13_-_Darwinian_medicine
Lecture Notes
Not about letting natural selection run it’s course.
Does not contradict with traditional medicine, they can work in tandem with each other.
Darwinian medicine works cooperatively with allelopathic medicine. WHY you get disease, not HOW you get disease like traditional medicine.
Antibiotic resistance, type 2 diabetes, cancer, obesity, autoimmune diseases, are the results of not considering evolutionary medicine.
Three main principles:
Symptoms as adaptations: (Ex: Inflammation, morning sickness, fever, pain) Treating symptoms often hurts you more because those symptoms are adaptations.
Pain: draws attention to harmful stimuli, reduces re injury, motivates learning. Painkillers extenuate the healing process.
Inflammation: Immune response that directs immune cells towards a site of damage
Morning sickness: Protects a fetus from being poisoned due to the varied diet of humans. Thalidomide caused flipper babies because it suppressed this adaptation.
Fever: an immune response to increase the temperature of the body and heighten the immune response.
Evolutionary arms race: Losing battle with bacteria because they evolve so much faster than we do. This is why resistant strains of bacteria are so much more proliferant.
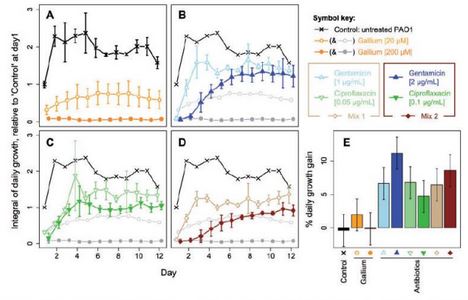
Evolutionary solution: Attack cooperative adaptations of bacteria → Biofilm communities.
Bacteria need Siderophore to bind Iron
Only certain bacteria can capture Siderophore so they are dealing with teh cost and benefit
Other non-producing ones get only the benefit.
SOLUTION: Inject Gallium, Siderophores bind gallium instead of Iron. Bacteria can’t use Gallium.
Those producing cells are getting no benefit + cost. So they are being selected against.
What’s left are the nonproductive ones, which can’t support a biofilm community.
Same with cancer: Select against angiogenic cancer cells using endostatins because it inhibits angiogenic factors, this kills angiogenic cells as well as the regular cells.
3. Evolutionary mismatches: Adaptive traits are good in one environment, bad in another. (Obesity, sea turtles)
Obesity: We are adapted to avoid negative energy balances, meaning we are adapted to conserve energy as much as possible. This adaptation has carried on to the modern day. Adapatation to crave fat and sugar to ensure adequate nutrition for themselves and their offspring during times when food was sacrce. We have this strong adaptation because we needed that strong motivation because getting food during hunter-gatherer times was really hard. Change in accessibility over time made it so those calorie rich-foods are not as hard to get, but we still have that stong motivation and desire to each those high calorie foods which causes us to overeat during modern times of higher accessibility. It used to be impossible to acquire too many calories, now it is impossible not to. This is why it’s easy to put on fat but not muscle.
