Week 1
Guide:
Black text- textbook (main info)
blue text- powerpoint additions
green text- professor added
orange text- personal info I added to help understand
What is Research:
to search again
to examine carefully
diligent and systematic inquiry
discovery
goal is to to develop and empirical body of knowledge for a discipline
Research is systematic, rigorous, logical investigation with the aim of answering questions about nursing phenomena. (pg 6)
Phenomena can be defined as occurrences, situations, or facts that are perceptible by the senses. (pg 6)
Research is systematic: there is a method to finding something. If you do something in your research and repeat the study, the findings should be the same.
Role of Research in Nursing:
The Significance of Research to Practice:
expands the discipline’s unique body of scientific knowledge
forms the foundation for evidence-informed nursing practice
allows practice to change with work environments and the most common health issues
Nurses use research to affect positive outcomes for their patients.
Evidence-informed Decision-Making:
Refers to a “continuous interactive process involving the explicit, conscientious and judicious consideration of the best available evidence to provide care” (CNA, 2010, p.1).
With evidence-informed practice, the methods for gathering evidence are the same as the processes used for evidence-based practice; however, the evidence also incorporates expert opinion, clinical expertise, patient preference, and other resources.
It focuses on amore inclusive and interactive process of decision making that pertains to all nurses
Involves acknowledging and considering the myriad factors that constitute decision- making, taking into account patient preference, culture, history, and local context. (pg 7)
Evidence-Based Practice:
The process of systematically finding, appraising, and using research findings as the basis for clinical practice for making decisions about patient care.
EBP is the process by which nurses make clinical decisions based on the best available research evidence, their clinical practice and patient preferences, in the context of available resources.
Evidence generated by nursing research provides support for the quality and cost-effectiveness of nursing intervention.
Practice based on evidence from nursing research is an approach that enables clinicians to provide the highest quality of care in meeting the multifaceted needs of patients and families.
Within the context of nursing, evidence-based practice is a “problem-solving approach to the delivery of health care that integrates the best evidence from well-designed studies and patient care data and combines it with [clinical expertise and] patient preferences and values” (Melnyk et al., 2010, p. 51).
Evidence-based practice: Research is completed, published in academic journals, and then assessed to determine application to clinical practice—this results in practice that is evidence based. (pg 7)
The strict application of algorithms and guide lines, along with selective trials that overlook multiple morbidities, means that individual patients are not always receiving the most appropriate care.
Evidence-based practice can become rigid and not consider patient preferences, individuality, and contexts.
So we have moved on from an evidence based approach to an evidence informed approach.
Similarities | Differences | |
Evidence Based | begins with a question | in a research study, the question is tested with a de sign appropriate for the question and with specific methods (sample, instruments, procedures, and data analysis) |
Evidence Informed | begins with a question | a question is used to search the literature for studies already completed and then you critically appraise this literature in order to answer your clinical question. |
Yes, as nurses, you can practice Evidence-Based Practice (EBP) while making evidence-informed decisions. These two concepts are complementary and often work hand-in-hand in clinical settings.
Here's how they connect:
1. Evidence-Based Practice (EBP):
Core Focus: EBP emphasizes using the best available scientific evidence—usually from research studies like randomized controlled trials, clinical guidelines, or systematic reviews—to guide clinical care.
Process: EBP involves a structured process:
Ask a clinical question.
Acquire the best available evidence.
Appraise the quality of the evidence.
Apply the evidence in practice.
Assess the outcomes.
- Goal: To improve patient care by using reliable, research-backed information.
2. Evidence-Informed Decision Making:
Core Focus: While EBP prioritizes research, evidence-informed decision making is more flexible and integrates other important factors:
Best research evidence
Clinical expertise
Patient values and preferences
Contextual factors like resources, cultural considerations, and individual patient needs.
- Goal: To make decisions that are informed by evidence but are also personalized to the specific context or patient situation.
How Do They Work Together?
EBP provides the foundation of reliable, research-backed knowledge. It ensures that your care is grounded in the best science available.
Evidence-informed decision making takes this further by incorporating clinical judgment and patient-centered care into the mix. While EBP guides you with solid evidence, decision making acknowledges that every clinical situation may require adaptations based on individual patient needs and real-world constraints.
Example:
A nurse treating a patient with chronic pain may use EBP to review the latest clinical guidelines on pain management, selecting the most effective interventions based on research.
However, through evidence-informed decision making, the nurse also considers the patient's personal preferences, cultural background, previous experiences with pain management, and the availability of resources at the hospital. The nurse may adapt the treatment based on these factors while still relying on the core evidence provided by EBP.
In Practice:
- Nurses practice EBP by relying on research and clinical guidelines, but they make evidence-informed decisions by balancing that evidence with the patient's specific circumstances, preferences, and context. This allows for more personalized, patient-centered care that is still rooted in solid evidence.
