Reproductive System
REPRODUCTIVE SYSTEM
designed to facilitate the process of human sexual reproduction
the reproductive system is a collection of internal and external organs — in both males and females — that work together for the purpose of procreating
due to its vital role in the survival of the species, many scientists feel that the reproductive system is among the most important systems in the entire body
of the body’s major systems, the reproductive system is the one that differs most between sexes, and the only system that does not function until puberty
the male reproductive system is responsible for delivering sperm to the female reproductive system
Gametogenesis
the production of sex cells or gametes and the process of fertilization that eventually leads to the development of human embryo
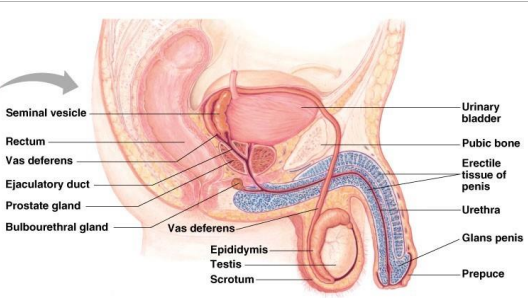
MALE REPRODUCTIVE SYSTEM
the male reproductive system performs the following functions:
secretion of the male sex hormones
production of sperm cells
transfer of sperm cells
the male gonads are the testes (singular: testis) hanging in the scrotum
sperm production requires a slightly lower temperature than the human body that is why the scrotum hangs loosely outside the body cavity
however, when the testis fails to descend, it leads to sterility because of the inhibiting effect of normal body temperature on sperm development
in males, the reproductive organs include the penis, the testes, a number of storage and transport ducts, and some supporting structures
the two oval-shaped testes (also called testicles) lie outside the body in a pouch of skin called the scrotum, where they can maintain the optimum temperature for sperm production – approximately 5° F, lower than body temperature
testes are oval-shaped glands responsible for the manufacture of sperm and the sex hormone testosterone
from each testis, sperm pass into a coiled tube – the epididymis – for the final stages of maturation
INSIDE THE SCROTUM
the scrotum contains two testes (testicles) where sperm are manufactured within tubes called seminiferous tubules, and the two epididymises where sperm are stored
unlike female egg maturation, which occurs in cycles and ceases at menopause, sperm production is continuous, reducing gradually with age
each epididymis is a tube about 20 feet long, which is tightly coiled and bunched into a length of just 2 inches
SPERMATOGENESIS
the process of producing sperm cells
takes place in coiled tubules called seminiferous tubules in the testes
MAKING SPERM
each testis is a mass of more than 800 tightly looped and folded vessels known as seminiferous tubules
inside each tubule, sperm begin as blob-like cells called spermatogonia lining the inner wall
these pass through a larger stage, as primary spermatocytes, then become smaller as secondary spermatocytes, and begin to develop tails as spermatids
as all of this happens, they move steadily towards the middle of the tubule
the spermatids finally develop into ripe sperm with long tails
thousands of sperm are produced every second, each taking about two months to mature
DIFFERENCE OF SEMEN AND SPERM
semen, also known as seminal fluid, is much more than just sperm
sperm is only about 5 to 10% of any given male single ejaculation and the rest is fructose (aka sugar), fatty acids, and proteins to nourish the sperm during their journey
SPERM COUNT
a man will produce roughly 525 billion sperm during his whole lifetime and close to 1 billion per month
there are around 200 to 500 million sperm in an average in a single male human ejaculation
