Microbiology
22/01/2024-Lecture 01
Infectious Disease
Viruses
Viruses are acellular, They do not fit into any of the 3 domains of life.
It is not clearly understood how they are related to the domains or their members.
Each viral unit as a particle.
Each viral particle consists of a nucleic acid genome wrapped in a protein coat.
The protein coat is referred to as the capsid.
In some viruses this capsid is surrounded by a lipid envelope.
Compared to the structure and organisation of cellular life, the structure and orgganisation of viruses is clearly minimalistic.
Smaller than eukaryotic cells,
Viral structure
Viral capsid- madebup of repeating, identical subunits which self assemble into structures.
Since viruses require host for their replication, they are under constant pressure to have compact genomes.
They have evolved to produce proteins that can self-assemble into structures.
Capsid protein can self assemble on their own or with the help of other proteins into structures.
Capsid protein form different viruses can self-assemble in different ways thereby determining the overall shape the virus.
Based on the capsid shape viruses can be broadly classififed into 3 types; Helical, Icosahedral and Complex.
Bacteria
Fungi
Eukaryotes
Types of Phylum of Fungi
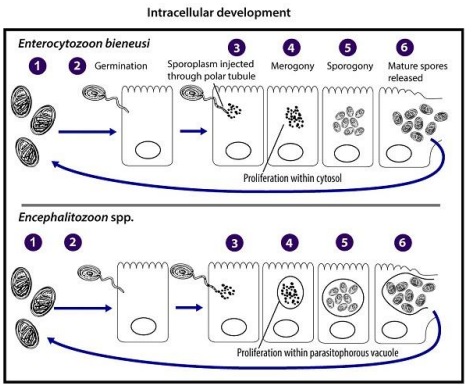
Microsporidia
LAck Mitochondria
Unicellular
Replicate via host cell.
Produce spores for reproduction
Ascomycota
Morphologically diverse, yeast to moulds.
Ascus-sac with 8 spores.
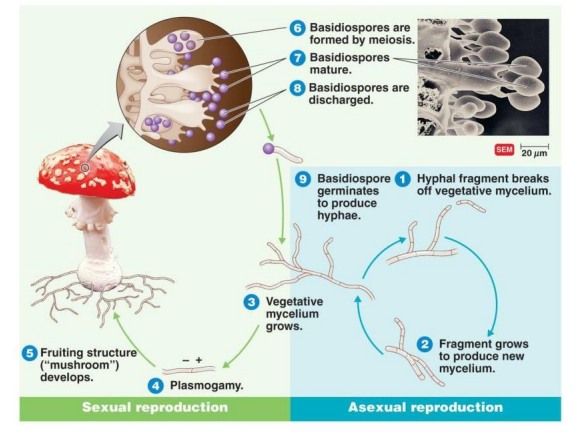
Basidiomycota
Club Shaped end cells- basidia,
Usually 4 spores.
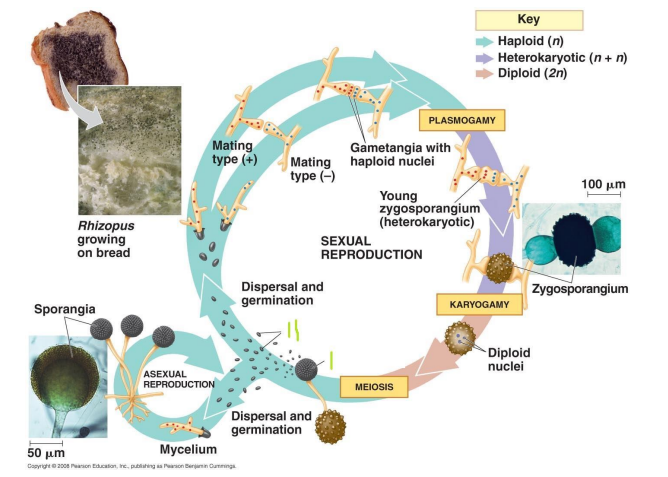
Zygomycota
Sporangium- Ball of wool like appearance.