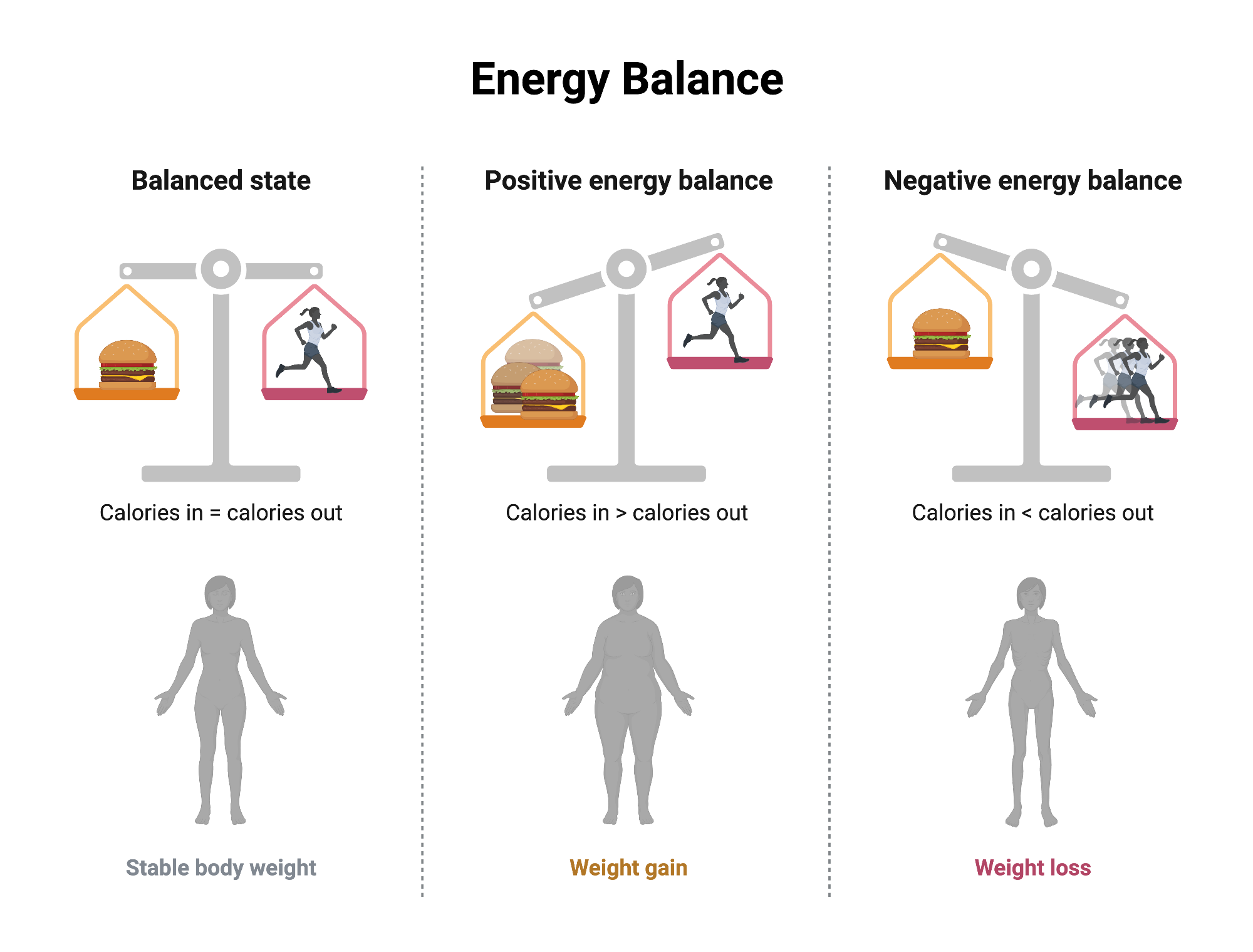
Type 1 diabetes: We are adapted to avoid negative energy balances and conserve energy. We want to have a slow metabolism so that we do not burn away all of the fat too quickly because food is scarce. So a slower metabolism will be selected for. This adaptation is present as a mutation in the TCF7L2 gene that causes you to underproduce insulin so that you don’t consume resources too quickly and conserve them. This is now maladaptive and the reason why people have type 1 diabetes because the environemnt we are currently living in does not call for extreme methods of conserving energy.
Environmental development of the immune system: The immune system develops from exposure. Oversterilization in the modern environment takes that capacity to develop away becuase there is no exposure to learn from, thus leading to autoimmune diseases and allergies which is basically the immune system being underdeveloped and not being able to recognize what is good and what is bad.