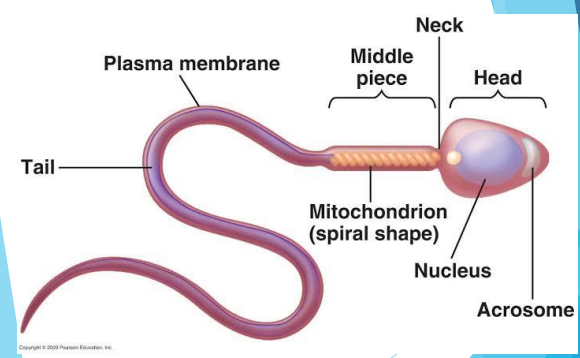
SPERM CELL
a sperm is about 1/500 inch long, but most of this is a tail
the sperm head is only 1/5000 inch, about the same size as a red blood cell
sperm develop in the testes and consist of a head, a midpiece, and a tail
the head contains the nucleus with densely coiled chromatin fibers (chromosomes), with a front section – the acrosome that contains enzymes for penetrating the female egg
the midpiece has a central filamentous core with many mitochondria spiraled around it, to give it energy to move the tail which propels it forward
PARTS OF THE MALE REPRODUCTIVE SYSTEM
Testis (plural testes)
produces sperm cells
Scrotum
sac of skin that holds the testis
Seminiferous Tubules
highly coiled tubules where the sperm are formed
Epididymis
where the sperm are temporarily stored
Penis
deposits sperms into the vagina during mating
Vas deferens (tube)
carries sperm from testes to urethra
Urethra
carries sperm and urine out of the body
Glands
provide liquid in which sperm can swim
Seminal vesicle – secretes a fluid that makes up most of the components of the semen
Prostate gland – secretes a slightly alkaline milky fluid that is discharged as part of the semen
Bulbourethral gland (Cowper’s gland) – secretes a thick and clear mucus that lubricates and neutralizes any trace of acidic urine in the urethra
Organ / Component | Primary Functions |
|---|---|
Testes | produce sperm and hormones |
Accessory Organs | |
Epididymis | acts as site of sperm maturation |
Ductus Deferens (Sperm Duct) | conducts sperm between epididymis and prostate gland |
Seminal Vesicles | secrete fluid that makes up much of the volume of semen |
Prostate Gland | secretes fluid and enzyme |
Urethra | conducts semen to exterior |
External Genitalia | |
Penis | contains erectile tissue; deposits sperm in vagina of female; produces pleasurable sensations during sexual activities |
Scrotum | surrounds the testes and controls their temperature |
FEMALE REPRODUCTIVE SYSTEM
the female reproductive system has the following functions:
produces female sex cells
receives sperm cells from the male
nurtures the development of and provides nourishment for the new individual
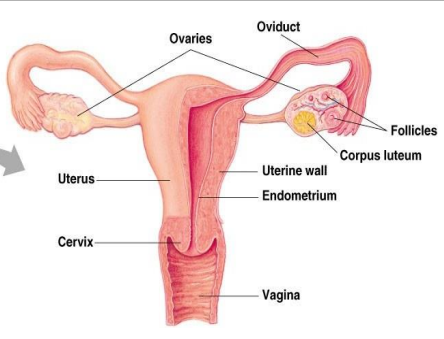
the female reproductive system includes external and internal genitalia
the vulva and its structures form the external genitalia
the internal genitalia includes a three-part system of ducts: the uterine tubes, the uterus, and the vagina
this system of ducts connects to the ovaries, the primary reproductive organs
the ovaries produce egg cells and release them for fertilization
fertilized egg develop inside the uterus
unlike the male, the female reproductive organs are located entirely inside the body
from puberty, their function is to ripen and release an egg at regular intervals, and, if the egg is fertilized, to protect and nourish the embryo and fetus
no eggs are manufactured after birth – a female is born with a full set
REPRODUCTIVE TRACT
the female reproductive glands (ovaries) are located within the abdomen
this release occurs roughly once a month as part of the menstrual cycle
the ripe egg travels along the fallopian tube to the uterus, the muscular sac in which it develops into an embryo and then fetus
EGG CELLS FROM THE OVARIES MOVE THROUGH THE UTERINE TUBES
the uterine tubes (also called fallopian tubes or oviducts) connect the ovaries to the uterus
the walls of each tube have an external serous layer, a middle muscular layer, and an internal mucous layer that is continuous with the inner lining of the uterus