May be aseptate
Chitosan cell wall.
Fungi are a kingdom in Eukaryota
In between Plantae and animalia/
There is a presence of membrane bound organelles
They are similar to plants have they have a cell wall.
Evolutionary Level
Fungal cells are similar to human cells compared to bacterial cells.
This has implications in therapeutic interventions.
Unicellular
Yeasts
Multicellular
Moulds
Dimorphic Fungi
Existance in both yeast and mould forms.
E.g Candida ALbicans, Is a yeast outside the body and a mould inside the human body.
Terminology
Mycology
Study of Fungi
Mukes
Fungi
Mycoses
Fungal Diseases
Dermato Mycoses
Fungal Diseases of the skin
Moulds
Long Branching filamentous structure (Hyphae)
Sometimes filamentous structures are separated into cell-like units by septa.
Hyphae; Vegetative (mycelium) & Aerial.
Multicellular
Aerial produces spores
Mycelium- root like structures.
Yeasts
Unicellular
Non filamentous
Spherical or Oval
Divide by Budding and Fission.
Dimorphic Fungi
Fungo can be broadly classifies into yeasts and moulds, dependent upon the growth phenotype.
Dimorphic- Some fungi have both the growth forms, a yeast and mould for,.
Many dimorphic fungi are pathogenic.
In most cases, alteration between the two forms is dependent on temperature.
Fungi Characteristics
Fungi are eukaryotic, cellular processes are similar to other eukaryotic organisms.
Similar to plant cells. Fungal cells have a cell wall, but the cell wall is made up of chitin,.
They reproduce via Budding, fission or spores.
Capable of growing at different pH;s.
Most fungi require less nitrogen than bacteria.
They are more resistant to osmotic pressure than bacteria.
Fungi can metabolise complex carbohydrates.
They are chemoheterotrophs.
Derives its energy from chemicals.
Most filamentous fungi require oxygen
Most yeasts are anaerobic.
Fungal Reproduction
Can be sexual and Asexual
In asexual reproduction;
The mycelium produces genetically identical unicellular haploid spores.
In sexual reproduction;
Teo different mycelia mate and produce a diploid zygote.
The diploid zygote then undergoes meiosis producing haploid spores.
Haploid spores germinate into mycelium.
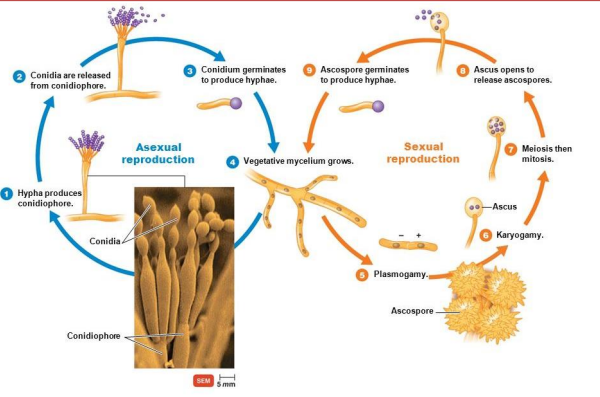
Ascomycota Reproduction
Microsporidia Reproduction
Basidiomycota
Zygomycota
Yeast Reproduction
Microsporidiosis.
CAndidiasis.
ASpergillosis.
Histoplasmosis.
Coccidiodomycosis.
Ergotism.
Parasitology
Parasite - An organism which lives in or on another organism and benefits by deriving nutrients at the other's expense.
Parasitoid- An insect whose larvae live as parasites which eventually kill their hosts.
Obligate Parasaite - Only purpose is to exist in the parasitic relationship.
Many organisms have complex life cycles involving one or more host or hoshts.
Human parasitic infections are a huge problem in tropical regions- but not exclusively.
Definitive Hosts- Final host in which the parasite reaches maturity and undergoes sexual reproduction,
Intermediate Hosts- Host in which the parasite undergoes developmental stages.
