Lecture 9_Bone and Skeletal tissues
Chapter 6: Bone and Skeleton
Overview
Focuses on the skeletal system, its structure, and various functions.
Explores osteoporosis as a significant health concern related to bone integrity.
Skeletal Cartilages
Characteristics:
All contain chondrocytes in lacunae and an extracellular matrix.
Types of Cartilage:
Hyaline Cartilage:
Provides support, flexibility, resilience.
Only contains collagen fibers; most abundant type.
Found in articular surfaces, costal cartilage, respiratory structures, and nasal cartilage.
Elastic Cartilage:
Similar to hyaline but with elastic fibers for strecht and recoil.
Located in the external ear and epiglottis.
Fibrocartilage:
Contains thick collagen fibers for tensile strength.
Found in menisci of the knee, intervertebral discs, and pubic symphysis.
Growth of Cartilage
Types of Growth:
Appositional Growth (out—— in)
Cartilage-forming cells in perichondrium secrete matrix against external face of existing cartilage.
Action of Chondroblast: They produce new cartilage matrix, leading to an increase in the overall width and thickness of the cartilage structure.
Chondroblasts are toward the periphery and as they mature they move to the center as chondrocytes.
Interstitial Growth (in—— out):
Chondrocytes within lacunae divide(mitosis) and secrete matrix, expanding cartilage from within.
Calcification of Cartilage:As the cartilage matures, it undergoes calcification, where minerals are deposited in the matrix, leading to a hardening of the tissue and contributing to the transition from cartilage to bone during endochondral ossification.
Normal during bone growth; hardens cartilage but isn't bone until osteoid is laid down on top.
Perichondrium: A layer of dense connective tissue that surrounds cartilage, providing support and protection, as well as serving as a source of new chondrocytes during growth and repair.
Classification of Bones
Total Bones: 206 named bones in the skeleton.
Two Groups:
Axial Skeleton:
Comprises the skull, vertebral column, rib cage.
Appendicular Skeleton:
Includes bones of upper/lower limbs
Girdles attaching limbs to axial skeleton
Functions of Bones
Seven Key Functions:
Support: Framework for body and organs.
Protection: Shields brain, spinal cord, vital organs.
Movement: Provides levers for muscle action.
Mineral and Growth Factor Storage: Reservoir for calcium and phosphate.
Blood Cell Formation: Hematopoiesis in red marrow.
Triglyceride Storage: Energy reserve.
Hormone Production: E.g., Osteocalcin regulates bone formation.
Bone Anatomy
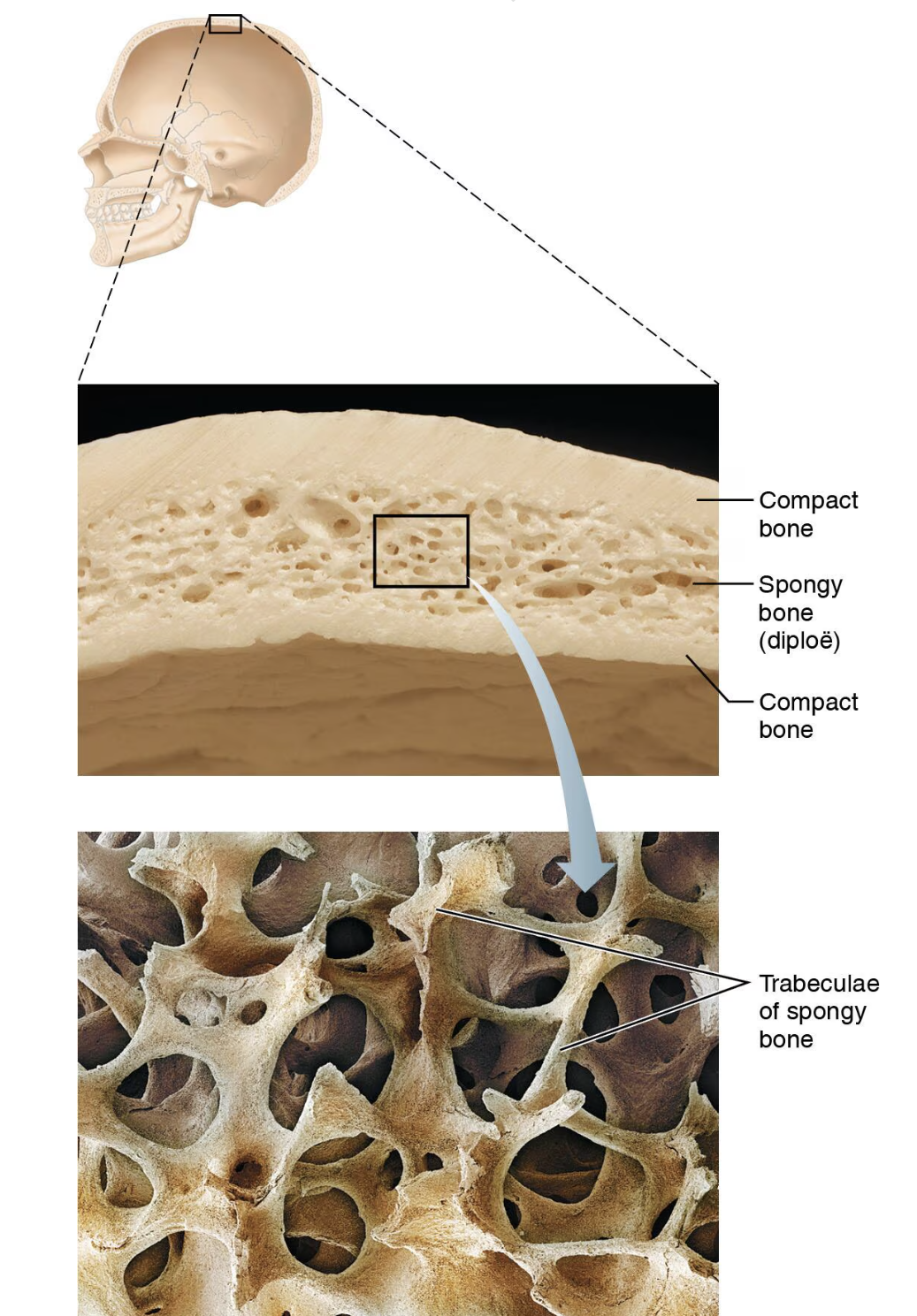
2 Big Bone Textures:
Compact Bone (lamellar): Dense outer layer, smooth and solid.