each uterine tube can be divided into three parts:
infundibulum
isthmus connects with the uterus
a dilated portion, the ampulla, curves over the ovary
egg fertilization usually occurs in the ampulla, the eggs then travel through the isthmus to the uterus
THE VAGINA: A TUNNEL WITH THREE CORE FUNCTIONS
the vagina extends down from the cervix, the lower part of the uterus, to the vestibule, which is part of the vulva and the external genitalia
it sits behind the bladder and in front of the rectum
an inner mucous membrane lines the smooth muscle walls of the vagina
this lining, like the inner layer of the uterine tubes, is continuous with the mucous lining of the uterus
the vagina has three core functions:
carries menstrual flow outside the body
receives the male penis during sexual intercourse
serves as a birth canal during labor
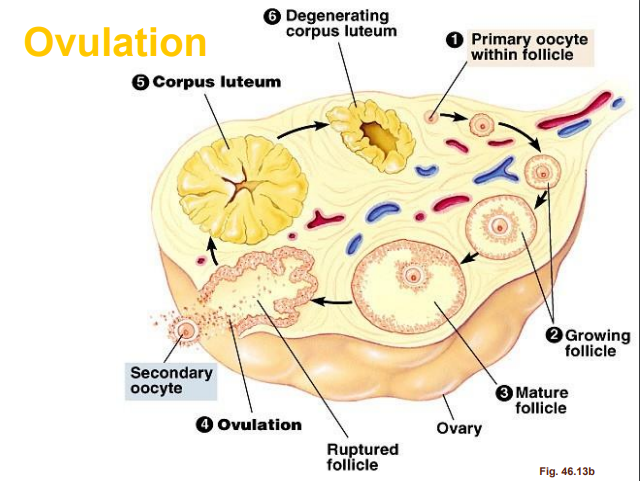
OVULATION
an ovary contains thousands of immature egg cells
during each menstrual cycle, follicle-stimulating hormone (FSH) causes one egg to begin development; this takes place inside a primary follicle
the follicle enlarges as its cells proliferate and begins to fill with fluid, becoming a secondary follicle that moves to the ovary’s surface
it also increases its production of the hormone estrogen
a surge of luteinizing hormone (LH) causes the follicle to rupture and release the ripe egg – this is ovulation
the lining of the empty follicle thickens into a corpus luteum – a temporary source of hormones
PARTS OF THE FEMALE REPRODUCTIVE SYSTEM
Ovary
produces egg cells
slightly flattened bean-shaped bodies, each about two to five cm in length and two to three cm in width
Follicles
from these the female sex cells, egg cells, or ova develops
Oviduct
fallopian tube or uterine tube
site of egg fertilization
passageway through which the ovum passes from the ovary to the uterine cavity
Uterus
serves as the site of egg implantation
where the fertilized egg develops
Vagina
receives the penis of the male during mating
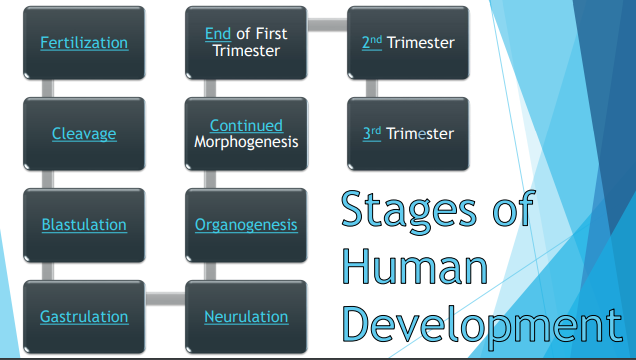
FERTILIZATION: A SPERM AND AN EGG FORM A ZYGOTE
union of two kinds of gametes resulting to the formation of a fertilized egg called zygote
the sperm and the egg are called gametes
they each contain half of the genetic information necessary for reproduction
when a sperm cell penetrates and fertilizes an egg, that genetic information combines
the 23 chromosomes from the sperm pair with 23 chromosomes in the egg, forming a 46-chromosome cell called a zygote
the zygote starts to divide and multiply
as it travels toward the uterus it divides to become a blastocyst, which will burrow into the uterine wall
EMBRYO
refers to the earliest stage of development of an organism into which the zygote develops through a series of cell divisions
THE ZYGOTE BECOMES AN EMBRYO: DEVELOPMENT PRIOR TO AND DURING IMPLANTATION
the blastocyst attaches to the wall of the uterus and gradually implants itself into the uterine lining
during implantation, its cells differentiate further
at day 15 after conception, the cells that will form the embryo become an embryonic disc, other cells begin to form support structures
the yolk sac, on one side of the disc, will become part of the digestive tract
on the other side, the amnion fills with fluid and will surround the embryo as it develops
other cells groups initiate the placenta and umbilical cord, which will bring in nutrients and eliminate waste
OOGENESIS
formation of egg cells or ova
takes place in numerous round structures called follicles
WHAT HAPPENS WHEN THE EGG IS NOT FERTILIZED?