Advantages
Disadvantages
Ectoparasites.
Ticks and Mites
Visit the surface of the host to feed.
Some may be the vectors for endoparasitic organisms (Malaria and mosquitous)
They are macroscopic.
Classed as macropatasites.
Pediculosis
Lice
Endo- Parasites
Protozoa
Malaria
Other infectious agents
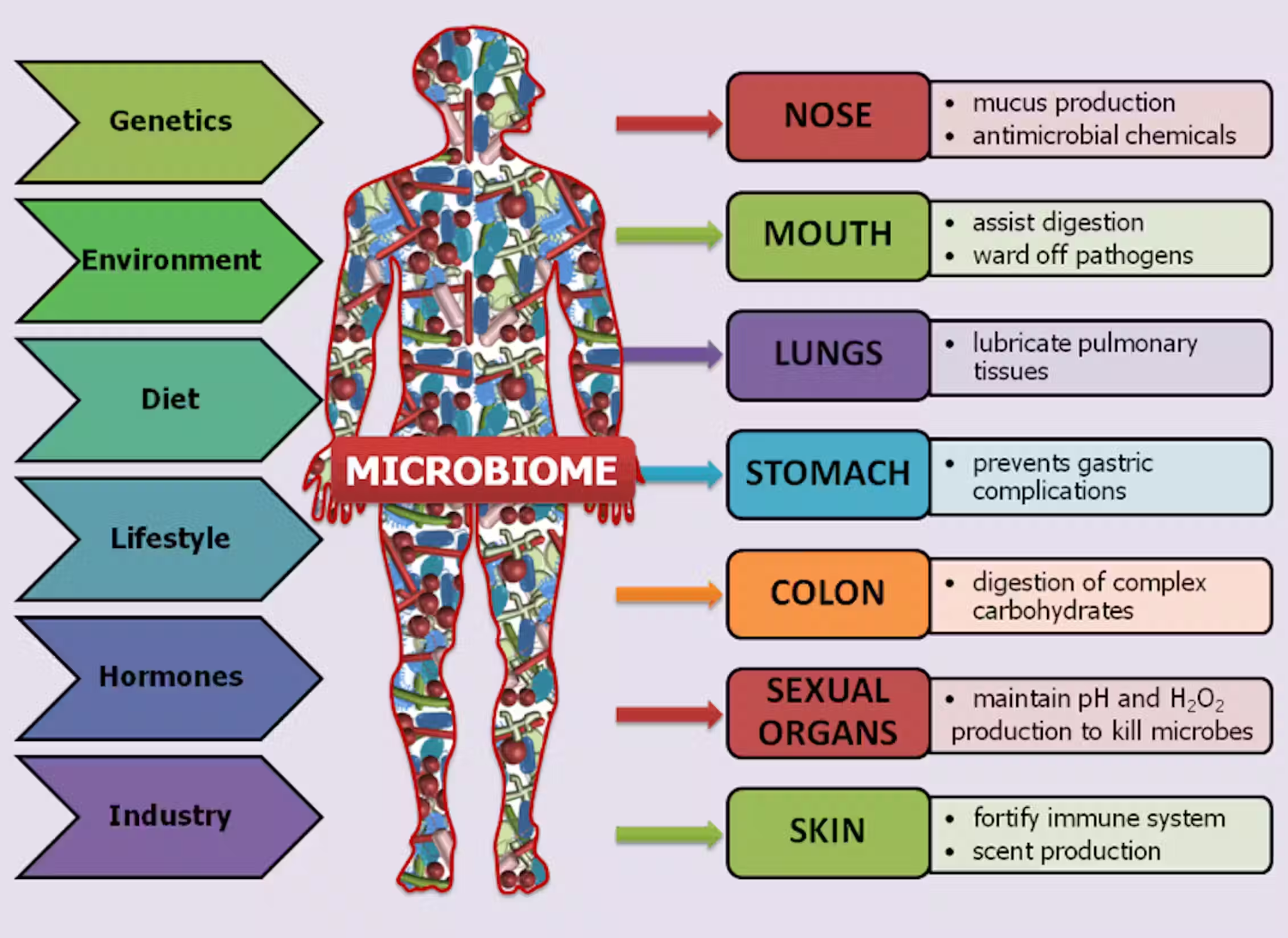
Microbiome
‘Germ Theory’ - Infectious disease is spread by microscopic, living, causative agents.
