1: Nursing—The evolution of a profession
What is nursing?
Definitions of Nursing
A profession that draws from the social, behavioural, and physical sciences.
A profession that addresses responses from people and families to promote healthy living, maintenance, and health problems.
It is the act of utilising the environment of the patient to assist him in his recovery (Florence Nightingale, 1860).
She considered a clean, well-ventilated and quiet environment is important for recovery.
It is assisting the individual, sick or well, in the performance of those activities contributing to health, its recovery, promoting quality of life or to a peaceful death that the client would perform unaided if he or she had the necessary strength, will or knowledge (Virginia Henderson, 1966).
Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of the ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. (ICN, 2002)
Nursing also helps individuals carry out prescribed therapy, to be independent of assistance and function to maximum potential as soon as possible ( Crisp et al 2013 ).
Themes of Nursing
Nursing is caring
Nursing is an art
Nursing is a science
Nursing is individual centred
Nursing is holistic
Nursing is adaptive
Nursing is concerned with health promotion, health maintenance and health restoration
Nursing is a helping profession.
Providing nursing care
Technical skills, clinical experience, and theoretical knowledge is required.
Expertise is required for interpreting clinical situations and for complex decision making.
Nurses makes clinical judgement about the care needed for individuals based on fact, experience, and standards of care.
Patients, Consumers, and Clients
Patient:
Historically implied passivity and dependence on healthcare providers.
Still commonly used in Australian healthcare settings.
Associated with the medical model of health.
Consumer:
An individual or group that uses a service of commodity.
Implies an active seeker of healthcare services with specific needs and expectations.
Emphasizes the individual's role in making informed decisions about their care.
Associated with the consumer model of healthcare.
Client:
A person who engages the advice or services of another who is qualified to provide this service.
Suggests a collaborative relationship between the individual and healthcare provider.
Emphasizes the individual's responsibility for their own health.
Associated with the person-centred model of care.
Historical Perspectives
The word “nurse” is derived from Latin word meaning to nourish or cherish.
In some cultures, illness, injuries, or death are involved with superstition and witchcraft.0
Sickness was a punishment for wrongdoings, and a sign of evil spirits.
Treatment were used to prescribed by witch doctors and priests—using old herbal remedies.
Crusades — a series of religious wars between the 11th and 13th centuries, which played a significant role in the development of organized nursing.
Military Religious Orders
Knights of St John of Jerusalem: also known as the Hospitallers, they founded hospitals throughout the Mediterranean region and provided medical care to soldiers, pilgrims, and the general public.
Teutonic Knights: Based in Prussia, they also established hospitals and provided medical care to their members and the local population.
Knights of St Lazarus: This order focused on caring for those suffering from leprosy, establishing leper houses across Europe.
Secular Orders
Ursulines: Founded in the 16th century, they focused on education and social work, including healthcare.
Poor Clares: A Franciscan order, they established hospitals and provided nursing care.
Beguines: A lay religious movement, they often engaged in charitable work, including healthcare.
Benedictines: A monastic order, they operated hospitals and provided medical care to their communities.
Augustinian Sisters of the Hôtel Dieu — established in the 12th century in Paris, this order is considered the world's oldest order of nuns devoted purely to nursing.
16th Century
Henry VIII's dissolution of English monasteries led to the closure of many hospitals that provided care to the sick and destitute.
Workhouses were established to house the poor, but conditions were often appalling.
Public pressure forced Henry VIII to allow the re-establishment of hospitals in London, such as:
St. Bartholomew’s Hospital: Established in 1123 by Rahere, a Norman canon.
St. Thomas's Hospital: Established in 1106 by the Archbishop of Canterbury.
St. Mary’s Hospital: Established in 1845.
The quality of care in these hospitals was often poor due to insufficient staffing and inadequate facilities.
18th Century : Dark Ages of Nursing
Hospitals were often overcrowded, dirty, and poorly ventilated.
Nurses were frequently uneducated, poorly trained, and of low moral character.
Characters like Sairey Gamp and Betsy Prig in Charles Dickens' Martin Chuzzlewit reinforced negative stereotypes about nurses.
Prominent Figures in 19th to 20th century
Theodor Fliedner: He established “Kaiserwerth” in 1836 Germany, to train selected women as deaconesses.
Elizabeth Fry: Inspired by Kaiserwerth, she founded the Protestant Sisters of Charity to provide compassionate care to the sick.
Agnes Jones: A prominent figure in nursing reform, she revolutionized conditions in workhouses and established a nursing school.
Florence Nightingale: The founder of modern nursing.
Florence Nightingale
Early Life and Education:
Born in 1820 in Florence, Italy.
Received a comprehensive education, unusual for women of her time.
Felt a strong desire to pursue nursing, despite family opposition.
Career Highlights:
Spent time at the Kaiserwerth Deaconess House, a nursing school in Germany.
Appointed Superintendent at Establishment for Gentlewomen in 1853 in London.
Led a team of nurses to Scutari in Crimean War to care for wounded soldiers.
Implemented significant sanitary reforms, improving conditions for soldiers and reducing mortality rates.
Became known as the "Lady of the Lamp" for her dedication to caring for the sick.
Founded the Nightingale School of Nursing at St Thomas' Hospital.
Legacy:
Pioneered nursing education and training.
Made significant contributions to public health and sanitation.
Received widespread recognition and acclaim for her work.
Nursing History in Australia
Aboriginal People — the first people or nation who arrived in Australia from SEA, and was acknowledged as traditional caretakers of land.
The white or British colonisation introduced modern nursing in AUS.
Sydney Hospital: first hospital in Australia, opened in 1811.
Irish Sisters of Charity: first five trained nurses who arrived in Sydney in 1838 to provide care to the sick.
The 1840s marked the end of convict transportation to Australia, opening the way for free settlers.
In 1851, the discovery of gold led to a significant population influx—which necessitated the development of basic infrastructure, including healthcare.
Prior to 1868, nursing practices were unprofessional and unregulated.
Nurses lack training and basic education.
Hospitals were unsanitary and patients received inadequate care.
Patients has negative experience at hospitals and avoided seeking care.
Henry Parkes (Colonial Secretary of NSW), wrote a letter to Nightingale requesting her to provide nurses to Australia to clean up hospitals. She sent six of her best trainees to set up a training school, this included:
Lucy Osburn: A pioneer in Australian nursing education, she established the first training school for nurses in Melbourne in 1879.
Mary Barker: Known for her work in bush nursing, she traveled to remote areas of Australia to provide healthcare to settlers and Indigenous communities.