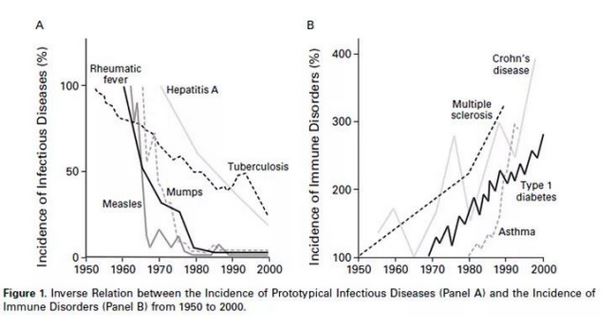
Helminthes (intestinal paarsites) cause a lower incidence of immune disorders.
Hygiene hypothesis: Lower incidence of infection in early childhood is responsible for the increase in moderm immune system related disorders.
Immune system coevolved with “old friends”
Immune system does not develop normally without “old friends”
Innovations in hygiene/santiation reduces exposure to old friends and leads to modern immune system related diseases such as MS, T1 diabetes, allergies, inflammatory intestinal diseases.
More autoimmune diseases in urban areas than rural areas.
BUG questions
How does Darwinian medicine differ from traditional medical approaches?
Traditional medicine focuses on the immediate cause and treatment of disease. HOW?
Darwinian medicine emphasizes understanding the evolutionary reasons behind diseases and adaptations. WHY?
What are the three main themes of Darwinian medicine? Briefly explain each.
Symptoms are adaptations
Evolutionary arms race → evolve one adaptations, another one evolve something else
Evolutionary mismatches → evolutionary traits become maladaptive in another environment
How would have evolutionary thinking averted the thalidomide disaster?
Evolutionary thinking emphasizes understanding the biological and developmental processes during pregnancy.
By considering the evolutionary role of certain medications during critical developmental periods, the potential risks could have been assessed more thoroughly.
Recognizing morning sickness as an evolutionary trait that has been evolved for a purpose because it serves an important reason. Emphasis on the why as opposed to the how.
Awareness of the variations in embryonic development among species might have led to more cautious testing of thalidomide before its approval.
Recognizing that drugs can have different effects on humans due to evolutionary adaptations could have prompted more rigorous safety standards.
The concept of teratogenic effects, or the impact of substances on developing embryos, could have been better integrated into the drug approval process, highlighting the need for extensive studies on fetal exposure.
Overall, an evolutionary perspective could have promoted a more precautionary approach to drug development and testing, potentially preventing the birth defects associated with thalidomide use during pregnancy.
Is morning sickness a non-functional disease or is it an adaptation? Provide evidence to explain your response.
Morning sickness is often viewed as an adaptation rather than a non-functional disease. Evidence supporting this includes:
Evolutionary Perspective: From an evolutionary standpoint, morning sickness may serve protective functions during early pregnancy by helping women avoid foods that could be harmful to the developing fetus.
Nutritional Avoidance: Pregnant women experiencing morning sickness often develop aversions to certain foods, particularly those that are rich in toxins or pathogens, which could pose risks to the embryo.
Reduced Miscarriage Rates: Studies have shown that women who experience morning sickness tend to have lower rates of miscarriage, suggesting that this symptom may contribute to better reproductive outcomes.
Hormonal Changes: The onset of morning sickness correlates with rising levels of pregnancy hormones like human chorionic gonadotropin (hCG), indicating a physiological response that may be beneficial for pregnancy health.
What is an issue with simply trying to exterminate pathogens like we do pests? What is an example of this?
Attempting to exterminate pathogens like pests can lead to several issues:
Resistance Development: Pathogens may evolve resistance to treatments, making them harder to eliminate over time.
Ecosystem Disruption: Just as the extermination of a single pest can disrupt local ecosystems, targeting pathogens may also lead to unintended consequences within the human microbiome and broader environmental health.
Loss of Beneficial Microbes: Some pathogens may have relationships with beneficial microbes that support immune system function; exterminating pathogens may inadvertently harm these beneficial species.
Example: The overuse of antibiotics to combat bacterial infections has led to the emergence of antibiotic-resistant strains, such as MRSA (Methicillin-resistant Staphylococcus aureus). This has made common infections harder to treat and raises concerns about public health.