Environmental sources of microorganisms
Soil
Cooking Meat (or not cooking lol)
Contamination of Water
Cough Droplets.
We are all inhabited by commensal microorganisms and a balance exists between the microorganisms and the epithelium.
This allows for microbial survival and the prevention of induction of inflammation.
Benefits of Commensals
Aids in maturation of immune system
Assist in digestions
Role in toxic degradation.
When there is an imbalance, the microorganisms can cause tissue damage.
The human microbiome
The microbiome works in harmony with various organs in the body and aids in their function.
From newborn, the newborns mouth is sterile and is then inoculated from the first feed onwards from mothers food.
This transmits the microorganisms to colonisation sites.
Acquisition of Oral Microbial flora
The moutb is initalluy hihgly selective for microorganisms.
On Epithelial Surfaces
Only a few oral species colonise,
They are Gram Positive and aerobic.
Mainly streptococci.
Thye are the pioneer species.
Within 2-3 months, gram negative anaerobic bacteria begin to appear.
It is not accidental.
It is a natural acquisition and selection process.
Microorganism Host Relationship
Symbiosis refers to the relationship between different organisms.
Various types of symbiotic relationships exists such as commensalism, mutalism and parasitism.
Commensalism.
Microorganism benefits, host is neither harmed nor helped.
Mutualism or True Symbiosis
Both microorganism and host benefits.
The host is not harmed and derives a clear benefit.
Parasitism
Microroganism benefits but the host is harmed.
COnsequences of a parasitic relationship
Infection!!!!!!!!!!!!!!!!!!!!!!!
Exogenous Infections
Aquatic
Zoonoitc e.g Salmonella
Saprophytic e.g Tetanus
Endogeneous
Infective endocarditis
Microbial symbiosis with human host
Normal microbial flora consists of microorganisms that engage in commensal in mutualistic relationship with us. If it was a parasitic relationship, they would be caustyaive agents of disease.
We are therefore not activelyu harmed by a microbial flora and derive some degree of benefit from many microbial components.
TMany of these organisms can engage in a aprarsitic relationship if given the opportunity.
THe human microbiome
The human microbiome is not a composed homogenouslt in all areas of the host.
Different physiological sotr are primarily colonised by different microbial species.
This is primarily due to different site being chatacterised by different environments that microgransims can specialse to colonise.
Colonisation of the intestine can require different specialisation to colonisation of the skin.
Nosocomial Infection- Infection picked up in a hospital.
The Virome
This is the viral component to the microbiome
A significant amount of our genome is of viral origin,
REtroviruses utilse reverse transcription to produce DNA from RNA.
The Mycobiome
Fungal composition of the microbiome
Composition is fairly well characterisedf but the impact on human health is not as clear,
There is not as much research available as to the mycobiome. #
The microbiome and Human Health
Synthesis of vitamins
Promotion of intestinal angiogenesis .
SCFA production of fermentation of fibre.
Modulation of CNS,
Protection afaint=st pathogens,
Immune system development,
Promotion of fat storage.
Enhances metabolis,
Prevention against autoimmunity..
Innate Immunity
Ef bb fv
Specific & Non-SPecific Immune Systems
Innate- Non-specific, rapid, aspects are inducible
Broad response effective against a range of threats.
Adaptive- Specific, targeted, inducible and capable of adapting to threats, (specificity and memory.