Spongy Bone (Trabecular): Honeycomb structure of thin-flat pieces beneath/covered by compact bone.
Thin plates of spongy/trabecular bone are sandwiched between connective tissue membranes: Periosteum(outer layer), and Endosteum (inner layer)
Structure of Short, Irregular, and Flat Bones:
Thin plates of spongy bone covered by compact bone, bone marrow within and throughout spongy bone.
Features of Spongy(trabecular) bone. fig 6.
Diploe: the layer of spongy bone found between two layers of compact bone in flat bones, such as the skull, which helps reduce weight while providing strength.
Long Bone Structure
Key Elements:
Diaphysis: Tubular shaft (long axis) with compact bone surrounding the medullary cavity; location of Yellow bone marrow( long bones)
Epiphyses: Ends of bones.
External compact bone; internal spongy (trabecular) bone.
Articular cartilage covers articular sufaces - Hyaline cartilage that reduces friction and absorbs shock at the joints.
Epiphyseal line: seen between diaphysis and epiphysis: the remnant of the epiphyseal plate, which is responsible for bone growth during childhood and adolescence, indicating the closure of the growth on epiphyseal plate once hyaline cartilage is ossified and skeletal maturity is reached.
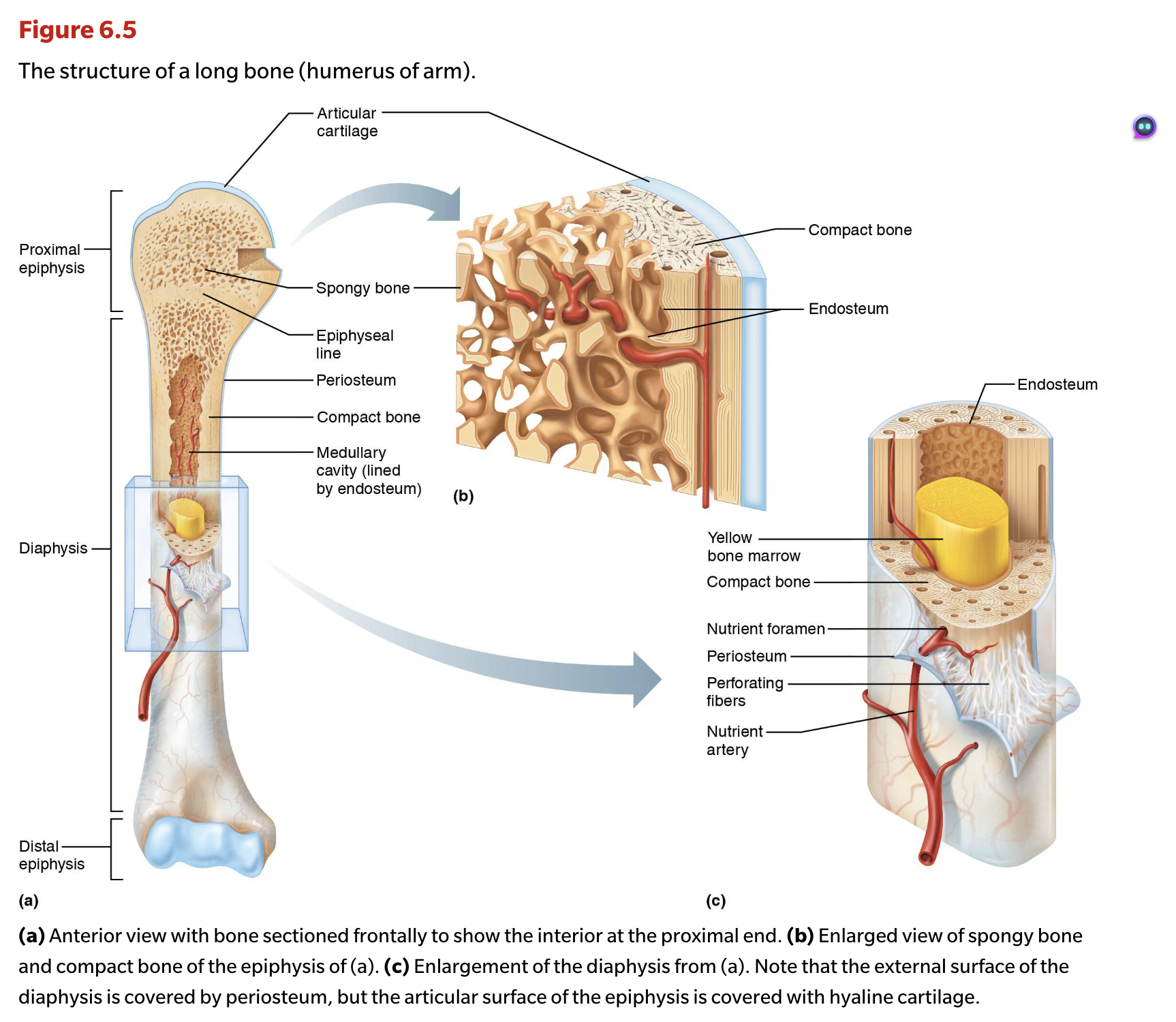
Membranes of Bone fig 6.5c
Periosteum:
Double-layered membrane covering bone surfaces except joint surfaces.
Outer fibrous layer of dense irregular connective tissue.
