Indications for ABG investigations - Sudden unexplained dyspnoea
- Cyanosis
- Abnormal breath sounds
- Severe unexplained tachypnoea
- Excessive accessory muscle use
- Changes in mechanical ventilator settings
- Cardiopulmonary resuscitation
- Abnormal CXR findings
- Nasal flaring
- Changes in cognition
| Terminology of ABG analysis - pH = degree of alkalinity or acidity in blood
- PaCO2 = partial pressure of dissolved CO2 in plasma
- PaO2 = partial pressure of dissolved O2 in blood
- HCO3 = level of bicarbonate in blood
- SaO2% = percentage of haemoglobin saturated with oxygen (arterial oxygen saturation)
| Acidosis = ↓ pH - Depression of CNS (lethargic/disorientated = coma)
Alkalosis = ↑ pH - Over excitability of CNS and peripheral nerves (muscle spasms)
pH normal range: 7.35-7.45 |
Respiratory aspect of acid-base imbalances - Compensated for by kidneys
Normal range for PaCO2 = 35-45 mmHg |
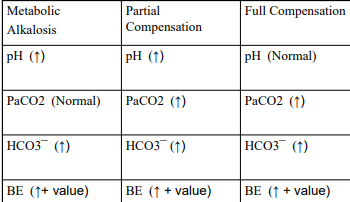
Metabolic aspect of acid-base disorders HCO3- normal ranges: 22-26 mmol/l - HCO3 ↓: pH ↓ = metabolic acidosis
- HCO3 ↑: pH ↑ = metabolic alkalosis
- Compensated for by adjustment in ventilation
| Buffer system - Measurement reflecting non-respiratory portion of acid-base balance
- Base excess (BE) normal ranges: -2 to +2
- + value = base added or acid removed
- value = acid added or base removed
|
Oxyhaemoglobin dissociation curve 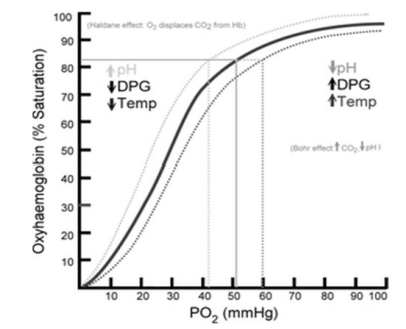 |
Clinical presentation of CO2 retention  | Clinical presentation of CO2 loss 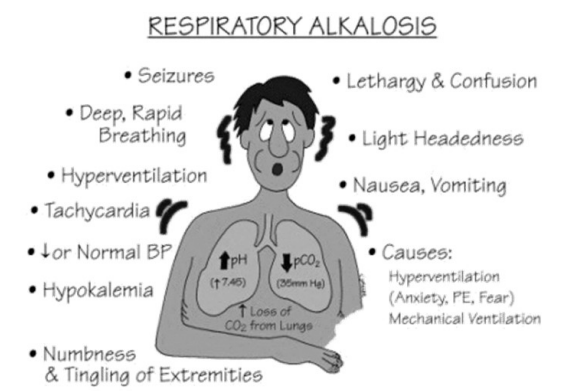 |
Clinical presentation of metabolic alkalosis 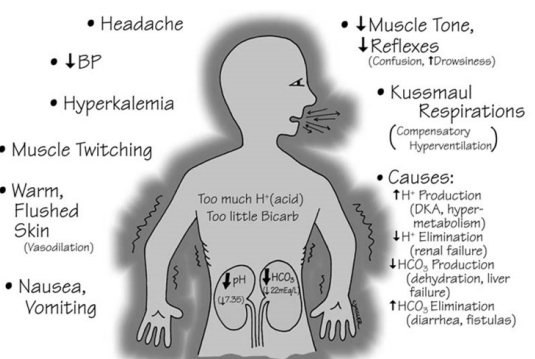 | Clinical presentation of metabolic acidosis 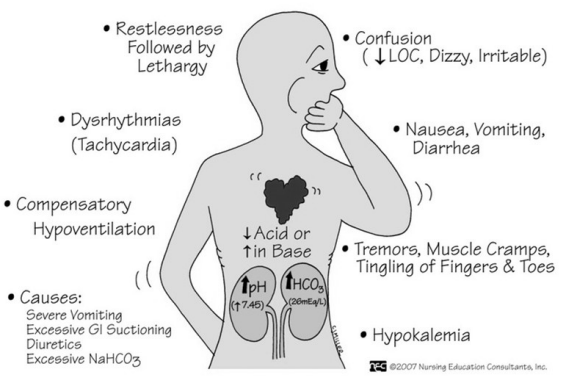 |
Oxygenation - PaO2 = arterial
- PAO2 = alveoli
PAO2 determined by: - Ventilation
- Inspired oxygen (FiO2)
- Atmospheric pressure
PaO2 determined by: - Age: Expected PaO2 = 100.1 – [0.323 x age in years]
- Concentration gradient from O2 in alveolus to capillary
- Width of alveolus capillary membrane → Interstitial lung disease, fibrosis
- Surface area available for diffusion → emphysema (dilated A), pneumonia, atelectasis
Oxygenation relies on: - Association and dissociation of haemoglobin with oxygen
- Red blood cells count and prober Hb concentration
Tissue perfusion | Normal PaO2 – room air - > 80 mmHg = normal
- 70-80 mmHg = mild hypoxemia
- 60-70mmHg = moderate hypoxemia
- < 60mmHg = severe hypoxaemia
Normal PaO2 – oxygen therapy - >100 mmHg = normal
- 80-100 mmHg = mild hypoxemia
- 70 – 80 mmHg = moderate hypoxemia
- < 70 mmHg = severe hypoxemia
|
Oxygen saturation - Extent to which Hb in arterial blood is saturated with oxygen (SaO2)
- SaO2 – measurement collected from arterial blood gas print out.
- SpO2 – measurement collected from pulse oximeter (noninvasive)
- Normal range: > 97%
| Steps to take when analysing an ABG - Review all clinical data from file
- Review previous ABG’s
- pH: 7.4 - Acidosis or alkalosis
- PaCO2: 35-45 mmHg (↑/↓)
- HCO3: 22-26 mmol/l (↑/↓)
- PaO2 not related to acid-base balance (will guide oxygen therapy)
| Compensation of acid-base disturbance - Primary respiratory problem - pH & PaCO2 move in opposite direction
- Primary metabolic problem – pH & HCO3 ¯ move in the same direction
- Partial compensation - pH still abnormal but other system begins to compensate (PaCO2 or HCO3 ¯)
- Full compensation - pH restored to normal
|
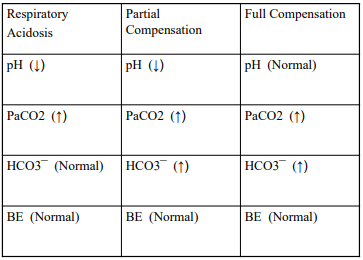  | Causes of ABG abnormalities Respiratory acidosis - primary reduction in alveolar ventilation relative to CO2 production Causes: - Respiratory
- Acute upper airway obstruction e.g. asphyxia
- Massive pulmonary oedema
- Thoracic traumatic injuries
- Non-respiratory
- Drug overdose causing hypoventilation
- Neurological conditions (Guillian Barre syndrome, Myasthenia Gravis, Spinal Cord injury)
|
Causes of ABG abnormalities Respiratory alkalosis - primary ↑ in alveolar ventilation relative to CO2 production Causes: - Hyperventilation (anxiety)
- Asthma
- Mechanically ventilated pts- large minute volumes
|
Causes of ABG abnormalities Metabolic acidosis - Firstly, buffers lost excessively/not produced sufficiently/ secondly, ↓ ability to excrete acids Causes: - ↑ in metabolic acid production – Ketoacidosis/Lactic Acidosis
- Loss of HCO3 ¯ (Buffers)- Diarrhoea
|
Causes of ABG abnormalities Metabolic alkalosis - Abnormal nr of HCO3¯ accumulate in blood / abnormal nr of H+ ions lost from the plasma) Causes: - Nasogastric suction (loss of stomach acid)
- Persistent vomiting (loss of stomach acid)
- Diuretic therapy
- Excessive administration of NaCO3
- Volume depletion
| Venous blood gas analysis Normal: - pH = 7.31-7.41
- PO2 = 37-42mmHg
- PCO2 = 42-50mmHg
|
NORMAL VALUES - pH = 7.35-7.45
- PaCO2 = 35-45mmHg
- HCO3 = 22-26 mmol/l
- BE = -2 to +2
- PaO2 = within notes!
- SpO2 = pulse oximeter
- SAO2 = from ABG
|
- Refers to therapeutic application of O2 at [conc] > room air (Room air = 21% O2 or FiO2 0.21).
- Assists with ↑ alveolar O2 conc.
- Used to prevent/treat hypoxemia
- Hypoxemia = abnormal low oxygenation of arterial blood. Caused by hypoventilation, diffusion abnormalities, ↓ FiO2 (e.g. high altitudes) and HB deficiencies, PaO2 is low, elevated lactate values
- Hypoxemia determined by arterial blood gas analysis (PaO2 & SaO2)/ pulse oximeter reading (saturation <90% = severe)
- Hypoxemia progress to hypoxia = insufficient O2 availability at tissue level
- Hypoxemia = PaO2 < 60mmHg or SaO2< 90% (severe hypoxemia)
- Clinical scenarios: acute illness e.g. pneumonia, following trauma, after myocardial infarction, short-term use following surgery and chronic conditions e.g. chronic heart failure & COPD
- Oxygen therapy is medically prescribed e.g. device to be used & % of O2 to be given
- Physiotherapy documentation should thus clearly indicate the device, flow rate & O2% observed during treatment
- Effect of oxygen therapy should be closely monitored overtime e.g. ABG results and/or pulse oximetry (SpO2)
| Clinical relationship between SaO2 and PaO2 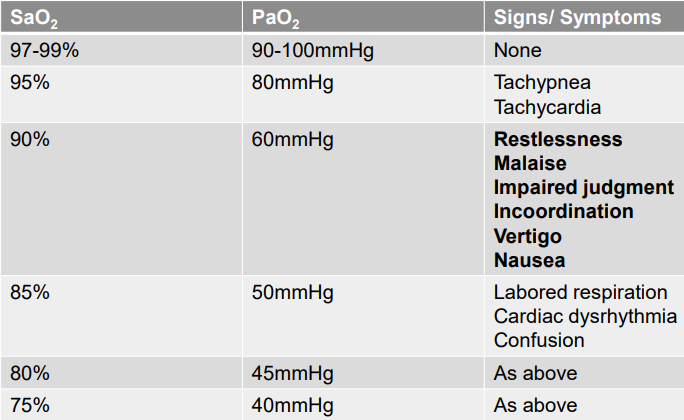 |
Complications of oxygen therapy - Impaired respiratory drive-in hypercapnia COPD
- Oxygen toxicity → stiff lung syndrome
- Blindness in Children
- Absorption atelectasis in mechanical ventilated pts.
- Drying of mucous membrane
- Pt dependency
- Fire/explosion hazard
|
Delivering oxygen therapy: - O2 source
- Flow meter
- O2 delivery device
|
Oxygen delivery systems: spontaneously breathing pts: 1) Variable performance devices, 2) Fixed performance devices, 3) Enclosure systems |
- Variable performance devices
- Deliver O2 at relatively low flow rates e.g. 2-15 L/min.
- Sensitive to pt’s ventilation pattern and resp rate.
- Not possible to accurate predict the FiO2 delivered by these devices.
- FiO2 ↑ by approximately 4% for every 1 L/min ↑ in O2 flow
Example: FiO2 as per flow rate - Room air = 21% O2
- 1 L/min provides 24% O2
- 2L/min provides 28% O2
- 3 L/min provides 32% O2
- 4L/min provides 36% O2
Variable performance devices – nasal cannula - Consist of two soft prongs, 1 cm long, that is inserted in the ant nares & connected to O2 source via narrow bore tubing.
- Pt’s nasopharynx acts as reservoir making this device sensitive to the pt’s resp rate.
- Used at a flow rate of 0.25-6L/min.
- Flow rate > 4L/min often result in nasal dryness – humidification needed
Variable performance devices – simple oxygen devices - Plastic device which covers mouth & nose and has exhalation ports on the sides of the mask.
- The air inlet is at the base of the mask which is connected with narrow bore tubing to the oxygen source.
- Room air is entrained through the inlet into mask as O2 enters thus ↑ the total flow delivered
- Additional room air may enter the mask through the exhalation ports.
- The mask acts as a reservoir between pt breaths.
- Used when a flow rate of 5-10L/min is required.
- Thus able to provide +/- 40%-60% of oxygen
Variable performance devices – reservoir masks - Partial rebreathing mask and non-rebreathing mask
- Like simple O2 mask, but has 1l reservoir bag but with non-rebreathing mask has additional one-way valves
- Reservoir bag ↑ the reservoir volume thus the potential for higher FiO2 occurs
Partial rebreathing mask - O2 flows to pt during inhalation but during exhalation source O2 & the 1st 1/3 of expired air enters the reservoir bag. This expired air consists of high O2 content and low CO2 as it was the air in the anatomical dead space.
- As the bag fills, the last 2/3 of expired air (high in CO2) passes through the exhalation ports.
- O2 flow during inspiration should be sufficient to prevent bag deflation to minimize CO2 inhalation.
- Reservoir bag should remain at least 1/3 to ½ full on inspiration, not completely deflate.
- If the flow rate is ≥ 10L/min it could provide 40-70% oxygen concentration.
Non-rebreathing mask - A one-way valve is positioned between reservoir bag and mask to prevent exhaled air entering the bag.
- Two one-way valves are position at the exhalation ports.
- During inhalation, negative mask pressure closes the two valves over the exhalation ports preventing air entering the mask but opens the valve at the base of the mask allowing oxygen delivery.
- During exhalation the reverse occurs.
- When flow rate is ≥ 10 L/min the device may provide oxygen concentration of 60-90%.
| - Fixed performance devices
- Delivers relatively high gas flows, aimed to equal/exceed the pt’s peak inspiratory flow
- Thus resulting in know or fixed FiO2
- E.g. = venturi mask (air entertainment mask)
- Masks of Venturi mask has large exhalation port at each side of mask
- Connected to base of mask is a 10cm corrugate tube which is then connected to an adapter.
- This adapter contains narrow jet orifice surrounded by an air entrainment port or cage.
- The source of O2 flows through narrow jet orifice at a high velocity.
- Air enters the entrainment port/cage due to shearing forces at the boundary of the jet flow.
- This entrained air dilutes the gas delivered to the mask.
- The total flow delivered depends upon the jet orifice diameter, the flow of the gas and the cross-sectional area of the entrainment port/cage
- Different adaptors are available and O2 concentrations of 24-60% can be delivered.