The Innate Immune System
COnsists of
Physcial Barriers
Antimicrobial peptides and enzymes
The complement system
Non-SPecific Cellls
Inflammation
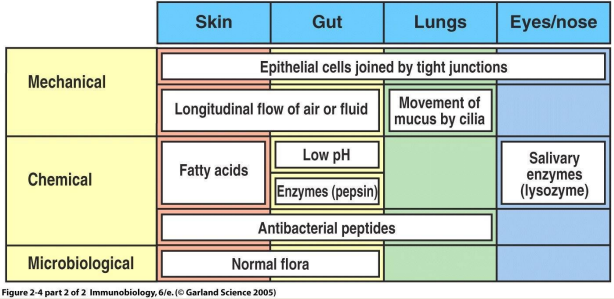
Exterior Defences
They are an effective barrier, very few infectious agents can penetrate intact skin.
Mechanical Barriers- Skin, cillia, hair, earwax, sweat.
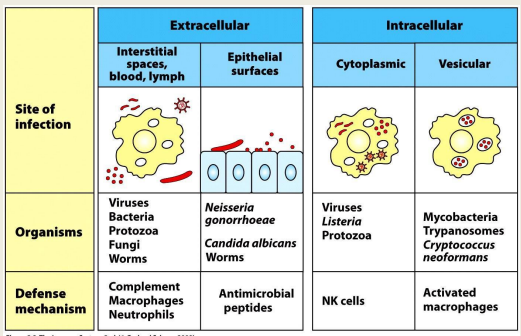
Pathogens gain access through the mucosal epithelia such as gastrointestinal,urogenital, nasipharynx and lung.
Physiological barriers- coughing, sneezing, urination, diarrhoea.
SOme pathogens infect the body by entering the blood directly.
Immune response- Eliminate infectious agents and minimise the damage they cause.
Physica Barriers
Pathogens can enter the body at different points, each of these points have their own physical barriers, these barriers must be breached in order to initiate an infection.
Defence depends on, the breaching of these physical barriers.
The innate defence are dependent on where the pathogen resides.
Epithelial Barriers
Tight junctions are the basis of the epithelial barrier.
Epithelium provides a location for other immune factors.
Enzymes such as lysozyme
Cryptdins and a-defensins
B-defensins,
Acidic stomach pH,
Surfactants.
Mucus and Villi
Normal Gut flora.
First Line of Defence
We are born with non-specific defences that do not require prior exposure to a harmful substance or threatnenitn cell, thus called innate immunity,
Such as,
Granulocytes
Mast Cells,
Monocytes.
Dendritic Cells, Macrophages.
NAtural Killer Cells..
Physical Barriers- EPithelia
Epithelia comprise both the skin and the linings of the bodys passages.
Including the Respiratory Tract, Gastrointestinal Tract, Urogenitaltracts.
Epithelial Cells are held together by tight junctions, multiprotein junction complexes form a seal to prevent leakage of fluids and entry of pathogens,
A pathogen must bind to, or cross an epithelia in order to cause an infection.
Immune System cells derive from haematopoietic stem cells.
Physical Barriers- EPidermis
Epidermis is the skin, consists of multiple layers of cells.
The stratum granulosim and spinosum contain lamellar bodies.
These organelles contain lipids which form a watertight lipid layer.
REspiratory Tract
Bronchial Cilliated EPithlial Cells.
Gut
Mucus secreting goblet cells.
Antimicrobial proteins e.g PAtoeth Cells.
COmmensal bacteria out compete pathogens.
ANtimicrobial peptides.
Protection by immune system
REcognition of pathogen & REsponse
Any pathogen needs recognisinf
Mount a reaction to eliminate it.
Specific recognition enable a specific response.
Non-specidic recognition ebables a non specific response
Immune recognition- distinguishign foreign invaders from self-components. Triggers an effector response that eliminates or neutralises the invader.
Immunological Memory- Certain exposures induce a rapid and heightened immune reaction upon a later attach called a memory response.