Sharpey’s fibers (Perforating fibers) secure to bone matrix.
Osteogenic layer up against bone: contains primitive stem cells - osteogenic cells.
Many fibers and blood vessels.
Anchoring points for tendons and ligaments.
Endosteum:
Delicate connective tissue lining internal bone surfaces, involved in bone growth and repair.
Covers trabeculae of spongy bone.
Lines canals that pass through spongy bone.
Contains osteogenic cells that can differentiate into osteoblasts and osteocytes, contributing to the maintenance and remodeling of bone tissue.
Hematopoietic Tissue in Bones
Red marrow Location:
Found mainly in trabecular cavities of spongy bone and diploë of flat bones (sternum)
Adult long bones have little red marrow; heads of femur and humerus only.
Red marrow in diploe and some irregular bones is most active.
Bone Cell Types. 4 major cell types.
Major Bone Cells:
Osteogenic Cells: Stem cells developing into other bone cells.
Osteoblasts: Matrix-synthesizing and secreting cell ; responsible for bone growth.
Osteocytes: Mature bone cells that monitors and maintains the mineralized bone matrix.
Osteoclasts: Cells that degrade(resorbs) bone tissue.
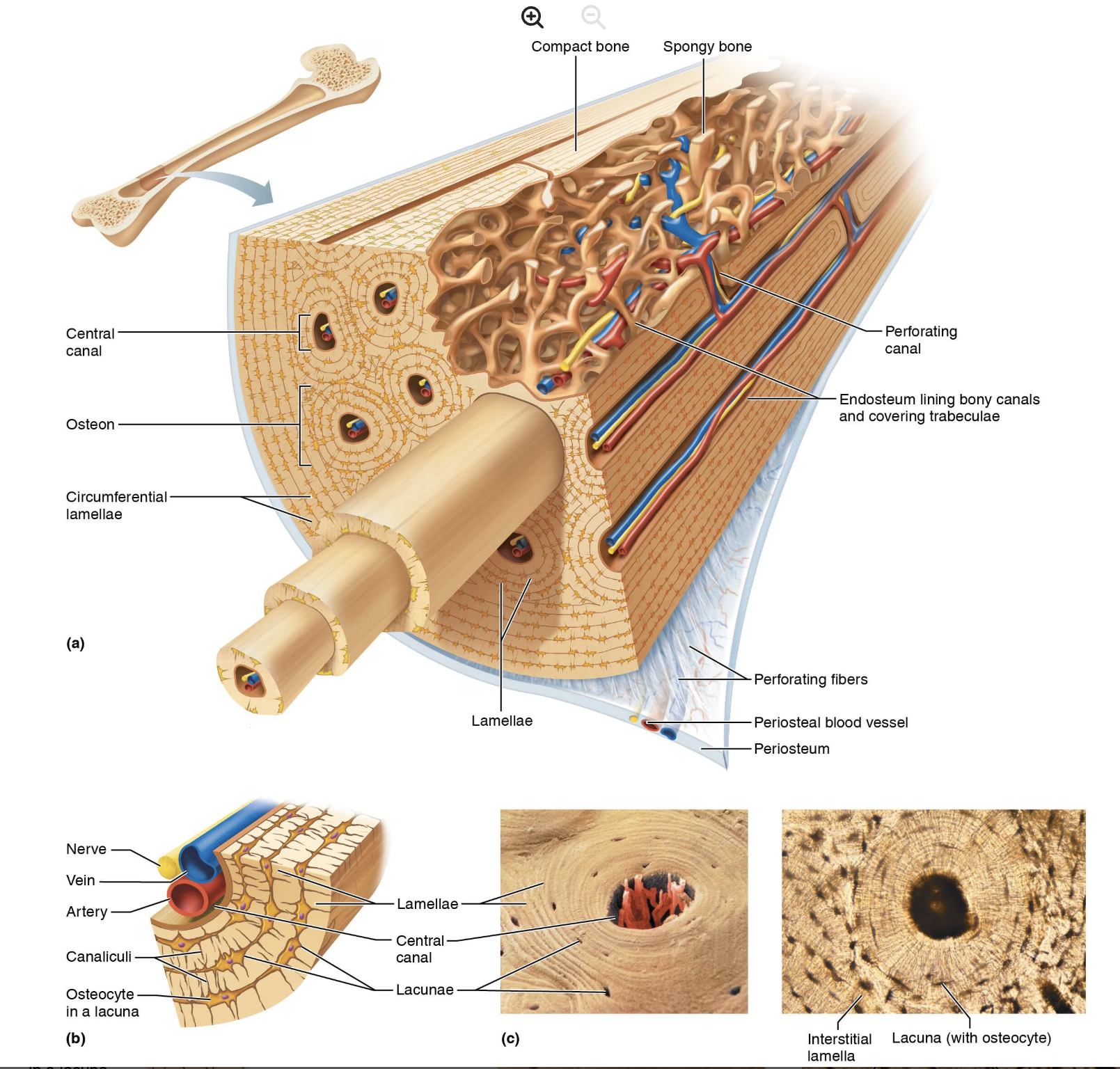
Microscopic Anatomy of Bone
Compact Bone (lamellar):
Composed of structural units called osteons or Haversian systems.
The central canal contains blood vessels and nerves; lamellae form concentric rings.
Collagen fibers in adjacent rings run in different directions.
Withstands stress-resist twisting.
Canals and Canaliculi.
Central (Harversian) canal: runs through core of osteon; contains blood vessels and nerves that supply the bone, facilitating communication and nourishment throughout the bone tissue.
Perforating canals (Volkmann's canals): connect adjacent osteons
Connects blood vessels and nerves of periosteum, medullary cavity, and central canal.
Lacunae: small cavities that contain osteocytes.
Canaliculi: hair like canals that connect lacunae to each other and central canal, allowing for the exchange of nutrients and waste products between osteocytes and the blood supply.