Conclusion:
Yes, nurses practice Evidence-Based Practice while making evidence-informed decisions. EBP provides the scientific foundation, while evidence-informed decision making ensures that this science is applied in a flexible, patient-centered, and context-sensitive manner. Both are essential for delivering high-quality, individualized care.
Without evidence informed decision making and evidence based practice there would be fatal consequences such as poor patient outcomes and deaths.
Using Research in Practice
Synthesis of knowledge (research, theory, and clinical experiences)
Effect of philosophy
Making a change in practice
Evaluation of change for patient, provider, and health care system
E-T-P Link
Research links theory, education, and practice. (pg 8)
Theory informs practice, how knowledge based only on experience can be biased and limited, and how approaching clinical problems with systematic, scientific research methods can improve patient outcomes.
The way we synthesize knowledge:
Education
The knowledge you gain through your educational program, whether theory or research based, will inform the decisions that you make in your practice
Theory
Practice
Research and Trends
Trends that influence nursing research
An emphasis health disparities among the Indigenous peoples.
An emphasis on underservices communities and vulnerable populations.
A focus on palliative care and Medical Assistance in Dying.
An increased prevalence of life-threatening illnesses due to new life-sustaining technologies.
An increase in mental health illnesses.
An expanding population of older people.
An expanding population with chronic illnesses and the impact on health care.
The impact of Covid on the health of individuals and communities.
A focus on the maternal-neonatal mortality occurrences.
Two priority health challenges that have been identified are improving access to addiction and mental health services, and home and community care (CFHI, 2020b). These two areas were identified by the Government of Canada as shared health priorities between federal, provincial, and territorial governments (Health Canada, 2018). (pg 15)
Nurse’s Role in Research
Nurse’s role in research includes:
Consumer- we consume the knowledge by following the evidence based practice and guidelines in our work
Generator of clinical questions- the questions we ask our colleagues practice, like “is this the best way to do this?”
Investigator/participant in research- by asking and doing the work for it
Protector of research participants
19th Century History
Key events of the 19th century:
Nursing becomes a formal discipline
Florence Nightingale publishes “Notes on Nursing” in 1859 and introduces the systematic collection and exploration of data to support health promotion and disease prevention
Schools of nursing are beginning to the established but research is in the very early stages of development
20th Century History
Key events from 1900 to 1940:
Emphasis not on research but on preparation of nurses for practice
Key events from 1950 to 1999:
First master’s program in nursing in Canada
First federally funded grant for nursing research
Doctoral programs U of A, UBC, McGill, U of T
Established the Nursing Research Fund, budgeting $25 million for nursing research in Canada
21st Century History
Key events from 2000 to 2012:
Growth of universally based Registered Psychiatric Nursing programs
First masters degree a U of B for Registered Psychiatric Nurses
COVID-19 Impact on Research
Created numerous challenges and opportunities for research in nursing.
Many projects and funding decisions delayed due to pandemic.
Has generated a plethora of research ideas and topics.
International Perspectives
Global research community made possible.
Cross-cultural and cross-national studies could be implemented.
Requires networks, databases, web sites, funding, respect for cultural perspectives.
International organizations create valuable and accessible partnerships.
For example, the World Health Organization (WHO, n.d.) has established a series of collaboration centres to advance health care for the global community. (pg 14)
Critical Thinking Challenges
What research roles are you interested in?
What effects will evidence-informed patient outcome studies have on the practice of nursing?
Have you had any experiences that make you question nursing practice?
Why is it important to have interdisciplinary and international research perspectives?
What topics in nursing do you think require further research?
Evidence informed patient outcome studies improve patient care, guided decisions by the best evidence. Improve nursing competencies, such as critical thinking problem solving, and professional development. Also cost effective care, patient satisfaction, interpersonal collaborations.
Questions from chapter 1(textbook) & Summary of Key Points:
What is the most appropriate source of information for evidence-informed practice?
A. Charge nurse
B. Attending physician
C. Clinical practice guideline
D. Nightingale’s notes on nursing
Answer: C. Clinical practice guideline
Rationale: These should be systematically developed and based on the most recent evidence.
Why are interdisciplinary networks important in research?
A. Collaboration can help solve complex problems
B. Nurses do not do independent research
C. Research funding needs to be spread across disciplines
D. There is overlap in the scopes of practice
Answer: A. Collaboration across disciplines improves patient outcomes
Rationale: It is important for research to be focused on patient outcomes, and this occurs across many disciplines.
What drives the priorities for health care research?
A. Political agenda
B. Changes in values in society
C. Trends and issues in health care
D. The United Nations
Answer: C. Trends and issues in healthcare
Rationale: Research is frequently substantiated by solving pressing problems.
Nursing research expands the body of scientific knowledge that forms the foundation of evidence-informed nursing practice.
Nurses gain research literacy through education and practical experience. As users of research, nurses must have a basic under standing of the research process and must demonstrate critical appraisal skills to evaluate the strengths and weaknesses of research be fore applying the research to clinical practice.
