using knowt Ch. 24 Assessment of the Integumentary System
Assessment: Integumentary System
Author: Margaret R. RateauConceptual Focus:
Health Promotion
Tissue Integrity
Learning Outcomes:
Describe the structures and functions of the integumentary system.
Link the age-related changes in the integumentary system to differences in assessment findings.
Obtain significant subjective and objective data related to the integumentary system from a patient.
Compare the components for describing primary and secondary lesions.
Perform a physical assessment of the integumentary system using appropriate techniques.
Specify the structural and assessment differences in light- and dark-skinned persons.
Distinguish normal from common abnormal findings of a physical assessment of the integumentary system.
Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the integumentary system.
Key Terms:
Alopecia
Dermis
Epidermis
Erythema
Hirsutism
Intertriginous
Keloid
Keratinocytes
Melanocytes
Mole (Nevus)
Pruritus
Sebaceous Glands
Overview of the Integumentary System:The integumentary system is the largest organ of the body, composed of skin, hair, nails, and certain glands. The skin consists of two major layers: the epidermis (outer layer) and the dermis (inner layer), with the subcutaneous tissue lying beneath the dermis. The skin's complexity is comparable to other organs, but its visibility allows for easy assessment. Observing and palpating the skin aids in identifying abnormalities, understanding their significance, and facilitating early intervention.
Structures and Functions of Skin and Appendages
Structures
Epidermis
The epidermis, the outer layer of the skin, is relatively thin, ranging from 0.5 mm on the eyelids to 1.5 mm on the palms and soles. It has no lymphatic or vascular structures and is supported by passive circulation from the dermis. The epidermis consists of 5 distinct layers:
Stratum Corneum: The surface layer.
Stratum Germinativum: The deepest layer.
Most epithelial cells are keratinocytes (90%), with other cells including melanocytes, Langerhans’ cells, and Merkel cells. Keratinocytes originate in the basal layer, mature, and move to the surface over approximately 28 days, where they form the stratum corneum. Keratin, produced by keratinocytes, is essential for the skin's protective barrier function.
Melanocytes in the basal layer produce melanin, protecting against UV sunlight and giving color to skin and hair. Melanin production is stimulated by sunlight and hormones. Differences in melanin and melanocyte distribution result in varying skin colors across individuals.
Langerhans’ cells are immunocompetent and crucial for immune responses; depletion of these cells can lead to increased susceptibility to skin diseases. Merkel cells, also in the basal layer, are involved in the sensation of light touch.
The basement membrane zone between the epidermis and dermis acts as a support structure and facilitates fluid exchange. Damage to this zone can result in blisters.

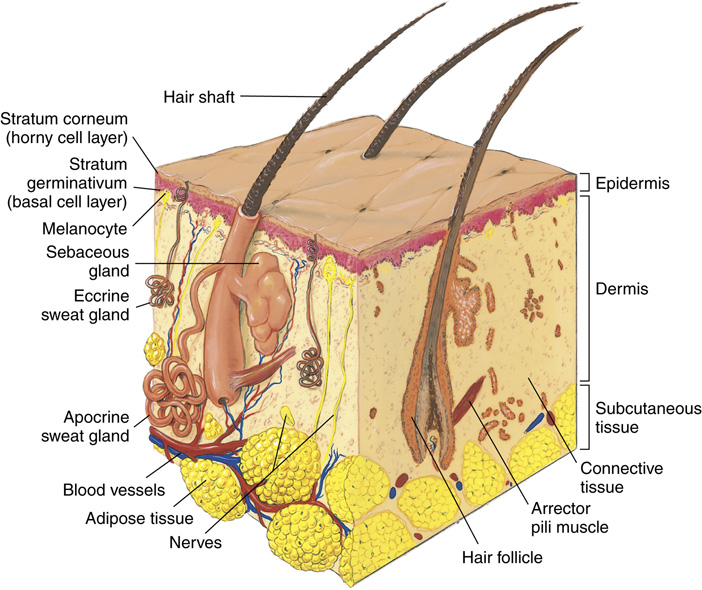
Dermis
The dermis, situated below the epidermis, ranges from 0.6 mm on the eyelids to 3.0 mm on the back and palms. This layer is very vascular, containing blood vessels, nerves, lymphatic vessels, hair follicles, and glands.
