Lecture 8_Integument (2)
Cells change in structure and appearance from Stratum Basale to stratum Corneum. This is accomplished by specialized form of Apoptosis (programmed cell death).
As cells move up through the layers, they become more keratinized, nucleus and organelles break down, and plasma membrane thickens resulting in a tough, protective outer layer that is essential for skin barrier function.
Cells slough off as dandruff and dander.
Shed 50,000 cells every minute.
1. Epidermis. Keratinized stratified squamous epithelium. 5 layers.
Stratum Corneum. The outermost layer composed of dead keratinized cells that provide a protective barrier against environmental damage, water loss, abrasion, penetration, against biological and chemical assaults.
Stratum Lucidum. A thin, translucent layer found only in thick skin areas such as the palms and soles, composed of several layers of flattened, dead keratinocytes that contribute to the overall toughness of the epidermis.
Stratum Granulosum. Cell appearance changes. Keratinization begins. This layer contains keratinocytes that begin to flatten and lose their nuclei, as well as lamellar granules; water resistant glycolipid slows water loss. Cells above this layer die because they are to far from dermal capillaries.
Stratum Spinosum. Contains web-like system of intermediate prekeratin filaments attached to desmosomes that provide strength and flexibility to the skin. This layer also contains Dendritic (Langerhans) cells, and Macrophageskey activator of the immune system.
Stratum Basale. This is the deepest layer of the epidermis, where cell division occurs. It is primarily composed of a single row of actively mitotic stem cells that produce new keratinocytes(daughters) push upwards to replenish the upper layers of the skin. Melanosomes and Dendritic cells. Melanocytes compose 10 -25% of this layer.
2. Dermis.
Innervated and vascularized.
Contains epidermal hair folicules; Sebaceous glands, and Sudoriferous glands, which play crucial roles in thermoregulation and skin hydration.
Papillary Layer
Looser Areolar connective tissue.The uppermost layer of the dermis, characterized by thin collagen fibers and numerous capillaries, providing nutrients to the epidermis and aiding in thermoregulation.
Dermal papillae. Small, peg-like projections that interdigitate with the epidermis, increasing the surface area for exchange of gases, nutrients, and waste products.
Meissner’s corpuscle ( light touch receptors)
Phagocytes, such as macrophages can patrol for microorganisms.
Reticular Layer.
Dense Irregular connective tissue contains elastic fibers that provide strech-recoil properties.
Collagen fibers; provide strength and resiliency, allowing the skin to withstand tension and deformation without damage. Binds water
Pacinian corpuscle (lamellated) for pressure sentitivity, which are located deeper in the dermis, play a crucial role in detecting deep pressure and vibration, enhancing our tactile perception.
3. Hypodermis (subcutaneous layer)
Not part of the skin but shares some functions.
Mostly Adipose tissue that absorbs shock and insulates.
Anchors skin to underlying structures, mostly muscles.
4. Accessory & Other Structures
Sebaceous Gland:
Widely distributed; not in thick skin of palms and soles.
Most developed from hair follicles and secrete into hair follicles.
Secrete Sebum; Oily secretion
Bactericidal
Softens hair and skin.
Sudoriferous Gland
Eccrine sudoriferous glands: secretory ducts connect to pores that open up at the epidermis. Secretion is sweat; 99% water, electrolytes, antibodies, dermicin (microbe-killing peptide) and metabolic wastes.
In all skin surfaces except nipples and parts of external genitalia.
Apocrine sudoriferous glands: Secretory ducts empty directly into hair follicles.
Hair Shaft
Hair Root
Hair Papilla
Hair Bulb
Hair Follicle
Arrector Pili Muscle.
Homeostatic Imbalance
Striae
Silvery-white scars commonly known as "stretch marks"
Result from extreme stretching causing dermal tears.
Blister
Formed from acute, short-term trauma.
A fluid-filled pocket separates the epidermal and dermal layers.
Skin Color
Skin color is influenced by three main pigments:
Melanin
The only pigment produced in the skin.
Carotene
Hemoglobin
Melanin
Has two forms ranging from reddish-yellow to brownish-black.
Variations in skin color are due to the amount and form of melanin.
Produced in melanocytes, consistent relative numbers across different individuals.
Melanin migrates to keratinocytes, forming protective "pigment shields" for nuclei.