deterioration of corpus luteum
maturation of a new follicle for the next reproductive cycle of the female
breaking down of the uterus lining which is discharged as menstrual flow
MENSTRUATION
a discharging of blood, secretions, and tissue debris from the uterus that occurs in non-pregnant females
GONAD
primary male and female reproductive organs
MALE | FEMALE | |
|---|---|---|
Gonad | Testes | Ovary |
Gamete | Sperm | Ovum (Egg) |
Hormones | Androgen | Estrogen |
Testosterone | Progesterone |
MALE ANATOMY
MALE REPRODUCTIVE HORMONES
CELLS OF THE TESTES
Leydig (interstitial) cells
synthesize hormones and produce testosterone in the presence of LH
Sertoli cells
synthesize sperm (spermatogenesis)
nurse cell of the testicles that is part of seminiferous tubules
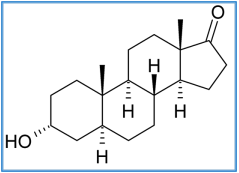
ANDROGEN
male sexual and reproductive function
secondary male characteristics
bone and muscle development and metabolism
released from testes
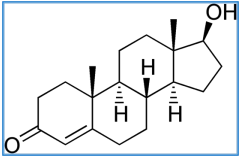
TESTOSTERONE
primary sex hormone and anabolic steroids in male
development of male reproductive tissues (testes and prostate)
released from testes
PRIMARY SEXUAL CHARACTERISTICS
associated with the reproductive system
development of vas deferens, external reproductive structures
stimulate spermatogenesis: sperm production in sertoli cells (lifetime process)
SECONDARY SEX CHARACTERISTICS
not directly related to the reproductive system
develops characteristics at puberty
deepening of voice
facial and pubic hair
muscle growth
increased secretion of body oils (associated with body odor)
MALE REPRODUCTIVE HORMONES
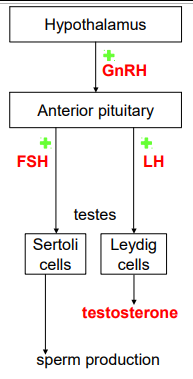
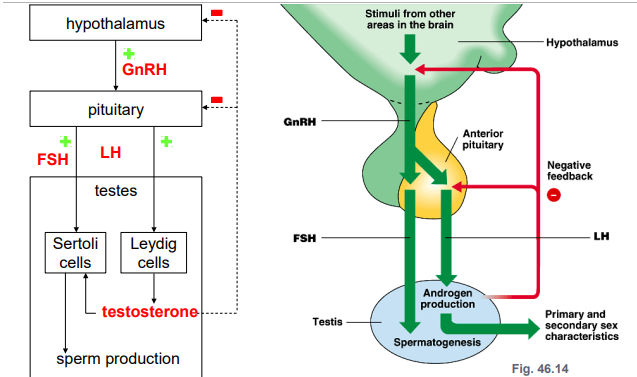
Hypothalamus: Gonadotropin-releasing hormone (GnRH)
Anterior Pituitary: Gonadotropic hormones FSH and LH
Sertoli cells: FSH stimulates spermatogenesis
Leydig cells: LH stimulates hormone secretion
Androgen and Testosterone: affects primary and secondary sexual characteristics
GONADOTROPIC HORMONES
two types:
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
peptide hormones
present in both male and female
plays an important role for reproduction
GONADOTROPINS IN MALES
FSH
act on Sertoli cells to increase spermatogenesis (nontropic)
LH
stimulate Leydig cells to make androgens (tropic)
MALE REPRODUCTIVE HORMONE: NEUROENDOCRINE PATHWAY – NONTROPIC
Location | Hormone |
|---|---|