The dermis comprises three types of connective tissue:
Collagen: Provides strength and durability, critical in wound healing.
Elastic Fibers and Reticular Fibers: Provide elasticity and support.
The dermis has two layers:
Papillary Layer: Thin and contains ridges that form fingerprints.
Reticular Layer: The thicker, deeper layer made of dense collagen bundles.
Subcutaneous Tissue
The subcutaneous tissue is beneath the dermis, consisting of loose connective tissue and fat cells, providing insulation, cushioning, and energy storage. It connects the skin to underlying structures like muscle and bone.

Skin Appendages
Skin appendages include hair, nails, and glands (sebaceous, apocrine, and eccrine). They extend from the epidermis into the dermis and receive nutrients from it.
Hair: Covers most of the body except for specific areas like palms and soles. Hair color results from heredity and melanin type and amount. Hair grows about 1 cm per month and individuals lose approximately 50-100 hairs daily.
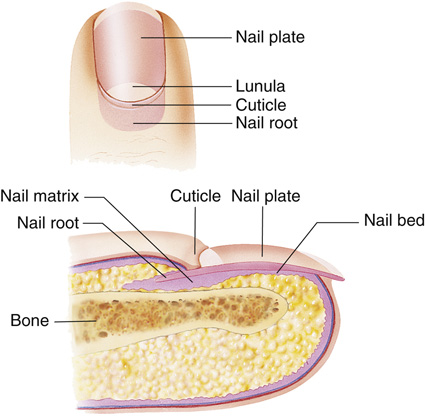
Nails: Made of keratinized cells. The visible portion is the nail body, while the nail root lies hidden beneath the skin. The lunula is the site of nail growth.
Glands:
Sebaceous Glands: Secrete sebum, which lubricates the skin and hair. These glands are influenced by sex hormones.
Apocrine Sweat Glands: Located in areas like the axilla and groin; connected to hair follicles and become active at puberty.
Eccrine Sweat Glands: Found across most of the body; primary functions include cooling the body and waste excretion.
The secretion and activity of eccrine glands can increase significantly under extreme conditions, helping with body temperature regulation.


Functions of the Integumentary System
Main Functions
Protection: The skin acts as a barrier against external environmental factors, such as bacteria and viruses, preventing invasion and excess water loss.
Insulation: The fat in the subcutaneous layer insulates the body and provides protection from trauma.
UV Radiation Protection: Melanin in the skin screens and absorbs UV radiation.
Sensory Function
The skin contains nerve endings and special receptors that collect sensory information from environmental stimuli, including pain, heat, cold, touch, pressure, and vibration.
Heat Regulation
The skin controls body temperature through vasoconstriction and vasodilation in response to internal and external temperature changes. It helps regulate body temperature through insensible water loss (600 to 900 mL daily) from the lungs and skin.
Excretory Function
Sebum and sweat lubricate the skin surface and play a role in the excretory function.
Vitamin D Synthesis
The epidermis synthesizes vitamin D when UV light acts on precursor cells, which is crucial for calcium and phosphorus balance.
Gerontologic Assessment Differences in Integumentary System
Changes and Assessment Findings
Skin:
↓ Subcutaneous fat, muscle laxity, degeneration of elastic fibers, collagen stiffening ➔ Wrinkling, sagging skin, delayed flattening when pinched.
↓ Extracellular water and sebaceous gland activity ➔ Dry, flaking skin.
Increased capillary fragility ➔ Bruising.
↑ Melanin in basal layer ➔ Solar lentigines (age spots).