Bessie Chant: A prominent figure in nursing education, she was the first Principal of the Sydney Hospital School of Nursing.
Eliza Blundell: A nurse who served in the South African War, she was recognized for her bravery and leadership.
Annie Millar: A nurse who served in the Australian Army Nursing Service during World War I, she was awarded the Military Medal for her bravery under fire.
Haldon Turriff: A nurse who served in World War I, Turriff was awarded the Military Medal for her bravery under fire.
Australian Nurses in Wartime
Boer War (1899-1902)
60 nurses were sent to the war.
Three were awarded with Royal Red Cross medals
Frances Hines: the first Australian woman to die in a declared war.
World War I (1914-1918)
Australian Army Nursing Service (AANS): established in 1902, a branch of the Australian Army that provides nursing care to soldiers and their families.
At war outbreak, nurses served at field and based hospitals in Australia, including Egypt, England, France, Belgium, Greece, Salonika, Palestine, Mesopotamia, and India.
2139 Australian nurses served in World War I.
World War II (1939-1945)
Nurses served in England, Egypt, Palestine, Libya, Greece, Syria, Ceylon, Malaya, Singapore, Papua New Guinea and the Solomon Islands and throughout Australia.
Capture of first six Australian nurses at Rabaul (1942).
65 nurses were evacuated on SS Vyner Brooke.
12 died when it was sunk off in Sumatra.
21 died in Banka Island Massacre.
32 became prisoners of war in Sumatra (around Palembang).
Vivian Bullwinkel: The sole survivor of the 1942 Banka island massacre. She hid for 12 days before surrendering and spent 3.5 years in captivity.
Progress of Nursing in Australia
Year | Milestones |
1811 | Sydney Hospital opens; nursing undertaken by convict men and women |
1836 | Deaconess Institute of Kaiserwerth, Germany, is founded |
1838 | Five Irish Sisters of Charity, Australia’s first trained nurses, arrive in New South Wales |
1848 | Opening of Yarra Bend Asylum at what was to become known as Melbourne to enable the mentally ill to be transferred from gaol |
1860 | Florence Nightingale publishes Notes on Nursing: What It Is and What It Is Not |
1868 | Sir Henry Parkes requests Nightingale provide trained nurses for New South Wales. |
Arrival of Lucy Osburn and five Nightingale nurses at Sydney Infirmary (to become Sydney Hospital). | |
1871 | Nightingale-trained matron appointed to the Alfred Hospital, Melbourne |
1899 | Australasian Trained Nurses Association is founded in New South Wales |
1920 | South Australia becomes the first state to pass nursing registration legislation. |
1922 | Western Australia follows suit to pass nursing registration legislation. |
1924 | New South Wales and Victoria also introduce nursing registration laws. |
Formation of Australia Nursing Federation (ANF) | |
1933 | Australian Capital Territory nursing registration commences |
1949 | Formation of College of Nursing Australia (now RCNA) |
1952 | Nursing Research , a journal reporting on the scientific investigations of nursing, established in the United States |
1960s-1970s | Concerns about low recruitment rates and high attrition rates in nursing training. Many are qualified but not entering workforce. |
The creation of a second tier of nurses, Enrolled Nurses (ENs), to address staffing shortages. | |
Nurses expressed increasing dissatisfaction with their wages and working conditions. | |
1975 | First nursing diploma program in Australia in a College of Advanced Education (CAE) in Melbourne, followed quickly by programs in New South Wales, South Australia and Western Australia |
1983 | New South Wales announces that all nursing education in the state will be transferred to CAEs by 1985. |
International Council of Nurses embeds in new constitution the categories ‘first-level nurse’ (the Registered Nurse, RN) and ‘second-level nurse’ (the Enrolled Nurse, EN). Magnet Hospital research begins in the United States. | |
1984 | Australian federal government announced full support for the transfer of nursing education into the tertiary sector. |
1985 | One university and 12 Colleges of Advanced Education offered the Diploma of Applied Science (Nursing) for the first time. |
1987 | The Nurses Registration Act of 1953 dictated that education was to consist of 75 hours of lectures during one year of practice. |
The ‘nursing aide’ title was changed to ‘Enrolled Nurse’, and a syllabus, approved by the Board, was instituted. | |
1990 | All nursing education transferred to tertiary sector and at degree level in Australia |
TAFE NSW was founded and was formed through the amalgamation of 35 technical and further education colleges in NSW. Students receive 360 hours of theoretical instructions, and 40 weeks rotated through clinical areas which is required by the Board. | |
1992 | The nomenclature ‘Bachelor of Nursing’ was adopted. |
2000 | International nursing shortage is recognised and becomes a government priority in Australia. |
Increase in ‘medical error’ becomes an international concern | |
2002 | Two national reviews in Australia, the Senate Review of Nursing and a National Review of Nursing Education |
2004–2006 | National Nursing and Nursing Education Taskforce in Australia |
2005 | Australian Nursing Council becomes Australian Nursing and Midwifery Council (ANMC) |
2007 | Australian federal government announcement of national system of regulation and accreditation for health professionals—including nurses and midwives |
2010 | The Australian Health Practitioner Regulation National Law Act 2009 comes into effect. |
The Australian Health Practitioner Regulation Agency (AHPRA), the organisation responsible for the registration and accreditation of 10 health professions across Australia, is established. | |
ANMC is established as the accreditation authority responsible for accrediting education providers and programs of study for the nursing and midwifery profession. | |
2011 | Accreditation process for Nursing Courses in Australia is taken over by ANMC; ANMC becomes Australian Nursing and Midwifery Accreditation Council (ANMAC). |
Unification of Royal College of Nursing, Australia (RCNA) and The College of Nursing (TCoN) to become Australian College of Nursing. |