- Indicated flow rate is proved at the base of the adaptor.
- Humidification is not done if flow less than 4 l/min due to interfering with O2 delivery
- Often used for hypercapnia COPD pts
|
- Enclosure systems
- Oxygen delivery to infants and children
- Examples: oxygen tents, oxygen hoods, incubators
|
Domiciliary oxygen therapy - When a pt requires O2 therapy at home.
- Includes:
- Long-term oxygen therapy (LTOT) – oxygen delivered for ≥ 18hours per day, flow rate set to maintain a PaO2 level > 60mmHg & SpO2 > 90% on waking rest.
- Nocturnal oxygen therapy (NOT) e.g. prescribed for those with lung disease who desaturate to SpO2 ≤ 88% for > 1/3 of the night.
- Ambulatory O2 therapy e.g. individuals on LTOT that require O2 therapy needed during ambulation.
|
Assessment for home oxygen: - Pulse oximetry measurement < 92% = useful as screening tool
- ABG done to determine & assess eligibility of LTOT.
- LTOT is indicated:
- Stable daytime partial arterial oxygen concentration (PaO2) is ≤ 55 mm Hg (7.3 kPA) at rest or
- Stable daytime PaO2 is 56–59 mm Hg (7.4–7.8 kPa) and there is evidence for hypoxic organ damage (including right heart failure, pulmonary HPT, or polycythaemia)
| Domiciliary oxygen therapy cont. - Systems include oxygen concentrators, compressed gas cylinders, liquid oxygen systems
- Delivery devices are usually nasal cannula
Oxygen concentrators – electric device that uses molecular sieve to separate O2 from nitrogen in room air Compressed gas cylinders - Most common used device
- Cylinder positioned in trolley
- Disadvantages – heavy, requires regular delivery, and changing of regulator
Liquid oxygen systems - Consists of large stationary unit where small canisters can be filled with liquid O2
- Limited by cost & requires deliveries
| Contraindications for home oxygen therapy Not given to: - Pts with severe cardiopulmonary disease who complains of dyspnoea, but who maintain PaO2 > 60 mmHg.
- Pt’s who continue to smoke cigarettes due to ↑ fire risk & probability that the poorer prognosis conferred by smoking will offset treatment benefit.
- Pt’s who have not received adequate therapy for underlying medical condition(s) responsible for causing hypoxaemia.
- Pts who are not sufficiently motivated to undertake the discipline required in using oxygen therapy for the prescribed number of hrs per day.
|
General physiotherapy considerations with oxygen therapy - If pt is receiving continues O2 on the ward, treat at the bedside if portable oxygen isn’t available.
- Document device & supplemental O2 used during physiotherapy interventions.
- Ensure device is fitted correctly and flow of O2 as should be according to order and specific device.
- Monitor the pt’s skin for potential breakdown due to pressure from mask of cannula. Provide appropriate padding without interfering with fit of device.
- Observe mask for accumulation of sputum & clear/change if needed.
|
Perioperative period - Time lapse surrounding a surgery
- Divided into preoperative, intraoperative/ operative, postoperative
- Depending on the specific surgery & pt presentation PT services may be involved in pre- & post- operative period.
- Enhanced recovery after surgery (ERAS) is pt-centred, evidence-based, MDT approach to optimise outcomes following surgery
| Pre-operative physiotherapy - Intervention prior to a surgical procedure.
- Can start before hospital admission (Prehabilitation) or during hospital admission prior to surgery
Aims for pre-operative physiotherapy - Prevent/minimize adverse physiological changes associated with major surgical procedures
- Educate pt on role of PT and post-op recovery
| Indications for pre-operative physiotherapy - Indicated for pts at risk of developing post-op pulmonary (PPC) complication e.g. basal segment collapse, atelectasis, poor cough effort, DVT → PE
Prehabilitation - Strategies implemented prior to elective surgeries that aim to improve pts’ capacity to withstand anticipated stressors, improve post-op outcomes & ↓ postoperative risk.
- Exercise programmes focused on strength training, improving exercise tolerance, optimising diet, and ↓ worry
- Exercise programme can be group class or home programme
- Programmes:
- 3-7 days per week, 2-4 weeks in length before elective surgeries
- Includes education, breathing exercises, respiratory muscle strengthening & exercises to improve aerobic exercise capacity
- Ideal exercise intensity – 40%-70% of HRmax
|
What are post-op pulmonary complications? (PPC) - Any complication affecting resp system following anaesthesia & surgery e.g. respiratory infections, atelectasis etc.
- Impact of PPC
- Mortality ↑ in short & long term.
- Length of hospital stay ↑.
- Hospital costs ↑.
| Factors increasing the risk of PPC Pt centred factors - Age (individual > 60 years of age)
- Frailty - ↓ fx status
- Smoking status
- Acute respiratory infection in last month
- Comorbidities
- Overweight/ Obesity/ Diabetes/ HPT
- Chronic respiratory disease (COPD & Asthma) or Congestive Heart Failure or CVA history
Other factors - Duration of surgery & time of anaesthesia (> 2 hours)
- Surgery type - ↑ risk:
- Open vs laparoscopic
- Abdominal surgery (Upper > Lower), thoracic surgery, neck surgery, neurosurgery, and major vascular surgery.
- Emergency vs elective
- Re-operations
|
Pre-op physiotherapy principles - Introduce self to gain trust & ↓ anxiety levels of pt.
- Assess pt’s risk for developing PPC
- Assess pt with special focus on the pt’s fx status, muscle strength & exercise tolerance
- Education on following aspects:
- Role of physiotherapy
- Probable site of surgical incision and precautions
- Presence of medical equipment e.g. drips
- Effects of anaesthesia
- Importance of optimal post-op positioning & early mobilization
- Maximize pulmonary fx pt:
- Teach supported coughing as appropriate to surgical site
- Deep breathing exercises and inspiratory muscle training
- Teach circulatory exercise to assist with prevention of DVT’s e.g. ankle pumps and static quadriceps.
- When assess and respiratory symptoms present – full cardiopulmonary treatment indicated.
|
Definition of surgical procedures - Open-thoracotomy - surgical incision in chest wall to open & gain access to thoracic cavity to explore, biopsy or treat lesion.
- Laparotomy - surgical incision through abdominal wall to gain access to the abdominal cavity to explore & correct any structural injury.
- Median sternotomy - surgical incision made through sternum to gain access to mediastinum to correct any structural abnormality.
|
Thoracotomy Three basic approaches: - Posterior lateral thoracotomy
- Latissimus dorsi, serratus ant, rhomboid, trapezius
- Painful + and shoulder muscle dysfunction
- Muscle sparing thoracotomy
- Sparing of latissimus dorsi & serratus ant
- ↓ pain & shoulder dysfx
- Limited anterior and lateral thoracotomy
- Small incision over ant chest wall
- Dissection of pectoralis maj and min
- Approaches dependent on surgeons’ preference & aim
|
Indications for thoracotomy surgery - Thoracic trauma e.g. flail chest, rupture diaphragm, rupture pericardium
- Lung cancer
- Localized bronchiectasis
- Severe COPD e.g. lung reduction surgery
- Empyema e.g. decortication
|
Common thoracic surgical procedures - Lobectomy – removal of one or two lung lobes
- Pneumonectomy – removal of entire lung
- Sleeve resection – resection of upper lobe together with sleeve of the main bronchus to preserve the lung tissue
- Removal of a lung segment
- Removal of wedge section of lung
- Pleurectomy – partial stripping of the parietal pleura
- Pleurodesis (surgical) – application of irritant to pleura
- Decortication – removal of thickened pleura/drainage of pus
- Oesophagectomy – removal of part/entire oesophagus
- Oesophagogastrectomy – removal of the lower portion of the oesophagus and the stomach
| Abdominal surgery - Minimal access surgery e.g. laparoscopic procedures.
- Laparoscopic procedures are less invasive & pts recover faster with less risk of PPC developing.
- Conventional laparotomy through ‘open’ incision ↑ risk for PPC
‘Open abdomen’ - Indiv had laparotomy performed but incision wasn’t closed with sutures
- Abdominal cavity closed with vacuum dressing attached to suction source to allow for drainage
| Indications for laparotomy - Elective surgery e.g. rectal cancer (anterior resection)
- Abdominal trauma
- Explorative surgery due to blunt trauma
- Penetrating trauma
|
Indications for median sternotomy - Obstruction in coronary arteries e.g. CABG
- Thoracic trauma e.g. stab wound to chest wall involving mediastinum
- Fractured sternum with instability
|
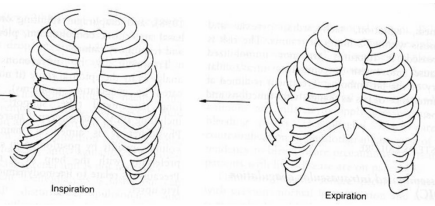
Effects of surgery on respiratory process - Lung volumes
- ↓ vital capacity and FRC
- VC [40% less] & FRC [70% at 24hrs post-op]
- Changes may persist to 5-10 days post op
- Respiratory muscle function
- Diaphragmatic excursion ↓
- V/Q mismatch & hypoxemia commonly occur
- Mucociliary clearance & cough effectiveness ↓
- PPC may develop in high-risk pts.
- Effects on the resp system = combination of result of anaesthesia, surgery performed, pain levels of individ & physical inactivity post-op
|
Effects of anaesthesia - ↓ mucociliary activity (paralysing effect on cilia)
- Dehydration if high flow O2 used causing sputum retention
- Basal atelectasis due to intubation, positioning during surgery & use of paralyzing agents during surgery
- Hypoxemia, severe cases hypoxia
| Post-operative presentation - Pain
- Pt may present with slight pyrexia
- Nasogastric tube
- IV lines
- Wound Drains
- Urine catheter
- Monitoring devices
|
Management of post-op pain - To ↓ physiological symptoms e.g. tachycardia/HPT
- ↓ secondary resp dysfunction by ↑ tidal volumes & effective coughing
- Allow pts to start with mobilisation
|
Methods of pain relief - Intramuscular
- Intravenous
- Epidural (Catheter inserted into thoracic/lumbar epidural space)
- Peripheral blocks e.g. intercostal nerve block, intra-pleural analgesia
- Pt controlled analgesia (PCA)
- Pt controlled epidural analgesia (PCEA)
| Self-study portion: Main and Denehy – table 11.3 (pg. 527), table 11.5 (pg. 528-231) Main and Denehy – post-op pain and pharmacological management (pg. 516-521) |
Basic aims of port-op PT - Assess for signs of PPC
- Re-inflation of collapsed lung
- Maintain adequate ventilation
- Removal of excess secretions & improve pt’s cough effort
- Monitor humidification & O2 therapy
- Monitor analgesia
- Bed mobility (moving in bed, transfer comfortable supine to sit)
- Early mobility out of bed
- Prevent joint stiffness and posture re-education
Relate these to case study | Assessing for PPC: Melbourne Group Scale (MGS) PPC diagnosed in presence of 4/more - Arterial de-saturation on room air (SpO2 < 90%)
- CXR reports atelectasis/ consolidation
- ↑ temperature > 38⁰ with no signs of infection outside lungs
- Sputum [yellow/green] differing from preoperative status
- Infection signs on sputum microbiology
- ↑ WBC >11.2 x 109 L or admin of post-op resp antibiotics
- Diagnosis of pneumonia/chest infection by physician
- Readmission to ICU/high care due to respiratory problems/ abnormal breath sounds
| Post-op physiotherapy - Assess & id problems to guide selection of treatment
- Techniques could include:
- Deep breathing exercises
- Supported coughing
- Nebulization
- Early mobility out of bed to improve V/Q matching
- TENS to manage pain with thoracotomy & laparotomy pts
- UL & trunk movements.
- Inspiratory muscle training against resistance
- PEP devices to assist with sputum clearance
- Home exercises to ↑ activity level & improve exercise tolerance after discharge
|
Key points of managing post-op pt during physiotherapy - Always assess if pain is adequately managed e.g. monitor pain levels with VAS
- Note if pt has pinpoint pupils and is drowsy
- Check vital signs & O2 saturation
- If pt had spinal block/epidural for pain mx, always assess motor & sensory fx of LL, especially before mobilizing!
- Liaise with medical team regarding mobilization orders.
- Ensure adequate length in tubing when moving pt
- Don’t kink lines
- If pt has any drainage tubes attached observe for leakage prior to moving a pt
- Take note of urine catheter during activity
- If positioning pt ensure tubes, catheter is supported
- Mobilise pts with shoes/barefoot but never on socks
- Stand close to pt when mobilizing for the first time
- Teach supported coughing
- IV lines
- Is it running?
- Is their blood tracking in the line?
- Has the IV tissued?
| Physiotherapy precautions (thoracotomy) - Supported huffing & coughing
- If a pneumonectomy was performed, pt shouldn’t lie on non-operative side (operated side should be down if pt is able to lie on this side). To ↓ risk of fluid moving onto remaining lung & causing damage to anastomosis of bronchial stump. Check with the surgeon regarding local protocol for positioning pt in side-lying.
- Transfer pt out of bed over non-operative side.
- No manual chest clearance techniques directly on incision
- No head down tilting with PD
| Physiotherapy precautions (laparotomy) - Supported huffing and coughing
- No prone positioning
- No aggressive manual chest clearance techniques on anterior basal lung segment if pt has an ‘open abdomen’.
- Liaise with medical team regarding mobilisation orders
- Teach transferring from supine over the side-lying position
|
Physiotherapy precautions (median sternotomy) - Supported huffing and coughing
- When doing activities with the upper extremities above 90 degrees, done with bilateral arm movements. Below 90 you can use unilateral movements
- No prone positioning
- Support sternum with fx activities e.g. rolling in bed, moving from side-lying to sitting on EOB
- When assisting pt to move up in bed or stand up don’t use shoulder girdle as lever as bone formation is occurring at sternum. Support around thoracic cage
- Time for following sternotomy precautions will depend on pt, e.g. risk factors for sternal instability, comorbidities, and recovery period
|
Physiotherapy precautions (median sternotomy) - Support sternum during thoracic movements
- If pt requires upper extremity during fx activities, e.g. sit to stand, keep arms close to body.
- If pt wish to lift object keep upper extremity close to body. If pain felt at incision site, the weight is too much.
- Time for following sternotomy precautions will depend on pt e.g. risk factors for sternal instability, comorbidities & recovery period but is usually followed for 6 weeks
|
OLDCART Onset Location Duration Comorbidities Associated Radiation/referral Treatment |
Definition of lifestyle choices - Diseases of lifestyle = Non-Communicable Diseases (NCDs)
- Of long duration & slow progression.