↓ Blood supply ➔ Diminished rosy appearance, skin cool to touch, reduced sensitivity.
↓ Proliferative capacity ➔ Delayed wound healing.
Hair:
↓ Melanin ➔ Gray or white hair.
↓ Oil ➔ Dry, coarse hair, scaly scalp.
↓ Hair density ➔ Thinning and hair loss.
Nails:
↓ Peripheral blood supply ➔ Thick, brittle nails, reduced growth.
Increased keratin ➔ Longitudinal ridging.
↓ Circulation ➔ Prolonged blood return on nail blanching.
Gerontologic Considerations: Effects of Aging on Integumentary System
Many skin changes occur with aging. Depending on how you view yourself, the normal, visible effects of aging on the skin and hair may have a profound psychologic effect. Having a youthful look may affect a person’s self-image, and the appearance of the signs of aging can threaten self-concept.
Aging Effects on Skin Structure
The junction between the dermis and epidermis flattens, causing the skin layers to lose their tight bond, making skin tears and other trauma more common as the epidermis separates from the dermis.
Collagen and Elastic Fibers: Collagen fibers stiffen, and elastic fibers degenerate, leading to a decrease in subcutaneous tissue, contributing to wrinkling.
Dry Skin: Fewer free fatty acids in the epidermis result in dry, scaly, and itchy skin. This, combined with scratching, increases the risk for skin cracks and secondary infections.
Subcutaneous Fat: Decreased subcutaneous fat significantly increases the risk for traumatic injury, hypothermia, and skin shearing, elevating the potential for pressure injuries.
Effects of Chronic UV Exposure
Chronic UV exposure is the major cause of premature aging or photoaging and skin wrinkling.
Cumulative Damage: Sun damage is cumulative; areas such as the face and hands, which are sun-exposed, show more pronounced wrinkling compared to sun-protected areas.
Skin Cancer Risk: Photoaged skin is more susceptible to skin cancers as UV exposure diminishes the skin's ability to repair cellular damage.
Other Contributing Factors: Diabetes, smoking, and alcohol use also contribute to skin aging effects.
Changes in Hair and Nails
Reduced Melanocytes: Fewer melanocytes lead to faded hair color.
Dry, Thin Hair: Hormonal and vitamin deficiencies can cause hair to become dry and thin, leading to alopecia.
Nail Changes: The growth rate of hair and nails decreases; nails become brittle, more susceptible to splitting and yellowing, and toenails may thicken with age.
Gland Atrophy: With aging, apocrine and eccrine sweat glands atrophy, resulting in dry skin and reduced body odor.
Benign Neoplasms and Skin Lesions
Benign neoplasms related to the aging process can occur, including:
Seborrheic Keratoses: Common benign skin growths.
Vascular Lesions: Such as cherry angiomas and skin tags.
Actinic Keratoses: Premalignant lesions that appear on areas of chronic sun exposure, increasing the risk for squamous and basal cell cancers, particularly in individuals with fair skin and light eyes.
Assessment of Integumentary System
General Skin Assessment
The general skin assessment begins with your first contact with the patient and continues throughout the examination. Take note of the overall condition of the patient’s skin and hair, recording a general statement about the skin’s physical condition. Specific areas of the skin will be assessed when examining other body systems unless the chief complaint is a skin problem.
Normal Physical Assessment of Integumentary System (Table 24.2)
Skin:• Evenly pigmented; no petechiae, purpura, lesions, or excoriations• Warm, good turgor
Nails:• Pink, oval, adhere to nail bed with 160-degree angle
Hair:• Shiny and full; amount and distribution appropriate for age and gender• No flaking of scalp, forehead, or pinna
Case Study: Patient Introduction
D.A. is a 74-year-old woman who presents with concerns related to "spots" on her face, which she believed to be age spots. She became worried after a friend was diagnosed with malignant melanoma.