How can we kill pathogens without invoking a strong response to selection?
Targeting Pathogen Vulnerabilities: We can focus on specific aspects of pathogen biology that are less likely to lead to resistance. For instance, exploiting essential metabolic pathways unique to the pathogen may minimize the chance of resistance development.
Target non-essential traits (Gallium)
Target multiple pathways simultaneously
Combination Therapy: Using multiple agents that target different pathways or aspects of the pathogens can reduce the likelihood of resistance, as it becomes more difficult for pathogens to adapt to multiple treatments simultaneously.
Periodic Drug Rotation: Alternating between different types of treatments can prevent pathogens from becoming resistant to any one agent by changing the selective pressure they experience.
Vaccination: Promoting immune recognition of pathogens through vaccination decreases the necessity for aggressive treatments and allows the immune system to manage infections without applying strong selection pressure that might lead to resistance.
How did researchers demonstrate that bacteria didn’t evolve resistance to Gallium? How was this demonstrated with endostatin and cancer?
Observations were made under controlled conditions with continuous exposure to Gallium.
Gallium disrupts iron metabolism without dirupting it entirely.
In contrast, endostatin, used in cancer treatment, often leads to the development of resistance as cancer cells adapt to treatment pressure.
Endostatin's effectiveness relies on disrupting tumor blood supply rather than directly targeting cancer cells.
The differing mechanisms of Gallium and endostatin highlight how resistance patterns can vary based on the biological context of treatment.
What is the “hygiene hypothesis”? What are the three main lines of evidence that support it?
The "hygiene hypothesis" suggests that a lack of early childhood exposure to infectious agents, microorganisms, and parasites increases susceptibility to allergic diseases by suppressing the natural development of the immune system.
Immune system co-evolved with other species which are old friends
The immune system does not develop properly without exposure to old friends
Innovations in hygiene reduce exposure to old friends
This leads to emergence of modern immune system diseases
Three Main Lines of Evidence Supporting the Hygiene Hypothesis:
Rise of autoimmune conditions are correlated withe cleaner conditions
Kids on farms
Exposure to microbes in early life.
Rural vs Urban Environments: Studies show that children from rural areas, who are more exposed to various pathogens and animals, have lower rates of allergies compared to those raised in urban environments with better hygiene practices.
Family Size and Birth Order: Evidence indicates that children from larger families or those who are born later in birth order are less likely to develop allergies, possibly due to increased exposure to infections from siblings.
Exposure to Pets: Growing up in households with pets is associated with reduced allergy and asthma rates, suggesting that exposure to animal dander and microbes may help develop a more robust immune system.
Allergies are clearly a mistake, but why are allergic reactions so strong?
Allergic reactions are often characterized by an exaggerated immune response to harmless substances. The strength of these reactions can be attributed to several factors:
Allergic responses evolved as strong immune defenses against pathogens, which are now maladaptive
Immune System Overactivity: The immune system may misidentify harmless substances (allergens) as threats, leading to an overreaction and an excessive release of histamines and other chemicals that cause symptoms.
Genetic Predisposition: Individuals with a family history of allergies may be more prone to stronger allergic reactions due to inherited genetic factors that influence immune response.
Environmental Exposures: Early exposure to allergens may prime the immune system, leading to heightened sensitivity and stronger reactions upon subsequent exposure.
Inflammatory Mediators: Allergic reactions are mediated by inflammatory substances released by immune cells, leading to symptoms like swelling, redness, and itching that can manifest strongly due to increased sensitivity.
Cytokine Release: The presence of cytokines, which are signaling proteins in the immune response, can amplify the intensity of reactions, further contributing to the severity of symptoms.
What is the notion of “old friends” in Darwinian Medicine. Explain an example of how reuniting humans with an “old friend” led to the reduction of a current disease.
The concept of "old friends" suggests that certain microorganisms (parasites and bacteria) co-evolved with humans and are essential for immune system functioning.