Hypothalamus | Gonadotropin-releasing hormone (GnRH) |
Anterior Pituitary | Gonadotropins: Follicle-stimulating hormone (FSH) |
Effect: Sertoli cells | Spermatogenesis |
MALE REPRODUCTIVE HORMONE: NEUROENDOCRINE PATHWAY – TROPIC
Location | Hormone |
|---|---|
Hypothalamus | Gonadotropin-releasing hormone (GnRH) |
Anterior Pituitary | Gonadotropins: Luteinizing hormone (LH) |
Testes: Leydig cells | Androgens: Testosterone |
Effect | Primary and secondary sexual characteristics |
MALE REPRODUCTIVE HORMONAL CONTROL
NEGATIVE FEEDBACK
testosterone negatively feedback to the hypothalamus and pituitary to decrease the production of GnRH and LH
FEMALE REPRODUCTIVE HORMONES
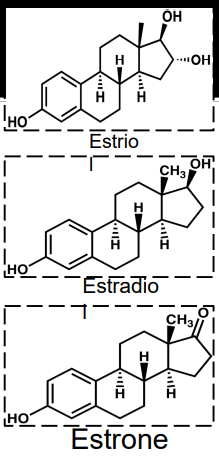
ESTROGEN
female sex hormones
three compounds
Estriol
Estradiol – predominant
Estrone
develops secondary sexual characteristics
breast development
wider hips
fat deposition
OVARY FOLLICLE CELLS
primary oocyte
egg that can be fertilized by sperm
granulosa cells
provide nutrients for primary oocyte
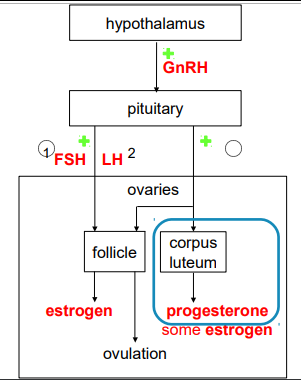
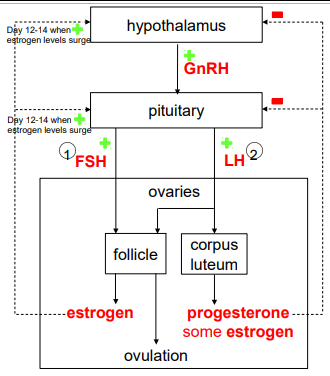
OVARIAN CYCLE REGULATION: NEUROENDOCRINE PATHWAY
Location | Hormone |
|---|---|
Hypothalamus | Gonadotropin-releasing hormone (GnRH) |
Anterior Pituitary | Gonadotropins: Follicle-stimulating hormone (LH) |
Ovaries: Follicle & Corpus Luteum | EstrogenProgesterone |
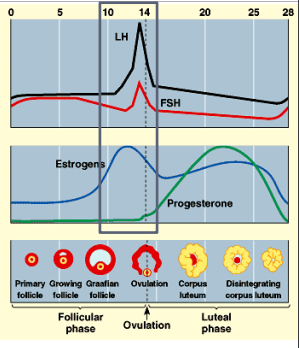
GONADOTROPIN-RELEASING HORMONE (GnRH)
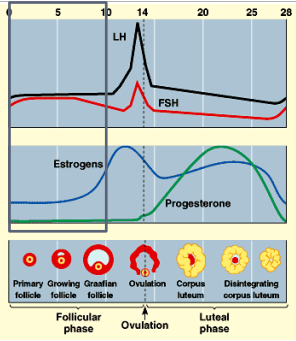
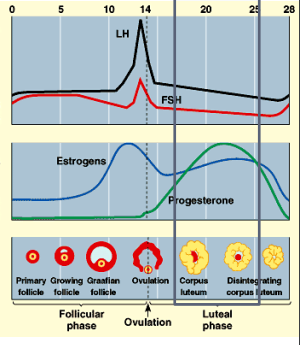
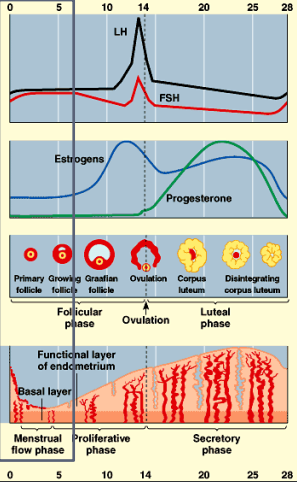
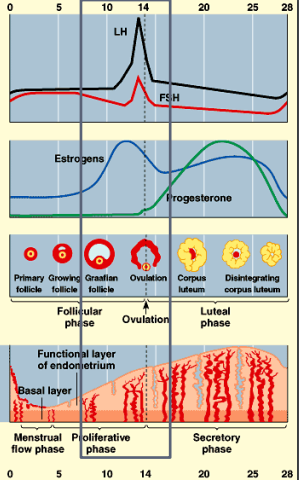
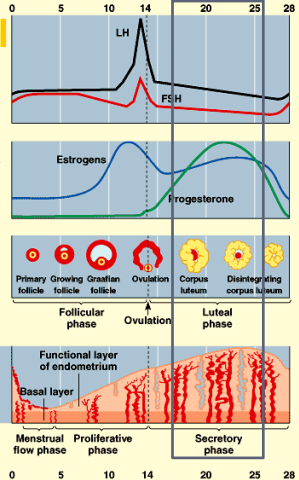
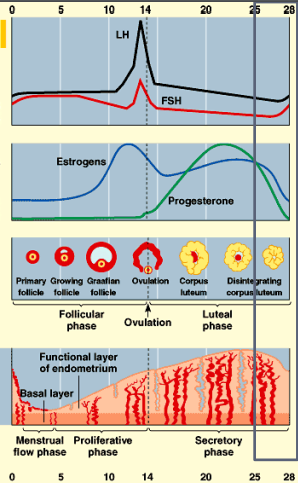
GnRH levels not shown in graph or right but correlates to the rise in LH/FSH levels
released in slow waves during follicular phase
rate of release is increased (peaked) when approaching ovulation
rate decreases greatly during luteal phase
GONADOTROPINS IN FEMALES
FSH
stimulates growth of follicle (maturation) in follicular phase
LH
luteinizes the follicle into the corpus luteum
induces ovulation
matures the corpus luteum in luteal phase
OVARIAN CYCLE
Follicular phase
growth of several follicles but only one matures while others disintegrate
egg in follicle enlarges
coat of follicle thickens
fluid-filled cavity inside follicle develops and bulges
Ovulation
follicle and wall of ovary rupture
