Human Physio Cardiovascular
Cardiovascular system
- The Heart
- muscular pump that drives flow of blood to various organs
- Blood vessels
- conduit through which the blood flows
- Blood
- fluid that circulates around the body
- carrying materials to and from the cells
Blood flow through cardiovascular system
- Arteries take blood away from heart.
- Veins return blood to the heart.
- Series flow: blood travels trhough systemic and pulmonary circuits in series
- portal system: two capillary beds connected in series
Anatomy of the heart
- Located in thoracic/chest cavity between the lungs
- Pericardium - a double serous membrane
- Visceral pericardium - next to heart
- Parietal pericardium - outside layer
- Serous fluid fills the space between the layers of pericardium
Heart wall
Composed of three distinct layers
Epicardium
- connective tissue layer
- same as visceral pericardium
Myocardium
- cardiac muscle, thickest layer
Endocardium
- endothelium
- contains the Purkinje fibers

Heart chambers and Valves
- Four chambers
- Two atria receive blood returning to the heart from vasculature
- Two ventricles receive blood from atria and push the blood out of heart
- Heart valves
- Promotes unidirectional blood flow
- Atrioventricular (AV valves) - between atria & ventricles
- Semilunar valves - between ventricles and arteries
Path of blood flow
- Blood comes into the right atrium from the body
- Moves into the right ventricle
- Pushed into the pulmonary arteries in the lungs.
- After picking up oxygen, the blood travels back to the heart through the pulmonary veins into the left atrium
- Into to the left ventricle and
- Out to the body's tissues through the aorta.
Electrical conduction in the heart
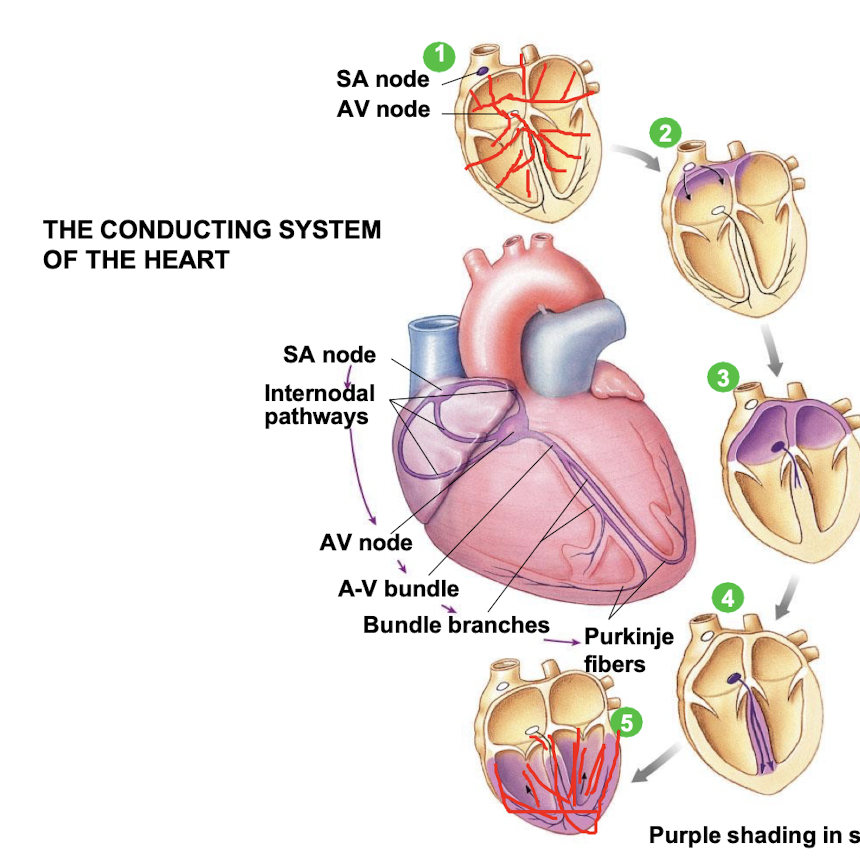
- SA node depolarises
- Electrical activity goes rapidly to AV node via internodal pathways
- Depolarisation spreads more slowly across atria. Conduction slows through AV node.
- Depolarisation moves rapidly through ventricular conducting system to the apex of the heart.
- Depolarisation wave spreads upward from the apex.
Control of heart rate
- Both SA node and AV node - capable of generating spontaneous action potentials
- SA node usually sets the pace of heartbeat
- fires more frequently than AV node (70 impulses/min compared to 50 impulses/min)
- cells in AV node stimulated by impulses coming from SA node → go into refractory period
- If SA node fails to fire or if impulses from it are blocked, the AV node can take over
Electrocardiogram (ECG)
P wave
- Atrial depolarisation
QRS complex
- Ventricular depolarisation and atrial repolarization
T wave
- Ventricular repolarization

P-Q interval
- conduction through AV node
Q-T interval
- ventricular systole (contracting)
T-Q interval
- ventricular diastole (relaxing)
R-R interval
- one heart beat
Cardiac Cycle
- Events associated with flow of blood through the heart during a single complete heartbeart
- various phases in the pumping action of heart
- periods of valves opening and closure
- changes in atrial, ventricular and aortic pressire
- changes in ventricular volume
- two major heart sounds
Phases of cardiac cycle
The heart cycles between contraction (systole) and relaxation (diastole)