Lamellae
Interstitial lamellae: incomplete layers of bone matrix found between the osteons.
Remnants of osteons cut by bone remodeling.
Circumferential lamellae: layers of bone matrix that encircle the entire bone, providing structural support and strength to the outer surface, helping to resist bending and torsion.
Anatomy of Spongy bone.
Appears poorly organized, consists on:
Trabeculae
Align along lines of stress to help resist it.
No osteons
Contain irregularly arranged lamellae and osteocytes interconnected by canaliculi.
Capillares in endosteum supply nutrients.
Chemical Composition of Bone
Includes cells and osteoid.
Osteogenic cells, osteoblasts, osteocytes, bone-lining cells, and osteoclasts.
Osteoid: 1/3 of organic bone matrix secreted by osteoblasts.
Made of ground substance (proteoglycans and glycoproteins)
Collagen fibers
Contributes to structure: provides tensile strength and flexibility.
Resilience of bone due to collagen molecules.
Organic = Cells+ osteoids—- Matrix
Inorganic = Hydroxyapatities(calcium phosphate) providing hardness and strength.
65% of bone by mass
Mainly of tiny calcium phosphate crystals in and around collagen fibers.
Responsible for hardness and resistance to compression.
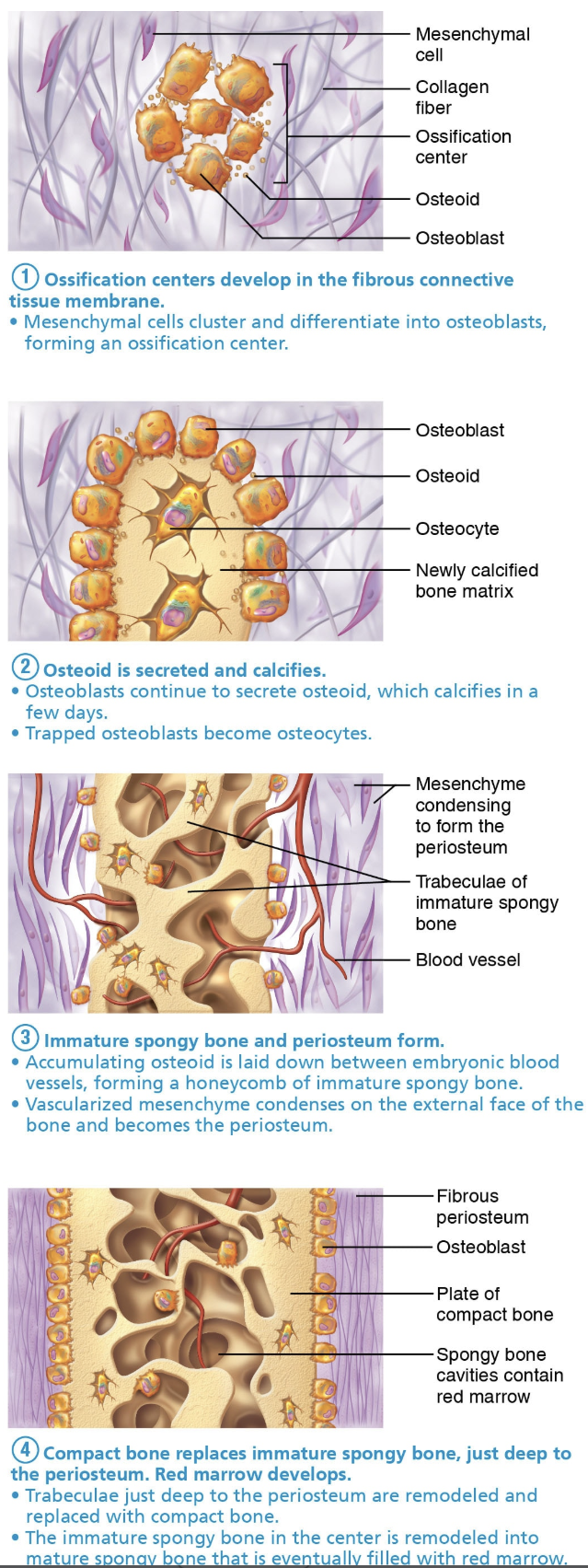
Bone Development
Ossification(osteogenesis): formation of bone tissue from Hyaline Cartilage
Formation of bony skeleton.
Begins in the 2nd month of development.
Postnatal bone growth:
continues after birth until early adulthood.
Bone remodeling and repair:
Involves lifelong remodeling and repair.
Two Types of Ossification:
Both are used for pre-natal development of bones.
Intramembranous Ossification: Directly forming bone from fibrous membranes.
This process forms the cranial bones of the skull (e.g., frontal, parietal, occipital, and temporal bones) and the clavicles.
Ossification centers develop in the fibrous connective tissue membrane.
Mesenchymal cells cluster and differentiate into osteoblasts, forming an ossification center.
Osteoid is secreted and calcifies.
Osteoblasts continue to secrete osteoid, which calcifies in a few days.
Trapped osteoblasts become osteocytes.
Immature spongy bone and periosteum form.
Accumulating osteoid is laid down between embryonic blood vessels, forming a honeycomb of immature spongy bond.
Vascularized mesenchyme condenses on the external face of the bone and becomes the periosteum.
Compact bone replaces immature spongy bone, just deep to the periosteum. Red marrow develops.
Trabeculae just deep to the periosteum are remodeled and replaced with compact bone.
The immature spongy bone in the center is remodeled into mature spongy bone that is eventually filled with red marrow, contributing to the overall function of hematopoiesis in adults.
