TUT-P week 3 preparation
Chapter 19, section 6 “Pulmonary rehabilitation“
Pulmonary rehabilitation = PT assessment + therapy
Therapies = exercise training, education, behavior change, improve physical and psychological aspects, improve adherence and promote healthy behavior
Treatment can change depending on the disease specific aspects
PT assessment outcomes and goals
Exercise prescription and training
Self management education
Nutritional intervention
Psychological support
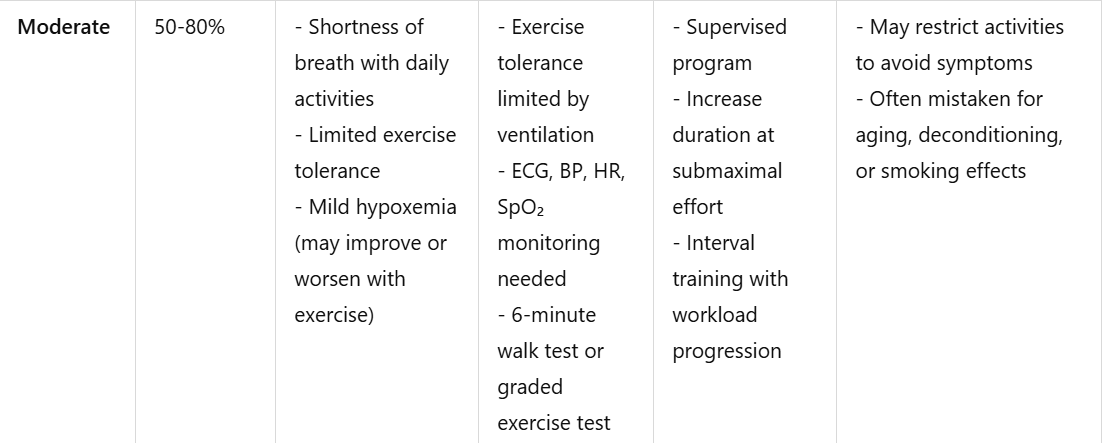
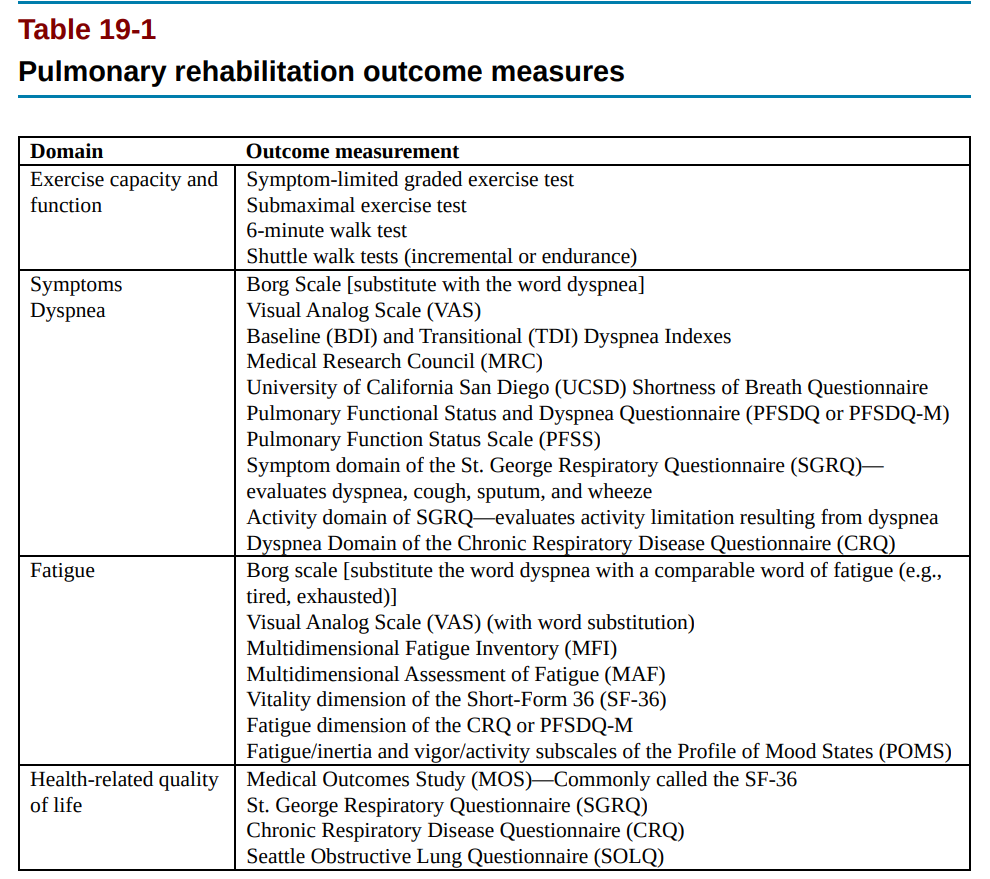
Choosing goals and outcomes in PR
SMART goal
We make a realsitoc goal, we start working on it, how to assess the outcome of the treatment? → how do we assess if there are any improvements?