Modern lifestyles have reduced exposure to these organisms, particularly in industrialized countries, increasing rates of autoimmune and allergic diseases.
Example: Helminth therapy involves intentionally infecting patients with specific helminths (parasitic worms).
This therapy aims to restore immune balance.
It has been linked to reductions in autoimmune conditions and allergies, such as inflammatory bowel disease, highlighting the importance of re-establishing these evolutionary relationships.
Why does low gut microbial diversity influence the likelihood of acquiring allergies? What is one tested way parents can reduce the chance of their offspring acquiring allergies?
Low gut microbial diversity can increase the likelihood of developing allergies.
A diverse gut microbiome helps regulate immune responses and fend off allergic reactions.
Reduced diversity can lead to an underdeveloped immune system that misidentifies harmless substances as threats, triggering allergic responses. This is due to lack of exposure causing less learning of what’s bad and what’s good.
One tested method for parents to help reduce the chance of their children acquiring allergies is to expose them to a variety of microbes during early childhood through activities such as spending time in nature or owning pets, breastfeeding, having a vaginal birth.
This exposure can help develop a more robust and balanced immune system, decreasing allergy risk.
Why is your immune system so closely tied to the gut (why is so much of the immune system located there)?
The immune system is closely tied to the gut due to several reasons:
High Density of Immune Cells: A significant portion of the body's immune cells resides in the gut-associated lymphoid tissue (GALT), which plays a crucial role in bowel immunity and helps to respond to antigens encountered in the gastrointestinal tract.
First Line of Defense: The gut acts as a barrier to pathogens, with immune cells ready to respond to any pathogens that penetrate this barrier. It is where we face the greatest exposure to pathogens and teh external environment.
Microbiome Interactions: The gut contains a diverse microbiome that interacts with the immune system, helping to train immune responses and maintain an appropriate balance between tolerance and activation, preventing unnecessary inflammatory responses.
Nutrient Absorption: The gut is essential for nutrient absorption, which is crucial for maintaining immune functions, as nutrients play vital roles in the production and function of immune cells.
Constant Antigen Exposure: The gut is continuously exposed to various antigens from food and microbes, requiring sophisticated immune responses to discriminate between harmless and harmful substances, which maintains immune homeostasis.
The gut needs to maintain a balance between bad bacteria and keeping good microbes.
Why would the immune system goof and attack insulin producing cells in the pancreas instead of the pathogenic bacteria they were meant for?
The immune system may mistakenly attack insulin-producing cells in the pancreas due to several factors:
Molecular Mimicry: Some pathogens might have antigens that resemble those found on the insulin-producing cells, leading to the immune system mistakenly targeting both. The beta cells produce a heat-shock stress protein that resembles pathogenic bacteria, which is why the body attacks it. The TB vaccine allows the immune system to differentiate between pathogens and the pancreas cells.
Genetic Predisposition: Certain genetic factors can increase the likelihood of autoimmune reactions. If an individual's immune system is genetically programmed to be more aggressive, it may misidentify healthy cells as threats.
Environmental Triggers: Infections or other environmental factors can initiate autoimmune responses, especially in genetically predisposed individuals, causing the immune system to lose its ability to differentiate between self and non-self.
Immune Regulation Failure: The immune system has regulatory mechanisms to prevent attacking the body’s own cells. If these mechanisms fail, it may lead to attacks on insulin-producing cells, contributing to conditions like type 1 diabetes.
Why would the Tuberculosis vaccine (BCG vaccine) be useful for preventing the onset of diabetes?
The BCG vaccine may modulate immune responses.
It may reduce inflammation, a key factor in type 1 diabetes development.
Diabetes is associated with an autoimmune attack on insulin producing cells.
Pathogens stimulates the immune system in a way that helps retrain the immune system to distinguish between good cells and bad cells.
Can potentially prevent autoimmune attacks on insulin-producing beta cells in the pancreas.
Associated with lower incidence of diabetes in some studies.
Enhances regulatory immune responses, improving metabolic health.