- Main types of non-communicable diseases are cardiovascular disease, cancers, chronic respiratory diseases, and diabetes
- NCDs disproportionally affect low-and middle-income countries (2/3 of NCD deaths occur in these countries – 28 million)
| Role of physiotherapy - Provide evidenced-based intervention to prevent and address NCDs through the following:
- Providing evidence-based primary & secondary prevention programmes for mx of NCDs
- Promotion of health & wellness & improving quality of life
- Improving & maintaining physical activity & maintaining functional independence
| Risk factors for lifestyle diseases - HPT
- Diabetes
- Mellitus
- Obesity
- Metabolic syndrome
|
Hypertension - Elevated arterial BP abnormally sustained at rest.
- BP influenced by pain & anxiety, more than one reading required over time before given diagnosis
- Two general forms of hypertension exist:
- Essential/idiopathic HPT due to lifestyle behaviours
- Secondary hypertension due to other causes e.g. renal disease, pregnancy etc.
- HPT values differ at different age groups
|
HPT related to age groups  | Risk factors for HPT - Smoking
- Dyslipidaemia:
- total cholesterol > 5.1 mmol/L
- LDL > 3 mmol/L
- HDL men < 1 & women < 1.2 mmol/L
- Diabetes mellitus
- Men > 55 years, Women > 65 years
- Family history of early onset of CVD
- Waist circumference ↑: Men ≥ 94 cm, Women ≥ 80 cm
|
Clinical presentation of HPT - Normally asymptomatic
- Complains of headaches, blurred vision, dizziness
| Management of HPT - Effective mx important as it can lead to e.g. heart failure, stroke, and chronic renal failure.
- Lifestyle info given to all pts when BP is measured irrespective of abnormal readings.
|
Management of HPT include: - Lifestyle modification at all stages
- Drug therapy
| Drug therapy - Mono or combination therapy
- Combination therapy consists of:
- Diuretic
- Ca channel blocker
- ACE inhibitor
- Angiotensin receptor blocker
- B-blocker
See end of summary for drug table |
Physical activity/exercise - Physical activity = any body movement produced by contraction of skeletal muscles that results in ↑ caloric requirements above resting energy expenditure
- Exercise = type of physical activity that is planned, structured, and includes repetitive body movements to improve/maintain one or more components of physical fitness
| Classification of physical activity intensity 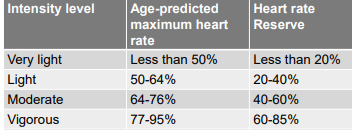 |
Classification of physical intensity 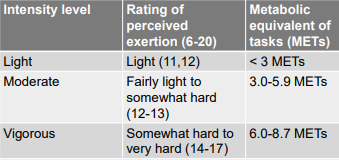 |
Metabolic equivalents - Functional activity defined according to O2 consumption required
- MET = ratio of rate of energy expended during activity to rate of energy expended at rest.
- 1MET = energy expenditure for sitting quietly.
- 1MET = 3.5ml oxygen per kg body weight
- A 4 MET activity expends 4 times the energy used by the body at rest.
- Metabolic equivalent activity charts
|
Public health physical activity recommendations - Adults move more & sit less throughout day. Some physical activity is better than none.
- Adults (18-64 years of age) 150 minutes of moderate intensity activity throughout the week/at least 75 mins of vigorous act throughout week/ equivalent combination of moderate- and vigorous-intensity activity.
- Can also perform a combination of moderate to vigorous activity during the week
- For additional health benefits moderate activity should ↑ to 300 minutes per week/vigorous to 150 minutes per week.
- Muscle strengthening on 2 or more days per week of major muscle groups.
- Don’t forget flexibility exercise
- MET minutes and Health Benefits depend mainly on total weekly energy expenditure due to physical activity.
- Suggested weekly range to achieve health benefits: 500 to 1,000 METminutes per week
- Example: If a person does a 4 MET activity for 30 minutes, he or she has done 4 x 30 = 120 MET-minutes (or 2.0 MET-hours) of physical activity.
- Example: If a person does a 4 MET activity for 30 minutes 3 times a week he or she has done 4 x 30 x 3 = 360 MET-minutes (or 6.0 MET-hours of physical activity
|
Physical activity vital sign - Screening to determine how much activity someone is doing
- On average, how many days per week do you engage in moderate to strenuous exercise (like a brisk walk)?
- On average, how many minutes do you engage in exercise at this level?
- Calculate the total minutes per week by multiplying the answers of the two questions (minutes per week).
|
Exercise considerations - Prescription to consider pt’s co-existent problems & health status e.g. orthopaedic problems.
- Aerobic exercise training should be the focus. Flexibility and strengthening activities can also be included.
- Use Borg scale to assess perceived exertion as medications my blunt HR response.
- Avoid Valsalva maneuver during resistance training – breath holding and straining
| Assessment for chronic lifestyle disease - Clinical hx of pt
- Aims of treatment (pt & practitioner)
- Medical management e.g. medications
- Other therapies e.g. dietician & psychologist
- Assessment of vital signs
- Physical assessment e.g. strength (1RM), physical activity level, exercise capacity, BMI, waist circumference, waist: hip ratio, stress levels etc.
- Outcome measures
| Exercise prescription for hypertension Aerobic and resistance training - Frequency: Aerobic most days of the week, resistance 2-3d/wk.
- Intensity: Moderate intensity
- Aerobic; 40-60% HRR or 60-75% HRmax or “moderate” level on perceived exertion scale
- Resistance; 60-80% 1-RM
- Time: 30-60 mins of continuous/ intermittent aerobic exercise & resistance, 8-12 reps for each of the major muscle groups
- Type: Aerobic exercises with resistance training
- Progression slowly in all components
|
Example of calculating HR max A 55-year-old man with stage 1 HPT 220 – 55 = Age-predicted maximum HR (HRmax) = 165 0.60 of 165 = 99 bpm 0.75 of 165 = 123.75 bpm Thus training range according to HRmax = 99 – 124 bpm | Example of calculating HRR A 55-year-old man with stage 1 HPT. Resting HR = 60 bpm Age-predicted maximum HR = 165 bpm HRR = HRmax – HRrest = 165 – 60 = 105 bpm Target HR = (40-60% of HRR) + RHR 105 x 0.40 = 42 + 60 = 102 bpm 105 x 0.60 = 63 + 60 = 123 bpm Thus range for training is 102 – 123 bpm | Diabetes mellitus (DM) - Metabolic disease characterized by ↑ blood glucose from defects in insulin secretion and/or an inability to use insulin.
- Elevates risk for cardiovascular disease & neuropathies (peripheral and autonomic).
- Type 1: destruction of beta cells in pancreas
- Type 2: ↑ cellular resistance to insulin, result in compensatory hyper-secretion of insulin that ultimate lead to failure in insulin production
|
Diagnosis and classification of DM - Other specific types - Genetic deficits of B-cell function, genetic deficits in insulin action, diseases in exocrine pancreas, endocrinopathies, drug/chemical induced, infections, other genetic syndromes characterised by diabetes e.g. down syndrome etc.
- Gestational diabetes: Hyperglycaemia (glucose intolerance) with onset or first recognised during pregnancy.
|
Diagnosis of DM - Presence of any one of the following three factors:
- Presence of polyuria, polydipsia, weight loss, blurred vision & random plasma glucose (regardless of last meal) of ≥ 200mg/dl (11.10 mmol/l).
- Fasting plasma glucose ≥ 126mg/dl (6.99 mmol/l) (no food intake for last 8 hours).
- Two-hour post load glucose ≥ 200mg/dl (11.10 mmol/l) using a 75g oral glucose load dissolved in water.
- Glycated hemoglobin A1c ≥ 6.5% (Specific requirements should be considered)
|
- Normal fasting plasma glucose ˂ 100mg/dl (5.55 mmol/l)
Management of DM include: - Nutritional therapy (Dietician consultation)
- Exercise therapy to control hyperglycaemia
- Education regarding foot care
- Drug therapy - Revise pharmacology notes
|
Foot care advice for pts with DM - Inspect feet daily for abrasions, blisters, and cuts. Use a mirror if soles cannot be seen. If poor vision, ask another person to check.
- Wash feet daily with lukewarm water and soap.
- Test temp of water with hands
- Dry feet carefully especially between toes.
- Apply hand cream to feet especially dry areas.
- Wear clean socks or stockings daily.
- Cut nails straight across & file down edges with an emery board.
- Wear comfortable shoes that fit and don’t rub.
- Inspect inside of shoes for any objects before putting on shoes
|
Diabetic keto-acidosis (DKA) - State of severe uncontrolled diabetes caused by insulin deficiency
- Characterized by hyperglycaemia, hyperketonaemia, and metabolic acidosis
- Caused by infections, new cases of DM, insulin error and insulin omissions
|
Symptoms of DKA - ↑ polyuria & thirst, weakness, drowsiness, abdominal pain, dehydration, hypotension, tachycardia, hypothermia, deep and rapid respiration (Kussmaul breathing pattern – rapid deep breaths)
- Odor of acetone on pt’s breath
- Blurred vision
- Leg cramps
- Nausea & vomiting
- Confusion
|
Management of type 1 DM - Physiological insulin regimen (insulin injected subcutaneously)
- Assessment of control
- Aim for blood glucose levels 6.5 – 7.5 mmol/L before meals & overnight and < 9 mmol/L two hours after main meals
- Dosage adjustment
- Diet and exercise
- Education about diabetes
|
Management of type II DM - Correct use of medication
- Education
- Exercise
- Weight loss
- Stop smoking
- Foot care
- Lifestyle modification
|
Considerations during exercise for DM pts - Diabetes must be stable.
- Carry medical info about condition in case of adverse effects e.g. medical alert bracelet.
- Insulin uptake may ↑ if injected into exercising limb e.g. rather use abdomen than thigh.
- Autonomic neuropathy leads to abnormal HR & BP responses
- Peripheral neuropathy leads to sensory loss, poor balance, and coordination.
- Peripheral neuropathy requires good foot care. Pts should check feet before and after exercise.
- Effects of exercise on glucose levels last < 72hrs, so exercise should be frequent and regular
- Signs of hypoglycaemia: shakiness, weakness, abnormal sweating, nervousness, anxiety, tingling in the mouth and fingers and hunger.
- Blood glucose monitoring before & for several hours after exercise is prudent when beginning or modifying an exercise programme.
|
Exercise prescription for DM Aerobic and resistance training - Frequency: 3-7 d/wk.
- Moderate intensity:
- Aerobic; 40-60% HRR or 60-75% HRmax or “moderate” level on perceived exertion scale. Better blood glucose control might be achieved with higher intensities.
- Resistance; 60-80% 1-RM
- Time: minimum of 150 min/week. Additional benefits accrued if ↑ act to ≥ 300min/week.
- Type: emphasize activity that includes large muscle groups in rhythmic & continuous contraction.
| Obesity - More calories consumed than used during physical activity
- BMI (body mass index) used to diagnose obesity
- BMI: weight in Kg divided by height in meters squared (kg/m2)
- Abdominal obesity: waist circumference and waist: hip ratio
 |
Abdominal obesity Waist circumference - Standing, arms at sides, feet together & abdomen relaxed
- Horizontal measure taken at narrowest part of torso
- Take two measurements and re-test if measurement is not within 5mm of each other.
Normal values: 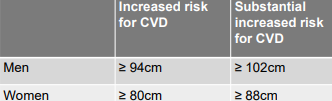 Waist to hip ratio | Management of obesity - Changing eating behaviour (dietician consultations)
- ↓ of energy intake of 500-1000kcal/day.
- Exercise therapy
- ↑ physical activity to minimum of 150min/week of moderate intensity
- Progress to > 250 min/week to promote long-term weight control.
- Include resistance training to assist with losing weight.
- Bariatric surgery
|
Exercise prescription for obesity - Aerobic, resistance and flexibility exercises
- Frequency: ≥ 5 d/wk. to maximize caloric expenditure
- Intensity: Moderate to vigorous intensity exercise. Initial moderate (40-60% HRR). Progress to more vigorous ≥ 60% HRR.
- Time: Minimum of 30min/day and progress to 60min/day.
- Type: Primary mode should be aerobic of large muscle groups. Add resistance and flexibility exercises as HTN.
|
Bariatric surgery - Indications for bariatric surgery:
- BMI ≥ 40 kg/m2
- BMI ≥ 35 kg/m2 with 1 or more severe obesity-related conditions.
- Pre-operative screening: Medical, dietician, physiotherapy, psychologist.
- Post-operative management as per surgical pt.
- Post-discharge exercise prescription for prevention of weight gain.
- Minimum of 150 min/week
- Progress to ≥ 250 min/week moderate-to-vigorous intensity
| Type of bariatric surgeries - Adjustable gastric band
- Sleeve gastrectomy
- Roux and Y gastric bypass
- Biliopancreatic diversion with duodenal switch
(Diagram in notes) |
Metabolic syndrome Diagnosis needs at least 3 of the following: - Fasting glucose > 110 mg/dl
- BP > 135/85 mmHg
- Plasma triglycerides > 150 mg/dl
- HDL < 45 mg/dl (men) & < 50 mg/dl (women)
- Waist circumference > 102 cm (men) and > 88cm (women)
- Management: Weight loss programme (diet consultations and exercise therapy)
| Physiotherapy pt education - Self-monitoring of vital signs assessment and clinical parameters
- Record vital signs & other clinical parameters
- Perceived effort/breathlessness assessment when performing exercise
- Specific exercise programme as it relates to aim of programme
- Red flags to watch out for during exercise
|
When to stop exercise - Struggling to keep pace/rhythm.
- Significant ↑ in SOB influencing ventilation capacity.
- Complaining of chest pain.
- If arterial O2 sats level falls >10% in pts who this is required due to other diseases.
- Signs of poor perfusion e.g. light headedness, confusion, ataxia, pallor, cycyanosis, cold and clammy skin.
- Signs of hypoglycaemia
| HPT DRUG TABLE 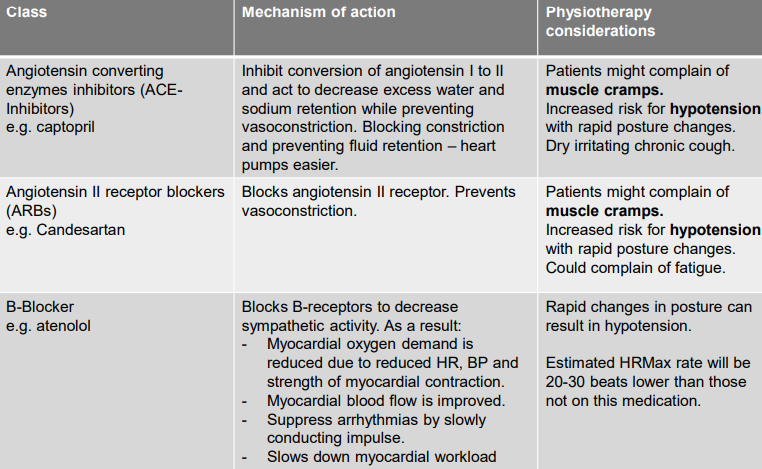 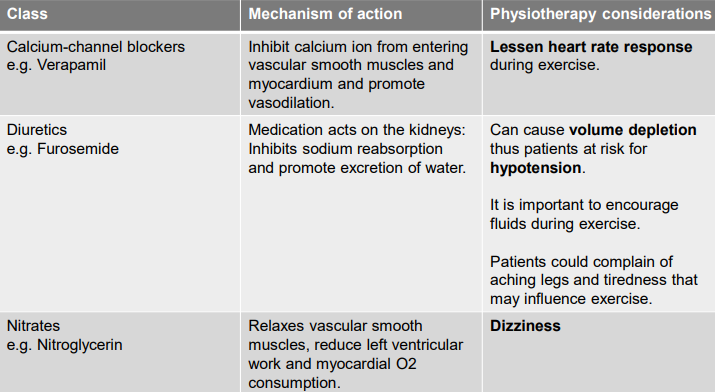 |
Cause of injury - Classification according to site(s) & mechanism of injury.