Site of the infectoo and type of pathogen determine which immune response is effective.
Viruses, bacteria and some protozoa replicate inside host cells, therefore these infectred cells have to be destroyed.
Many bacteria a nd parasites live in tissues therefore different immune response is neede.d
Phagocytosis
Plasma membrane of phagocytic cells, expands around the particulate material which may include whole pathogenic organis,s
Phagosomes in macrophages have reactive oxygen species, neutrophils contain lactoferrin.
Granules and lysosoymes fuse with phagosome producing phagolysosume where digestive enzymes are secreted into.
Receptor Mediated Endocytosis
1)Molecule binds to protein receptor
2) Receptor-molecule moves to clatharin-coated pit.
3) Cell membrane folds inwards.
4) Formation of a coated vesicle/
5) Vesicl e fuses with an endosome
6) REceptors and molecules separate.
Soluble molecules in innate immune response.
Lysosymes- Hydrolytic enzyme able to cleave bacterial cell wall.
Inteferons - A group of proteins produces by virus-infected cells.
Cytokines- Chemokines, interleukins,
Collectins - Proteins that directly disrupt the vace=terial lipid membranes or by aggravating the bacteria to enhanac e susceptibilyty to phagocytosis.
COmpliment- A group of serum proteins in an inactive state. When activated, able to damage the membranes of pathogenic organisms. Activation is a cascade reaction with each component sequentially acting on others.
AMP- AntiMicrobial PEptides
Hsot defence peptides- usually 10 to 50 residues long.
A key com[onent of the innate immune system, they act against resistanc epathogenic organisms.
Defensisn- by neutrophils, macrophages and epithelial cells.
Cathelicidin, by neutrophils and epithelilals cells.
Lactoferrin - in milk and secretions.
AMP Mechanisms
Teo modes of action - Direct Killing & Immuene modulation.
Direct Killing
PAMPS - PAthogen ASsociated Molecular Pattens
A successful PAMP induces a widespread non specific response.
Must be
Easily distinguishable
Essential for pathogen survival.
PResent on a wide range of pathogens.
There is a constant selective pressure on the immune system to respond to these PAMPS.
Microbial PAMPS- Lipopolysscccharides, Porins, peptidoglycans, glycodlipids…….
PPRS- Pattern REcognition receptors.
p
Thr complement Pathway
Pattern REcognition
Adaptive Immunity
Adaptive Immunity
Provided by lymphocytes
Adapts to pathogens
Long Lasting (memory cells).
Neutrophils & Macrophages
Key cells of innate immunity
B & T cells
Key cells of adaptive immunity
Antibodies, amde by B cells, are important molecules and mediators of the adaptive immunity.
T cells need the help of MHC to see antigens.
Lymph and Kymph nodes
Lymoh percolates through the tissues, collecting cells and antigens,
Cell encounters occur in specialised lymphoid tissue
Lymphocyte training,
Antigenic Specificity
Can distinguish subtle differences among antigens.
ANtibodies can identify a single amino acid difference between two pathogenic proteins,
Diversity
In the recognition of molecules; can recognisea single type of organism and differentiate among this with minor genetic variations.
Immunologic Memory
A second encounter with the dame antigen induces a heigthenes state of immune reactivity.
Confers immunity.
Self-Non Self recognition
Ability to distinguis self from non self and respond only to nonself is essential
Primary Immune response
The first encounter with a pathogen.
Longer lag time.
Less specific response.
Secondary Immune REsponse
Faster response.
Second and subsequent infections eith the same pahtogen,
More specific response.
Principle of vaccination.
COmponents of adaptive immunity
Cellular- T cells
Humoral- B cells
Success of acquires immune response depends on the functions of both the cellular and humoeal responses as well as interactions with them.
Immune System Cells
All immune system cells are derived from haematiopoitic stem cells.
Heamtopoeiss is the formation of blood cells.
White blood cells, leukpcutyes, immune system cells.
Haematopoeisis shifts during development and occurs throughout life in bone marrow.