Prominent Figures in Australian Nursing
Figure | Contribution to Australian Nursing |
Florence Nightingale (1820–1910) | Though not Australian, her principles of nursing greatly influenced nursing education and practices in Australia, laying the foundation for modern nursing. |
Lucy Osburn (1836–1891) | Brought Nightingale's nursing principles to Australia and established the first professional nursing service at Sydney Hospital in 1868. |
Jean Bell (1873-1959) | She was essential in reforming nursing training at the Royal Melbourne Hospital, apart from her stint abroad in 1914 as Principal Matron of the First Australian General Hospital in the army during World War I. |
Jean Henderson (1891–1977) | Prominent in advancing nursing education in Australia and helped establish the Australian Nursing Federation. |
Annie M. Sage (1895–1969) | Director of the Army Nursing Service during World War II, known for improving military nursing services in Australia. |
Elizabeth Kenny (1880–1952) | Pioneered treatment for polio patients, known as the "Kenny Method", which significantly influenced rehabilitation nursing in Australia. |
Dame Edith Anderson (1890–1954) | One of the first Australian nurses to serve internationally, contributing to global health and promoting Australian nursing abroad. |
Muriel Knox Doherty (1896-1988) | She founded Preliminary Nurse Training at Sydney's Royal Prince Alfred Hospital in 1936. She also founded: Council of the New South Wales College of Nursing; Australasian Trained Nurses' Association, and the National Florence Nightingale Memorial Committee in Australia after returning. |
Gwendolen Burbidge (1904-2000) | She wrote the first Australian nursing textbook, Lectures for Nurses, in 1934. She became the first Australian infectious disease hospital's matron when she returned to the country. She was the Australia's delegate to the International Council of Nurses. |
Margaret Scott (1912–1999) | Influential in psychiatric nursing and a key figure in developing mental health nursing standards in Australia. |
Mavis Mitchell (1911–1996) | Known for her contributions to nursing education, especially in remote and rural areas, improving healthcare accessibility in underserved regions. |
Vivian Bullwinkel (1915-2000) | The sole survivor of the 1942 Banka island massacre. After WW2, she worked as a civilian nurse at Heidelberg Repatriation Hospital and was Fairfield Infectious Diseases Hospital's Director of Nursing |
Dame Dorothy Reading (1913–2012) | Advocate for public health and community nursing, instrumental in developing home nursing services and public health policies in Australia. |
Mary Evans (1915-2004) | A trained midwife in Queen Victoria Memorial Hospital, and joined the Home Midwifery team in Melbourne District Nursing Service. |
Faye McMillan (b. 1971) | First Indigenous Australian to become a registered pharmacist, she is a leader in Aboriginal health and nursing, contributing to closing the health gap. |
Sally Goold | A Wiradjuri woman to became the first Indigenous registered nurse in NSW. |
Adjunct Professor Debra Thoms | Former Chief Nursing and Midwifery Officer of Australia, known for her leadership in health policy, nursing advocacy, and improving standards of practice. |
Professor Jill White | A prominent figure in nursing education, she has contributed to the professional development of nursing standards and research in Australia. |
Nursing practice in Australia
Competency standards/standards for practice
Nursing and Midwifery Board of Australia (NMBA) — responsible for the standards relating to the professional practice or nurses and midwives.
Standards of nursing practice
Serve as objective guidelines for the provision of nursing care and to evaluate that care.
Developed from a basis of strong scientific research and the advice of clinical experts.
Provides method to ensure people receive high-quality care, to ensure that nurses know what it is necessary to provide expert nursing care, and ensure that measures are in place to determine that care meets specific standards.
Educational institutions can recommend students for registration only if they have demonstrated and maintained the required standards.
Scope of Practice
Nurses and midwives must be educated, competent, and permitted by law to perform.
The scope is influenced by:
Settings in which they practise
Health needs of people
Level of competence and confidence of th enurse
Service provider’s policy requirements.
Supervision of ENs by RNS
Direct Supervision — the supervisor (RN) is present, observing, working with, guiding and directing the EN.
Indirect Supervision — the supervisor (RN) works in the same facility as EN, but does not constantly observing their activities. RNs must be available for reasonable access.
Factors that influence scope of practice
Type of setting (e.g. healthcare agency, educational organisation, community health service)
Location of the setting (e.g. urban, rural or remote, community, acute care)
Characteristics of individuals (e.g. health status, age, learning needs)
Focus of healthcare activities (e.g. health promotion, research, education)
Complexity of practice (e.g. health acuity of the individual/population)
Level of responsibility/accountability of the healthcare provider
Resources that are available/accessible as part of the health service.
Unregulated healthcare workers
Health Services Assistants (HSA) and Assistants in Nursing (AIN) — provide support to registered nurses and other healthcare professionals in acute care settings. They are often responsible for tasks that do not require the full scope of a registered nurse's expertise.
Assisting with patient care activities, such as bathing, dressing, and feeding
Monitoring vital signs
Collecting specimens
Preparing patients for procedures
Maintaining a clean and safe environment
Personal Care Workers (PCW) or Personal Care Attendants (PCA) — provide personal care and support to individuals in a variety of settings. They typically focus on activities of daily living (ADLs) and other personal care tasks.
Assisting with personal hygiene, such as bathing, dressing, and grooming
Assisting with mobility, such as transferring and walking