- Site e.g. skeletal, pulmonary, heart & great vessels or diaphragm injury.
- Mechanism: blunt/penetrating trauma.
- Blunt – forces distributed over large tissue area e.g. MVA.
- Penetrating – forces distributed over small area & penetrating the body e.g. GSW.
| Complications of thoracic trauma Aspects to consider during PT - Hypotension due to blood loss.
- ↑ HR due to blood loss & stress response
- Respiratory distress due to V/Q mismatch caused by specific injuries.
- In severe cases altered cognitive status
| Thoracic injury: chest wall - Superficial soft tissue injuries - E.g. hematomas, abrasions, lacerations
- Deep soft tissue injuries - E.g. Degloving injuries
- Investigate potential for underlying injuries e.g. rib fractures
|
Rib fractures - Occur due to blunt chest trauma & id by assessing CXR or CT-scan
- Ribs usually fracture at point of impact/posteriorly where ribs are weaker.
- Simple rib fracture – single rib
- Multiple rib fractures – >1 rib, & bone fragments can displace
- Most common ribs fractured are rib 7 to 10
- If fractures present in rib 1-3 then consider whether injuries are not present at the cervical spine & brachial plexus.
- If the 10th, 11th, or 12th ribs are fractured, liver/spleen injuries are often present.
- When an individual has multiple rib fractures other conditions are also present e.g. pneumothorax, haemothorax or pulmonary contusions.
|
Flail chest - Multiple adjacent ribs fractured in multiple places separating a free-floating segment & moves independently.
- Paradoxical breathing observed at flail segment
- Pt will have pulmonary contusions in underlying lung segments
- Surgical stabilization of flail rib fractures done when pt continues to suffer + poor oxygenation & significant displaced ribs that could lead to deformity
 | Complications of rib fractures - Pneumonia
- Respiratory failure
- Post-traumatic empyema (pus in intrapleural space)
- Fracture non-union
- Chronic pain with long term disability
|
Thoracic injury: sternal fracture - Common with high velocity injuries
- Blunt Trauma (hit steering wheel or seatbelt injuries)
- Associated with multiple rib fractures/flail segment
- Associated with intra-thoracic injuries e.g. cardiac contusion
|
Medical management of chest wall injury - Pain management
- O2 therapy
- Positive pressure devices with O2 therapy e.g. non-invasive /mechanical ventilation
- Operative stabilization of flail chest if pt continues to suffer from poor oxygenation & significant displaced ribs that could lead to chest wall deformity.
- Open reduction and internal fixation if sternal fractures are overlapping
|
Surgical stabilisation of flail rib segments - Intramedullary stabilization with rib splint and screw fixation with anatomical rib plate
- Screw fixation with U-plate
(Pictures in notes) | Assessment findings: chest wall - Complaint of discomfort & SOB
- Elevated vital signs & altered breathing pattern (shallow breathing)
- Asymmetry with chest wall movements e.g. flail chest
- Abnormal thoracic expansion findings
- Abnormality in auscultation findings if lung parenchyma/intra-pleural space affected.
- Poor cough effort
- ↓ in fx activities
- Abnormalities in trunk, shoulder, and cervical spine ROM
- ↓ exercise tolerance
|
Physiotherapy precautions: chest wall - Adequate analgesia prior to treatment.
- No manual chest wall techniques (vibrations, shaking, percussions) on a flail segment.
- Can use mechanical vibromat on a flail segment if chest clearance techniques are needed.
- Simple rib fractures - can perform gentle percussions but no shaking/ vibrations if techniques necessary. Adequate analgesia is still required, and pt should consent.
- Support of fractures with huffing and coughing
- Support sternum if fractured or sternotomy performed with huffing and coughing.
- If median sternotomy performed to stabilize sternum, follow median sternotomy precautions.
- Liaise with thoracic surgeon with regards to precautions when surgical stabilization of flail chest was performed as it pertains to side-lying positions and manual chest clearance techniques
|
Intra-pleural space abnormalities – pneumothorax - Air infiltrates pleural space
- ↑ intra-thoracic volume due to air occupying the pleural space → lung collapse & compression of underlying lung.
- Causes: Blunt/penetrating trauma
- Types: tension pneumothorax, open pneumothorax.
- On CXR – abnormality found at top of lung (black)
|
Pneumothorax Tension pneumothorax - Occurs following injury to lung which results in air leak with a one-way valve effect.
- Air accumulates in intra-pleural space with progressive build-up of pressure resulting in lung compression and mediastinal shift.
- If not addressed can lead to: ↓ venous return, ↓ CO, diaphragmatic inversion, subcutaneous emphysema.
Open pneumothorax - (sucking chest wound) large open chest wound where air flows through open wound.
- Emergency Rx: dressing sealed on 3 sides
|
Symptoms of pneumothorax: Sings of pneumothorax: - Bruising, laceration, surgical emphysema
- ↓ chest wall mvt on affected side
- Affected hemi thorax appears larger in volume
- Hyper resonance on percussion note & ↓ air entry on affected side with auscultation
- CXR abnormalities
|
Intra-pleural space abnormality: haemothorax - Blood accumulating in pleural space
- Contused visceral or parietal pleura
- Puncture/laceration of lung by rib #
- Penetrating chest wounds
- Injuries to major vessels (aorta, pulmonary artery, veins, internal mammary artery)
- 200 ml of blood present in pleural space before visible on CXR
- On CXR – abnormality found at bottom of lung (white)
| Signs and symptoms of haemothorax - Like pneumothorax
- Thoracic expansion – ↓ on affected side.
- Auscultation: ↓ breath sounds on affected side
- Percussion note = dull or stony dull on affected side
|
Chest x-ray features Pneumothorax - Black border around lung field (lung border pulled away from rib cage)
- No peripheral markings visible
- Partial/Full collapse of underlying lung
Haemothorax - Grey discoloration over lung (supine)
- White density over mid-and lower lung region with meniscus sign (sitting)
|
Medical management of haemo/pneumothoraces - Remove air & fluid from pleural space through intercostal drain insertion into 5th/6th intercostal space
- Management of pain e.g. oral analgesia, pleural block, epidural
- O2 therapy to combat hypoxemia
|
Principles of underwater seal drainage/ICD Underwater seal - Prevents air re-entering pleural space.
- Distal end submerged 2cm
- Hydrostatic resistance of +2cmH2O
Creation of pressure gradient - High gradient to low gradient
- Intra-pleural pressure
Gravity - Fluid drains by gravity
- ICD below insertion site
|
ICD assessment Swing – fluid moving to and from pt in tube - Breathing cycle
- If no swing – drained completely
Bubbling - Indicates air leak from pleural space
- Degree of bubbling: cough, expiration, in/expiration
- No bubbling – drained completely
Drainage - Pattern
- <100 ml/hour – drain to be removed
| Physiotherapy precautions: intra-pleural abnormalities - Cough with ICD support
- Review ICD activity daily with treatment
- Be aware where ICD is during treatment
- Clamp tube when lifting higher than insertion site.
- ICD should always be below insertion site.
- If pt on negative suction review orders as to disconnection with mobilisation away from bedside.
|
General criteria for removal of ICD - < 100ml over 24 hrs
- Minimal swing
- CXR: full expansion
- Breath sounds present over whole thorax
- No air leak
|
PT Mx: chest wall & intra-pleural abnormalities Aims of physiotherapy: - Optimize lung volumes
- Optimize cough effort
- Prevent secondary chest infections
- Ensure optimal pain mx
- Encourage early mobilization
- Prevent ↓ in joint ROM
- Encourage ICD drainage
- Improve exercise tolerance as pt’s acute pathology ↓
- Educate pt regarding condition & physiotherapy precautions.
| Physio treatment - Treatment modalities for ↓ lung volume
- ACBT
- Trunk and thoracic mobs
- Aerobic exercise
- Deep breathing exercises with UL ROM exercises
- Treatment modalities to address poor cough effort
- Teach huffing
- Teach supported coughing
- Treatment modalities for sputum retention
- Postural drainage
- Nebulisation
- PEP bottles and blow bottles
- Mechanical vibromat
|
Empyema - Collection of pus in pleural space
- Caused by pneumonia, TB, lung abscess, chest injuries etc.
- Treatment:
- Antibiotics and ICD
- Decortication if above unsuccessful
Physiotherapy - Id problem? Lung volume? Sputum retention? Work of breathing - Use treatment modalities as appropriate |
Broncho-pleural fistula - Continues air leak > 24 hours following pneumothorax
- Characteristics of pt
- Excessive bubbling characteristic in IC
- Continues irritating cough
- SOB
- Physiotherapy considerations
- Fistula resolved if bubbling in ICD resolves and CXR resolved
|
Pulmonary contusion - Major component of chest trauma
- Lung parenchyma injury/bruising
- Interstitial oedema fluid & blood fills alveolar spaces → consolidation
- Hypoxemia, ↓ lung compliance, ↑ airway resistance, ↓ diffusing capacity
- CXR: areas of consolidation (white)
- Medical Rx: oxygen therapy for respiratory distress
Physiotherapy Treatment: - Id problem: lung volume? Sputum retention? Breathlessness
- ACBT, IPPB to improve oxygenation, humidifying airways, positioning for V/Q matching, MOBILIZATION ASAP
| Injuries to the diaphragm - Result of penetrating trauma
- High velocity trauma- abrupt ↑ in intra-abdominal pressure
- Abdominal contents move into thorax
- 68% of diaphragmatic injuries – left hemi-diaphragm
- 25% of injuries – right hemi- diaphragm
- Displaced abdominal contents visible on CXR
- Mediastinal shift & resp failure
- Surgical repair
Physiotherapy Rx - Treatment following surgical correction as for laparotomy
- Optimize lung volumes
- Clear retained sputum
- Mobilize ASAP
|
Physiotherapy precautions: pulmonary contusions - Review secretions with every treatment
- Haemoptysis C/I for manual chest clearance techniques
- Review how hb & platelet levels change over time for signs of active bleeding
|
Physiotherapy precautions: cardiovascular injuries - Monitor vital signs
- Monitor dizziness/fatigue during treatment
- Monitor effort with activity
- Palpation of pulse rate to id rhythm abnormalities
- When mobilizing a pt stand close by
| Cardiovascular injuries Most common sites: - Myocardial rupture – sternotomy/ thoracotomy for repair
- Myocardial contusion
- Pericardial laceration – pericardiectomy
- Pericardial haemorrhage – pericardial window
Cardiac tamponade - Develops when there is active bleeding into pericardium with continuous accumulation of blood compressing heart chambers & prevents proper filling of chambers
- Severe Hypotension
- Medical Emergency
- Medical mx:
- Surgery to repair vessels
- Mx in ICU post-op
PT as for post-op pt |
What is heart failure - Clinical syndrome where pts complains of specific symptoms.
- During assessment the following signs may be present: elevated jugular venous pressure, pulmonary crackles on auscultation and peripheral oedema.
- Structural and/or functional abnormalities of the heart present that result in elevated intra-cardiac pressures and/or inadequate cardiac output at rest/during activity.
- Structural heart failure may include left-sided, right-sided, or biventricular dysfunction.
- Left-sided HF dysfunction of the left ventricle and right-sided HF dysfunction of the right ventricle.
- Biventricular HF is when both ventricles fail.
- Functional HF is due to systolic or diastolic dysfunction of the left ventricle
- Heart failure presentations: chronic (CHF) or acute (AHF)
- CHF is when indiv has known diagnosis of heart failure/they have gradual onset of symptoms over time
- AHF = symptoms severe enough for indiv to seek medical review that may result in hospital admission.
| Left ventricular dysfunction - Left ventricle cannot empty or fill effectively.
- Capillary hydrostatic pressure ↑ in lungs and pulmonary oedema develops.
- Left ventricle ejection fraction (LVEF) used to determine level of dysfunction of ventricle.
- LVEF measured by echocardiography
- Ejection fraction = measurement expressed as % of how much blood left ventricle pumps out with each contraction.
Systolic dysfunction results in ↓ of LVEF and thus a ↓ in CO - HF with ↓ ejection fraction (HFrEF).
- LVEF is ≤ 40% indicates significant dysfunction
- Mildly ↓ ejection function (HFmrEF).
- LVEF is between 41% to 49%
Diastolic dysfunction results due to ↓ ventricular filling but LVEF preserved. - Heart failure with normal ejection fraction (HFnEF) or also called HF with preserved ejection fraction (HFpEF).
- LVEF ≥ 50%
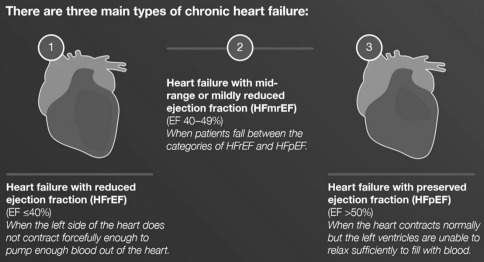 |
Left sided heart failure - Left ventricle cannot empty/fill effectively
- Capillary hydrostatic pressure ↑ in lungs and pulmonary oedema develops.
- Symptoms: orthopnoea, exertional dyspnoea, paroxysmal nocturnal dyspnoea, cough, fatigue, reduced exercise capacity
- Signs: tachypnoea, tachycardia, reduced breath sounds at lung bases, crackles at basal lung segments
| CXR: left ventricular failure - As left atrial pressure ↑ blood shunted to upper zones.
- Interstitial pulmonary oedema follows (perihilar haze and ↑ density over the lower zones)
- Kerley B lines (fluid fills and distends the interlobular septa)
- Kerley B lines (septal lines) visible in costophrenic angles (horizontal lines)
- Enlarged heart develops as failure becomes progressively worse.