Discussion Questions
Which type of assessment should you perform: comprehensive, focused, or emergency?
What are the possible causes of D.A.’s facial lesions?
What questions would you ask D.A. to determine the possible causes?
Subjective Data
Conduct the interview with a sensitive and nonjudgmental approach, as visible skin problems may affect the patient’s body image and self-concept. A thorough health history can reveal possible causes and their impact on the patient's life.
Important Health Information
Health History
A health history reveals previous trauma, surgery, or disease involving the skin. Note conditions linked to jaundice, delayed wound healing, cyanosis, or pallor, and gather information on food sensitivities, allergies, skin reactions to insect bites, and UV light exposure.
Medications
Document a thorough medication history, asking about skin-related problems from medications, and documenting the use of specific skin treatments (e.g., for acne).
Health History Questions (Table 24.3)
Health Perception–Health Management:
• Describe your daily hygiene practices.
• What skin products are you now using?
• Describe any current skin problems, including onset, course, and treatment.
Nutritional-Metabolic:
• Describe any changes in your skin, hair, nails, and mucous membranes.
• Have you noticed any recent changes in the way sores or wounds heal?
Elimination:
• Have you noticed recent changes in your skin related to excess sweating, dryness, or swelling?
Activity-Exercise:
• Do your leisure or work activities involve using any chemicals that might irritate your skin?
Sleep-Rest:
• Does your skin problem keep you awake or awaken you from sleep?
Cognitive-Perceptual:
• Do you have any pain associated with your skin problem?
Self-Perception–Self-Concept:
• How does your skin make you feel about yourself?
Role-Relationship:
• Has your skin problem changed your relationships with others?
Surgery or Other Treatments:
• Determine if any surgeries or treatments have been done on the skin, such as cosmetic surgery or phototherapy.
Make sure to document all findings comprehensively to provide a clear understanding of the patient's skin condition and any potential underlying issues.
Functional Health Patterns
Health Perception–Health Management Pattern
Assess health practices related to daily hygiene, including self-care habits.
Inquire about the frequency of sunscreen use and its sun protection factor (SPF).
Note the use of personal care products (e.g., shampoos, moisturizing agents, cosmetics), including brand names, quantity, and frequency.
Record a description of any current skin problems, including onset, symptoms, course, and treatment.
Document any medications used for treating hair loss.
Diseases With Skin Manifestations (Table 24.4)
Systemic Problem | Skin Manifestations |
|---|---|
Cardiovascular | |
Peripheral vascular disease | Loss of hair on hands and feet. Delayed capillary filling. Dependent rubor (redness), pain |
Rheumatic heart disease | Petechiae, urticaria, nodules, erythema |
Thromboangiitis obliterans (Buerger disease) | Pallor or cyanosis, gangrene, ulceration |
Venous ulcers | Leathery, brownish skin on lower leg; itching, concave lesion with edema. Scar tissue with healing |
Endocrine | |
Addison disease | Loss of body hair (especially axillary), generalized hyperpigmentation (accentuated in folds) |
Androgen deficiency | Development of sparse hair. Marked ↓ in sebum production |
Androgen excess | Enlarged facial pores, male sex characteristics, acne, accelerated coarse hair growth |
Diabetes | Erythematous plaques of shins, delayed wound healing, neuropathy, acanthosis nigricans (velvety, dark skin on the neck and in skin folds) |
Glucocorticoid excess (Cushing syndrome) | Atrophy, striae, epidermal thinning, telangiectasia, acne. ↓ Subcutaneous fat over extremities. Thin, loose dermis. Impaired wound healing. Increased vascular fragility. Mild hirsutism. Excess collection of fat over clavicles, back of neck, abdomen, and face |