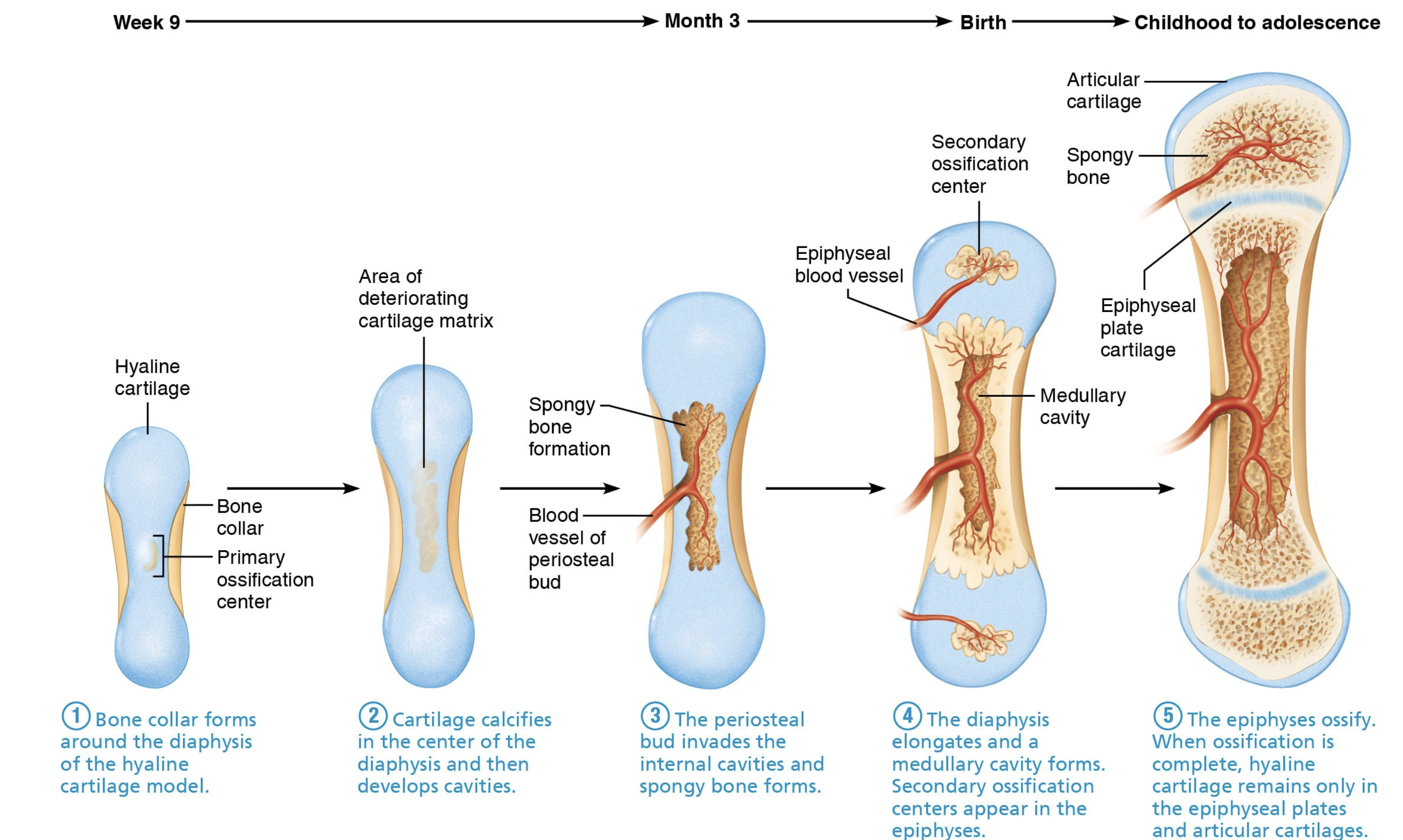
Endochondral Ossification: Replacing hyaline cartilage.
This process forms all bones below the base of the skull, except for the clavicles.
Bone collar forms around the diaphysis of the hyaline cartilage model.
Cartilage calcifies in the center of the diaphysis and then develops cavities.
The periosteal bud invades the internal cavities and spongy bone forms.
The diaphysis elongates and a medullary cavity forms. Secondary ossification centers appear in the epiphyses.
The epiphyses ossify. When ossification is complete, hyaline cartilage remains only in the epiphyseal plates and articular cartilages.
Bone Growth
Types of Growth:
Interstitial Growth: Lengthening long bones at epiphyseal plates (hyaline cartilage).
Concurrent remodeling of epiphyseal ends to maintain proportion.
Results in 5 zones within Interstitial growth, each with distinct characteristics:
1) Resting(quiescent) zone
2)Proliferation (mitosis) zone
3) Hypertrophy(older cartilage cells enlarge)
4) Calcification zone:(matrix calcifies; cartilage cells die; matrix begins deteriorating; blood vessels invade cavity)
5) Zone of Ossification (new bone forms).