- Bilateral pleural effusions may develop over time
Xray examples in notes |
Right ventricular dysfunction - Right ventricle mechanics & fx altered due to ↑ pressure/volume overload.
- Right atrial pressure ↑
- Peripheral capillary hydrostatic pressure ↑
- Oedema in lower extremities & pitting oedema.
- Main cause of RVD is LV dysfunction induced by pulmonary HPT. Other causes could be myocardial infarction, valve disease etc.
|
Biventricular heart failure - Left & right ventricle dysfunction.
- Pts experiencing acute exacerbation of HF typically present in biventricular HF.
- Left-sided HF = in pulmonary vascular congestion, right ventricular overload, and ultimately systemic venous congestion.
- Pts typically present with pulmonary & peripheral signs & symptoms of fluid overload including dyspnoea, cough, jugular venous distention, and peripheral oedema.
| Prevalence of heart failure - Prevalence in Europe – 1 to 2% of adults.
- Prevalence ↑ with age e.g. 1% for individuals < 50yrs and 10% for individuals over 70yrs.
- Slightly higher in females.
- ESC Long-Term Registry, in the outpt setting, reports that 60% have HFrEF, 24% have HFmrEF, and 16% have HFpEF.
- USA - HF ↑ nearly 20% from 5.7 million (2009–2012) to 6.5 million (2011–2014)
|
Aetiology of heart failure in SSA 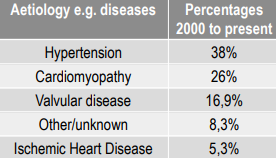 |
Prevalence of hypertensive heart disease - Hypertensive heart disease is cardiac damage due to chronic HPT that may lead to heart failure.
- Prevalence in individuals older than 65 years of age:
- 30-40% in rural West Africa
- 50% in semi-urban West Africa
- 30%-50% in East Africa
- 50%-60% in South Africa
| Symptoms of heart failure - SOB at rest or with physical activity
- Orthopnoea
- Paroxysmal nocturnal dyspnoea (PND)
- Swelling at the ankles, feet, legs, abdomen
- Fatigue
- Rapid or irregular heartbeats
- Cough
- Rapid changes in weight – related to fluid retention
|
Signs of heart failure - Elevated jugular venous pressure
- Peripheral oedema (ankle, sacral, scrotum)
- Tachypnoea & Tachycardia
- Pulmonary crackles
- Pleural Effusions on CXR
|
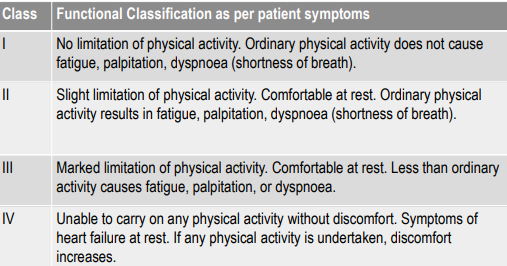
Classification of severity of heart failure - American Heart Association/American College of Cardiology (AHA/ACC) and New York Heart Association (NYHA) have created 2 complementary classification systems
- Structurally, HF staged based on extent of structural damage to myocardium and represents irreversible progression of disease severity (Stage A to D)
- The NYHA functional classification categorizes four classes of HF based on symptoms with physical activity. There can be progression and regression
 | Physical fxn of individ with HF - Physical fx influenced by symptoms.
- Rehab outcome measures often included in studies:
- Six-minute walk test (6MWT)
- Short Physical Performance Battery test (SPPB)
|
Rehab values of 6MWT - Minimal clinical importance difference in pt with heart failure = 32 meters
- Less optimal outcome in chronic HF individuals if 6MWT value are:
- ≤ 300 meters poorer prognosis
- ≤ 200 meters – pts with stable HF with ↑ risk of death
|
Short physical performance battery (SPPB) Balance subscale - Side by side
- Semi-tandem
- tandem
Four-meter walk subscale Sit-to-stand subscale - single chair stand
- five chair stands
 |
Definition of zone colours with clinical manifestation 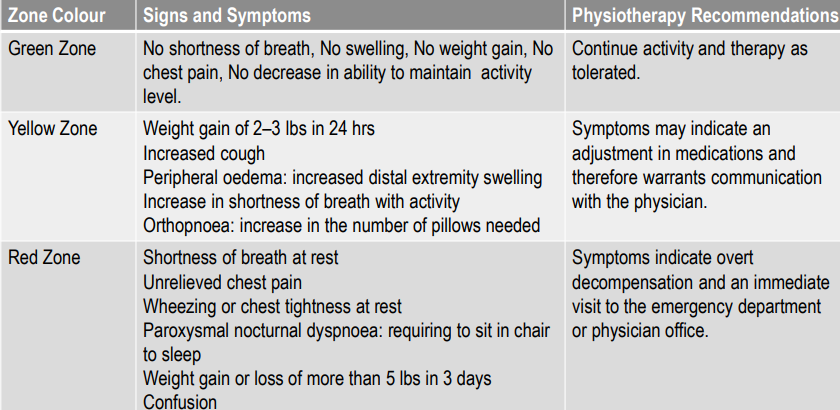 |
Management strategies - Modification of risk factors by behaviour change activities, e.g. smoking cessation, healthy diet, engaging in physical activity & exercise.
- Indiv pt & caregiver education
- Pharmacotherapy
- Implantable devices
- Heart transplantation
| Medical management of HF Surgical application of ventricular assistive devices (VAD) - Biventricular pacemaker
- Implantable cardioverter-defibrillator (ICD)
- Extracorporeal left ventricular assistive device
| Physiotherapy for HF Aim for hospital phase - Assessment of pt to id impairments and develop treatment programme.
- Education on heart failure and behaviour risk factors
- ↓ and teach management strategies to address symptoms e.g. SOB
- Improve fx ability & exercise tolerance by initiating slow graded mobilization and exercise
- Prevent secondary hospital complications
Physiotherapy strategies for SOB - ACBT – breathing component
- Relaxation positions (pacing strategy)
- Pacing strategy – place stairs throughout house to recover and continue walking
- Pacing according to ADLs
Physiotherapy strategies for graded mobilisation - Assess balance, teach on mobility aid, assess stairs and walking with aid, educate caregiver as well
- Implement walking programme
- Teach how to monitor pulse rate and breathlessness
Exercise prescription suggestions - Frequency & timing: Initially short bouts of exercise e.g. 5-10 minutes with rest periods, 2-3 times daily; progression – ↑ time e.g. up to 20 minutes, 1-2 times daily
- Intensity: Perceived effort (MBS <3) or individual tolerance; HR below 120bpm or baseline HR +20-30bpm
|
Precautions during hospital PT management - Monitor vital signs before & after treatment (HR, RR, BP, SpO2)
- Regularly palpate pulse rate during treatment
- Monitor intensity level of breathlessness
- Observe pt closely e.g. colour & signs of cyanosis
- Monitor secretions closely as it may be pulmonary oedema instead of infective secretions
- Pacemaker precautions
| Relative contraindications to continuing exercise – acute phase - Unusual HR response e.g. ↑ of 50 beats with low-level activity
- BP indicative of HTN e.g. abnormal high SBP (>210mmHg) or DBP (>110mmHg)
- Drop in SBP (>10mmHg) with low-level exercise (Not just a drop when standing/changing position)
- Symptoms with activity e.g. angina, excessive dyspnoea, excessive fatigue, mental confusion, severe claudication (8/10 pain)
- Signs of pallor, cold sweat, ataxia
|
Cardiac rehabilitation ‘The coordinated sum of activities required to influence favourably the underlying cause of cardiovascular disease, as well as to provide the best possible physical, mental and social conditions, so that pts may, by their own efforts, preserve or resume optimal functioning in their community and through improved health behaviour, slow or reverse progression of disease’ | Cardiac rehab available to people with - Acute coronary syndrome
- After revascularisation e.g. coronary artery bypass graft surgery
- Stable heart failure
- Stable angina
- After heart valve repair/replacement
- After heart transplant or ventricular assist devices
- Other arteriosclerotic diseases e.g. peripheral artery disease, transient ischaemic attack
|
Key components of cardiac rehab - Health behaviour modification
- Education
- Exercise training
| Core components of cardiac rehab - Health behaviour change and education
- Lifestyle risk factor modification & mx
- Psychosocial health
- Medical risk mx
- Long term strategies to maintain change
- Audit and evaluation of implemented interventions
|
Phases of cardiac rehabilitation: |
Phase 1: In-hospital rehabilitation - Content of rehab dependent on problems id, condition treated & complications developed
- Surgical procedure e.g. CABG vs post-angiography or medical mx of indv with symptom exacerbation in chronic HF pt or post myocardial infarc
- Hospital length of stay: CABG +/- 5-7 days, PCI d/c within 48 hours
- The usual team members – medical doctors e.g. cardiologist, cardio-thoracic surgeon, pulmonologist, nursing staff, physiotherapists, dietician, pharmacist
- Activities frequently included: chest clearance techniques, progressive gradual mob exercises, education on precautions to condition, education on exercises done in hospital and immediate discharge phase, education regarding dietary suggestions & pharmacological matters, monitoring symptoms & educate on how to mx symptoms
Aims of phase 1 cardiac rehab - Pt has clear lung fields & able to clear secretions independently
- Pt able to fx at intended ADLs
- Pt has some knowledge of heart disease
- Pt can cope with their symptoms
- Pt & caregiver is knowing about home exercise programme on discharge.
- Pt and caregiver is knowing about the ‘do and don’t’ activities
| Phase 2: Outpt rehabilitation programme - Formats - Home programme and/or attendance of outpt programme. All formats have supervision incorporated.
- Outpt rehab consist of an intake/ assessment procedure, a treatment phase and re-evaluation.
- Cardiac risk stratification = careful evaluation of clinical & fx status of the pt, starting with clinical hx & physical, laboratory and adjunct tests to classify the subject individually in a risk range e.g. low, medium, high risk for events.
|
Immediate post-discharge phase (Recovery phase) - Period of high anxiety for pts and caregivers
- Pt continues with home exercise programme and advice given on discharge from hospital.
- Contact with pt’s primary care provider/ specialists/ rehab team & referral to 2’ prevention programme as needed.
- Aim: ↑ walking time & distance (walking programme)
|
Phase 3 supervised cardiac rehab programme - Format will determine health practitioners involved.
- Health practitioners that could be involved: Medical doctors, cardiac nurse, exercise specialists, pharmacists, dieticians, counsellors, psychologists, OT
Pt induction to the programme – what should be covered - Aims of exercise programme
- Use of equipment
- Safety aspects, self-monitoring and pacing of exercise
- Setting exercise goals and maintaining a home exercise and activity diary.
|
Pt assessment - Clinical background
- Past medical and surgical hx
- Any physical complaints e.g. NY class of SOB
- Establish aims for treatment
- Physical assessment – Physical activity level, Vital signs, Anthropometric measures, Muscle strength, ROM, balance etc., Exercise tolerance, Quality of life
| Presentation of pts with CVD - Pain
- SOB
- Palpitations
- Fatigue
- Weakness
- Swelling of the lower extremities
- ↓ in physical function
| Risk stratification for cardiac rehab - Different protocols available to evaluate pt’s risk for A/E during exercise
- Low, moderate & high risk
- Pts signs & symptoms used to categorise pts.
E.g.: Low risk (LVEF >50%), Moderate risk (LVEF 40-50%), High risk (LVEF <40%) E.g.: AACVPR stratification algorithm for risk of event |
Contraindications for exercise - Unresolved/unstable angina
- Uncontrolled HPT (SBP > 200mmHg, DBP > 110mmHg)
- Orthostatic drop in BP > 20mmHg with symptoms
- Symptomatic hypotension
- Uncontrolled arrhythmias
- Resting/uncontrolled tachycardia (RHR > 100bpm)
- New/recurrent symptoms of breathlessness, lethargy, palpitations, or dizziness.
- Unstable heart failure e.g. swelling of ankles and/or weight gain > 2 kg over 2 days
- Recent embolism
- Any acute illness with fever
- Severe orthopaedic conditions that would prevent being able to exercise
- Unstable/uncontrolled diabetes
|
Monitoring exercise intensity - HR – Palpation of radial artery
- Any signs of dizziness & fatigue levels
- Perceived effort with Modified Borg scale
- MET – Monitor exercise intensity according to MET table set for common activities
| Exercise prescription – outpt - Frequency: at least 2-3 d/wk other days walk/ leisure activities. Frequency depends on pt’s baseline
- Intensity: 40-80% of HRR, moderate-strong level
- Time: Warm-up & cool-down +/- 5-10 mins. Goal for conditioning = 20-60 mins.
- Type: Aerobic focussed with strength & flexibility
|
High intensity or aerobic interval training - Not indicated for all but could be used in stable cardiac disease pts.
- High-intensity interval training/ aerobic interval training: Warmup, Alternating bouts of moderate and then high intensity aerobic activity, Cool down period
|
Strength training and resistance prescription - Individualized.
- Introduced as out-pt
- Frequency – minimum 2 x per week
- Intensity – upper body (30-40% of 1RM), lower body (50-60% of 1RM)
- Time – 1 set minimal (2-4 sets optimal) of 10-15 reps
- Type – 8-10 different muscle groups (Exercise large muscle groups then small groups)
|
Pt consideration for resistance training - Minimum 6 to 10 weeks after date of MI or cardiac surgery.
- Minimum of 3 weeks following trans-catheter procedure.
- No signs of:
- Acute congestive heart failure.
- Uncontrolled dysrhythmias.
- Unstable symptoms.
| Exercise programme format - Warm-up
- Circuit design with combination of aerobic and strength stations
- Cool down
- Home-based CR
|
Educational components - Pathophysiology & symptoms
- Physical activity, diet, smoking
- Weight management
- Other risk factors e.g. BP, diabetes, lipids
- Psychological & emotional self-mx
- Social factors and ADLs
- Pharmaceutical & surgical interventions
- Sexual dysfunction
- Cardiopulmonary resuscitation
|
Circuit design with minimal equipment  | Transition to long-term community-based exercise - When medically and psychological stable, pts should transition from supervised rehab to integration into community exercise.
- Self-mx of chronic disease
- Demonstrate: Significant improvement in fx capacity (≥5 METs), Psychological adaptation to chronic disease, Demonstrate acceptance of behavioural and lifestyle changes
|
Emergency procedures - Emergency equipment including defibrillator
- Staff members trained in BCLS and defibrillation
- Emergency protocols in place
|
Human immunity Non-specific defences - Barriers (skin, mucous membranes)
- Inflammatory rxn (phagocytes, mast cells, eosinophils, natural killer cells)
- Protective proteins (interferon and other plasma proteins)
Specific defences - T-lymphocytes
- B-lymphocytes
- Specific defence systems in body consist of: Cellular immune system (T-cells) & Humoral system (B-lymphocytes)
- When helper T-cells notice virus/bacterium they start immune system response by alerting other cells of immune system such as B-cells & CD4 cells to migrate via bloodstream to affected tissues & interact with foreign material to assist with destroying them.