Where do lymphocytes come from?
Both B cells and T cells start off in the bone marrow.
They develop from Haematopoietic Stem Cells by a process ca;;ed Haematopoiesis.
HSCs become common lymphocyte progenitors which then differentiate into the different Cells.
B cells stay in the bone marrow whilst T cells go to the thymus to mature.
Generation of CLonal Diversity- Production of T and B cells with all possible receptors.
Clonal Selection - Selection, proliferation and differentiation of individual T and B cell receptors for a specific antigen.
T and B cells
T cells can wipe out infected or cancerous cells.
Also direct the immune response by helping B lymphocytes to eliminate invading pathogens.
B cells have the ability to transform into plasmacytes and are responsible for producing antibodies.
Lymphocytes present receptors for antigen recognition with different specificity on their surfaces.
Cell-Mediated Immunity
REsistance to pathogens or cancerous cells from the activation of T cells.
ACtivated T cells form subsets of effector cells along with memory cells.
Effector cells actively engage in immune responses.
Memory Cells remember the specific antigen and responding more rapidly and effectively against future infections.
T cells are particulary important in protection against viruses and pathogens that are resistant to killing by normal neutrophiles and macrophages.
Types of T cells
Cytotoxic T cells (Tc)
Attack and kill targets directly such as cells infected by viruses or cancerous cells.
Helper T cells (Th)
Stimulates the activity of other leukocytes through cell to cell contact or through the secretion of cytokines (assembly of macrophages for pahgocytosis, trigger B cell activation).
REgulatory t cells (Tr)
Shut down an immune response after the antigens have been destroyed and prevent inapporpriate immune reactions.
Memory T cells (™)
Respons quickly to a second challenge of the same antigen.
B Cells
Stromal cells of the bone marrow.
Humoral Immune Response
ANtibody Mediatied Immunity
Mediated by a population of antibodies, that can produce more antibodies rapidlyty to a second challenge with the same antige,
Antibodies circulate in the blood and bind to antigens on infectious agents, resulting in direct activation of the microorganis, or activation of a variety of inflammatory mediators to destroy pathogens.
ANtibodies are primarily responsible for protection against many bacteria and viruses.
Antibodies
Y shaped proteins that are specific to each pathogen
Able to lock onto the surface of an invading cell and mark it for destruction by other immune cells.
Immunoglobulin is a serum glycoprotein produced by plasma cells.
Antibody is one particular set of immunoglobulin which have a specificity to a particular antigen.
Consists of four polypeptides; Two heavy chains and two light chains.
Dual functions; Antigen binding and biological activity mediation.
Types of Immunoglobulins
IgA
Secreted into mucus, saliva, tears and colostrum
Tags pathogens for destruction
IgD
B cell receptor, stimulates release of igM.
IgE
Binds to mast cells and basophils.
Allergy and antiparasitic activity.
IgG
Bidns to phagocytes.
Main blood antibody for secondary responses.
Crosses placenta.
IgM
Fixes complement.
Main antibody of primary responses.
B-cell receptor
Immune system memory.
Antigen-Antibody Binding
When antigens bind to antibodies it changes the shape of the antigen molecule slightly so the hidden regions are exposed.
ANtibodies may protect the host by covering sites on the microorganism that are needed for attachment thereby preventing infection.
Most toxins of bacteria are proteins that bind to cell surface molecules and damage cells.
Protective antibodies can bind to the toxins and prevent their interaction with host cells.
Active Immunity Vs Passive Immunity
Natural Immunity
Natural immunity is the deliberate exposure to a causative agent.
Active Natural Immunity
A child develops measles and acquires an immunity to subsequent infection.
Passive Natural Immunity
A foetus receives protection from the mother through the placenta or an infant from the mother's milk.
Artificial Immunity
Articial immunity is another deliberate exposure to a causative agent.