Providing companionship and emotional support
Preparing meals and feeding clients
Managing personal belongings
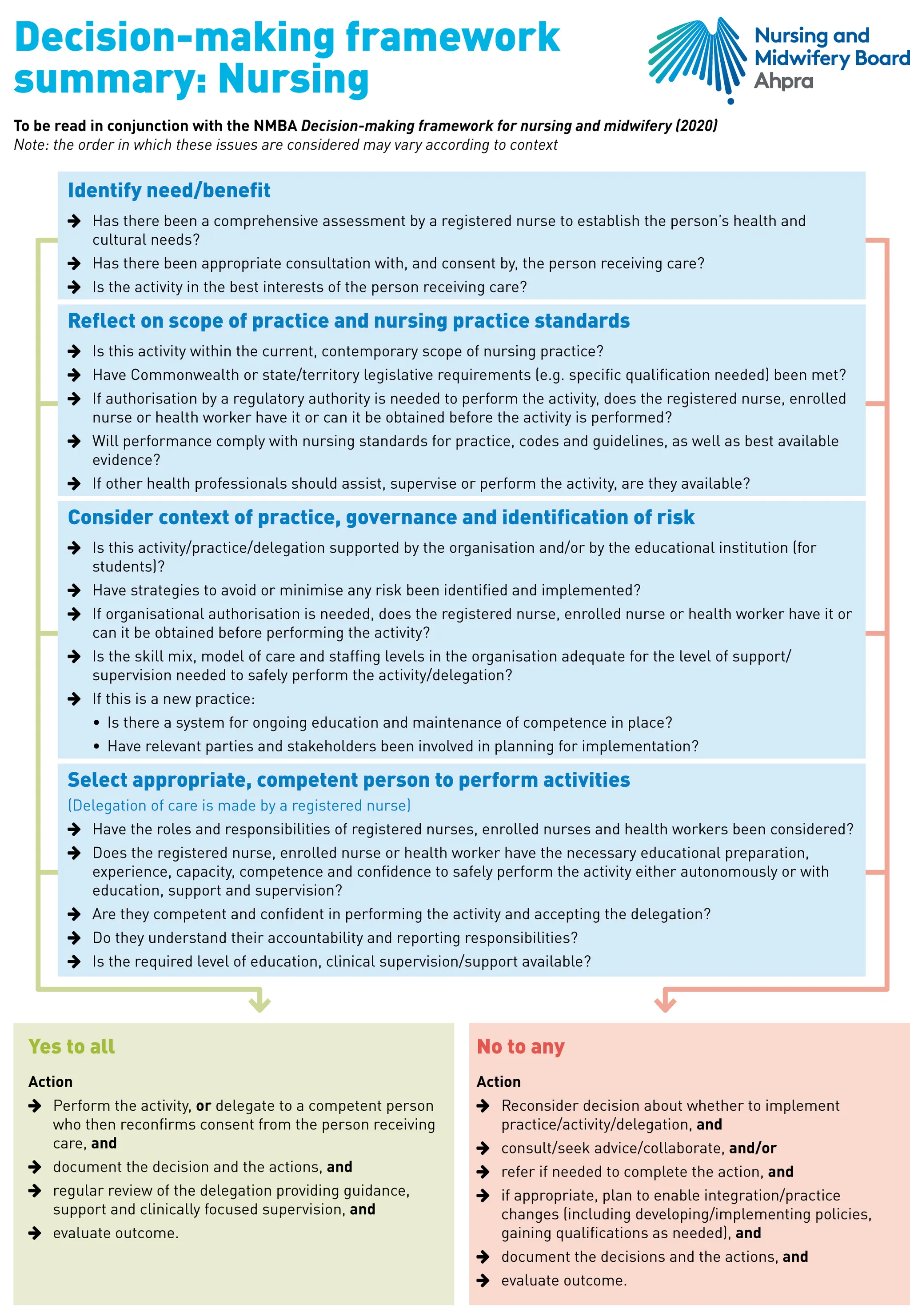
Decision-making Frameworks
NMBA Decision-making framework considerations:
Am I educated?
Am I authorised?
Am I competent?
Scope of practice tools for nursing and summaries are guide to decision making relating to scope of practice and delegation and to promote decision making that is consistent, safe, person centred and evidence based.
They provide a tool for nurses and employers to use:
When considering or determining scope of practice and to clarify expectations of nursing practice
When employers are creating, interpreting and planning policies that apply to nursing practice
As a performance criterion for nurses
To stimulate professional discussion related to decision making and scope of practice.
Nurse work is a combination of knowledge, judgment, and skills that guide their practice.
Code of Ethics
International Council of Nurses (ICN) Code of Ethics for Nurses — effective 1 March 2018, and has four principal elements that outlines the standard of ethical conduct.
Nurses and people
Nurses have a responsibility to respect the human dignity, worth, and uniqueness of all individuals.
Treat all people with compassion and respect, regardless of their background, culture, or beliefs.
Promote the health and well-being of individuals and communities.
Protect the rights of individuals and advocate for their needs.
Nurses and practice
Nurses should practice in accordance with the highest professional standards.
Maintain competence and continually update their knowledge and skills.
Use knowledge and skills to promote the health and well-being of individuals and communities.
Be accountable for their actions and decisions.
Nurses and the profession
Nurses should act with honesty and integrity in all their professional relationships.
Promote the development of the nursing profession and contribute to its advancement.
Work collaboratively with other healthcare professionals to provide high-quality care.
Advocate for the rights of nurses and ensure that they have the resources and support they need to practice effectively.
Nurses and co-workers
Nurses should collaborate with other healthcare professionals to provide the best possible care for patients.
Respect the contributions of other members of the healthcare team.
Maintain a respectful and supportive work environment.
Advocate for fair and equitable treatment of all healthcare workers.
Registration
In order for nurses to register they need to prove that they meet the following registration standards, set by the national board for nursing, the NMBA:
Continuing professional development
Criminal history
English language skills
Professional indemnity insurance arrangements
Recency of practice.
Nursing and Midwifery Board of Australia (NMBA)
Functions
Registering nursing and midwifery practitioners and students
Developing standards, codes and guidelines for the nursing and midwifery profession
Handling notifications, complaints, investigations and disciplinary hearings
Assessing overseas-trained practitioners who wish to practise in Australia
Approving accreditation standards and accredited courses of study.
They approve:
Policies
Professional standards
Guidelines
Position statements
Frameworks and
Fact sheets
Professional standards:
Codes of ethics and conduct for both midwives and nurses.
Professional practice guidelines for: informing a national board about where you practise; advertising of regulated health services; and guidelines for mandatory notification.
Guidelines covers: CPD; nurses applying for endorsement as Nurse Practitioner and for scheduled medicines; Standards for practice; registration standards; frameworks for the assessment of national standards for practice; and re-entry to practice policy.
Standards can be used by:
Individual nurses to assess their own performance or the performance of their peers
Regulatory authorities to assess nurses involved in professional misconduct matters
Higher and vocational education authorities who use competency standards as a framework for course development
Employers who use competency standards for employment assessment and development of job description forms
The profession, for communication to consumers of the standards which can be expected from a Registered or Enrolled Nurse
Standards and codes
Code of Professional Conduct for Nurses
ICN Code of Ethics for Nurses and Midwives
Australian Health Practitioner Regulation Agency (AHPRA)
Protects the public and set standards and policies that all registered health practitioners must meet.
Supports the NMBA in its primary role of protecting the public
Manages the registration processes for health practitioners and students around Australia
Has offices in each state and territory where the public can make notifications about a registered health practitioner or student
On behalf of the boards, manages investigations into the professional conduct, performance or health of registered health practitioners, except in NSW where this is done jointly by the Health Professional Councils Authority and the Health Care Complaints Commission
On behalf of the national board, publishes national registers of practitioners so important information about the registration of individual health practitioners is available to the public
Works with the Health Complaints Commission in each state and territory to make sure the appropriate organisation investigates community concerns about individual, registered health practitioners
Supports the boards in the development of registration standards, and codes and guidelines
Provides advice to the Ministerial Council about the administration of the national registration and accreditation scheme.
Australian Nursing and Midwifery Accreditation Council (ANMAC)
Development of accreditation standards
Accreditation of Australian nursing and midwifery courses
Accreditation of Australian providers of nursing and midwifery courses
Assessment of, for the purposes of permanent migration, internationally qualified nurses and midwives
Provision of policy advice on matters relating to accreditation and skilled migration of nurses and midwives.