- Memory T-cells retain affinity for antigen released by bacteria/virus that have been destroyed and can detect reinfection of body by these foreign agents much quicker the second time around.
| Immune systems (cont) - B lymphocytes produce immunoglobulins (antibodies) (IgA, IgD, IgE, IgG, IgM)
- Each B lymphocyte programmed to make one specific antibody for a specific virus/bacterium.
- Ig’s (antibodies) develop & retain affinity for foreign proteins (bacteria, viruses) & neutralize their actions by coating proteins & speeding their uptake by other cells of the immune system (killer T-cells, phagocytes, etc).
- Human immune system consists of 75% IgG, 15% IgA, 10% IgM, small percentages of IgD & IgE
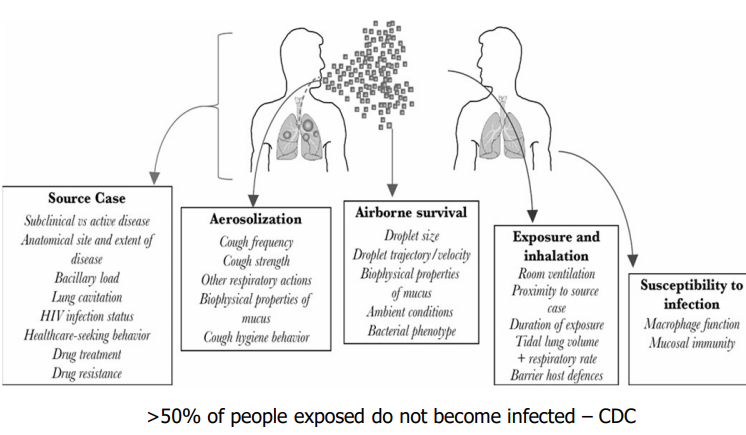
| Tuberculosis - Recent stats indicate 9 mil cases of active TB worldwide per year.
- 1 death every 20 secs from TB
- Tuberculosis is nr 1 killer in SA - >500 000 cases per year.
- High incidence related to HIV pandemic, immigration patterns, immunosuppression through use of other drugs.
- TB is most frequent cause of death in people with HIV
- Caused by Mycobacterium tuberculosis organism
- Airborne organism which can remain viable in the air for up to 48 hrs depending on environmental factors
- Effective contact rate of room is determined by:
- Room ventilation rate (calculated as the number of air exchanges per hour)
- Room volume
- Occupation density
- UVC exposure
- Duration of exposure
- TB affects lungs, lymph nodes, kidneys, liver, GIT, CNS and can also affect any other area
- Possible to have extra pulmonary TB infection without a simultaneous pulmonary TB infection.
- Incubation period very variable – however the development of an acquired cell mediated immune response is about 6–8 wks following initial infection
|
Risk factors for TB - Poverty – poor nutrition, poor sanitation, & low education levels (↑ default rate of HAART and TB Rx)
- Overcrowding (effective contact rate of a room)
- Homelessness
- Smoking ↑ risk of contracting TB by 40%, ↑ risk of relapse post treatment. Smoking ↑ time taken for a TB pt to smear & culture convert. Completion & cure rates are lower in smokers.
- Steroid therapy
- HIV infection (10 x greater risk of developing TB)
- Time spent in mines & prison is directly proportional to risk of contracting TB (effective contact rate of a room)
- Working in hospitals, using public transportation, and working in transportation industry
|
Primary TB - 1st TB infection in person without specific immunity against TB
- Best aerated portions of lungs are infected
- No immediate tissue reaction
- Metastatic bacilli lodge in lung apices, kidneys, brain, growing long bones
- Specific immunity established after 6 weeks
- Primary lesion heals through caseation necrosis
- It is not unusual to contract TB.
|
 |
Lung cavity formation Correlates with: - Organism load
- Treatment outcome
- Risk of acquiring drug resistance
- Infection risk posed to community
Cavity formation associated with primary and post-primary TB |
Complications associated with thoracic TB - Lung abscess
- Bronchopleural fistula
- Pleural effusion
- Post TB bronchiectasis
- Secondary superimposed infection
- Respiratory distress leading to respiratory failure due to destroyed lung
| Post-primary TB - May never occur if initial immune response against TB infection strong
- Is activated by:
- Progression of initial infection
- Re-activation of infection
- Re-infection by TB organism (especially in TB-endemic areas)
| Thoracic TB – signs & symptoms - Persistent cough > 3 wks
- Weight loss
- Lassitude & weakness
- ↑ temperature
- Loss of appetite
- Night sweats
- Chest pain
- Bloodstained sputum (haemoptysis)
- Breathlessness (pleural effusions)
- Anaemia
- Clubbing (fingers and toes)
|
TB diagnosis - Medical hx & clinical manifestations
- Skin test – Purified Protein Derivative (PPD) test or Mantoux test
- Radiological imaging (cannot confirm diagnosis on x-ray alone)
- Sputum test - smear microscopy for acid-fast bacilli
- Culture for sputum to confirm M. tuberculosis to distinguish between first TB infection and drug-resistant TB
New, more definitive lab methods: - Phenotypic methods: Culture and drug sensitivity testing (DST)
- Genotypic methods: GenXpert, LPA/Hines or PCR
- GenXpert and LPA/PCR are used for rapid diagnosis and should always be followed up by culture and DST
- Tuberculin testing mostly done on HIV + pts.
- Injected with TB
- Wheal formation
- Inspection of wheal 48-72 hours after injection –if induration (swelling) is > 4mm, test is positive, and pt put isoniazid therapy for 6 months
- Tuberculin testing not done on pts with suspected drug resistant TB as it is not specific – sputum culture is done
|
Miliary TB - Occurs in 1.5% of all TB cases
- 100% mortality rate if not detected or treated
- 10% mortality if treated timely
- Risk factors
- Cancer
- HIV infections
- Organ transplantation
- Diabetes
- End stage renal disease
- CXR indicates white granules throughout lung fields
|
Management of pts with TB - Antibiotic therapy
- 1st line drugs – Isoniazid, Rifampicin, Ethambutol, Pyrazinamide (PZA)
- 2nd line drugs – fluoroquinoles
- 3rd line drugs - Kanamycin, Amikacin, Capreomycin
- Directly Observed Treatment Short course (DOTS programme) – clinics
|
Drug resistance in TB - Acquired resistance (2’ resistance) - pts with drug sensitive TB can’t/don’t take meds as required
- Transmitted resistance (primary resistance) - infecting organisms already resistant
Contributing factors to DR TB 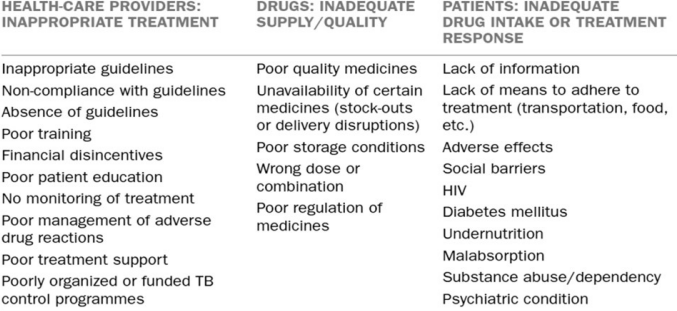 |
|
- Mono-resistance: resistance to any one of 1st line drugs - either Isoniazid or Rifampicin or Ethambutol or PZA
- MDR-TB: resistance to Rifampicin and Isoniazid, with/without resistance to other first line anti-TB drugs.
- Pre XDR-TB: resistance to Rifampicin, Isoniazid along with resistance to fluoroquinoles. 5
- XDR-TB: resistance to Rifampicin, Isoniazid, fluoroquinolones, and resistance to any one injectable anti-TB drugs: Kanamycin, Amikacin, and Capreomycin.
- XXDR TB: recently identified; resistant to all TB medication – no cure. This is less common as there are new drugs used to treat DR TB (bedaquiline, delaminid, etc) however this may not last long as there are already cases reported to be resistant to these new drugs due to defaulting.
|
Physiotherapy and TB Chest clearance - Sputum sampling (often induction)
- ACBT & Mx of breathlessness
- Manual chest therapy & PD
- Adjunctive techniques
Rehabilitation - Strength training
- Aerobic exercise to improve endurance
Education - Management of secretions in community
- Home exercise prescription
- Medication adherence
|
Physiotherapy management – drug resistant TB - Many TB pts are HIV +, making them more susceptible to complications
- Preventative measures (infection control)
- Due to the immunocompromised state of many pts and side effects of TB drugs, neurological complications are common. E.g. stroke, peripheral neuropathy, tuberculomas, HIV related brain atrophy, etc.
- Education important. Many side effects of TB drugs are severe and cause the pts to default. Sometimes they do not have consistent access to food and thus stop taking the medication.
- Always ensure your treatment sessions include education (cessation of smoking and drug use) and social issues are addressed.
- Drug resistant TB can precipitate COPD thus relevant management for that should be done.
- Remember to treat pt holistically, ensure that pt can return to work and that pt’s return to community is not compromised
|
Safety in the management of pts with TB - Often a delay in diagnosis of active TB in HIV-infected pts due to atypical CXR features & negative sputum smears
- Adherence to infection control guidelines NB so PTs minimize own risk of contracting TB.
- N-95 masks worn (handle it correctly, test the seal)
- Surgical masks worn by pts with TB to ↓ number of infectious particles left in room
- Keep windows open to ensure adequate ventilation
|
HIV – opportunistic infections Brain - Cryptococcal meningitis
- Toxo (toxoplasmosis)
- AIDS dementia complex
Eyes Mouth and throat - Cold sores and ulcers
- Thrush (oral candidiasis)
Blood - Hyperglycaemia
- Dyslipidaemia
Lungs - Histoplasmosis
- PCP (pneumocystis jiroveci pneumonia)
- TB
Bone Heart Liver Stomach - CMV (cytomegalovirus)
- Crypto (cryptosporidiosis)
- MAC (mycobacterium avium complex)
Reproductive system - Genital ulcers
- HPV (human papillomavirus)
- Cervical cancer
- Menstrual problems
- PID (pelvic inflammatory disease)
- Vaginal yeast infections (candidiasis)
Body | Pneumocystis Jiroveci pneumonia (PJP) - Id manifestation of clinical syndrome of HIV (AIDS)
- Pts with low CD4 counts & ↑ viral load placed on prophylactic antibiotic therapy to prevent onset of PJP (HIV, cancer, RA meds that ↓ CD4 count)
- Mortality rate associated with development of PJP is high – hence prophylactic therapy
|
PJP diagnosis - Symptoms: fever, cough, fatigue, & severe SOB
- Slow onset.
- Cough dry with little/no sputum.
- May/may not have added sounds on auscultation.
- CXR: PJP not always visible.
- Sputum induction – diagnosis made 70% of the time.
- Bronchoscopy: very accurate for Dx.
|
PJP treatment Medical - Hydration through fluid intake or IV.
- O2 therapy
- Drug Rx dependent on organism cultured.
- Antifungals = amphotericin B, fluconazole
- Antibiotics = penicillin, amoxicillin, Bactrim, Septra
- Short-course corticosteroids with antibiotics
- Those pts on HAART tend to have CD4 counts > 200 cells/mm3 and go through stepwise withdrawal from antibiotic therapy prophylaxis.
- Pneumocystis bacteria that are present in HIV pts led to development of COPD in pts with HIV due to chronic low-grade inflammation of airways
- In pts with persistent pneumocystis infections (recurrent infections throughout year) are at risk for developing COPD
|
Physiotherapy and PJP Hypoxemia - Positions of breathlessness (relaxation positions)
- Neb with saline (0.9% NaCl) to humidify airways
- ACBT emphasizing BC and TEE
- Position for V/Q matching
Reduced exercise tolerance - Graduated exercise programme and mobilisation
- Wide spectrum of complications e.g. neurological, paediatric, cardiopulmonary
- Advise pt regarding healthy diet & vitamin & mineral supplements and refer to dietician
|
TB in people with HIV - How Soon after Infection with HIV Does the Risk of Tuberculosis Start to Increase?
- Persons infected with MTb only – 10% lifetime risk of TB disease
- Persons infected with MTb and HIV – 10% annual risk of TB disease
- Extrapulmonary and disseminated TB is greater in HIV-infected pts with advanced immunosuppression
- Extra-thoracic lymph node infection develops in 18 to 22%
- Most common sites are cervical (84%) and axillary (18%) nodes.
|
Overtraining signs - ↓ ability to exercise
- Mood changes & irritability
- General fatigue & depression
- Sore muscles & overuse injuries
- Insomnia
- Weight loss
| Exercise guidelines Asymptomatic person with HIV (CD4 > 500 x 106 /L): - 2 – 3x/week for 20 – 30 mins at easy level (combination of resistance & endurance training)
- Progression: 30 – 60 mins/session, 4 – 5 x/week at moderate level (occ high level)
Symptomatic person with HIV (CD4 = 200 – 500 x 106 /L): - 3 x/w for 15 – 20 mins at easy level (combination of resistance and endurance training)
- Progress: 3 – 4x/w, up to 40 mins, moderate level
Person living with Aids (CD4 < 200 x 106 /L): - 2 – 3x/w, 15 – 20 mins at easy level (combination of resistance and endurance training)
- Progress: 20 – 30 mins (with caution), 3 x/week, at easy level
|
Exercise therapy for HIV - Resistance training important to enhance muscle mass & boost immune system
- Cardiovascular exercises:
- ↑health by controlling BP, blood sugar levels, blood lipids and stress levels
- Avoid overtraining -> loss of lean body mass & suppresses immune system
|
Immune reconstitution inflammatory syndrome (IRIS) - Tuberculosis-immune reconstitution inflammatory syndrome (TB-IRIS) = abnormal, excessive immune response against alive or dead M. tuberculosis that may occur in either HIV-infected or, more rarely, uninfected pts.
- This can also happen with pt starting HAART for the 1st time or if pt has defaulted & was re-challenged with HAART
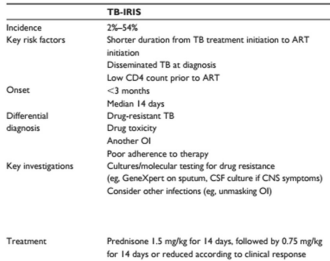 |
Implications for physiotherapy when treating pts with HIV - Adherence to infection control principles to ↓ the development of surgical site infections
- Pt rehab may be affected by sensory deficits associated with peripheral neuropathy in relation to re-education of gait and balance.
- Fatigue associated with ART may impact on the pt’s level of endurance – ↑ duration of rehab
- Up to 50% of people living with HIV/AIDS suffer from mental illnesses which may impact their adherence to therapy.
|
Mucus - Tracheobronchial mucus produced by goblet cells & seromucous glands.