All nurses, whether they possess baccalaureate, master’s, or doctoral degrees, have a responsibility to participate in the research process.
Programs of research studies and replication of studies will become increasingly valuable.
Research studies will emphasize clinical issues, problems, and outcomes. Priority will be given to research studies that focus on health promotion, care for the health needs of vulnerable groups, and the development of cost effective health care systems.
Both users of research and nurse researchers will engage in a collaborative effort to further the growth of nursing research and accomplish the profession’s research objectives
Knowledge Development
Knowledge gaps: the absence of theoretical or scientific knowledge relevant to the phenomenon of interest.
Nurses ask questions that require answers from experts in the field.
Absence of theoretical/empirical knowledge.
Knowledge generation: the conduct of research that provides answers to well-thought-out research questions.
Research questions are devised about a phenomenon.
Qualitative and quantitative methods are used to answer the questions.
Knowledge distribution: through journal articles, textbooks, and public presentations to nurses.
Knowledge is shared with profession through formal (presentation, journal publications, reports) and informal (media, Internet, social networks) reporting methods.
Knowledge adoption: nurses alter their practice based on published information or as health care organizations develop policies and protocols that are informed by newly generated knowledge.
New knowledge is used to alter practice.
New knowledge is used to develop policies and protocols.
knowledge reviewed and revision: as new health issues arise, advances in clinical practice occur, or knowledge becomes outdated.
New health issues lead to the asking of new questions.
Old knowledge is revised or excluded.
New questions prompt the need for new research.
And the cycle starts again at Knowledge gap
Nursing Knowledge
Nursing knowledge is created and interpreted at various levels of abstraction, ranging from the most abstract to the most concrete thinking. Fawcett has identified five components of nursing knowledge, which span a range of abstraction levels:
Most Abstract
Most Concrete
metaparadigm- worldview of the discipline, which distinguishes its focus
philosophy- addresses questions about existence, reality, knowing, and ethics as they pertain to nursing
conceptual model- set of concepts that address broad, general ideas of interest to the discipline
theory- translate concepts into testable questions that can be explored
empirical indicator- used in theory like instruments, experiments, or procedures
Various ways that nurses inform their practice:
Personal Knowledge:
knowledge that comes from the inner experiences and maturation of the nurse.
encompasses becoming a whole, aware, genuine, and authentic self
continual life process that occurs with deep reflection
allows for interpersonal relationships
Experiential Knowledge:
knowledge that comes from repeated exposure to situations that lead to the refining of earlier ideas and thoughts
involves movement along a continuum of novice, competent, expert, and practitioner
expert practitioner is fully engaged and attuned to each situation and responds on the basis of past learning
Ethical Knowledge:
moral component of nursing knowledge
encompasses the moral principles, codes, and theories of ethical conduct
the moment-to-moment judgement of what is “right” and “responsible”
involves confrontation and resolution of ethical conflicts
Aesthetic Knowledge:
the art of nursing
the expressive, intuitive, and creative aspect of nursing
practice that incorporates poetry, art, music, and stories, allowing a deep understanding of the human experience
Sociopolitical Knowledge:
contextual knowledge that moves beyond nurse- patient relationship and the profession
understanding of culture, society, and politics
awareness of how society is organized and it implications for health
Theoretical/ Empirical Knowledge:
scientific knowledge
development and testing of theories/theoretical models
observation and measurement of case-specific issues and phenomena
quantitative and qualitative research
Paradigms and Methods for Nursing Research
Paradigm
From the Greek word meaning “pattern.”
A set of beliefs and practices, shared by communities of researchers, that guide the knowledge development process.
Synonym of worldview, a general perspective on the complexities of the real world, with certain assumptions about reality
Paradigms help hare how a research develops, navigates their work, and interprets their findings.
We have to understand how it relates to the nature of our reality. Our reality depends on our view. For examples, we all have the same definition, feeling, and views of pain. But still, we have different pain thresholds. Another example is that giving birth is different for every mother.
Everything is one reality, but when you’re talking about the social science of feelings of people, its all different realities.
It’s important for us to be aware of paradigm in research because our paradigm, our worldview, affects our position and how we navigate research.
Types of Paradigmatic perspectives: positivism, constructivism, critical theory.
Philosophical Terms
Ontology: is the science or study of “being.”
Ontology addresses two primary questions: (1) What exists or what is real? and (2) Into what categories can existing things be sorted?
Nature of reality
Epistemology: addresses the issue of “truth.”
Epistemology addresses four key questions: (1) What is knowledge? (2) What are the sources of knowledge? (3) What are the ways we come to know something, in contrast to believing, wondering, guessing, or imagining? and (4) What is truth and what role does it play in knowledge?
Nature of truth
Key Differences:
Ontology focuses on the nature of reality—what exists.