Liaising with professional bodies, regulators and educators relating to standards of education and practice
Professional nursing organisations
Australian College of Nursing (ACN)
Formed in 2011 when Royal College of Nursing, Australia (RCNA) and The College of Nursing (TCoN) united.
It represents nurses in policy development, and is intent on advancing nurse leadership to enhance the healthcare of all Australians.
Australian Nursing and Midwifery Federation (ANMF)
Established in 1924 and was formerly Australian Nursing Federation (ANF) until name changed in 2013 to ANMF.
It is the national union for nurses and the largest professional organisation in Australia.
Its core business is the industrial and professional representation of nurses and nursing through the activities of a national office and branches in every state and territory.
National Enrolled Nurse Association (NENA) — ANMF’s special interest group for ENS, which promotes the value of ENs and raise awareness of the EN role in the community.
Congress of Aboriginal and Torres strait islander Nurses and Midwives (CATSINaM)
The representative body for Aboriginal and Torres Strait Islander nurses and midwives in Australia.
Its function is to increase the recruitment and retention of Aboriginal and Torres Strait Islander peoples into nursing and midwifery.
It promotes, supports and advocates for Aboriginal and Torres Strait Islander nurses and midwives and aims to close the gap in health for Aboriginal and Torres Strait Islander peoples.
Nursing—the profession
Profession — An occupation that requires extensive education and calling that requires a special knowledge, skill and preparation.
Characteristics of a Profession
An extended and broad-based education of its members
A theoretical body of knowledge leading to defined skills, abilities and norms
The provision of a specific service
Autonomy in decision making and practice
The regulation of practice, both legally through legislation, and ethically through a code of ethics for practice.
Nurse Education
Regulatory Bodies:
ANMAC (Australian Nursing and Midwifery Accreditation Council): Accredits nursing and midwifery education programs.
NMBA (Nursing and Midwifery Board of Australia): Approves nursing education providers and registers students.
AHPRA (Australian Health Practitioner Regulation Agency): Registers students and monitors their conduct.
Types of Nurses:
Registered Nurse (RN): Requires an undergraduate degree in nursing.
Duration: 3 years (standalone) or 4-5 years (combined with midwifery).
Responsibilities: Independent and interdependent practice, delegation of care to ENs and healthcare workers.
Career Paths: CNS, CNC, NUM, nurse educator.
Enrolled Nurse (EN): Requires a Diploma of Nursing.
Duration: 18-24 months.
Advancement: Can complete an Advanced Diploma or Bachelor of Nursing.
Unregulated Healthcare Workers: They are employed in healthcare facilities to undertake personal care tasks and activities of daily living.
Includes AIN, SW, PCW, PCA
Some requires Certification through VET sector.
Theories and Models of Nursing
Theory — an abstract statement formulated to explain or describe the relationships between concepts or events.
Nursing theory — conceptualises an aspect of nursing for the purpose of describing, explaining, predicting and/or prescribing nursing care.
Model — a conceptual framework developed from a set of concepts and assumptions; it provides the outline for which theory provides the functions.
A model represents structure while a theory suggests function .
Numerous conceptual models of nursing practice have been devised, most of which:
Are based on sound theory
Contain implied or explicit assumptions, values and goals
Are implemented by the nursing process.
Theoretical models serve as frameworks for nursing curricula, clinical practice and research.
Domain — a field or scope of knowledge of a discipline and contains the subject, central concepts, values and beliefs, phenomena of interest and the central problems of the discipline.
Paradigm — a model that explains the links to science, philosophy and theory accepted by the discipline.
Nursing Paradigm
Person: the recipient of nursing care
Environment: the internal and external surroundings that affect the person
Health: the degree of wellness or wellbeing that the person experiences
Nursing: the attributes, characteristics and actions of the nurse providing care on behalf of, or in conjunction with, the person.
Nursing theories can help make sense of processes and practices.
These are an attempt to elucidate the nature of nursing practice, the principles on which practice is based and the proper goals and functions of nursing in society.
These help create an understanding of the practice of nursing, how nurses interact with individuals and how nursing actions and provision of nursing care is structured.
Overview of selected nursing theories
Theory | Proponent(s) | Key Focus |
Environment Theory (1859) | Florence Nightingale | Links health to five environmental factors: fresh air, pure water, efficient drainage, cleanliness, and light. |
Theory of Interpersonal Relations (1952) | Hildegard Elizabeth Peplau | Stresses nurses understanding their own behaviour to help others identify difficulties. |
Typology of 21 Nursing Problems (1960) | Faye Glenn Abdellah | Nursing care is based on the individual's specific problems. 4 key areas of 21 nursing problems: comfort, hygiene and safety; physiological balance; psychological and social factors; and sociological factors. |
Deliberative Nursing Process (1961) | Ida Jean Orlando | Nurses should stay connected to patients, focusing on verbal and non-verbal cues to alleviate distress. |
Helping Art of Clinical Nursing (1964) | Ernestine Wiedenbach | Nursing care should be individualized to meet a person's needs. |
Nature of Nursing (1964) | Virginia Henderson | Identifies 14 basic human needs on which nursing care is based. |
Conservation Model (1967) | Myra Estrin Levine | Proposes principles of conservation for personal energy, integrity, and social and structural integrity. |
Behavioral System Model (1968) | Dorothy Johnson | Views the individual as a behavioral system composed of seven subsystems, like attachment, dependency, and achievement. |
Science of Unitary Human Beings (1970) | Martha Rogers | Focuses on the person as an irreducible energy field interacting continuously with the environment. |
Systems Model (1970) | Betty Neuman | Focuses on holistic care, preventing stress at three levels: primary, secondary, and tertiary. |
Self-Care Deficit Theory (1971) | Dorothea Orem | Proposes that self-care maintains health, based on self-care, self-care deficits, and nursing systems. |
Human-to-Human Relationship Model (1971) | Joyce Travelbee | Emphasizes nursing through human relationships, progressing through stages. |
Adaptation Model (1976) | Sister Callista Roy | Nursing focuses on a biopsychosocial adaptive system and modes of adaptation (physiological, self-concept, role function, interdependence). |
Transcultural Nursing Theory (1978) | Madeleine Leininger | Argues that caring is universal and varies transculturally, focusing on culture care preservation and restructuring. |
Philosophy and Science of Caring (1979) | Jean Watson | Centers on the humanistic aspects of caring, essential to nursing, using caritas processes. |
Goal Attainment Theory (1981) | Imogene M. King | Focuses on nurse-patient interactions, communication, and reaching mutual goals. |
Human Becoming Theory (1981) | Rosemarie Rizzo Parse | Highlights people as open systems interacting with the environment, co-creating health. |
Novice to Expert Theory (1982) | Patricia Benner | Proposes a five-level continuum for nurses’ skill development, from novice to expert. |
Roper, Logan and Tierney’s theory (1985) | Nancy Roper, Winifred W. Logan and Alison J. Tierney | Viewed the goal of nursing as helping people to prevent, alleviate, solve or cope with problems related to activities of living. |
Relationship of theories to nursing process
Nursing process — a tool and framework for contemporary nursing practice.