Through the following KEY AREAS:
1) Exercise capacity
PT increase in strength, endurance
learn strategies to manipulate environment
Measurement tools → graded exercise tests, time distance walk test, shuttle walk test, timed ADLs
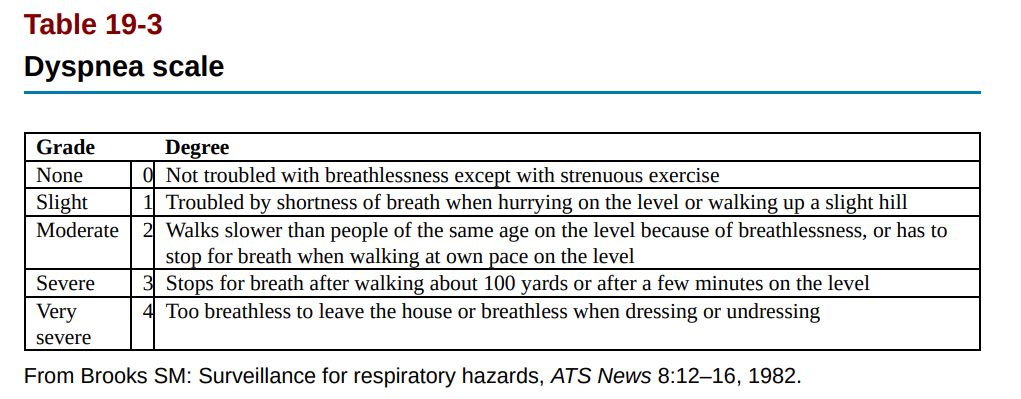
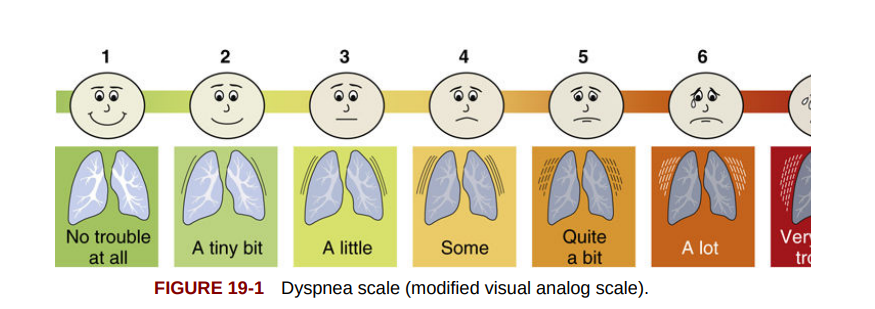
2) Symptoms (dyspnea, fatigue)
PT can better mobilize respiratory secretions
PT learns to improve strategies to relieve the symptoms
decrease respiratory exeberations
obtain good oxygen saturation
Measurement tools → BORG
3) Health related quality of life
PT stops smoking, drinking
PT shows adherence
PT improves coping skills
PT improves perceived quality of life
Measurement tools → behavioral surveys, self report tools (tabacco use journal)
4) Psychological status
PT improves anxiety, and depression
Measurement tools → depression scoring questionnaires
Other rehab goals
stop smoking
Pulmonary rehab (summary)
it starts in the acute stage (aka hospital)
there is a rehab team → multidisciplinary
PT usually has a support system (spouse, family)
Components of rehab: (named them at the beginning too → We can be aware of these aspects but we can’t treat everything)
PT assessment outcomes and goals
Exercise prescription and training
Self-management education
Nutritional intervention
Psychological support
Assessment
1) observation → posture changes due to breathing pattern, observation of breathing pattern, adoption of propping posture that inhibits mechanics
during the treatment plan, we should include chest wall mobility (to look into it further)
2) AROM-PROM → ribcage, shoulders, spine (changes due to lung diseases, poor posture, accessory muscle use during breathing)
postural changes lead to loss of rib cage mobility
hamstrings, triceps surae (loss of flexibility/ strength/ ROM due to disuse)
Note:
PT with pulmonary diseases usually present with MSK complaints (OA, RA, scoliosis, SCI, sclerodema)
The prolonged usage of corticosteroids leads to OA and general degeneration of tissues.