Epistemology focuses on the nature of knowledge—how we know what we know.
In practice, a researcher’s ontological beliefs influence their epistemological approach. For example, if a researcher believes that reality is objective (ontology), they might choose quantitative methods to gain knowledge (epistemology). Conversely, if they believe that reality is subjective and socially constructed, they might choose qualitative methods to explore individuals' experiences.
For example:
Ontology: qualitative research studies pain as subjective to the individual because one person’s reality differs from the next. There is no one reality. Different realities an explore experiences of people.
Epistemology: quantitative research has concrete parameters, such as rating pain on a scale of 1-10. This is one reality. More scientific, use tools and numbers.
Researchers should learn their paradigm, how they see the world. But sometimes, you can do a paradigm shift where you need both research types.
* ontology= qualitative
* epistemology= quantitative
Methodology: refers to discipline-specific principles, rules, and procedures that guide the research process.
Methods: are specific means of collecting and analyzing data
Key Differences:
Methodology is the theoretical framework or overall approach that shapes the entire research project.
Methods are the practical tools and techniques used to conduct the research.
Example in Context:
Methodology: A researcher chooses a qualitative methodology because they believe that personal stories will provide deep insights into patient care.
Methods: To collect data, they use interviews and thematic analysis (specific methods) to explore those personal stories.
Context - refers to the personal, social, and political environment in which a phenomenon of interest occurs.
The context of research studies can include physical settings, such as the hospital or home, or less concrete “environments,” such as the context that cultural understandings bring to an experience.
Aim of inquiry - refers to the goals or specific objectives of the research.
Key paradigms for nursing research
Positivist | Constructivist |
|
|
|
|
|
|
|
|
Post-positivism emerged in response to the realization that such objectivity is usually not possible and our observations cannot always be relied upon because they are subject to error and human bias—we all have different values, cultures, and life experiences and, thus, generate different interpretations.
Critical Realism is the blend of positivism and constructivism- offers middle ground that the world is not unknowable chaos (constructivism) or universal order (positivism). Social entities exist in dependently of human understanding. For example, discrimination and power imbalances exist regard less of whether humans recognize their influence.
Post-Positivism: Focuses on approximating objective reality, recognizes that knowledge is fallible, and aims for more accurate understandings of the world through empirical research.
Critical Theory: Focuses on power relations and inequality, aims to uncover social injustices, and advocates for research that leads to transformative social change.
Research Methods
The techniques used to structure a study and to gather, analyze, and interpret information
Quantitative research: most closely allied with the positivist tradition
Qualitative research: associated with the constructivist tradition
Positivists sometimes undertake qualitative studies, and constructivist researchers sometimes collect quantitative information.
Two Main Nursing Research Methods
Research methods are the techniques, procedures, and processes used by researchers to organize a study so that it provides answers to the research question.
Quantitative research: A formal, objective, systematic process in which numeric data are used.
to see cause and effect relationship (like levels of social support (cause) leading to high blood pressure (effect)
Qualitative research: A systematic approach used to describe and promote understanding of human experiences such as pain
discover and understand the meaning of an experience or process
when you use both, its called mixed methods.
Quantitative Research
Formal, objective, systematic process using:
measurement
hypothesis testing
data analysis
Traditional approaches such as experiments, questionnaires, surveys
A researcher would choose to conduct a quantitative research study if the question to be answered concerned testing for the presence of specific relationships, assessing for group differences, clarifying cause-and-effect interactions, or explaining how effective a nursing intervention was.
Goal is to test the relationship between two variables, to test the hypothesis
Objective and separate from the researcher. This means that as a researcher, you have no power to change anything; and you take what you can get. For example, if someone says their pain is an 8, it is an 8 and you cannot change it.
Quantitative Research Process
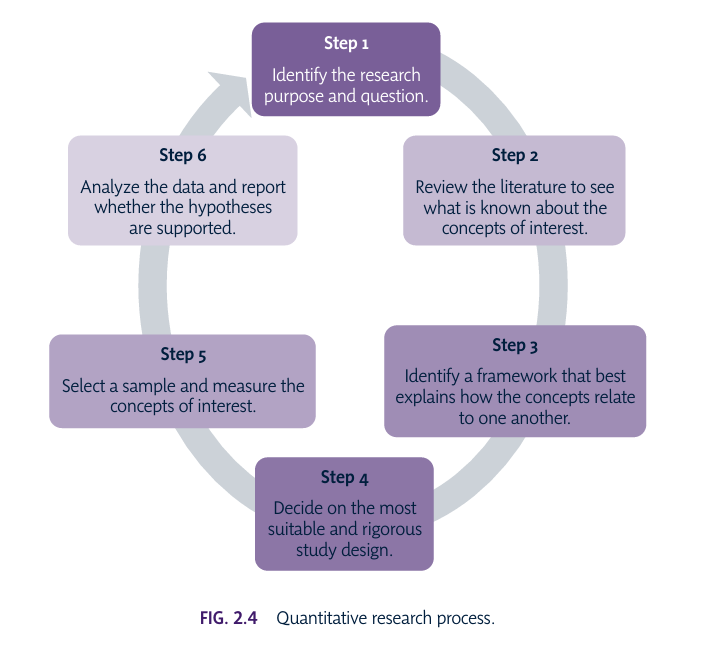
An important part of the quantitative research process is to decide which design is most appropriate for answering the research question. The numerous choices include descriptive, correlational, longitudinal, quasi-experimental, and experimental designs.