A series of planned steps that produces a particular end result.
A method used to assess, plan, deliver and evaluate nursing care.
Five components of nursing process
Assessment
Nursing diagnosis
Planning
Implementation
Evaluation.
The process ffers a systematic approach to nursing practice, enhances research opportunities and is compatible with many other systems in the healthcare delivery system.
Autonomy
Autonomy — a person is reasonably independent and self-governing in decision making and practice.
RN’s attain increased autonomy through higher levels of education, through clinical competence and in diverse practice settings.
All nurses are accountable for the type and quality of nursing care provided.
Influences of Nursing
Societal Influences on Nursing
The two World Wars significantly influenced the development of nursing in Australia, with many nurses serving overseas and contributing to the formalization of nursing as a profession. Nurses became essential figures in military and civilian care.
Technological Advancements in medical and healthcare systems have transformed the roles of nurses, enabling them to provide more complex and precise care, such as in critical care units and telehealth services.
Nurses in Australia have expanded from traditional bedside roles to include advanced practice, nurse practitioners, education, research, and leadership positions.
Demographic Changes
Australia has an increasingly ageing population, which has led to a higher demand for nursing services, particularly in aged care and chronic disease management. This demographic shift has influenced nursing education and specialisation in gerontology and palliative care.
A significant portion of Australia’s population lives in rural and remote areas. This has increased the demand for nurses who are trained to work in these challenging environments and provide comprehensive care with limited resources.
Australia's growing population and migration patterns have required nursing services to expand, increasing demand for a larger and more diverse nursing workforce.
Cultural Diversity
Australia is a multicultural nation, and the nursing workforce reflects this diversity. Nurses must be culturally competent to provide care to individuals from various cultural backgrounds. The inclusion of Aboriginal and Torres Strait Islander health perspectives has been crucial in culturally safe healthcare delivery.
Addressing health disparities among Indigenous populations has become a major focus, leading to the incorporation of cultural safety training in nursing education and policies to improve healthcare outcomes for Indigenous Australians.
Culturally and Linguistically Diverse (CALD) Populations: Nursing in Australia is influenced by the need to understand and respect cultural and linguistic differences. CALD populations require culturally sensitive care, which has led to the adoption of more inclusive practices.
Consumer Movement
Patient-Centered Care: Nurses and other healthcare providers work collaboratively with patients and their families in the decision-making process regarding care. This approach recognizes the consumer's rights and autonomy in their healthcare.
Increased Health Literacy: As consumers become more informed and health-literate, there is a greater expectation of transparency, communication, and participation in healthcare decisions. Nurses are now expected to educate and advocate for patients to navigate the complex healthcare system.
Healthcare Advocacy and Rights: The consumer movement has pushed for greater accountability and responsiveness from healthcare systems, including nursing. This has led to improved standards of care, safety measures, and the recognition of patient feedback in shaping nursing practice.
Human Rights Movement
Right to Healthcare: Nurses in Australia advocate for access to healthcare as a basic human right, influencing their role in ensuring equitable care for all individuals, regardless of socioeconomic status, race, or gender. This is particularly important in supporting marginalized groups.
Aged Care Reform: With the increased focus on the rights of older adults, the Aged Care Quality Standards have been implemented to ensure that elderly Australians receive dignified and person-centred care. Nurses play a crucial role in upholding these standards.
Disability Rights: The National Disability Insurance Scheme (NDIS) and other disability rights movements have shaped nursing care, especially for people with disabilities. Nurses now play a more active role in supporting independence and quality of life for individuals with disabilities.
Mental Health Advocacy: The human rights movement has emphasized the importance of mental health as a key aspect of overall health. Nurses have become frontline advocates for the rights of individuals with mental health issues, promoting respectful, stigma-free care.
Clinical Interests
The Nightingale Pledge
I solemnly pledge myself before God and this assembly to pass my life to purity and in the practice of my profession faithfully. I will abstain from what is deleterious and mischievous and will not take or knowingly administer any harmful drug. I will do all in my power to elevate the standards of my profession. And will hold in confidence all private matters that come to my knowledge in the practice of my calling. With loyalty, I will endeavour to aid the physician in his work. And devote myself to those committed to my care.
Job Description of a Floor Nurse (1887)
Daily sweep and mop the floors of your ward, dust the patients’ furniture and window sills.
Maintain an even temperature in your ward by bringing in a scuttle of coal for the day’s business.
Light is important to observe the patient’s condition. Therefore, each day fill kerosene lamps, clean chimneys, and trim wicks. Wash windows once a week.
The nurse’s notes are important to aiding the physician’s work. Make your pens carefully. You may whittle nibs to your individual taste.
Each nurse on day duty will report every day at 7 A.M. and leave at 8 P.M., except on the Sabbath, on which you will be off from 12 noon to 2 P.M.
Graduate nurses in good standing with the Director of Nurses will be given an evening off each week for courting purposes, or two evenings a week if you go regularly to church.
Each nurse should lay aside from each pay a goodly sum of her earnings for her benefits during her declining years, so that she will not become a burden. For example, if you earn $30 a month you should set aside $15.
Any nurse who smokes, uses liquor in any form, gets her hair done at a beauty shop, or frequents dance halls will give the Director of Nurses good reason to suspect her worth, intentions, and integrity.
The nurse who performs her labour, serves her patients and doctors faithfully and without fault for a period of five years will be given an increase by the hospital administration of five cents a day providing there are no hospital debts that are outstanding.
Australian army nursing service pledge of service
I pledge myself loyally to serve my King and Country and to maintain the honour and efficiency of the Australian Army Nursing Service. I will do all in my power to alleviate the suffering of the sick and wounded, sparing no effort to bring them comfort of body and peace of mind. I will work in unity and comradeship with my fellow nurses. I will be ready to give assistance to those in need of my help, and will abstain from any action which may bring sorrow and suffering to others. At all times, I will endeavour to uphold the highest traditions of Womanhood and of the Profession of which I am Part.