Self-management education
educational assessment to determine how well Pt understands her/his disease → helps both physio (determine exercises )and PT (safety, awareness)
didactic setting to practice
EX: PT able to recognize early signs of exacerbation, when to start antibiotic, steroid, branchiodilatators and when to contact PT/practitioner
PT knows anatomy, use/misuse of oxygen and how to tailor ADLs to his/her needs and how to clear airway
Note on nutrition: pulmonary diseases alter the BMI
How? nutrients and malabsorption, muscle and energy depletion → low BMI, or obesity (hyperventilation syndrome) and decrease in activity level and other comorbidities (diabetes, cardiac diseases)
WE DON"T DIAGNOSE → we ask for chart 🙂 → what should we look in chart?
labs (blood chemistry, blood counts)
pulmonary function tests
chest X-ray
arterial blood gas analysis (evaluation of gas exchange Co2 and O2)
ECG
medications, surgical interventions, ventilation, oxygen therapy
other medical diagnoses (cancer, cardiac disease, diabetes..)
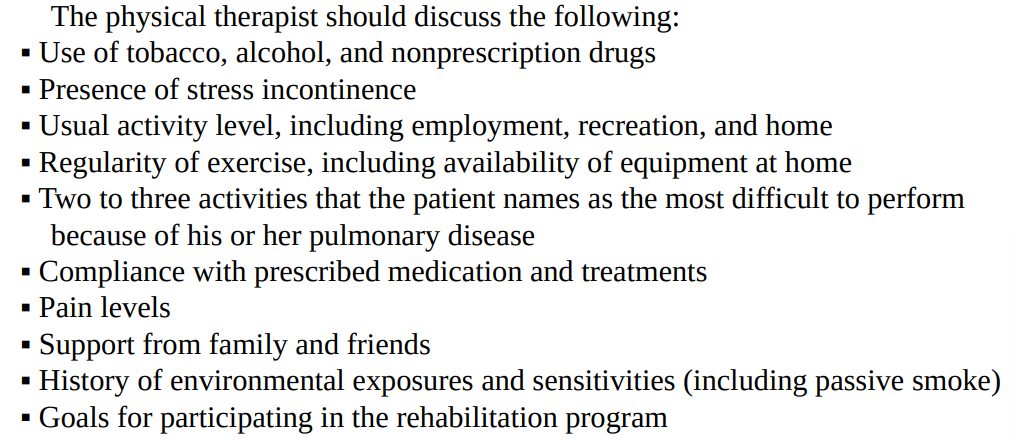
What should we ask PT? → Anamnesis
Assessment
1) Nutritional evaluation
weight measurement
BMI
Hight
2) chest evaluation
auscultation lung and heart
cough assessment
inspection breathing pattern
PT with problems in lung secretion, coughing, and airway clearance might benefit from bronchodilator therapy
PT that uses accessory muscles might benefit from instruction of breathing techniques
3) MSK evaluation
AROM/PROM
Strength assessment of extremities and trunk → which test??
posture
gait
skin inspection (blue skin → hypoxia)
Edema inspection
4) Functional assessment → lack of energy leads to decrease of level of activity and participation of PT
ADLs (shower, dressing)
balance and gait
prior level of functioning
need for adaptive equipment
fall risk
leisure, social, and family activity
how do we assess ADLs? → Functional independence measure (FMI), AMPS, FCE (functional capacity evaluation)
1) airway clearance
2) Functional training (to treat fatigue, weakness, and dyspnea)
Goals:
Adapting the environment to improve the ease of performing ADLs,
Altering the performance of tasks to decrease energy costs
Incorporating methods to relieve symptoms associated with activity
3) energy conservation → How do we improve this?