systematic
methodology emphasizes control of the research process
the environment in which the study is conducted, and how each variable is measured.
restricted to a preselected set of responses. (pg 31)
Study Example:
Topic: Evaluating the effect of exercise on reducing blood pressure in elderly patients with hypertension.
Step 1: Identify the Research Problem and Question
Research Problem: Hypertension is common among elderly patients, and non-pharmacological interventions such as exercise may help lower blood pressure.
Research Question: "Does a daily 30-minute walking program reduce blood pressure in elderly hypertensive patients?"
Hypothesis: Elderly patients who participate in a daily 30-minute walking program will have a lower blood pressure compared to those who do not exercise.
Step 2: Review of Literature
Action: Review existing research on exercise interventions and their effects on blood pressure, focusing on elderly populations.
Finding: Studies show moderate exercise can reduce blood pressure, but limited research focuses on elderly hypertensive patients in long-term care settings.
Step 3: Identify the Framework
Framework: The Health Belief Model (HBM) can be used to understand how patients' beliefs about the benefits of exercise influence their participation in the walking program. The framework suggests that individuals are more likely to engage in health-promoting behaviors (like exercise) if they believe it will reduce a health risk (like high blood pressure).
Concepts:
Perceived Benefits: Belief that exercise lowers blood pressure.
Perceived Barriers: Difficulty in maintaining exercise routines.
Self-Efficacy: Confidence in the ability to walk daily.
Step 4: Decide on the Study Design
Design: A randomized controlled trial (RCT) is the most rigorous design to test the hypothesis. Randomly assign participants to either an intervention group (daily 30-minute walking program) or a control group (no walking program).
Rigorous Design: Use randomization to reduce bias, ensure both groups are similar at baseline, and measure blood pressure pre- and post-intervention for accuracy.
Step 5: Select a Sample and Measure the Concepts
Sample: Select 60 elderly hypertensive patients from a long-term care facility. Randomly assign 30 to the walking group and 30 to the control group.
Measurement:
Independent variable: Participation in the walking program (yes/no).
Dependent variable: Blood pressure (measured using a standard sphygmomanometer).
Data Collection: Measure baseline blood pressure for both groups at the start of the study. After the 8-week walking program, measure blood pressure again to assess changes.
Step 6: Analyze the Data and Report Findings
Data Analysis: Use descriptive statistics (mean, standard deviation) to summarize blood pressure data for both groups. Perform a t-test to compare the mean changes in blood pressure between the walking group and the control group.
Example Results:
The walking group shows an average decrease in systolic blood pressure of 10 mmHg, while the control group shows no significant change.
The t-test shows a p-value < 0.05, indicating that the difference is statistically significant.
Conclusion: The hypothesis is supported—regular walking significantly reduced blood pressure in elderly hypertensive patients. This suggests that walking programs should be recommended as part of hypertension management for elderly patients.
Summary:
This simple quantitative study uses a randomized controlled trial to test the effect of daily exercise on blood pressure in elderly patients, following the six steps you've outlined, from identifying the problem to analyzing the results and confirming the hypothesis.
Qualitative Research
Evaluate subjective life experiences and give meaning to them
Focuses on understanding phenomena from an individual’s perspective
Approaches: observation, in-depth interviews, case studies, narrative analyses
A researcher would choose to conduct a qualitative research study if the question to be answered concerns the illumination and understanding of human experience, such as ill ness, loss, or life change.
Goal is to understand life experiences and generate the hypothesis
For example, if you ask how much pain the person is in, and they answer. You can share your own experience. You can change or influence the data of the study.