NMBA Enrolled Nurse Standards for Practice
Standard 1: Functions in accordance with the law, policies and procedures affecting EN practice
Demonstrates knowledge and understanding of commonwealth, state and/or territory legislation and common law pertinent to nursing practice.
Fulfils the duty of care in the undertaking of EN practice.
Demonstrates knowledge of and implications for the NMBA standards, codes and guidelines, workplace policies and procedural guidelines applicable to enrolled nursing practice.
Provides nursing care according to the agreed plan of care, professional standards, workplace policies and procedural guidelines.
Identifies and clarifies EN responsibilities for aspects of delegated care working in collaboration with the RN and multidisciplinary health care team.
Recognises own limitations in practice and competence and seeks guidance from the RN and help as necessary.
Refrains from undertaking activities where competence has not been demonstrated and appropriate education, training and experience has not been undertaken.
Acts to ensure safe outcomes for others by recognising the need to protect people and reporting the risk of potential for harm.
When incidents of unsafe practice occur, reports immediately to the RN and other persons in authority and, where appropriate, explores ways to prevent recurrence.
Liaises and negotiates with the RN and other appropriate personnel to ensure that needs and rights of people in receipt of care are addressed and upheld.
Standard 2: Practises nursing in a way that ensures the rights, confidentiality, dignity and respect of people are upheld
Places the people receiving care at the centre of care and supports them to make informed choices.
Practises in accordance with the NMBA standards codes and guidelines.
Demonstrates respect for others to whom care is provided regardless of ethnicity, culture, religion, age, gender, sexual preference, physical or mental state, differing values and beliefs.
Practises culturally safe care for (i) Aboriginal and Torres Strait Islander peoples; and (ii) people from all other cultures.
Forms therapeutic relationships with people receiving care and others recognising professional boundaries.
Maintains equitable care when addressing people’s differing values and beliefs.
Ensures privacy, dignity and confidentiality when providing care.
Clarifies with the RN and relevant members of the multidisciplinary healthcare team when interventions or treatments appear unclear or inappropriate.
Reports incidents of unethical behaviour immediately to the person in authority and, where appropriate, explores ways to prevent recurrence.
Acknowledges and accommodates, wherever possible, preferences of people receiving nursing care.
Standard 3: Accepts accountability and responsibility for own actions
Practises within the EN scope of practice relevant to the context of practice, legislation, own educational preparation and experience.
Demonstrates responsibility and accountability for nursing care provided,
Recognises the RN as the person responsible to assist EN decision making and provision of nursing care.
Collaborates with the RN to ensure delegated responsibilities are commensurate with own scope of practice.
Clarifies own role and responsibilities with supervising RN in the context of the healthcare setting within which they practice.
Consults with the RN and other members of the multidisciplinary healthcare team to facilitate the provision of accurate information, and enable informed decisions by others.
Provides care within scope of practice as part of multidisciplinary healthcare team, and with supervision of a RN.
Provides support and supervision to assistants in nursing (however titled) and to others providing care, such as EN students, to ensure care is provided as outlined within the plan of care and according to institutional policies, protocols and guidelines.
Promotes the safety of self and others in all aspects of nursing practice.
Standard 4: Interprets information from a range of sources in order to contribute to planning appropriate care
Uses a range of skills and data gathering techniques including observation, interview, physical examination and measurement.
Accurately collects, interprets, utilises, monitors and reports information regarding the health and functional status of people receiving care to achieve identified health and care outcomes.
Develops, monitors and maintains a plan of care in collaboration with the RN, multidisciplinary team and others.
Uses healthcare technology appropriately according to workplace guidelines.
Standard 5: Collaborates with the RN, the person receiving care and the healthcare team when developing plans of care
Develops and promotes positive professional working relationships with members of the multidisciplinary team.
Collaborates with members of the multidisciplinary healthcare team in the provision of nursing care.
Contributes to the development of care plans in conjunction with the multidisciplinary healthcare team, the person receiving care and appropriate others.
Manages and prioritises workload in accordance with people’s care plans.
Clarifies orders for nursing care with the RN when unclear.
Contributes to and collaborates in decision making through participation in multidisciplinary healthcare team meetings and case conferences.
Standard 6: Provides skilled and timely care to people whilst promoting their independence and involvement in care decision making
Provides care to people who are unable to meet their own physical and/or mental health needs.
Participates with the RN in evaluation of the person’s progress toward expected outcomes and the reformulation of plans of care.
Promotes active engagement and the independence of people receiving care within the healthcare setting by involving them as active participants in care, where appropriate.
Demonstrates currency and competency in the safe use of healthcare technology.
Exercises time management and workload prioritisation.
Recognises when the physical or mental health of a person receiving care is deteriorating, reports, documents and seeks appropriate assistance.
Standard 7: Communicates and uses documentation to inform and report care
Collects data, reviews and documents the health and functional status of the person receiving care accurately and clearly.
Interprets and reports the health and functional status of people receiving care to the RN and appropriate members of the multidisciplinary healthcare team as soon as practicable.
Uses a variety of communication methods to engage appropriately with others and documents accordingly.
Prepares and delivers written and verbal care reports such as clinical handover, as a part of the multidisciplinary healthcare team.
Provides accurate and appropriate information to enable informed decision making by others.
Standard 8: Provides nursing care that is informed by research evidence
Refers to the RN to guide decision making.
Seeks additional knowledge/information when presented with unfamiliar situations.
Incorporates evidence for best practice as guided by the RN or other appropriate health professionals.
Uses problem-solving incorporating logic, analysis and a sound argument when planning and providing care.
Demonstrates analytical skills through accessing and evaluating healthcare information and quality improvement activities.
Consults with the RN and other relevant health professionals and resources to improve current practice.
Standard 9: Practises within safety and quality improvement guidelines and standards
Participates in quality improvement programs and accreditation standards activities as relevant to the context of practice.
Within the multidisciplinary team, contributes and consults in analysing risk and implementing strategies to minimise risk.
Reports and documents safety breaches and hazards according to legislative requirements and institutional policies and procedures.
Practises safely within legislative requirements, safety policies, protocols and guidelines.
Standard 10: Engages in ongoing development of self as a professional
Uses EN standards for practice to assess own performance.
Recognises the need for, and participates in, continuing professional and skills development in accordance with the NMBA’s Continuing professional development registration standard.
Identifies learning needs through critical reflection and consideration of evidence-based practice in consultation with the RNs and the multidisciplinary healthcare team.