- No of cells that produce mucus ↓ from trachea to peripheral bronchi.
- Alveoli & bronchioles produce surfactant.
| Mucus pathology - Acute illness (e.g. pneumonia) causes oedema & abnormal production of mucus due to inflammation & irritation of airways.
- Changes in sputum may reflect improvement/deterioration in pt’s condition & response to treatment.
- Symptoms resolve as disease responds to treatment
- Chronic illness (e.g. COPD, bronchiectasis, CF) causes degeneration of ciliated cells which convert into mucus-producing goblet cells and lead to:
- Changes in rheological properties of mucus
- Mucus hypersecretion
- Mucus no longer assists with defence of upper airways and risk of infection ↑
- In chronic disease mucus viscosity ↑ as water is lost from mucus and number of macromolecules in mucus increases.
- Mucus stasis in airways lead to obstruction and atelectasis.
- An early sign of exacerbation of chronic disease is changes in nature & vol of sputum expectorated
| Sputum colour Clear = no infection White = minimal infection Yellow/green = infection Red = haemoptysis (fresh blood) Brown/rusty-brown = previous haemoptysis or lung tissue damage (old blood) or pneumococcus pneumonia infection Sputum colour chart  |
Terminology related to sputum Mucoid (M) = clear secretions Purulent (P) = coloured secretions Mucopurulent (MP) = mixture of M & P Bloodstained (B) = flecks of blood or plugs |
Sputum specimen - Specimen produced when a pt coughs up & expectorates pulmonary secretions
- Risk that specimen may contain mainly saliva
- Risk that specimen may be contaminated by oral organisms
- Doctors request these to diagnose bacterial infections & to help guide future treatment
- Therefore, adequate & representative sputum samples are of great importance
- Sputum specimen stained in the lab with Gram’s stain
- Antibiotic sensitivities performed on + cultures
|
Diagnosis of pulmonary infection – criteria needed - Purulent secretions
- White blood cells on Gram’s stain of sputum
- Cultured organisms
- Fever
- Raised white blood cell count from blood screen
- CXR infiltrates in the lung fields
- PaO2 reduction
|
Community-acquired pneumonia Signs and symptoms - Fever
- Pleuritis
- ↓ exercise tolerance
Organisms that account for most cases - Streptococcus pneumoniae
- Mycoplasma pneumoniae
- Influenza virus
|
Collection of sputum - 30 minutes after a meal
- Pt to rinse mouth with water prior to procedure
- Chest physiotherapy treatment
- Cough & expectorate sputum into sputum specimen jar
- Label specimen jar with pt name, hospital nr, ward, time that sample was taken, antibiotic Rx pt is currently receiving
|
Sputum induction - Performed in immunocompromised pts suspected to have PJP/TB
- Characteristic sign: dry cough
- Sputum induction helps to induce sputum
- Occasionally used for diagnosis of infection in pts with asthma, COPD, or cystic fibrosis.
|
Procedure for sputum induction - Hypertonic saline (3% – 5% NaCl) needs to be ordered from hospital pharmacy – on prescription
- Ultrasonic nebulizer/efficient jet nebulizer
- Pt ‘nil by mouth’ overnight
- Thorough brushing of teeth, tongue, and gums
- Rinse mouth with water or normal saline
|
Preparation for induction 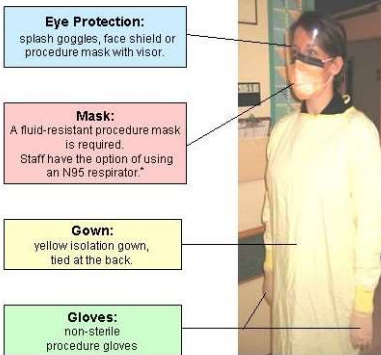 |
Induction procedure – 2 - Wear mask, apron, gloves during procedure -> most pts TB +
- Pt to inhale hypertonic saline for 20 min in isolated area
- During inhalation do ACBT with FET, cough & expectoration – can proceed with PD and manual chest therapy techniques if struggling to obtain sputum sample with ACBT alone.
- Expectorate sputum into sterile sputum specimen jar
|
Possible side-effects of induction - Rapid development of large pleural effusion if small effusion already present on CXR prior to sputum induction procedure
- Breathlessness
- Nausea
- Bronchoconstriction
|
Summary of sputum induction - Stay with pt during procedure to ensure proper sample obtained
- Universal precautions (protective equipment for infection control) mandatory
- Monitor pt during & after procedure for side effects
| |
Definitions - Cancer = disease characterized by cells which abnormally re-acquire the capacities of unrestrained reproduction and mobility
- Tumour = abnormal mass of tissue with a growth that exceeds that of normal tissue
- Primary tumour = original site of tumour development
- Secondary tumour = metastases developed away from primary tumour but are of same origin as primary tumour
| Causes of cancer Intrinsic factor Extrinsic factor - Chemical
- Physical
- Environmental
| Seven warning signs of cancer - C – change in bowel or bladder habits
- A – a sore that does not heal
- U – unusual bleeding or discharge
- T – thickening or lump in the breast, testicles or elsewhere
- I – indigestion or difficulty swallowing
- O – obvious change in the size, colour, shape or thickness of a wart, mole, or mouth sore
- N – nagging cough or hoarseness of the voice
|
Characteristics of tumour cells Benign - Encapsulated
- Slight vascularity
- Cells like parent tissue
- Well differentiated
- Slower growing
- Local spread
Malignant - Rarely encapsulated invasive
- ↑ vascularity
- Cells unlike parent tissue
- Variable aplastic
- Fast growing
|
Malignant tumours - Cells detach from growing tumour mass
- Cells infiltrate adjacent tissues & body cavities
- Cells invade preformed channels (blood vessels, lymphatics, nerves)
- Cells are disseminated throughout the body
- Sites most spread to are brain, liver, bone
| Lung cancer - Most common cause = smoking (87%)
- 1 in 10 life-smokers will develop lung cancer
- Individ susceptibility to lung cancer exists
- Entire bronchial tree at risk of cancer due to smoke exposure
- Lung Ca causes molecular damage – develops years after smoking stopped.
|
Types of lung cancer Non-small cell lung cancer - Accounts for 85% of lung cancers
- Adenocarcinoma most common form in males & females
- Squamous cell Ca forms in lining of bronchial tubes
- Large cell Ca (10%-20% bronchus Ca) – extensive bleeding & tissue damage
Small cell lung cancer - Accounts for 15% lung cancers
- Vicious type of cancer that progresses rapidly
|
Staging of cancer - Used internationally for all non-small cell lung cancers.
- Location and size of tumour (T)
- Amount of spread to lymph nodes (N)
- Presence or absence of metastases (M)
- Each category further scored 0 to 4
- Stage I lung cancer (T1N0M 0)
- Stage IV lung cancer (T4N4M4)
| Symptoms of lung cancer - Diffuse/aching chest, shoulder, or back pain unrelated to episode of coughing
- Change in vol/colour of sputum
- Haemoptysis
- Persistent coughing
- Harsh sounds with each breath (stridor)
- Recurrent lung problems e.g. unresolved pneumonia
- Breathlessness
- Hoarseness of voice
|
Symptoms elsewhere in body due to lung cancer - Loss of energy
- Unexplained weight loss
- Loss of appetite
- Muscle wasting and general weakness
- Headaches, bone, and joint pain
- Bone fractures not related to accidental injury
- Neurological symptoms (unsteady gait, memory loss)
- Neck or facial swelling
- Blood clots
- Nausea
| Diagnosing lung cancer - Needle biopsy
- Bronchoscopy
| Chemotherapy side effects - Hair loss
- Mouth ulcers
- Nausea
- Diarrhoea
|
Symptom control - Pain & nausea managed with radiation therapy, NSAIDS, corticosteroids, analgesia, anti-emetics, and TENS
- Intensity of rehab programme should be adjusted regularly to accommodate the pt’s systemic symptoms.
|
Side-effects of chemo- and radiation therapy - Some of these drugs may cause pulmonary toxicity & lead to development of fibrous scar tissue within lung parenchyma – pulmonary fibrosis may develop.
- Amount of damage related to dose and type of drug received
- Effects on heart include cardiomyopathy, fibrous scar tissue formation in the myocardium, and cardiac arrhythmias and in long term may cause resting tachycardia resulting in lower exercise endurance.
- The dose and type of drugs received influences the severity of complications that develop
- Death rattle in advanced disease
- Develops in late stage of disease due to cardiac failure & development of pulmonary oedema
- Managed with hyoscine to absorb pulmonary oedema fluid
|
Other cancers that affect the lungs - Kaposi’s sarcoma
- Mesothelioma
- Bronchoalveolar carcinoma
- Pancoast’s syndrome
|
Rehab of cancer pt - Physical
- Psychological
- Financial
- Emotional
- Need to understand
|
Physiotherapy assessment - Be aware of body image, the disease, treatment, pain, and pts expectations
- Be realistic and give confidence
| Physiotherapy and the cancer pt - Involved in every stage of disease
- Communication with & self-empowerment of pt very important
- Various skills required as the pt’s condition changes: respiratory, neurological, orthopaedic, rehabilitative, outpts, lymphedema
|
Physiotherapy management of pts with lung cancer - Empower pt with strategies to relieve breathlessness.
- Assist pt with secretion clearance & restore lung volumes postop
- Improve ability to perform fx activities on the ward.
- Improve exercise endurance by introducing progressive walking programme [Lin et al 2014, Cancer Nurs].
- Introduce high intensity endurance & strength training programme 5-7 weeks postop to improve O2 uptake, functional ability, and quality of life (QOL)
|
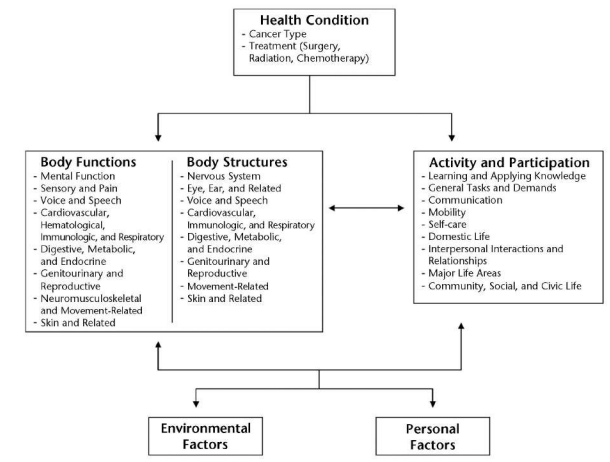 |
Breast cancer - South African women have 1/29 lifetime risk for developing breast cancer.
- Evidence suggests that breast cancer is becoming more common in SA.
- A small but important minority of breast cancer cases develop because of mutations of the BRCA1 and BRCA2 genes – referred to as hereditary breast and ovarian cancer.
- Genetic testing can be performed to determine the type of breast cancer.
|
FITT recommendations for pts with cancer - Programme should include aerobic (endurance), flexibility and resistance (strength) training.
- Frequency:
- aim is to progress aerobic training to 3-5 days/week
- progress resistance training to 2-3 days/week
- flexibility should be done regularly (even while receiving treatment in hosp)
- Intensity:
- slowly progress aerobic training to ultimately reach moderate (50%-60% pred HR) to vigorous (60%-85%) intensity
- Slowly progress resistance training to reach moderate intensity (60%-70% of 1RM)
- Time
- Several short bouts of exercises during the day is more useful that one long session esp if pt is undergoing active treatment.
- Slowly progress aerobic training to 150 mins/week (moderate intensity) or 75 mins/week (vigorous intensity).
- Slowly progress resistance training to reach at least 1 set of 12 reps
- Progression: monitor the pt closely for adverse signs to exercise and adjust FITT accordingly.
READ Exercise Training in Cancer Populations pages 722- 733 in Main and Denehy textbook (2016) - Cancer cachexia
- Risk factors to screen for during assessment
- Outcome measurement tools
- General contraindications and precautions during exercise
|
Diagnosis - Mammogram
- Needle biopsy
- Whole body CT scan
|
Management of breast cancer - Radioactive marker is placed within the tumour
- Chemotherapy initiated 1st especially if metastases noted in axillary nodes
- Following chemotherapy, whole body scan repeated to see how tumour responded
- Surgery will be performed
- Lumpectomy to conserve breast tissue
- Partial/complete mastectomy if indicated
- Radiation therapy commences after wound healing
|
Acute postop complications following breast cancer surgery 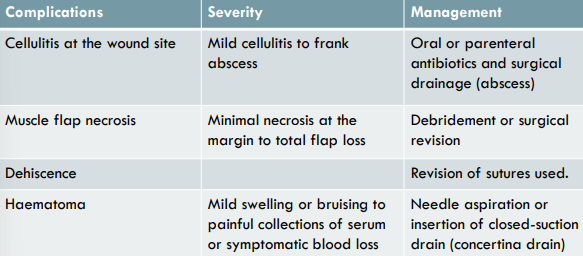 |
Pre-operative pt assessment – breast cancer - Pre-operative pt assessment important to establish the pt’s baseline UL to individualise postoperative rehabilitation strategies.
- Pre-operative physiotherapy assessment should include:
- Shoulder ROM
- Upper limb strength
- Arm function – pt reported outcome measure such as Disabilities of the Arm, Shoulder and Hand scale or Upper Extremity Functional Index.
- Comprehensive PT mx care plan for UL dysfunction which includes pre- and postoperative assessments of shoulder ROM with a progressive exercise programme, lymphedema awareness and individualised treatment, is highly effective
|
UL complications following breast cancer surgery - Dysfx of UL commonly occurs after surgery & radiation therapy for breast cancer.
- UL dysfunction involves:
- Restricted UL mob
- Pain from soft tissue and neural injury
- Lymphedema
- Impaired sensation (numbness, pins & needles, burning) and impaired strength
- UL dysfunction causes disability and negatively impacts quality of life (QOL)
- Axillary web syndrome (AWS) may contribute to upper limb dysfunction postoperatively.
- AWS is a sequelae of axillary lymph node dissection.
- Presents as series of cordlike structures that are visible and palpable beneath the axillary skin.
- These cordlike structures may extend past the elbow to the forearm and even to the wrist and thumb.
- AWS may be due to disruption of lymphatic vessels or veins during axillary surgery.
- Incidence of AWS is 44%-72% after axillary lymph node resection.
| Principles of physiotherapy management – breast cancer - Improve circulation postoperatively to assist with reduction in oedema.
- Optimal positioning of the shoulder on operated side to minimize pain and discomfort.
- Regain and maintain pre-op sh ROM.
- Regain pre-op UL strength.
- Restore functionality of the upper limb to pre-operative levels
|
Post-op rehab - Exercise precautions should be taken in the early postoperative period esp after breast reconstruction surgery.