Qualitative Research Process
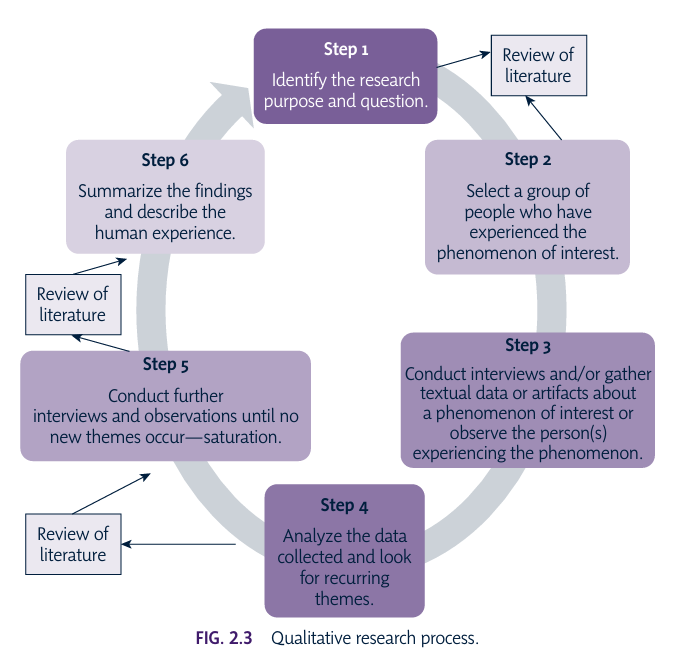
Generally conducted in natural settings.
Data are usually words and/or images rather than numbers.
Sample sizes are often relatively small when compared to quantitative research because the goal is to study a phenomenon in depth with people who can speak knowledgeably about an experience.
Thus, data from qualitative studies help nurses understand experiences or phenomena that affect patients, and this information in turn leads to improved care and stimulates further research. (pg 30)
Here’s a simple example of a qualitative study in nursing research, broken down into the six steps commonly used in the research process:
Study Example:
Topic: Exploring the experiences of cancer patients during chemotherapy.
Step 1: Identify the Research Problem
Purpose: Understand the emotional and psychological experiences of cancer patients during chemotherapy.
Research Question: "What are the lived experiences of cancer patients undergoing chemotherapy treatment?"
Step 2: Review of Literature
Action: Conduct a literature review to examine existing research on cancer patients' experiences, focusing on gaps related to the emotional and psychological aspects of chemotherapy.
Finding: Previous studies focus mostly on physical symptoms and side effects, but there is a lack of in-depth research on patients’ emotional and psychological journeys.
Step 3: Design the Study
Methodology: Use a qualitative phenomenological approach to capture the lived experiences of patients.
Sample: Purposively select 10 patients who are currently undergoing chemotherapy.
Data Collection Method: Use semi-structured interviews with open-ended questions to allow participants to share their personal stories in their own words.
Ethics: Obtain informed consent, ensuring patients are aware of the study's purpose, their voluntary participation, and confidentiality of their responses.
Step 4: Collect the Data
Action: Conduct in-depth interviews with each of the 10 participants. Example questions include:
"Can you describe how you feel emotionally during your chemotherapy sessions?"
"What has been the most challenging part of your chemotherapy experience?"
"How has this experience impacted your relationships and daily life?"
Recording: Record the interviews with participants' consent, transcribing them verbatim for analysis.
Step 5: Analyze the Data
Thematic Analysis: Read through the interview transcripts and identify recurring themes or patterns in the patients' experiences.
Example Themes:
Emotional isolation: Many patients report feeling emotionally isolated during treatment, even when surrounded by loved ones.
Fear of the unknown: Patients express fear and anxiety about the effectiveness of treatment and the future.
Coping strategies: Some patients describe using mindfulness or support groups to cope with the emotional toll of chemotherapy.
Coding: Assign codes to pieces of text that relate to these themes, and organize the data under each theme for further analysis.
Step 6: Interpret and Report Findings
Interpretation: Reflect on how the themes provide a deeper understanding of the emotional and psychological challenges faced by chemotherapy patients. Discuss how these findings can help healthcare providers offer better emotional support during treatment.
Report: Write up the results in a research paper, presenting the themes with supporting quotes from participants, and suggest implications for nursing practice, such as incorporating emotional support services into cancer care programs.
Example Conclusion:
The study highlights the emotional burden of chemotherapy, emphasizing the need for healthcare providers to offer more comprehensive emotional and psychological support. By understanding patients' lived experiences, nurses can improve patient-centered care, providing not only physical but also emotional comfort during treatment.
This simple qualitative study follows the six steps and results in meaningful insights into patients' experiences, which can directly inform practice in nursing care.
Quantitative and Qualitative Research
Quantitative | Qualitative |
Orderly procedures | Dynamic design |
Systematic/prespecified plan | Holistic |
Control over context | Context-bound |
Formal measurement | Humans as instruments |
Empirical evidence | Qualitative information |
Seeks generalizations | Seeks patterns |
*Epistemology | *Oncology |
Deductive | Inductive |
Positivist | Constructivist |
Ex “what is the prevalence of drug abuse in Toronto?” | Ex “which emotions are associated with the drug use of Toronto?” |
test the hypothesis | generate the hypothesis |
conceptual framework | theoretical framework |
Approaches to Science
Inductive reasoning: Start with details of experience and move to a general picture and is used by qualitative researchers.