Contributes to and supports the professional development of others.
Uses professional supports and resources such as clinical supervision that facilitate professional development and personal wellbeing.
Promotes a positive professional image.
Benner’s Stages of Nursing Expertise
Stage I. Novice | No experience (nursing student). Performance is limited, inflexible and governed by context-free rules and regulations rather than experience. |
Stage II. Advanced beginner | Demonstrates marginally acceptable performance. Recognises the meaningful ‘aspects’ of a real situation. Has experienced enough real situations to make judgments about them. |
Stage III. Competent practitioner | Has 2–3 years’ experience. Demonstrates organisational and planning abilities. Differentiates important factors from less important aspects of care. Coordinates multiple complex care demands. |
Stage IV. Proficient practitioner | Has 3–5 years’ experience. Perceives situations as wholes rather than in terms of parts, as in Stage II. Uses maxims as guides for what to consider in a situation. Has holistic understanding of the individual, which improves decision making. Focuses on long-term goals. |
Stage V. Expert practitioner | Performance is fluid, flexible and highly proficient. No longer requires rules, guidelines or maxims to connect an understanding of the situation to appropriate action. Demonstrates highly skilled intuitive and analytic ability in new situations. Is inclined to take certain action because ‘it felt right’. |
Continuing professional development
From 1 July 2010, Enrolled and Registered Nurses and midwives and nurse and midwife practitioners have been required to meet the Continuing Professional Development (CPD) Standard set by the NMBA:
Under this standard nurses are required to participate in at least 20 hours of CPD per year (nurses who are also registered as midwives must complete 20 hours as a nurse and 20 hours as a midwife)
One active hour of learning equals 1 hour of CPD
CPD must be relevant to the context of practice
Written documentation must be kept to demonstrate evidence of a minimum of 20 hours of CPD per year
Compulsory annual in-services can count towards CPD (e.g. annual infection control, CPR, fire training)
Audits are conducted annually by the board on a number of nurses and midwives in Australia
CPD activities can include attending conferences, seminars, courses and in-services, meetings, reading a journal article and reflecting on it, watching and reflecting on webinars.
Documenting CPD
Developed a learning plan based on learning needs (i.e. relevant to your context of practice)
Identified and prioritised learning needs based on an evaluation of practice against competency or professional practice standards
Participated in effective learning activities that are relevant to learning needs
Reflected on the value of learning activities and their effect on your practice.
Purposes of nursing theories and conceptual frameworks
In clinical practice:
Assist nurses to describe, explain and predict everyday experiences
Serve to guide assessment, intervention and evaluation of nursing care
Provide a rationale for collecting reliable and valid data about the health status of individuals, which are essential for effective decision making and implementation
Help to establish criteria to measure the quality of nursing care
Help build a common nursing terminology to use in communicating with other health professionals. Ideas are developed and words defined
Enhance autonomy of nursing by defining its own independent functions
In education:
Provide a general focus for curriculum design
Guide curricular decision making
In research:
Offer a framework for generating knowledge and new ideas
Assist in discovering knowledge gaps in the specific field of study
Offer a systematic approach to identify questions for study, select variables, interpret findings and validate nursing interventions.
Overview of selected nursing theories (-)
Henderson Theory’s 14 basic needs that provide a framework for nursing care.
Breathe normally
Eat and drink adequately
Eliminate by all avenues of elimination
Move and maintain a desirable position
Sleep and rest
Select suitable clothing; dress and undress
Maintain body temperature within normal range
Keep the body clean and well groomed
Avoid dangers in the environment
Communicate with others
Worship according to faith
Work at something that provides a sense of accomplishment
Play or participate in various forms of recreation
Learn, discover or satisfy the curiosity that leads to normal development and health.
Behavioural System Model’s collection of behavioural subsystems that interrelate to form a whole person:
Security-seeking behaviour
Nurturing-seeking behaviour
Mastery of oneself and one’s environment according to internalised standards of excellence
Taking in nourishment in socially and culturally acceptable ways
Ridding the body of waste in socially and culturally acceptable ways
Sexual and role identity behaviour
Self-protective behaviour.
Adaptation Model’s goals for nursing:
Meeting basic physiological needs
Developing a positive self-concept
Performing social roles
Achieving a balance between dependence and independence.
Roper, Logan and Tierney’s theory
Five main concepts
Activities of living
Factors affecting activities of living
Life span
Dependence–independence
The nursing process
The activities of living, which are the focus of the model, are:
Maintaining a safe environment
Communicating
Breathing
Eating and drinking
Eliminating
Personal cleansing and dressing
Controlling body temperature
Mobilising
Working and playing
Expressing sexuality
Sleeping
Dying.
Selected nursing theories and the nursing process
Orem’s general theory of nursing
Assessing
Involves collecting data about the individual’s capacities (knowledge, skills and motivation) to perform universal, developmental and health–deviation self-care requisites. Determines self-care deficits.
Diagnosing
Stated in terms of the individual’s limitations for maintaining self-care (a deficit in self-care agency).
Planning
Involves considering and designing, with the individual’s participation, an appropriate nursing system (wholly compensatory, partially compensatory, supportive-educative or a mix) that will help the individual achieve an optimal level of self-care (i.e. enhance the individual’s self-care agency).
Implementing
Assisting the individual by acting for or doing for, guiding, supporting, providing a developmental environment and teaching.
Evaluating
Determining the individual’s level of achievement in resolving self-care deficits and in performing self-care.
Roy’s adaptation model
Assessing
First-level assessment includes collecting data about output behaviours related to the four adaptive modes (physiological, self-concept, role function and interdependence modes).
Second-level assessment includes collecting data about internal and external stimuli (focal, contextual or residual) that are influencing the identified behaviours.
Diagnosing
Focuses on adaptation problems and uses one of three alternative methods:
Stating behaviours within one mode with their most relevant influencing stimuli
Clustering behavioural information and labelling it according to indicators of positive adaptation and a typology of common adaptation problems related to each mode. Roy provides a typology of indicators of positive adaptation and a typology of commonly recurring adaptation problems according to each of the four modes
Labelling a behavioural pattern when more than one mode is being affected by the same stimuli.
Planning
Setting goals in terms of behaviours the individual is to achieve and planning nursing interventions to promote the effectiveness of the individual’s coping mechanisms and adaptive behaviours.
Implementing
Altering and manipulating the focal, contextual and residual stimuli by increasing, decreasing or maintaining them.
Evaluating
Determining the individual’s output behaviours with those identified in the goals.