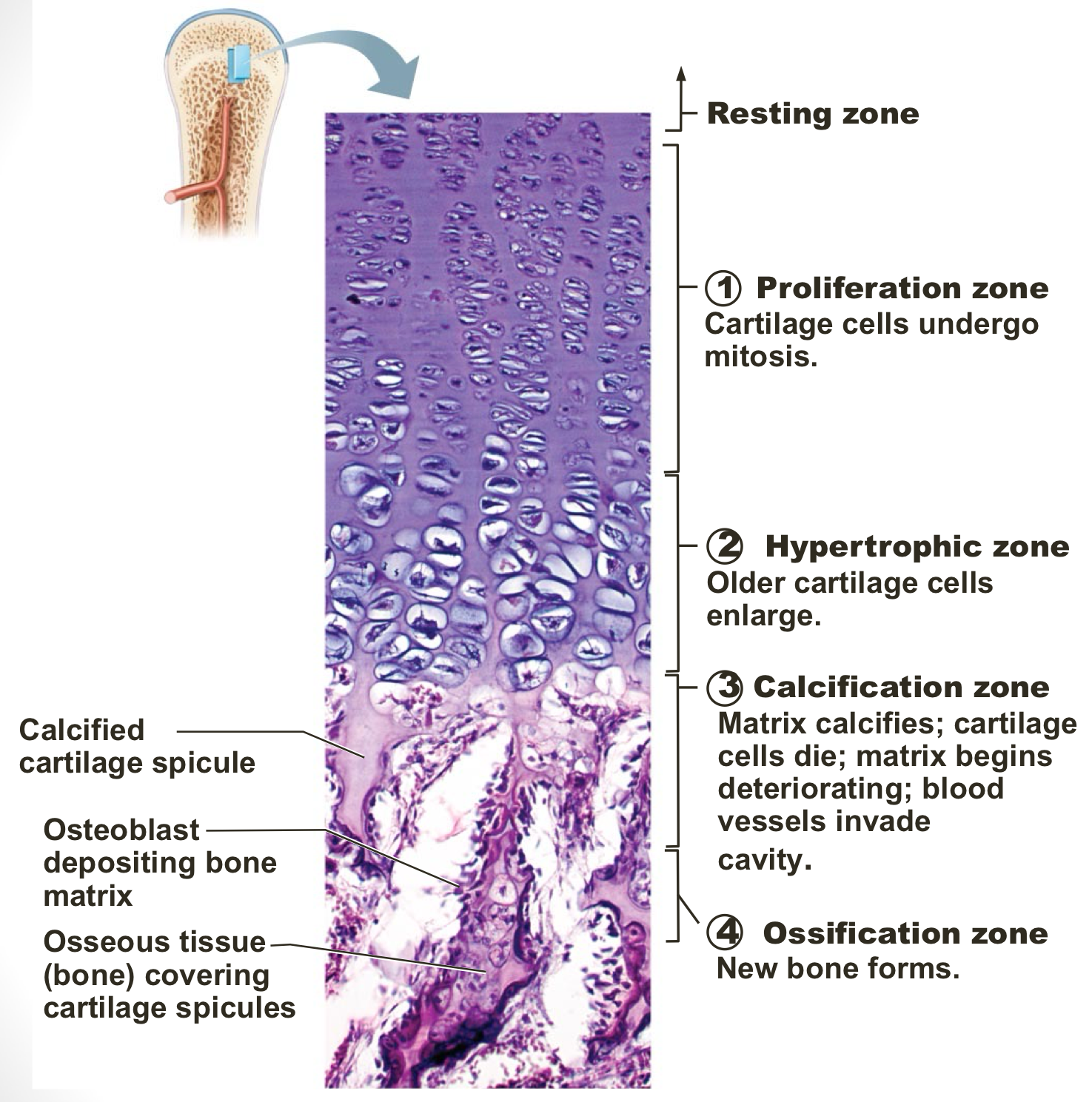
Epiphyseal plate closure - replaced with epiphyseal line.
Appositional Growth: Widening of bones through periosteum.
Occurs throughout life, allowing bones to increase in diameter and strengthen in response to stress and weight-bearing activities.
Osteoblasts beneath periosteum secrete bone matrix ion external bone.
Osteoblasts remove bone on endosteal surface.
Thicker, stronger bone but not too heavy.
Hormonal Regulation of Bone Growth.
Growth hormone: most important in stimulating epiphyseal activity in infancy and childhood.
Thyroid hormone:
Modulates activity of growth hormone.
Ensures proper proportions.
Testosterone (males) and estrogens (females) at puberty.
Promotes adolescent growth spurts.
End growth by inducing epiphyseal plate cloEsure, which ultimately determines the final height in both genders.
Excesses or deficits of any of these hormones cause abnormal skeletal growth.
Bone Homeostasis.
Bone Remodeling:
Continuous process involving deposition and resorption of bone.
Consists of bone remodeling and bone repair.
Occurs at surfaces of periosteum and endosteum.
Remodeling Units: adjacents Osteoblasts(bone deposit), Osyteoclasts(bone resorption)
Hormonal control of Blood Ca2+
Parathyroid hormone (PTH)
Produced by parathyroid glands.
Removes calcium from bone regardless of bone integrity.
Osteocalcin: regulates bone formation also protects against obesity, glucose intolerance, and diabetes mellitus.
Calcitonin is produced in the thyroid gland; it does not normally affect blood calcium levels, but does decrease blood calcium levels if taken as a drug at very high concentrations.