Sun exposure increases melanin production; excessive exposure can lead to skin cancer.
Carotene and Hemoglobin
Carotene
Yellow to orange pigment, visible primarily in palms and soles.
Accumulates in the stratum corneum and hypodermis.
Can convert to vitamin A, essential for vision and skin health.
Variations in skin tinge among some individuals, especially Asians, due to carotene and melanin differences.
Hemoglobin
Gives fair skin its pinkish hue.
Skin Color in Diagnosis
Cyanosis
Blue skin color due to low oxygenation of hemoglobin.
Erythema (redness)
Indicates fever, hypertension, inflammation, or allergy.
Pallor (blanching)
Occurs in anemia, low blood pressure, fear, or anger.
Jaundice
Yellow cast indicating liver disorders.
Bronzing
Caused by inadequate corticosteroid hormones in Addison's disease.
Black-and-blue marks (bruises)
Result from clotted blood beneath the skin.
Appendages of the Skin
Derivatives of the epidermis include:
Hairs and hair follicles
Nails
Sudoriferous (sweat) glands
Sebaceous (oil) glands
Hair
Composed of dead keratinized cells, containing hard keratin that is more durable than the soft keratin found in skin.
Not present in areas like palms, soles, lips, nipples, or certain external genitalia.
Functions of hair:
Alerts to insects on the skin.
Provides protection against physical trauma, heat loss, and sunlight.
Hair colors are attributed to melanin pigments, including yellow, rust, brown, and black.
Gray/white hair occurs from decreased melanin and increased air bubbles in the hair shaft.
Hair Follicles
Extend from the epidermal surface into the dermis.
Hair bulb
Expanded end of the follicle that contains the hair matrix, a region of actively dividing cells.
Hair follicle receptor (root hair plexus)
Contains sensory nerve endings, acting as touch receptors.
Arrector pili
Smooth muscle attached to the follicle, causing goosebumps and contributing to sebum secretion.
Hair papilla
Contains dermal tissue and blood supply to the hair bulb.
Types and Growth of Hair
Vellus hair
Fine, pale body hair found in children and adult females.
Terminal hair
Coarse and long hair found in eyebrows and scalp, becomes prominent at puberty.
Appears in the axillary and pubic regions of both sexes and on the face and neck of males.
Hair follicles have active and regressive cycling phases.
Average hair growth is about 2.25 mm per week, with loss of approximately 90 scalp hairs daily.
Sudoriferous (Sweat) Glands
Located on all skin surfaces except nipples and parts of external genitalia; approximately 3 million per person.
Two main types:
Eccrine sweat glands
Apocrine sweat glands
Eccrine Sweat Glands
Most numerous type of sweat gland.
Predominantly found on palms, soles, and forehead.
Ducts connect to pores; primarily functions in thermoregulation.
Secretions are primarily water (99%), along with salts, vitamin C, antibodies, dermcidin, and metabolic wastes.
Apocrine Sweat Glands
Confined to the axillary and anogenital regions.
Secrete sweat mixed with fatty substances and proteins, resulting in viscous fluid that becomes odorous upon bacterial interaction.
Generally larger than eccrine glands; ducts empty directly into hair follicles.
Become functionally active at puberty; specific functions are not entirely understood.
Modified apocrine glands include ceruminous glands (earwax secretion) and mammary glands (milk secretion).
Sebaceous (Oil) Glands
Distributed widely throughout the skin but are absent in the thick skin of palms and soles.
Most sebaceous glands develop from hair follicles, secreting into them.
Sebum
Oily secretion that softens hair and skin and has bactericidal properties.
Functions of the Integumentary System
Protection against chemical, physical, and biological barriers.
Regulation of body temperature.
Reception of cutaneous sensations.
Metabolic functions.
Blood reservoir (up to 5% of body blood volume).
Excretion of nitrogenous wastes and salts via sweat.
Protection – Chemical Barriers
Skin secretions create an acid mantle which retards bacterial growth.
Dermcidin found in sweat has bactericidal properties, along with certain substances in sebum.
Natural antibiotics (defensins) combat bacterial infections.
Melanin serves as a defense against UV radiation damage.
Protection – Physical Barriers
The flat, dead cells of stratum corneum surrounded by lipids provide a barrier against water and water-soluble substances.