1st → Identification of problematic ADLs
then modify the environment
example: modify the kitchen environment by positioning the equipment in a way that PT doesn’t have to bend, lift, places to rest, improve ventilation (window)
break the activity into pieces and apply:
slow down the pace
set priorities and organize activities to minimize wasted movement
plan an appropriate amount of time to complete tasks and include rest breaks
4) Relief of dyspnea
control breathing patterns during activities
improve the posture to improve breathing pattern
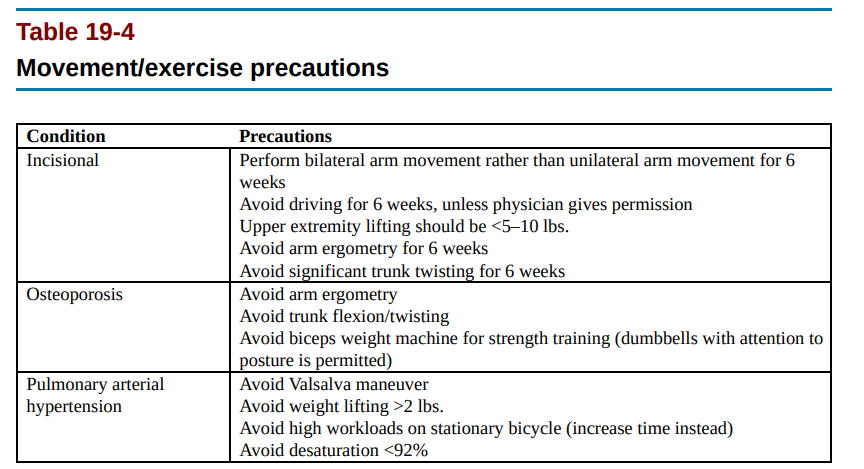
avoid bending (unwanted valsava maneuver and blood pressure changes)
EX: change the way PT laces the shoes
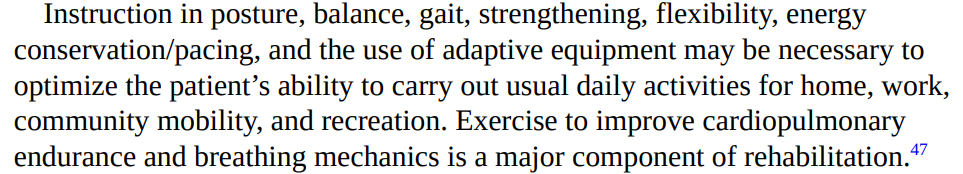
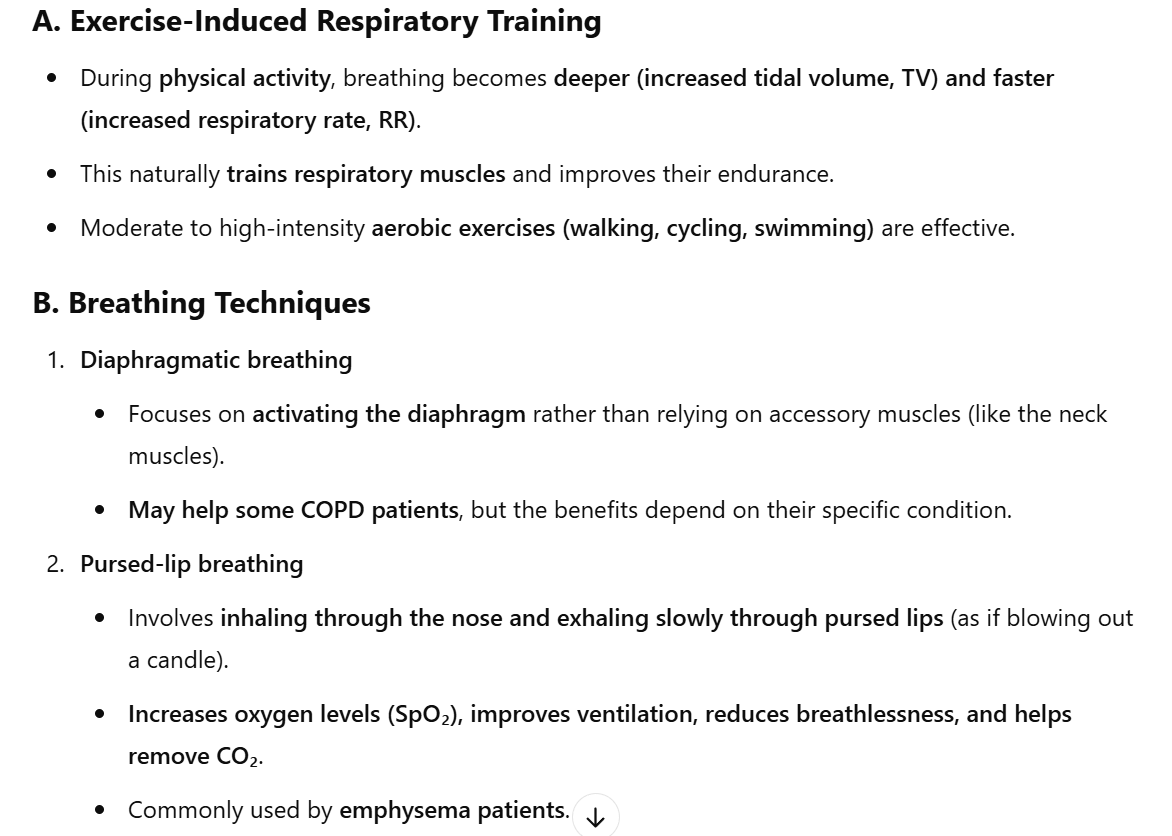
5) Breathing re-training
avoid breath holding, valsava maneuver, or unnecessary talking during tasks
use “Purse lip breathing“
forward-leaning posture might help (PT with flat diaphragms) and improve IAP and push diaphragm into the thorax
relaxation techniques
6) Oxygen evaluation use
Need to monitor PT during exercises, how?:
pulse oximetry, dyspnea scale, BORG scale, RR, HR, blood pressure
Physical conditioning