“figuring out what is there”
qualitative- “induce” or inject the quality of the study
move from small (details of experience) to large (general experience) - imagine the shape of the letter “i” it goes from small dot to big body
Develop a pattern from individual cases. For example: research interviews several cancer in pain and each share what they face. The researcher sees recurring themes like fatigue and tiredness. He concludes that cancer patients in pain feel fatigue.
Deductive reasoning: Start with a general picture and move to a specific direction; uses two or more concepts. This approach is followed by quantitative researchers.
“what is there”
quantitative- “deduce” how much (quantity)
In deductive reasoning, the researcher measures concepts that, when combined, enable the researcher to suggest relationships between the concepts.
nurses form the bigger picture and move in a specific direction. For example: they start with a hypothesis that patients having immunotherapy, the patient experiences anxiety. He takes data from two groups, one receiving immunotherapy and the other not'; he compares the data and sees if the hypothesis is true or not.
CASE STUDY
Currently, the law states that a woman must see a physician in person before she can use mifepristone (the abortion pill RU 486) to induce an abortion. The law prohibits using a video conference with the physician and the medication being administered by a nonphysician. Legislators are seeking information on which they can base their decisions.
Variable
The property that is being studied
Something that changes or varies:
Height
Weight
Religion
Ventilation
Health
Illness
Researchers often conduct studies to understand how changes in one variable relate to changes in another variable (e.g., sex and mental health).
Physical activity (independent variable) and blood pressure (dependent variable). We manipulate the independent to know the dependent.
Concept
Concept is an image or symbolic representation of an abstract idea (e.g., pain, knowledge, God).
Concepts are the major components of theory and convey the abstract ideas within a theory.
conveys abstract ideas
Theory
Theory is a set of interrelated concepts that serve the purpose of explaining or predicting phenomena.
A blueprint or a written or diagrammatic depiction of both the concepts that compose a theory and how they are related.
Theory guides practice and research; practice enables testing of theory and generates questions for research; and research contributes to theory building.
Hypothesis
A best guess or prediction about what a researcher expects to find with regard to the relationship between two or more variables.
A variable is: a defined concept; a property that takes on different values (ie gender, height)
We test it to either support it or refute it.
Conceptual Frameworks
Frameworks provide a general orientation to understanding a phenomenon of interest and identify what factors are most significant as we examine various aspects of health.
A conceptual framework is a structure of concepts, theories, or both that is used to construct a map for the study. It presents a theory that explains why the phenomenon being studied exists. Generally, a conceptual framework is constructed from a review of the literature or is developed as part of a qualitative research project (Imenda, 2014).
A conceptual framework is like a roadmap for your research. It shows how different ideas or concepts in your study are related to each other. It helps you organize and understand the relationships between the key factors you're investigating.
Think of it like this: if you're trying to understand why some people are healthier than others, your concepts might be things like diet, exercise, stress levels, and access to healthcare. A conceptual framework would show how you think these things interact. For example, maybe you believe that diet and exercise directly affect health, while stress and access to healthcare also influence health, but in a more indirect way.
Model of Conceptual Foundation
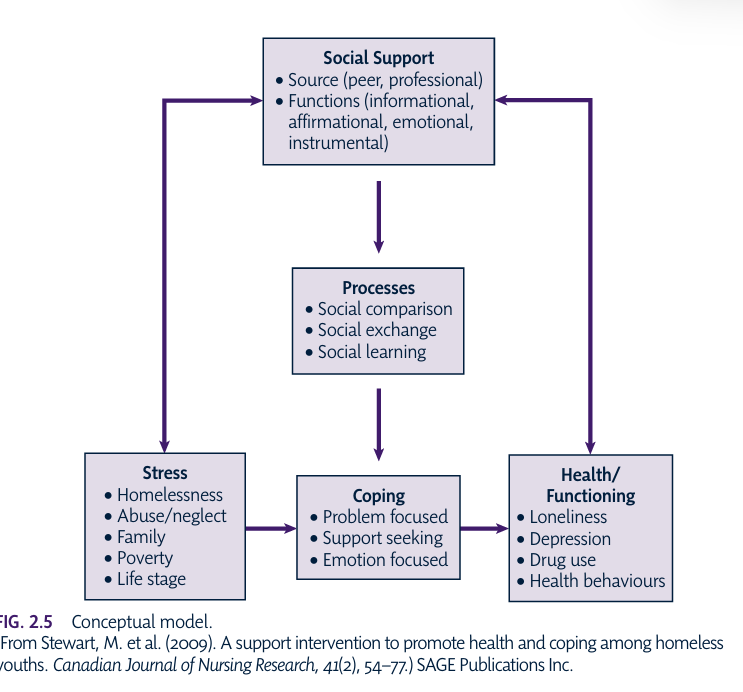
The Conceptual definition goes beyond the general meaning found in the dictionary; the concept is defined as it is rooted in the theoretical literature.
The Operational definition specifies how the concept will be measured—that is, what instruments will be used to capture the features of the variable.
