies:
also referred to as acquired deficiencies
far more common than primary deficiencies
causes
normal physiology conditions
refers to conditions that are normal like pregnancy or aging etc.
psychological stress
dietary insufficiencies
malignancies
physical trauma
medical treatments
infections
acquired immunodeficiency syndrome (aids)
acquired immunodeficiency syndrome (aids):
syndrome caused by a viral disease
human immunodeficiency virus (hiv)
depletes the bodys th cells
incidence
worldwide- 5 million/yr
U.S.- about 31,000/yr
400,000 currently living w aids
effective antiviral therapies have made aids a chronic disease
(as opposed to fatal)
epidemiology
blood borne pathogen
increasing faster in women than men
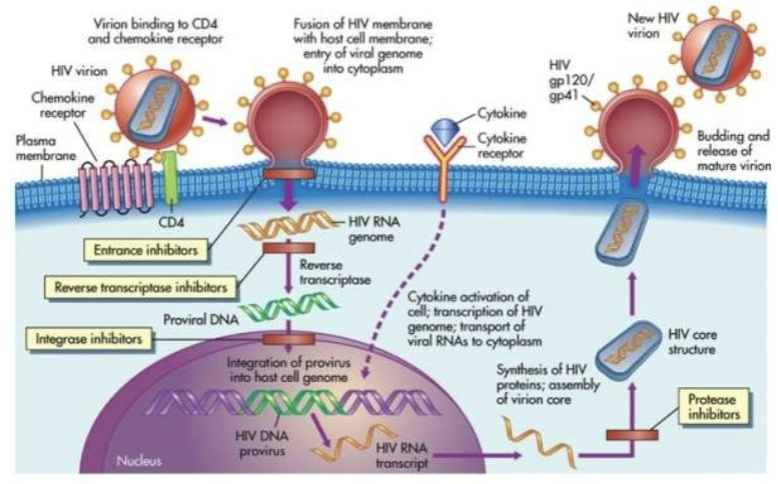
pathogenesis
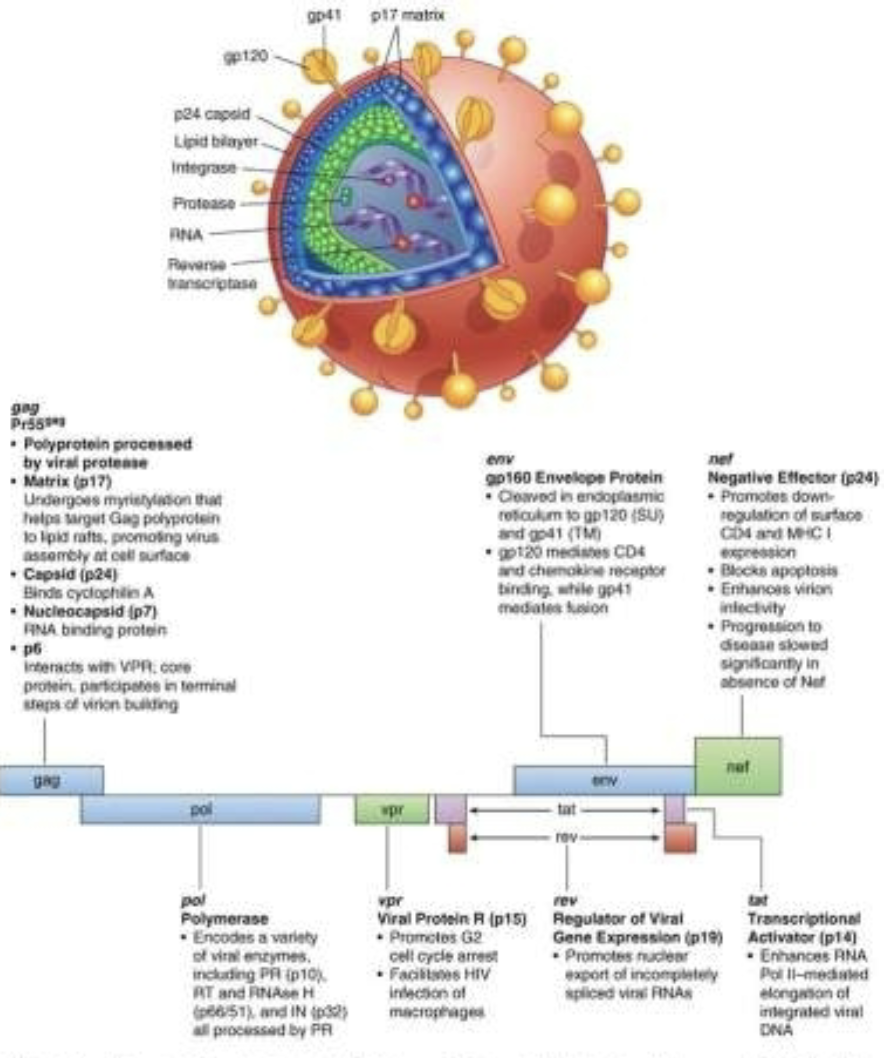
retrovirus
genetic information is in the form of rna
contains reverse transcriptase to convert rna into double stranded dna
integrase (used to insert the viral dna into the host dna)
human immunodeficiency virus (hiv):
structure
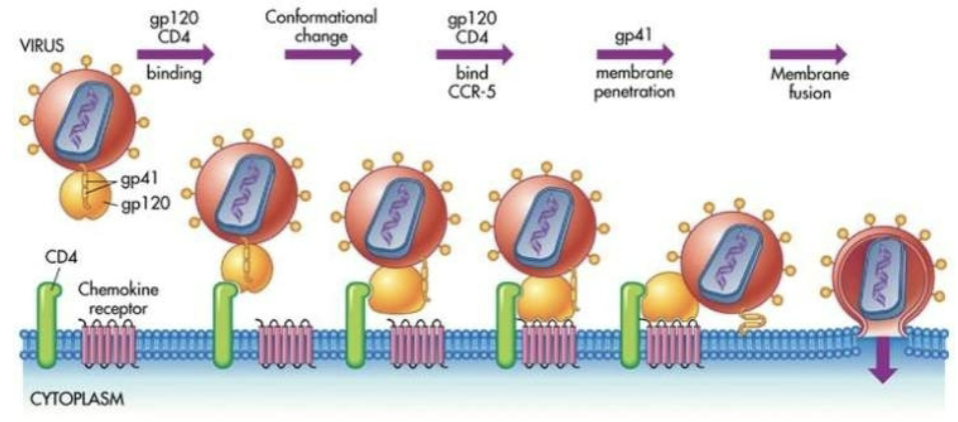
gp120 protein binds to the cd4 molecule found primarily on the surface of helper t cells
cd4+th cells (the + was in superscript, idk if its supposed to note something or be ‘and)
typically 800 to 1000 cells/mm3
reverses cd4/cd8 ratio
co receptors
cxcr4 and ccr5
strains can be selective for these receptors; influences the tropism of the target cells
tropism- the turning of all or part of an organism in a particular direction in response to an external stimulus
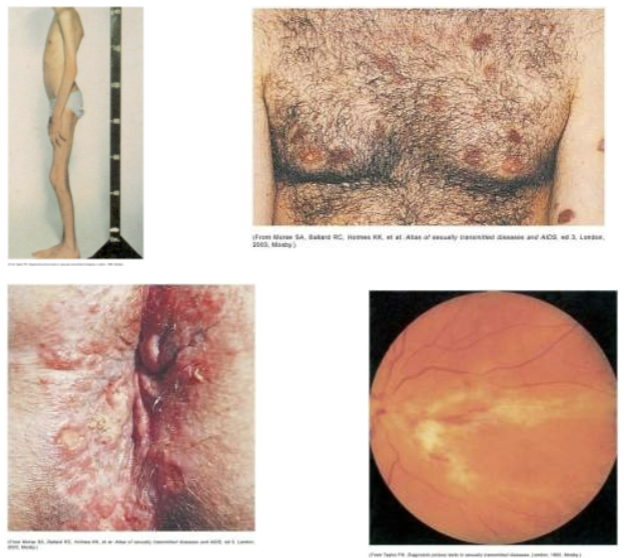
clinical manifestations
serologically negative, serologically positive but asymptomatic, early stages of hiv, or aids