egg is released
Luteal phase
follicular tissue develops into corpus luteum
corpus luteum secretes female hormones
OVULATION
FEMALE REPRODUCTIVE HORMONE
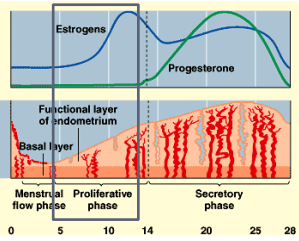
PROGESTERONE
corpus luteum secretes progesterone (and some estrogens)
correlates to thickening of endometrium
in order to accept fertilized egg and enable implantation and growth
if no implantation then corpus luteum disintegrates
progesterone isn’t secreted
decreased progesterone levels leads to:
stop of endometrium growth
endometrium breaks down (menstruation)
MENSTRUAL CYCLE
day 1 = first day of menstruation
menstrual flow phase
sloughing of endometrial lining
menstrual bleeding
Proliferative phase
endometrium regenerates and thickens
Secretory phase
endometrium continues to thicken
becomes more vascularized (blood vessels)
develops glands to secrete fluid rich in glycogen
FOLLICLE
granulosa cells of follicle secretes estrogen
ESTROGEN REGULATION: HIGH LEVELS
high estrogen: positive feedback on LH & FSH by stimulating GnRH
estrogen surge from follicle during day 12-14
LH & FSH surge
results in ovulation
ESTROGEN REGULATION
also responsible for the early thickening of the endometrium in the proliferative phase
ESTROGEN REGULATION: LOW LEVELS
estrogen secreted at low levels during most of the cycle
negative feedback on GnRH, LH, and FSH
ESTROGEN REGULATION
corpus luteum secretes estrogen and progesterone
both act together to negatively feedback on GnRH, LH & FSH
prevents ovulation
DUAL ROLE OF ESTROGEN
low estrogen concentration negative feedback
high estrogen concentration positive feedback
FEMALE REPRODUCTIVE HORMONE CONTROL
OVERVIEW OF FEMALE REPRODUCTIVE CYCLES
HORMONAL CONTROL IN FOLLICULAR PHASE
immature follicles have receptors for FSH but not LH
FSH stimulate follicular growth
granulosa cells of the growing follicles secrete estrogen
low levels of estrogen negatively feedbacks on LH and FSH
HORMONAL CONTROL NEAR OVULATION
estrogen surge
positive feedback on LH and FSH by stimulating GnRH
mature follicle have receptors for LH
LH induces ovulation
estrogen also stimulates thickening of endometrium
HORMONAL CONTROL IN LUTEAL PHASE
LH luteinizes remaining follicular tissue into corpus luteum
corpus luteum secretes estrogen and progesterone
both act together to negatively feedback on GnRH, LH & FSH
corpus luteum disintegrates