Theoretical Frameworks
Frameworks provide a general orientation to understanding a phenomenon of interest and identify what factors are most significant as we examine various aspects of health.
A theoretical framework may also be defined as a structure of concepts, theories, or both that is used to construct a map for the study.
It is based on a philosophical or theorized belief or understanding of why the phenomenon under study exists.
Function of a Framework
Beginning with the research question, the researcher is inclined to approach a research problem from the perspective of inductive or deductive reasoning. Qualitative researchers, who pursue an inductive reasoning approach, generally do not present a framework before beginning the discussion of methods. This is not to say that the literature will not be reviewed before the methods are introduced. Qualitative researchers may use a conceptual or theoretical framework to inform or sensitize them to existing thinking and theorizing about their topic (Bowen, 2006) but avoid using a framework to structure their analysis so that they are able to see freely what their data contain.
Conversely, researchers who use deductive rea soning must choose between a conceptual and a theoretical framework. In the theory literature, these terms are used interchangeably (Chinn & Kramer, 2015), although, in the case presented in the Critical Thinking Decision Path, each term is distinguished from the other on the basis of whether the researcher is creating the structure or whether the structure has already been created by someone else. In general, each of these terms refers to a structure that provides guidance for research by assisting the researcher in determining study variables and operational definitions. In other words, conceptual and then operational definitions will emerge from the framework. (pg 34)
Clarifies concepts
Identifies and states underlying assumptions of a study
Specifies relationship among and between concepts
A conceptual or theoretical model is a visual symbolic representation of the concepts in a framework.
Research Question Example
What is the relationship between the first occurrence of ambulation in patients after open heart surgery and the length of their hospital stay?
Definitions of “Hospital Stay”
Conceptual: Time during which a person is a registered patient at a hospital
Operational: Sum of days as a registered patient, beginning with admission day and concluding with dismissal day
Definitions of “Ambulation”
Conceptual: To walk from place to place, move about
Operational: Taking four steps without assistance
Evaluating a Framework
Is the framework clearly identified, consistent with a nursing perspective and appropriate for the topic?
Are the concepts and variables clearly and appropriately defined?
Did the study present sufficient literature to support the selected concepts and hypothesis?
Is there a logical, consistent, link between the framework, the concepts being studied, and the methods of measurement?
Are the study findings examined in relation to the framework?
Questions from chapter 2(textbook) & Summary of Key Points:
Nurses inform their practice through various ways of knowing. Which of the following is NOT true about how nurses use forms of knowledge in practice?
a. Theoretical knowing is relevant for practice.
b. Empirical knowing is acquired through the scientific process.
c. Personal knowing is based on opinion rather than fact.
d. Ethical knowing depends on an understanding of what is good.
Answer: C
Rationale: Personal knowing involves an existential awareness of self and others in relationship, which goes beyond the development of opinions.
Which of the following statements about research methods is true?
a. Qualitative research is not systematic.
b. Quantitative research eliminates bias.
c. Quantitative research always produces better evidence.
d. Qualitative research is more appropriate than quantitative research for questions about the meaning of an experience.
Answer: D
Rationale: A researcher chooses between qualitative and quantitative method, based on the question the researcher is asking. If a researcher wishes to discover and under stand the meaning of an experience, a qualitative approach would be appropriate.
Critical social theory influences nursing because it:
a. Shows nurses how power imbalances influence health.
b. Focuses on women at the expense of men.
c. Makes nurses view things negatively.
d. Brings theories into nursing research that are interesting but not directly relevant to nursing practice.
Answer: A
Rationale: Critical social theory emphasizes that reality and our understanding of reality are constructed by people with the most power in a particular time and place.
The scientific approaches used to generate nursing knowledge reflect both inductive and deductive reasoning.
The interaction among theory, practice, and research is central to knowledge development in the discipline of nursing.
Conceptual and theoretical frameworks can be created by the researcher as a result of the study findings or found in the existing literature and used to support the study.
The use of a framework for research is important as a guide to systematically identify concepts and, for quantitative research, study variables.
Conceptual and operational definitions are critical in the evolution of a study, regardless of whether they are explicitly stated in a research report.
In developing or selecting a framework for research, knowledge may be acquired from other disciplines or directly from nursing. In either case, that knowledge is used to answer specific nursing questions.
When you critique a framework for research, examine the logical, consistent link between the framework, the concepts for study, and the methods of data collection
Class Questions:
A set of interrelated concepts that provide a systematic view of a phenomenon is:
A. theory
B. Construct
C. Operational Definition
D. Model
Answer: A. theory
What is the first question to ask when critiquing the theoretical framework of a research study?
A. Is the framework for research clearly identified?
B. Is the framework consistent with nursing perspective?
C. Is the framework appropriate to guide research on the subject of interest?
D. Are the concepts and variables clearly and appropriately defined?
Answer: A. Is the framework for research clearly identified?