window period
th cells <200 cells/mm³
diagnosis of aids is made in association with various clinical conditions
atypical or opportunistic infections, and cancer
treatments and prevention
highly active antiretroviral therapy (haart)
reverse transcriptase inhibitors
protease inhibitors
new drugs
entrance inhibitors
integrase inhibitors
vaccine development
evaluation of immunity:
complete blood count (cbc) w a differential
subpopulations of lymphocytes
quantitative determination of immunoglobulins
subpopulations of immunoglobulins
assay for total complement
skin tests
treatment for immunodeficiencies:
gamma-globulin therapy
transplantation or transfusion
treatment w soluble immune mediators
gene therapy
microorganism/human relationship:
mutual relationship
normal flora
relationship can be breached by injury
they can leave their normal sites and cause infection elsewhere
opportunistic microorganisms
stages of infection:
colonization
invasion
multiplication
spread
classes of infectious microorganisms:
virus
chlamydia
rickettsia
mycoplasma
bacteria
fungi
protozoa
helminths
clinical manifestations of infectious disease:
variable depending on the pathogen
directly caused by the pathogen or indirectly caused by its products
fever
resetting the hypothalamus
exogenous pyrogens
endogenous pyrogens
countermeasures:
vaccines
induction of long lasting protective immune responses that will not result in disease in a healthy recipient
attenuated organism
killed organisms
recombinant viral protein
bacterial antigens
toxins
antimicrobials
inhibit synthesis of cell wall
damage cytoplasmic membrane
alter metabolism of nucleic acids
inhibit protein synthesis
modify energy metabolism