sharp decline in estrogen and progesterone
negative feedback removed
secretion of GnRH, LH & FSH begins
disintegration of endometrium
MENOPAUSE
the time in a woman’s life when her period stops
occurs around age 46-54
ovaries lose responsiveness to gonadotropins
decline in estrogen production
cessation of ovulation and menstruation
FEMALE REPRODUCTIVE SYSTEM
comparatively more complicated than male reproductive system
monthly cycle until menopause (~12 to 50 yrs)
one ovum produced per germ cell
FEMALE ANATOMY
HORMONES
chemical messengers of the body
important to maintain homeostasis
THE ROLE OF HORMONES IN FEMALE AND MALE REPRODUCTIVE SYSTEMS
human reproductive cycles are controlled by the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive organs
when the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone or GnRH to the anterior pituitary gland
this causes the release of follicle-stimulating hormones or FSH and luteinizing hormones or LH from the anterior pituitary gland into the blood
the body must reach puberty in order for the adrenal glands to release the hormones that must be present for GnRH to be produced
REGULATION OF REPRODUCTIVE HORMONE SECRETION IN MALES
FSH enters the testes and stimulates the Sertoli cells to begin facilitating spermatogenesis using negative feedback
LH also enters the testes and stimulates the interstitial cells of Leydig to make and release testosterone into the testes and the blood
a negative feedback system occurs in the male with rising levels of testosterone acting on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH
the hormone inhibin stops the release of GnRH and FSH, which will cause spermatogenesis to slow down
FUNCTIONS OF TESTOSTERONE
stimulates spermatogenesis
these secondary sex characteristics:
deepening of the vice
growth of facial, axillary, and pubic hair
beginnings of the sexual urge
REGULATION OF REPRODUCTIVE HORMONE SECRETION IN FEMALES
the follicle-stimulating hormones (FSH) stimulates development of egg cells or ova
follicle cells produce the hormone inhibin which stops FSH production
FUNCTIONS OF ESTROGEN
assists in endometrial regrowth
ovulation
calcium absorption
secondary sexual characteristics of females:
breast development
widening of the hips
shorter period necessary for bone maturation
FUNCTIONS OF PROGESTERONE
assists in endometrial regrowth
inhibition of the release of FSH and LH