Further research is needed to understand the underlying mechanisms.
What seems to be a cause of autism that is gaining some scientific support?
Recent research suggests that there may be a link between maternal immune responses during pregnancy and the development of autism in children. Some potential causes gaining scientific support include:
Maternal Infections: Infections during pregnancy can trigger immune responses that may affect fetal brain development.
Inflammation: Elevated levels of inflammatory markers in pregnant women have been associated with increased risk of autism in their offspring.
Expansiveness of gut microbiota plays a role in children developing autism.
Environmental Factors: Exposure to environmental toxins or chemicals during pregnancy may also play a role in the development of autism.
Genetic Factors: Genetic predispositions combined with environmental influences contribute to the likelihood of autism development.
Would you suspect that children growing up with dogs would develop fewer allergies? Why?
Growing up with dogs may lead to a lower incidence of allergies in children. This can be attributed to several factors:
Microbial Exposure: Dogs carry a variety of microorganisms that can help bolster a child's immune system by exposing them to diverse microbial environments. This exposure promotes immune system development and regulation, potentially reducing allergic reactions.
Early Immune Training: Exposure to animal dander and other environmental allergens during early childhood can 'train' the immune system to differentiate between harmful pathogens and harmless substances, preventing overreactions to common allergens.
Hygiene Hypothesis: The hygiene hypothesis suggests that reduced early exposure to pathogens, microorganisms, and parasites can lead to increased susceptibility to allergic diseases. Families with dogs may provide a more balanced exposure to these allergens, helping develop a robust immune response.
What effect does varying the methodology of pacifier cleaning have on the health of the baby
The methodology of pacifier cleaning can significantly impact the health of a baby. Different cleaning practices influence the exposure to microbes and allergens, which can shape the developing immune system. Here are some considerations:
Over-Cleaning: Excessive sterilization of pacifiers can lead to an overly clean environment, reducing exposure to beneficial microbes. This lack of exposure may increase the risk of allergic diseases by failing to train the immune system adequately.
Natural Exposure: Allowing pacifiers to be exposed to natural environments (though still ensuring they are clean) can introduce a variety of microorganisms that support immune development. This is aligned with the hygiene hypothesis, which posits that exposure to a diverse microbial environment strengthens immune function.
Cleaning Methods: Methods that use water and mild soap are generally recommended over harsh chemical disinfectants that may leave residues harmful to infants.
Parental Hygiene Practices: When parents clean their own mouths or simply rinse pacifiers with saliva instead of using sterilizers, it may expose infants to beneficial oral microbiota, fostering a diverse gut microbiome.
Cultural Practices: In some cultures, it is common for parents to clean pacifiers by sucking on them. These practices can contribute to microbial exposure that helps in developing a more resilient immune response.
Overall, why is being raised in an environment that is too clean bad for you?
Being raised in an environment that is too clean can be detrimental to health for several reasons:
Reduced Microbial Exposure: Limited contact with a diverse range of microbes during early development can hinder the immune system's ability to differentiate between harmful pathogens and harmless substances, potentially leading to increased allergies and autoimmune diseases.
Immune System Development: The immune system requires regular stimulation from various microbes to develop properly. An overly sterile environment may prevent this necessary exposure, leading to weakened immune responses.
Hygiene Hypothesis: This hypothesis posits that a lack of exposure to infectious agents can lead to a rise in allergic diseases. Children in overly clean environments may lack the immune training that occurs through exposure to different microorganisms.
Mental Health Effects: Growing up in a too clean environment can also affect mental health by limiting social interactions and play that expose children to different environments and experiences.
Balance and Resilience: A certain level of exposure to dirt and microbes is vital for building a healthy, resilient immune system. Without this balance, individuals may develop sensitivities and other health issues later in life.
Important facts
Immune development for babies: Birth canal, breast milk, mother’s skin, vagincal delivery, environment
In areas where you’re more likely to get intestinal worms, you’re less likely to get autoimmune disorders