Activity = intensity + workload + duration + frequency (reps) (+ symptoms + MSK discomfort → they must be noted)
In general, follow training principles, but be aware of PT abilities (increase difficulty in the treadmill but remember that PT can die and then it’s your fault)
GOALS:
cardiorespiratory endurance; maximizing work capacity; and improving strength, flexibility, and respiratory muscle function.
how to get there?
endurance training
aerobic endurance training (high or low intensity) → VO2 max
interval training is perfect (rest periods and high-intensity training)
Dosage:
3 to 5 times x week
60 to 120 minutes x session
over a course of 4 to 72 weeks
PT can perform exercise in autonomy, but needs to be explained
frequent rest breaks when necessary
Goal: achieve fewer rest breaks and at least 30 minutes of exercises within the first week of rehab
Mode:
walking (treadmill, track)
cycling (stationary or normal)
steps exercises
rowing
arm lifting weights
swimming
always include a warm-up and a cool-down
Intensity
PT needs to like the activity → also to help them cope with symptoms
always based on PT goals, training should be designing according to them
intensity relate to: time + workload + physiological response (→ check with BORG/dyspnea scale/MET level)
YOU NEED TO BE AWARE OF MAX HR (220 - age = max HR)
at rest
when moving
medications
Also, NEED TO KNOW If they are taking medicines or oxygen therapy during treatment (if they need a bronchodilator and they don’t use it while they exercise with you they will perish)
Upper and lower extremity training
most beneficial if training involves groups of muscles that are involved in functional living (train more based on functioning in ADLs)
what can PT do? → Walking ▪ Stationary cycling ▪ Bicycling ▪ Stair climbing ▪ Aquatic therapy
Strength training
weight lifting
How do we set Strength training for PT?
1) Low resistance at first (light weights, resistance bend)
2) increase first the reps and then the weight
3) If PT is strong → weight machines
Flexibility
we already talked about why this is important, look at the beginning of the chapter
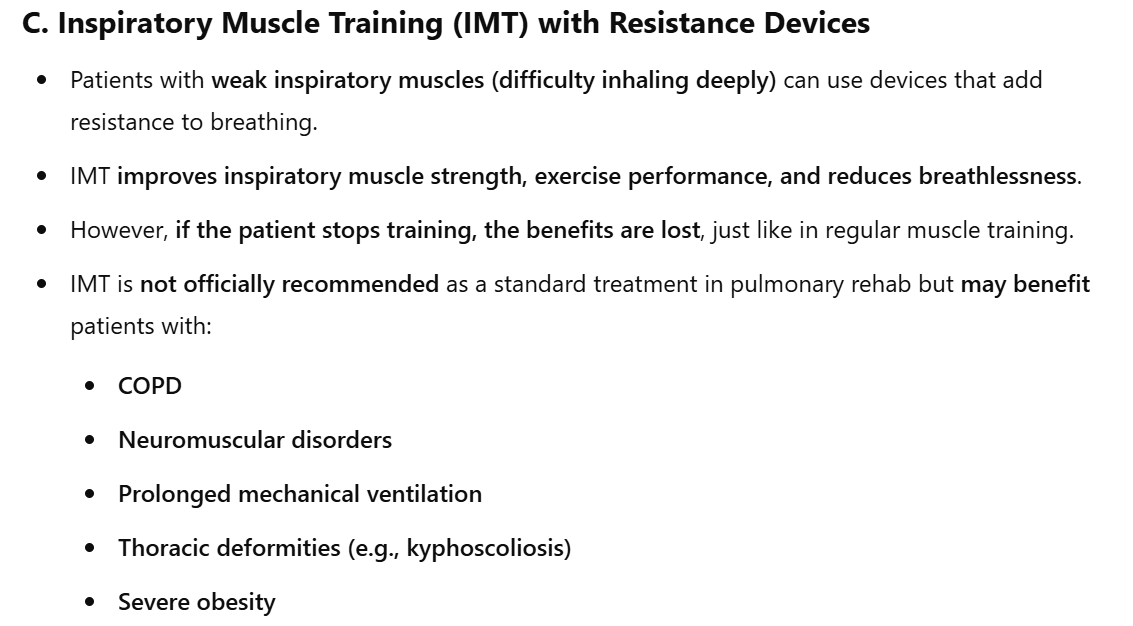
respiratory muscles exercises
improve the performance of respiratory muscles through exercise training
How to train these muscles? (note to self: from the book, it;s just a summary from chat)
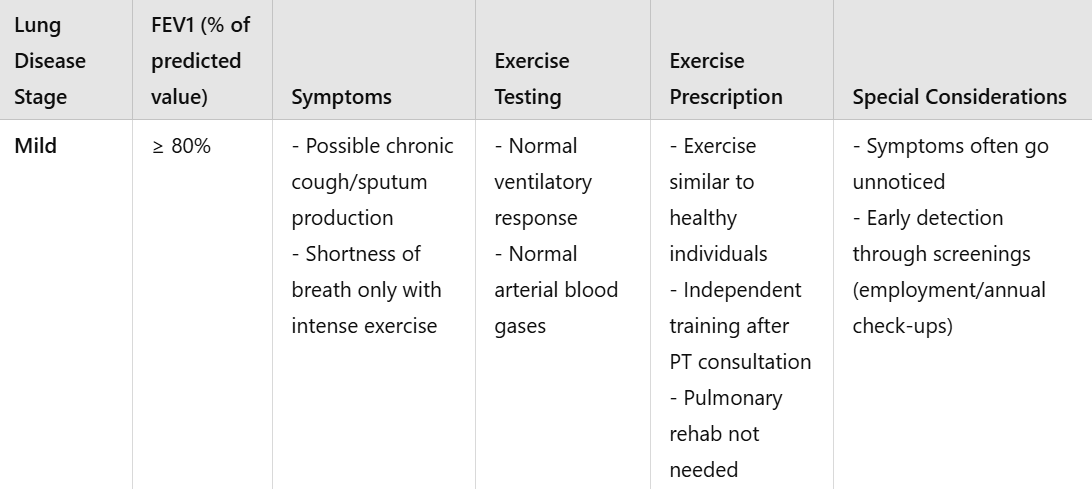
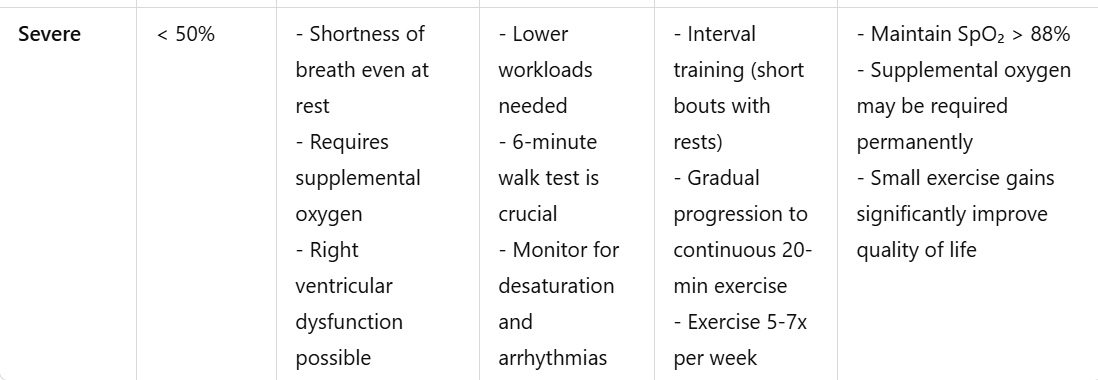
Exercise consideration for different stages of lung diseases