Hyperpituitarism (acromegaly) | Coarsened skin, deepened lines. ↑ Oiliness and sweating, acne. ↑ Number of nevi, hyperpigmentation; hypertrichosis (excess hair growth) |
Hyperthyroidism | ↑ Sweating, warm skin with persistent flush, thin nails, alopecia. Fine, soft hair |
Hypoparathyroidism | Opaque, brittle nails with transverse ridges. Coarse, sparse hair with patchy alopecia |
Hypothyroidism | Cold, dry, pale to yellow skin. Generalized nonpitting edema. Dry, coarse, brittle hair. Brittle, slow-growing nails |
Gastrointestinal | |
Cystic fibrosis | Abnormal sweat gland function |
Deficiency of essential fatty acids | Scaly skin |
Inflammatory bowel disease | Mouth ulcers, erythema nodosum |
Liver disease and biliary tract obstruction | Jaundice, itching, pigmentary abnormalities, changes in nails and hair, spider angiomas, telangiectasia |
Malabsorption syndrome | Acquired ichthyosis (dry, scaly skin) |
Hematologic | |
Anemia | Pallor, hyperpigmentation, pale mucous membranes, hair loss, nail dystrophy |
Clotting disorders | Purpura, petechiae, bruising |
Immune | |
HIV infection | Kaposi sarcoma, eosinophilic folliculitis |
Hodgkin lymphoma | Itching, sensitive skin |
Non-Hodgkin lymphoma | Papules, nodules, plaques, itching |
Metabolic | |
Nicotinic acid (niacin) deficiency | Redness of exposed areas of skin of hand or foot, face, or neck; infected dermatitis |
Vitamin B1 (thiamine) deficiency | Edema, redness of soles of feet |
Vitamin B2 (riboflavin) deficiency | Red fissures at corner of mouth, glossitis |
Vitamin C deficiency | Petechiae, purpura, bleeding gums |
Musculoskeletal and Connective Tissue | |
Dermatomyositis | Edema; purplish-red upper eyelids; scaly, macular erythema over knuckles |
Scleroderma | Leathery hardening and stiffness of skin |
Systemic lupus erythematosus | Discoid lesions, maculopapular semiconfluent rash (butterfly rash), alopecia, mouth ulcers |
Neurologic | |
Chronic sensory polyneuropathies, spinal cord trauma | Trophic changes in skin resulting from sensory denervation, pressure injuries, anesthesia, paresthesias |
Renal | |
Chronic kidney disease | Dry skin, itching, uremic frost, pallor, bruises |
Reproductive Organs | |
Paget disease | Eczematous patch of nipple and areola |
Primary syphilis | Chancre |
Secondary syphilis | Generalized skin lesions, alopecia |
Tertiary syphilis | Gummas |
Respiratory | |
↓ Oxygenation due to respiratory disease | Cyanosis |
Genetic Risk Alert
The primary risk factor leading to skin cancer and melanoma is environmental exposure to UV radiation, which damages DNA and can lead to skin cancer.
Inherited genetic factors can increase skin cancer risk, especially if there is a family history of melanoma.
Fair complexion individuals have an increased risk for skin cancer.
Obtain information about family history of skin diseases including congenital and familial diseases (e.g., alopecia, psoriasis) and systemic diseases with skin manifestations (e.g., diabetes, thyroid disease, cardiovascular diseases, immune disorders). Note any family and personal history of skin cancer, particularly melanoma.
Nutritional-Metabolic Pattern
Ask about the condition of skin, hair, nails, and mucous membranes.
Inquire about any dietary changes that could impact skin condition. A diet history should assess the adequacy of crucial nutrients for healthy skin and wound healing such as protein and vitamins A, D, E, and C.
Note any food allergies that may result in skin reactions.
For obese patients, ask about chafing or rashes in intertriginous areas (e.g., below breasts, axillae, groin), which are prone to infections like skin tags, candidiasis, intertrigo, and erythrasma.
Observe for any signs of excess or lack of sweating, and ask about poor or delayed wound healing.
Elimination Pattern
Inquire about skin-related issues such as dehydration, edema, and pruritus (itching), which indicate changes in fluid balance.