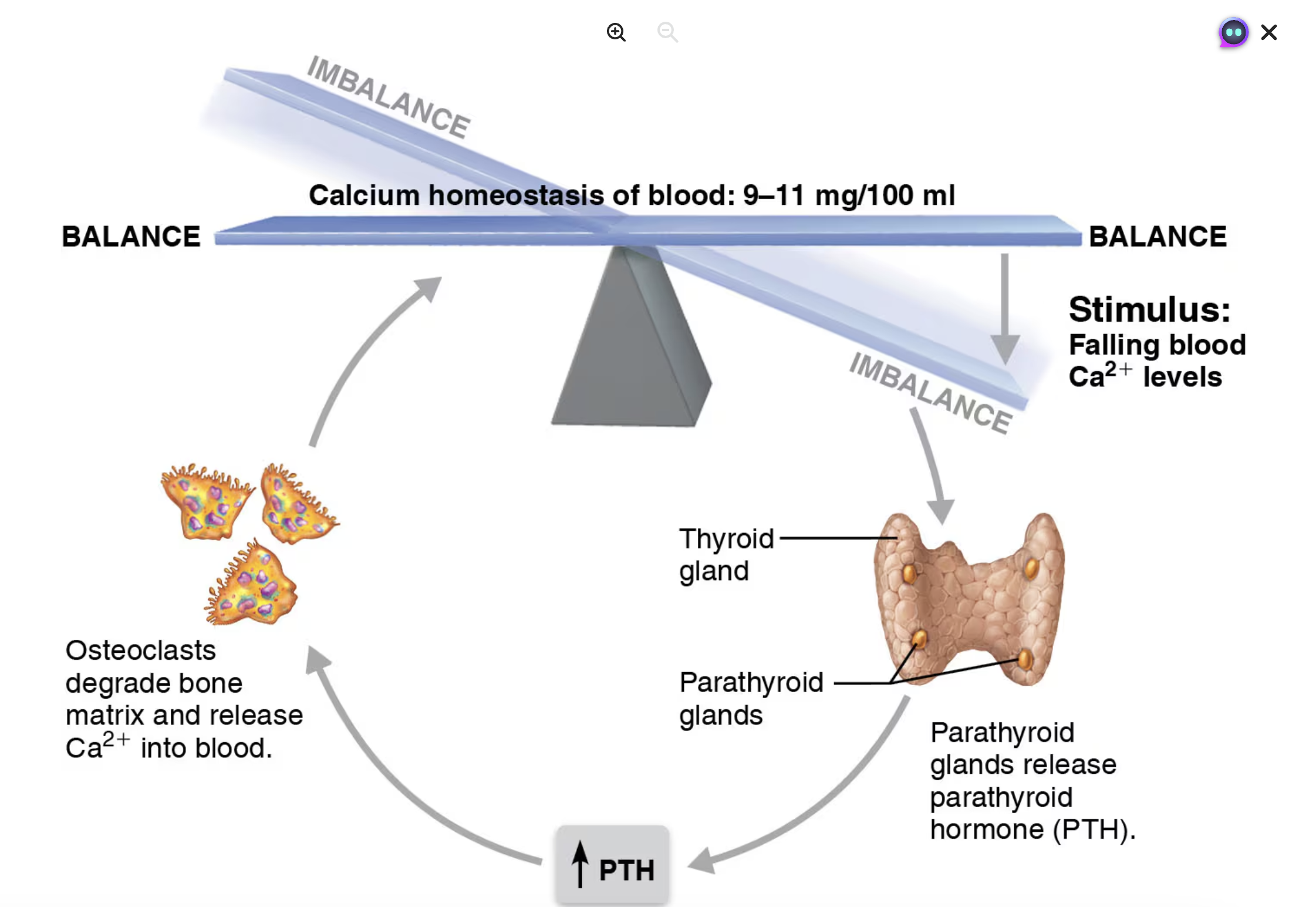
Calcium Homeostasis.
Severe Neuromuscular problems.
Hyperexcitability: causing Tetany and muscles and brain seizures when blood Ca2+ low.
Non-responsiveness - muscle weakness and depression, confusion, dementia and coma in brain when blood Ca2+ levels too high.
Hypercalcemia:a condition characterized by elevated levels of calcium in the blood, which can lead to a range of symptoms including nausea, vomiting, fatigue, and in severe cases, arrhythmias or kidney stones.
Fracture classification:
Position of bone ends after fracture.
Nondisplaced: ends retain normal position.
Displaced: ends put of normal alignment.
Completeness of break.
Complete: broken all the way through.
Incomplete: not broken all the way through.
Whether skin is penetrated
Open(compound) - skin is penetrated.
Closed(simple) - skin is not penetrated.
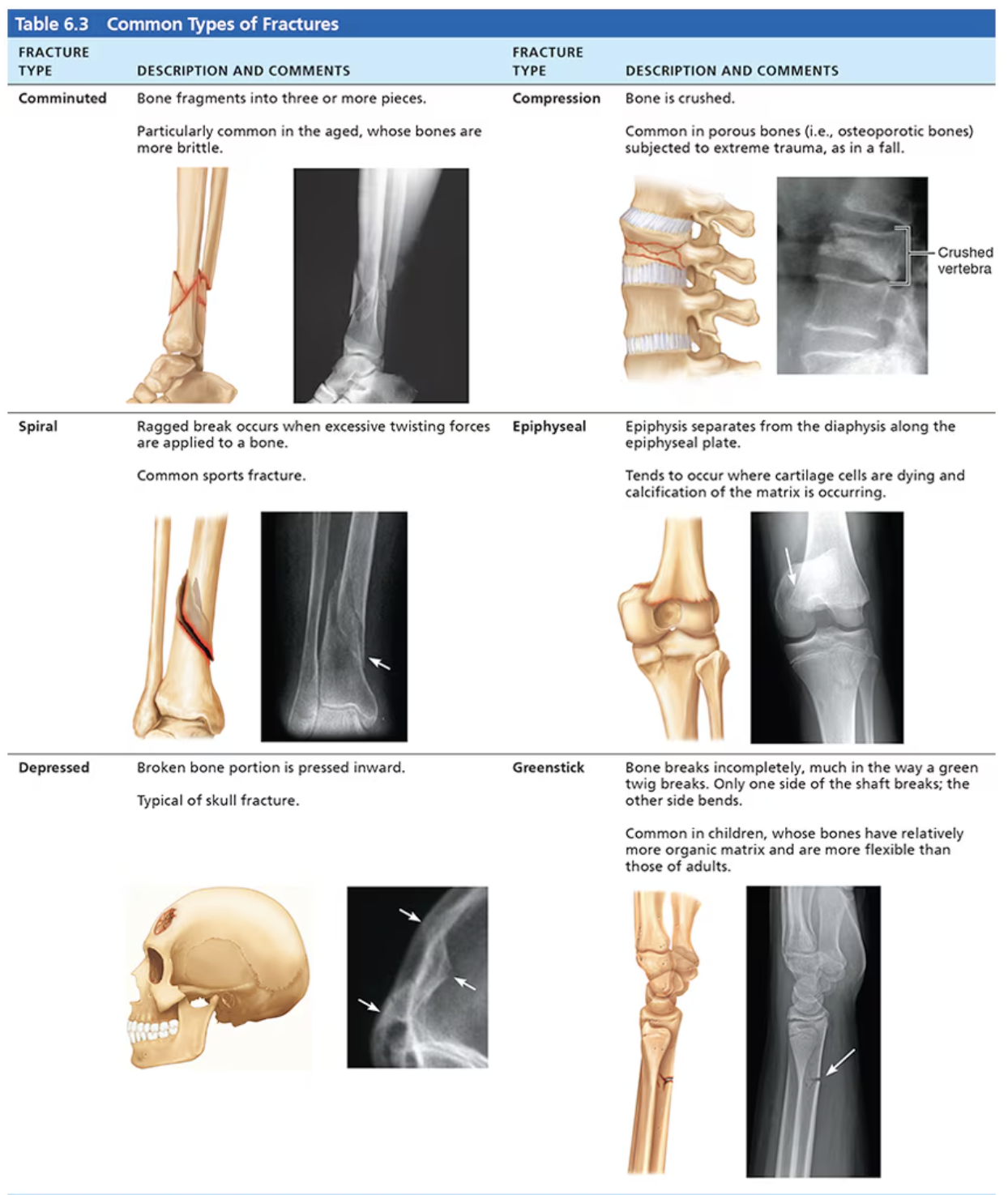
Comminuted : bone fragments into three or more pieces. Aged people since bones are more brittle.