- Late diastole - both sets of chambers are relaxed and ventricles fill passively.
- Atrial systole - atrial contraction forces a small amount of additional blood into ventricles.
- Isovolumic ventricular contraction - first phase of ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves.
- Ventricular ejection - as ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected
- Isovolumic ventricular relaxation - as ventricles relax; pressure in ventricles falls, blood flows back into cusps of semilunar valves and snaps them closed.
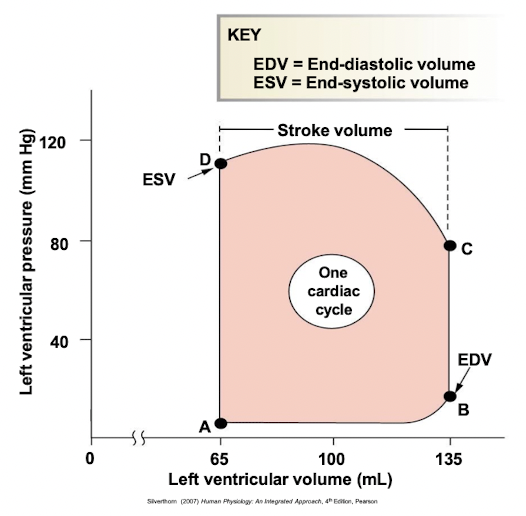
Pressure-volume curve
Left ventricular pressure-volume changes during one cardiac cycle
Stroke volume = EDV - ESV (70ml, at rest)
Cardiac output and control
- Cardiac output (CO) = volume of blood pumped by one ventricle per minute
- [[CO = HR x SV (heart rate x stroke volume)[[
Factors affecting cardiac output:
- determined by heart rate, stroke volume or both
SV is directly correlated with CO, the greater the SV the greater the CO.
SV represents the difference in the amount of blood between: EDV and ESV
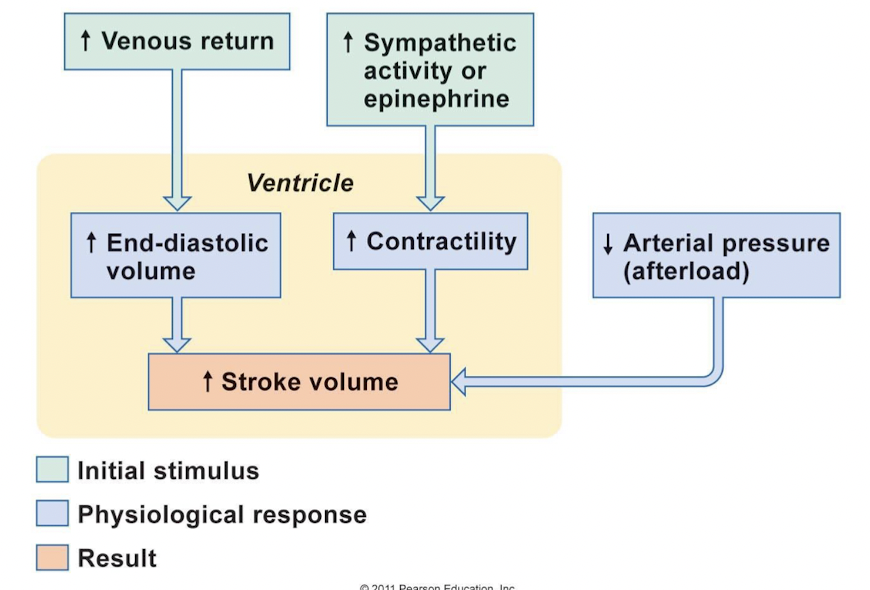
Control of stroke volume
- Stroke volume (SV)
- {{volume of blood pumped per ventricle per contraction{{
- directly related to force generated by cardiac muscle during contraction
- Primary factors affecting stroke volume:
- end-diastolic volume (EDV)
- ventricular contractility (force of contraction)
- Preload (relate to EDV, degree of muscle stretch)
- Afterload (pressure needed to eject blood out)
Ventricular contractility
- Contractility
- intrinsic ability of muscle fiber to contract at any given fiber length
- function of Ca2+ interaction with contractile filaments
- increase in contractility will increase stroke volume
- Ionotropic agent
- chemical that affects contractility → ionotropic effects
- positive ionotropic effects - e.g. catacholamines (sympathetic stimulation) and drugs enhance contractility
End-diastolic volume (EDV)
- volume of blood at the beginning of contraction (EDV) - determine the length of muscle
- preload - degree of myocardial stretch before contraction begins
- stretch of ventricular myocardium increases
- SV increases (length-tension relationship)
- Intrinsic control of cardiac function
- Relationship between EDV and SV
- Frak-Starling law of the heart
Frank-Starling law of the heart: Heart automatically adjusts its output to match EDV.
Increased EDV stretches muscle fibers.
- fibers closer to optimum length
- optimum length = greater strength of contraction
- increased SV
Factors affecting EDV
- primarily determined by end-diastolic pressure (preload)
- preload increases, EDV increases and SV increases
- preload affected by:
- filling time - depends upon heart rate
- atrial pressure - resulting from venous return and atrial contraction
- factor influencing venous return is central venous pressure
- central venous pressure rises, venous return increases, leads to increase in EDV
Summary of factors affecting stroke volume
Summary
- [ ] Relate phases of ECG to events of cardiac cycle
- [ ] Describe cardiac function and nervous system control of the heart
- [ ] Describe blood flow, volume and pressure in relation to the control of cardiac function