Active Artificial immunity
Intentional exposure e.g Vaccination
Passive Artificial Immunity
Injection of protective materials taht was developed by another individuals immune system
Immunisation
The principle of vaccination is based on specificit abd memory of adaptive immunity.
MEmory cells allow the immune system to mount a much stronger response on a second encounter with the antigen where the secondary response is faster and more effective than the primary response.
After a pthofen or is toxinf in a way that hey become innocuous without losing antigenicity.
Antibodies and T cells recognise particular parts of antigens, the epitopes and not the whole organism or toxin.
T-lymphocytes and ANtibodies are produces.
Vaccines
A weakened or dead form of a pathogen or subunits from it that aew known to stimulate the immune system to generate an immune response.
Vaccines are typically administered using an injection, some through nasal spray.
Pathogenesis
Host-Parasite Relationship
Microorganisms engage in relationships with host species.
This relationship is referred to as symbiotic.
Mutualism
A mutually beneficial relationship.
Commensalism
A relationship in which the host is neither harmed nor benefited whilst the coloniser benefits.
Many feeding relationships are commensal.
Parasitism
Oarasitism is a relationship in which the host is harmed and the parasite benefits.
This is the relationship microorganisms engage in when causing human disease.
The same microorganism can potentially engae in a parasitic of commensal/mutualistic relationship with the host dependant on the circumstances.
Whilst parasitic relationships benefit the parasite causing excessive harm to the host does not necessarily benefit the parasite.
It invites the possibility of coextinction.
If the parasite causes extinction of the host, it is also at risk of extinction,
Most parasites have not evolved to cause severe or debilitating disease but have evolved to conventional parasitism.
Direct & Indirect Pathogenesis.
Microorganisms ay directly cause disease or the immune sustem may cause inadvertant damage in attempts to target infecting microorganisms.
Direct Pathogenesis
In direct pathogenesis the microorganism directly induces harm to the host.
E.g Polio causies the lysis of motor neurones and therefore paralysis.
One form of direct pathogenesis is the lysis of host cells.
HIV mediation lysis of immune cells, which leads to immunodeficiency and ultimately AIDS.
Often associated with viruses as they are intracellulaar pathogens,
ANother form of direct pathogenesis is the release of exotixins that cause host damage.
Exotoxins are proteins released by bacterium
E.g Clostridium botulinum, releases a neurotoxin that acts at the nerve muscle junction and inhibits the release of acetylcholine, prevents the signalling events required for muscle stimulation.
Indirect Pathogenesis
The microorganism indirectly induces harm to the host.
HArm occurs as a consequence of immune activation.
AS the immune activation is a response to the presence of the microorganism, the microorganism can be considered responsible for the harm just indirectly.
E.g symptoms of the common cols are caused by localised inflammation as a response to the virus.
LPS stimulates a potent, widespread immune response, which immediately causes fever and inflammation,
Pathogenesis dissemination can cause septic shock, not primarily antibody based.
Hypersensitivity
Essentially hyperactivation of the immune system
Type 1- Immediate hypersensitivity, allergen triggers degranuation of mast cells to release histamine,
Type 2- Mediated by antibodies tagetins the infectious organism.
Type 3- Caused by high levels of immune complezxes, accumulating in tissues and blood vessels.
Type 4-m Cell mediated immunity invariably causes tissue damage.
Extreme Parasitism and coextinction
In general it os not beneficial for a parasite to cause dearh in the host.
In a symbiosis, the microorganism is dependant on a the host organism to some degree.
These relationships are often very specialised which creates th eissue of host availability, there is a threat of coextinction.
Parasitic microorganisms therefore typically cause limited disease.
The exceptions tend to be emerginf parasites where no abalance has evolced, other example have simply evolved to be extreme parasites.
Parasitic Castraters
Cause severe damage to the host in the form of castration but derive hughe benefits.
E.g Green Crabm penetrates the host results in gonad atrophy.
Parasitoids
Cause severe damage (death) but derive huge benefits.
Diagnosis
Eifexq
 Knowt
Knowt