- Prolonged immobility may lead to UL dysfunction.
- Initial declines in ROM and strength usually improve but recovery is often incomplete.
- UL exercise should commence on day 1 postoperatively in consultation with the surgeon.
| Initial postop treatment - Arm positioned in abduction with elbow supported on pillow.
- Muscle pump exercises of elbow and hand to improve circulation.
- When drain site pain is present, only exercise elbow and hand for muscle pump action.
- During first 2 postop weeks, glenohumeral exercises to 90° are encouraged
|
Progression of postop physiotherapy management - After 2 weeks, start with sustained stretches to point of discomfort (not pain) with glenohumeral forward flexion.
- Avoid vigorous exercises to minimize interference with regenerating lymphatic channels.
- After 21 days pt may gradually stretch shoulder through full ROM.
- Scar massage can commence when all scabs have disappeared, and the incision is well-healed (prepare skin for reconstruction surgery).
- Exercises must be continued for 6 – 12 months postoperatively
|
Physiotherapy management after hospital discharge - Before discharge, PT should arrange an outpt appointment for the pt to return for assessment 6 weeks postop
- Individual progression of UL exercises done according to assessment findings and an appropriate home exercise programme given.
- Surveillance for the onset of chronic lymphedema done at each visit to treat condition effectively when it arises.
- Assessment of QOL should be added to the outcome measures that are assessed at each visit.
- Pt follow-up in outpts dept until 12 months postop
|
Lymphoedema - Signs of overt lymphedema:
- Swelling
- Redness
- Heat
- Tight skin
- Pt describes heavy sensation limb
- Physiotherapy management includes:
- Manual lymph drainage through massage techniques
- Wearing of compression bandages on the affected limb
- K-taping: conflicting reports in research literature re its effectiveness.
|
Guidelines to reduce the risk of development of lymphoedema Together with adherence to exercise prescription, the pt must also: - Lift the arm in case of heaviness
- Avoid lifting heavy objects with that arm
- Use the arm as normally as possible
- Avoid limb constriction
- Avoid extremes of temperature
- Apply skin care
- Wear compression sleeve when flying
- Avoid an increase in weight
|
Physiotherapy in hospice care Role of PT in pts with < 6months to live - Symptom control
- Maximizing remaining functional abilities
- Providing care giver education
- Contributing to inter-disciplinary team communication
Thus - Maintaining pt’s self-identity
- ‘Actively’ awaiting death
|
Cervical cancer and human papillomavirus infection - 270 000 deaths annually due to cervical cancer
- 2nd largest cause of death in women in SA
- Causal link between human papillomavirus (HPV) infection & development of cervical cancer
- Sexual transmission predominant mode of HPV acquisition.
- Oncogenic HPV detected in > 99% of cervical cancer cases
- Prophylactic HPV vaccines significantly ↓ morbidity & mortality
- Oncogenic HPV types 6, 11, 16 & 18 account for most cervical cancer cases
- HPV associated with cancers of the anus, vulva, vagina, penis, oropharynx, mouth.
- HPV infection acquired within 5 years of sexual debut – most infections are asymptomatic & clear within 2 years
- Only fraction of women (1%) who are chronically infected with high-risk HPV types (6, 11, 16, or 18) will develop cervical cancer.
- HPV evades the immune system as it occurs locally at cervix & no presence of HPV in blood stream.
- HPV doesn’t cause cell death, immune system not alerted
- Vaccines for HPV types 6, 11, 16 and 18 (bivalent and quadrivalent) are prophylactic and have no effect if the person is already infected with HPV.
- Bivalent vaccine (Cervarix®) administered to females 15 – 26 yrs of age has 98 – 100% efficacy in preventing HPV infection.
- Quadrivalent vaccine (Gardasil®) administered in same age group has 96 – 100% efficacy.
- Those taking bivalent vaccine report more side-effects (pain, oedema, erythema)
- HPV more frequent in men than women but women develop cervical cancer and are therefore targeted re vaccination.
- Vaccine cost: Cervarix® (bivalent vaccine) = R 700 (excluding VAT); Gardasil® (quadrivalent vaccine) = R 770 (excluding VAT) currently in private sector.
- Vaccines need to be administered three times so cost in total is approximately R2 300 (excluding VAT) – medical aid savings.
|
- Prevalence ↑ over years
- SA has highest age-adjusted asthma death rate per million population in Africa
- 1.5% of 3.9 million SA with asthma die annually
- Many asthma deaths considered to be preventable
- Pts misjudge severity of & mortality risk associated
| Definition of asthma - Develops due to exposure to allergens/genetic predisposition
- Hyperreactivity of airways to stimuli that are normally harmless
- Chronic inflammatory condition of airways
- Reversible condition
- Signs & symptoms of asthma attack:
- Wheezing (high pitched, polyphonic) due to bronchospasm
- Breathlessness
- Cough productive of white/non-infected stringy secretions
| Precipitating factors of asthma attacks - Poverty
- Tobacco smoke
- Emotional stress/anxiety
- Allergens (food, house-dust mite)
- Animal hair
- Junk food
- Air pollution
- Pollen
- Weather
- Drugs (NSAIDS, aspirin, betablockers)
- Gastro-oesophageal reflux
|
Characteristic of classic asthma - Two main features occur together:
- Allergic inflammation with airway wall thickening and mucus production
- Airway smooth muscle dysfunction with bronchial hypersensitivity
- Bronchial hypersensitivity develops due to damage to epithelial cells from chronic inflammation.
- Bronchial hypersensitivity or airway inflammation alone are not sufficient to cause an asthma attack
|
Types and diagnosis - Extrinsic asthma = allergic asthma, occurs early in life, out grown
- Intrinsic (exercise-induced, emotion-induced or chemical-induced) asthma = present in adulthood, less responsive to Rx
- Diagnosis made on history of recurrent attacks & PF varies > 20% diurnally (per day), after exercise or broncholidator Rx
|
Aims of asthma management - Prevention of long-term symptoms that interfere with daily living (e.g. cough or SOB during night or after exercise)
- Maintain lung function near the person’s personal best measurements
- Allow person to participate in all ADLs – school, work, leisure etc.
- ↓ nighttime symptoms to achieve uninterrupted sleep
- Prevent repeated asthma attacks
- Best medicine treatment with fewest side effects
|
Medical management of asthma - Mild intermittent asthma
- Short acting inhaled ß2 -agonist only
- Generally inhaled corticosteroid (used 2 x daily ie Alvesco/Pulmicort) together with short-acting inhaled ß2 -agonist.
- Persistent asthma: as above but long-acting inhaled ß2 -agonist added (Symbicort or Seretide).
|
Hospitalization - Any history of prior intubation / mechanical ventilation
- Hx of poorly controlled asthma
- Inadequate response to therapy in 2 hrs of admission to Casualty dept
- PEFR < 75%
- Recurrence of recent exacerbation
- Social / personal factors
| 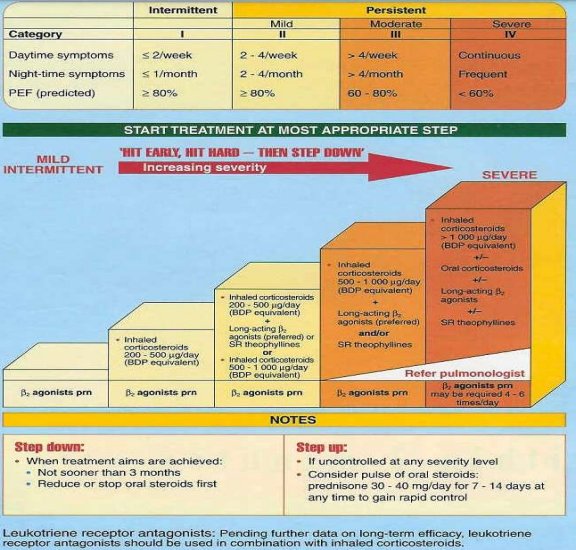 |
Signs of severe acute asthma exacerbation - Severe SOB sitting down
- Difficulty speaking
- Cold and clammy
- Central cyanosis
- ABG reflects low PaO2 with/without hypercapnia
- Silent chest on auscultation
- Pulsus Paradoxus (systolic BP drops) > 10mmHg
- SaO2 < 91%
- PEFR ≤ 33%
- Chest pain
- Slow RR
- Exhaustion and altered level of consciousness (lifethreatening)
|
Asthma drug therapy  |
What wheezes but is not asthma - Airway obstruction due to aspiration of foreign object or stomach acid
- Pulmonary oedema due to cardiac dysfunction
- Pneumonia
- Lung cancer
|
Principles of physiotherapy management of pt with asthma - Improve control of breathing by teaching pt breathing control (diaphragmatic breathing) in a position of relaxation
- Encourage removal of excessive retained secretions through indirect methods e.g. nebulisation, ACBT, mobilisation, encouragement to cough actively and expectorate secretions.
- Improve lung compliance & vols (post-acute phase) with ACBT (TEE).
- Maintain peripheral muscle strength with resistance training.
- Improve/maintain functionality and exercise endurance.
- EDUCATION of pt
- Use of non-invasive positive pressure ventilation (NIV) in casualty to reduce hospital admission rates.
| COPD OR ASTHMA? 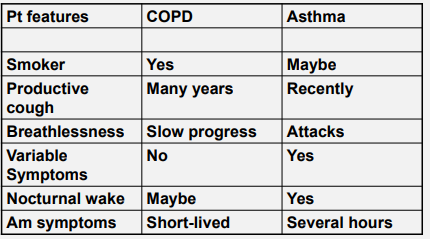 |
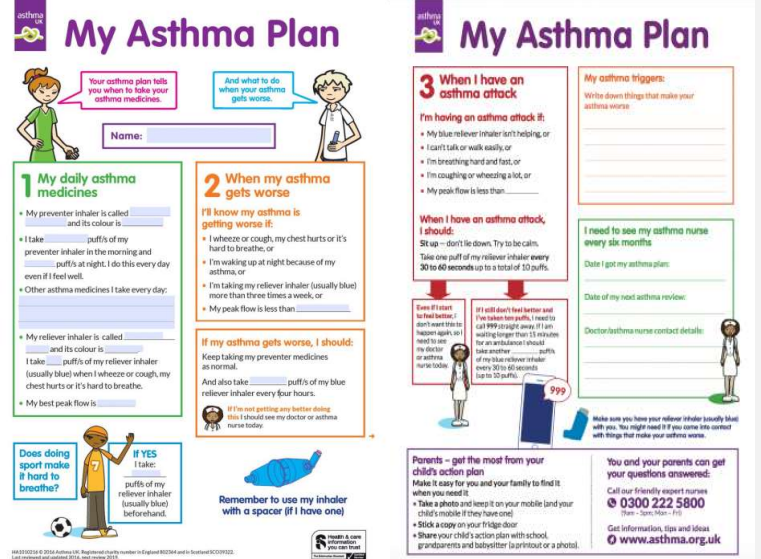 | Education – asthma action plan - Nature of asthma & how to avoid triggers
- How to recognize signs and symptoms
- Different types of Rx
- Side effects of Rx
- How to use inhaler
- How to use peak flow meter
- A written plan of action
|
What is pulmonary rehab? - Programme that helps improve well-being of people with chronic respiratory diseases (asthma, COPD, CF, bronchiectasis).
- It involves a long-term commitment from pt and team of healthcare professionals.
| Aims of pulmonary rehab - Maximize independent functioning in ADL
- Minimize dependence on others
- Reduce dyspnoea & improve muscle strength
- Improve exercise tolerance
- Efficient energy expenditure
- Education on disease process, medication & therapeutic techniques
| Benefits - Improved quality of life
- Reduced anxiety and depression
- Improved exercise tolerance
- Reduction in breathlessness & other symptoms
- Enhanced independence with ADL
|
Format of pulmonary rehab programmes - Based at PT dept of hospital and pt attends as an outpt.
- Based at home with regular visits from the physiotherapist.
- Combination of both.
| Resources required Desirable resources - Access/transport
- Floor space
- Equipment
- Refreshments
Optional equipment - Wall bars
- Bed/plinth
- Mini trampoline
- Bicycle
- Stairs
- Mats
- Treadmill
- Music player
Emergency equipment - Bronchodilator drugs
- Nebulizer & air comp
- SaO2 monitor
- Portable O2 cylinder
- Resuscitation equipment
- Emergency policy
Documentation - Travel/location details
- Programme details
- Assessment forms
- Exercise sheets
- Progress report forms
- Pt information material
|
Criteria for entry - Motivated to help self
- Motivated to change lifestyle
- Adequate functioning in group
- Suitable personality
- Shortness of Breath
- Reduction in ADL
- Stable & optimum medication
- Attendance for whole programme duration
|
Exclusion from pulmonary rehab - Pts with progressive disease i.e. cancer/neuromuscular disease
- Conditions where exercise is contra-indicated i.e. certain cardiac disorders
|
Pulmonary rehab team - Physician
- Physiotherapist
- Occupational therapist
- Nurse
- Dietitian
| Structure of programme - Aerobic and strengthening exercises of large muscle groups & thoracic mobility exercises
- Individual exercise prescription re frequency, duration, and intensity
- Respiratory muscle training
- Education on disease and management
- Education on diet and exercise
|
Exercise prescription guidelines - Length of programme: 14 – 24 sessions (supervised at least twice per week)
- Pts should exercise independently at home between gym sessions •
- Programme should offer combination of endurance and strength training
- Endurance (aerobic) training:
- Determine pt’s HRmax
- Aim for 20 – 30 minutes high intensity (60-80% of HRmax) endurance exercise (eg walking, cycling, jogging)
- In severe pts: 20 – 30 mins of interval training (short bouts high intensity training interspersed by rest)
- Resistance training:
- Both upper and lower extremities should be trained.
- Determine the pt’s 1RM
- Aim for 2 – 4 sets of 8 – 12 reps at intensities ranging from 50 – 85% of 1 RM
- Progression of training load based on pt’s tolerance
|
Outcome measures - Activities of daily living – London Chest Activity of Daily Living Scale
- Health-related quality of life – SF-36, St George’s Respiratory Questionnaire, Chronic Respiratory Questionnaire
- Dyspnoea – Medical Research Council Breathlessness Score, Borg Scale
- Exercise tolerance – 6MWD, Shuttle walk test, 3 min step test
|
Compulsory reading on MOODLE Ryrsø CK, Godtfredsen NS, Kofod LM, et al. Lower mortality after early supervised pulmonary rehabilitation following COPD exacerbation: a systematic review and meta-analysis. BMC Pulm Med 2018;18:154. Paneroni M, Simonelli C, Vitacca M, Ambrosino N. Aerobic exercise training in very severe chornic obstructive pulmonary disease: a systematic review and meta-analysis. Am J Phys Med Rehabil 2017;96:541-48. |