If urinary or fecal incontinence is a problem, assess the condition of the skin in the anal and perineal areas.
Activity-Exercise Pattern
Gather information on environmental hazards related to hobbies or recreational activities, including exposure to carcinogens, chemical irritants, and allergens.
Ask if any skin changes occur during exercise or physical activities.
Sleep-Rest Pattern
Discuss any changes in sleep patterns attributed to skin problems, particularly issues like itching that might disrupt sleep.
Poor sleep can manifest as dark circles under the eyes and decreased firmness in facial skin.
Cognitive-Perceptual Pattern
Assess the patient's perception of sensations such as heat, cold, pain, and touch.
Note any discomfort related to skin problems, particularly in intact skin, and inquire about reports of unusual skin sensations.
Patients with neuropathy might describe numbness, tingling, or crawling sensations. Ask about joint pain and assess joint mobility, as skin problems may affect mobility.
Self-Perception–Self-Concept Pattern
Explore feelings associated with having a skin problem, including sadness, anxiety, despair, or altered body image.
Visible skin issues like aging signs, acne, rosacea, or psoriasis can have significant emotional impacts.
Role-Relationship Pattern
Determine how skin problems influence relationships with family, peers, and coworkers.
Assess the impact of environmental factors such as occupational exposure to irritants and sun, which can lead to contact dermatitis.
Sexuality-Reproductive Pattern
Assess the impact of skin issues on sexual activity.
Note reproductive status relevant to treatment options, particularly in female patients using teratogenic drugs such as isotretinoin or topical fluorouracil for skin conditions.
Advise that pregnant women or women who could become pregnant should avoid these medications.
Coping–Stress Tolerance Pattern
Evaluate how stress may contribute to or exacerbate skin problems.
Discuss the coping strategies the patient employs to manage skin-related issues.
Value-Belief Pattern
Assess any cultural or religious beliefs that might affect the patient's self-image concerning their skin problem.
Discuss values and beliefs that may influence or restrict treatment options.
Case Study: Subjective Data Assessment for D.A.
Subjective Data
A focused subjective assessment of D.A. reveals the following:
History: Negative except for an appendectomy at age 16.
Medications: None at present. No known allergies (NKA).
Health Perception–Health Management: Washes her face with a skin cleanser in the morning and nighttime. After cleansing, she applies a moisturizer with SPF 15. She has used these facial products for the past 3 years since she first started noticing small age spots appearing. Before that, she just used soap and water.
Nutritional: D.A. reports that her skin seems drier as she ages but otherwise has no changes besides the “age spots.” Denies any changes in the way cuts or sores heal. No weight loss. Does not take any vitamins or mineral supplements.
Elimination: Although her skin is a little dry, D.A. does not perceive it to be excessively dry. Denies excess sweating or any swelling.
Activity-Exercise: Loves to garden and go for walks outdoors. Reports a history of frequent, sometimes severe, sunburns as a child. No use of sunscreen growing up but does remember her mother making her wear T-shirts over her bathing suits to help prevent sunburn. Has used sunscreen for the past 20 years when outdoors. Reapplies as needed.
Cognitive-Perceptual: Denies any pain or discomfort associated with skin lesions.
Coping–Stress Tolerance: Fearful that she might have skin cancer.
Discussion Questions
Which subjective assessment findings concern you most?
The history of frequent, severe sunburns as a child raises concern for potential sun damage leading to skin cancer. D.A.'s fear of developing skin cancer and the appearance of age spots also warrant close attention.
What should you include in the physical assessment? What specific characteristics of the skin lesions would you be looking for?
The physical assessment should focus on inspecting the skin lesions for their size, shape, color, texture, distribution, and any changes in the skin surrounding the lesions. Assess if the lesions are primary or secondary, check for any signs of inflammation or infection, and consider the possibility of malignancy based on the characteristics observed.