Keratin and glycolipids primarily block substances; limited penetration occurs for lipid-soluble substances (e.g., organic solvents, plant oleoresins, salts of heavy metals).
Protection – Biological Barriers
Dendritic cells in the epidermis can present foreign antigens to white blood cells.
Macrophages in the dermis perform similar functions, enhancing immune response.
DNA itself absorbs UV radiation, converting it to heat, providing additional protection.
Functions of the Integumentary System (Temperature Regulation)
Under normal conditions, routine insensible perspiration occurs (~500 ml/day) when environmental temperatures are below 31-32 °C.
Increased body temperature results in dilation of dermal blood vessels and heightened sweat gland activity (sensible perspiration) to cool the body.
Conversely, when body temperature drops, dermal blood vessels constrict, preventing heat loss.
Functions of the Integumentary System (Cutaneous Sensations)
Comprised of cutaneous sensory receptors that detect temperature, touch, and pain.
Metabolic functions includes the synthesis of vitamin D precursor and activation of certain hormones.
Acts as a blood reservoir (up to 5% of body volume) and aids in excretion of nitrogenous wastes and salt through sweat.
Skin Cancer
Most skin tumors are benign (non-cancerous) and do not metastasize.
Common risk factors involve UV radiation exposure (DNA mutations) and frequent skin irritation.
Major types of skin cancer include:
Basal cell carcinoma
Squamous cell carcinoma
Melanoma
Basal Cell Carcinoma
The least malignant and most common type of skin cancer.
Arises from stratum basale cells that proliferate, slowly invading dermis and hypodermis.
Characterized by shiny, dome-shaped nodules.
Typically cured by surgical excision in 99% of cases.

Squamous Cell Carcinoma
Represents the second most common skin cancer type affecting keratinocytes of the stratum spinosum.
Appears as scaly, reddened papules on the scalp, ears, lower lip, and hands.
Does metastasize but has a favorable prognosis if treated with radiation or removed surgically.
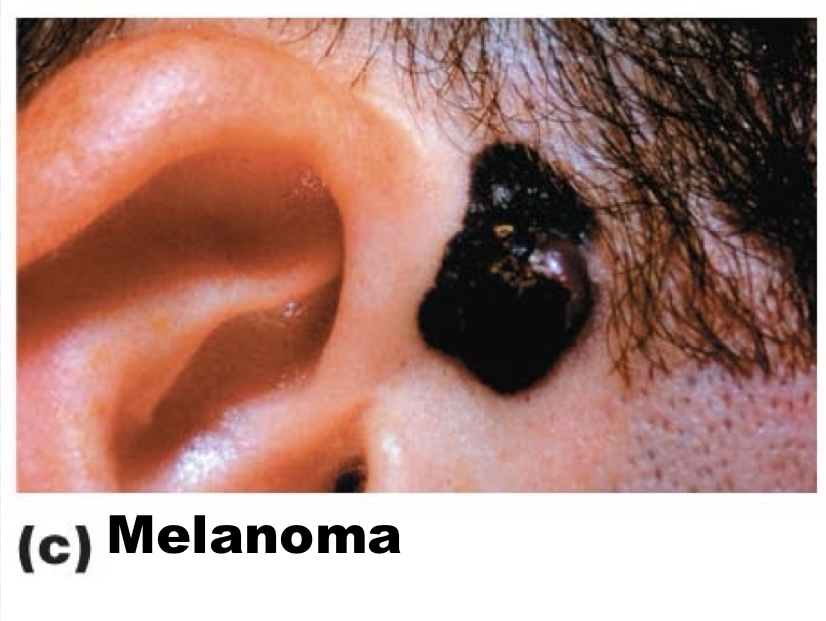
Melanoma
Represents the cancer of melanocytes and is the most dangerous form of skin cancer.
Highly metastatic and resistant to chemotherapy.
Early detection is critical; treatment involves wide surgical excision and immunotherapy.
Key indicators for early detection follow the ABCD rule:
A: Asymmetry
B: Border irregularity
C: Color variations
D: Diameter > 6 mm.
Burns
Tissue damage can occur from heat, electricity, radiation, or certain chemicals, leading to protein denaturation and cell death.
Immediate threats from burns include dehydration and electrolyte imbalance, potentially resulting in renal shutdown and circulatory shock.
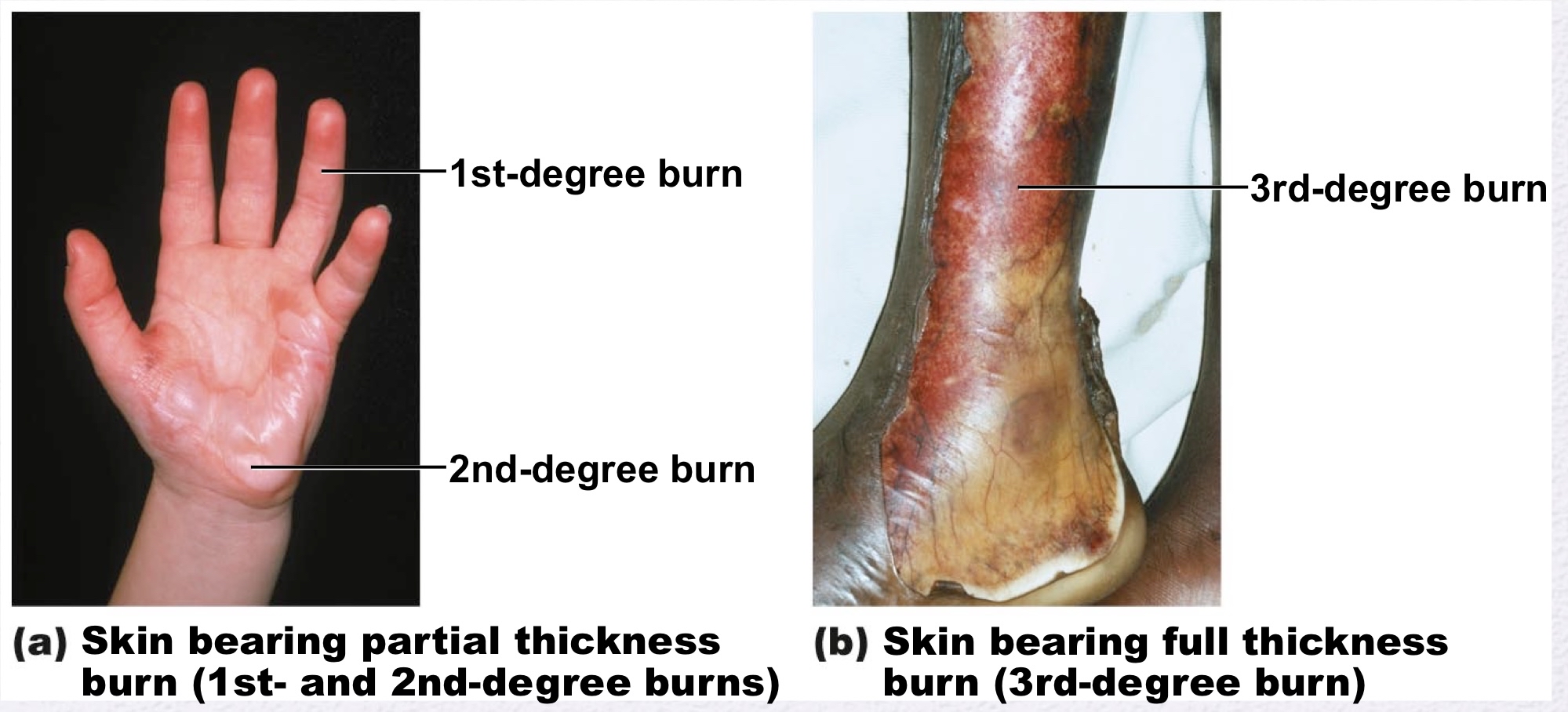
Burns Classified by Severity
Partial-thickness burns
First-degree burns
Damage limited to the epidermis, characterized by localized redness, edema, and pain.
Second-degree burns
Affect both the epidermis and upper dermis, resulting in blister formation.
Full-thickness burns
Third-degree burns
Involve the entire thickness of the skin, appearing gray-white, cherry red, or blackened.
These burns are generally painless due to nerve ending destruction and require skin grafting.
Severity and Treatment of Burns
Diagnostic criteria for critical burns:
25% of body experiencing second-degree burns.
10% of body affected by third-degree burns.
Involvement of hands, feet, or face with third-degree burns.
Treatment strategies include:
Debridement of damaged skin.
Antibiotic application.
Temporary coverings and skin grafts if necessary.