Compression: bone is crushed, often porous bones or bones subjected to extreme trauma.
Spiral: ragged break occurs when excessive twisting forces are applied to a bone.
Epiphyseal: epiphysis separates from the diaphysis along the epiphyseal bone.
Depressed: broken bone portion is presses inward. Typical of skull fracture.
Greenstick: bone breaks incompletely, much in the way a green twig breaks. Only one side of the shaft breaks; the other side bends. Common in children.
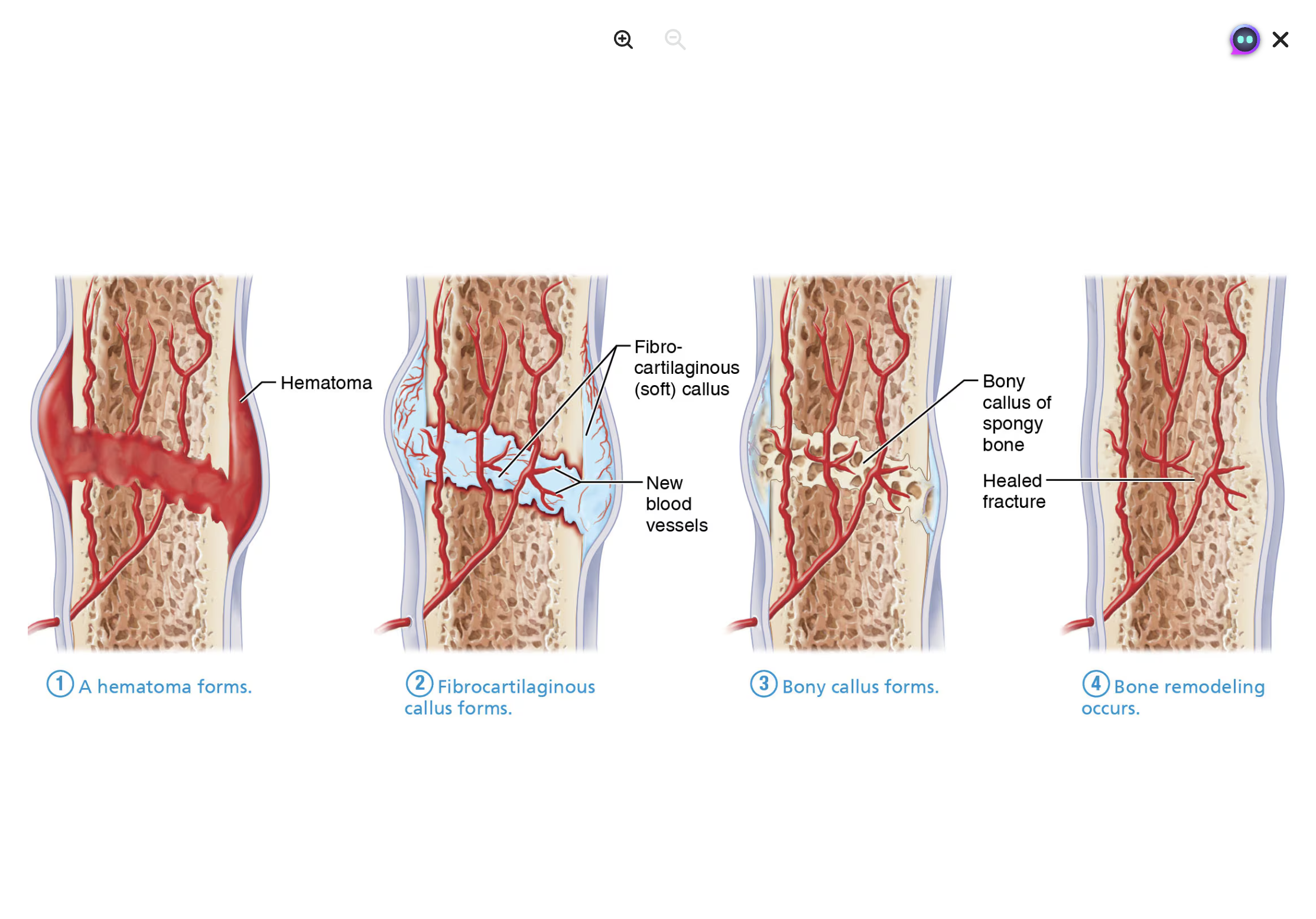
Fracture Repair Stages:
Hematoma Formation: Blood vessels tear, forming a clot.
Fibrocartilaginous Callus Formation: Cartilage matrix forms to bridge the break.
Bony Callus Formation: Callus converts to bone after about 2 months.
Bone Remodeling: Final structure resembles original bone.
/
Homeostatic Imbalances
Osteomalacia:
Soft, weak bones due to inadequate mineralization.
Pain upon bearing weight
Rickets(osteomalacia of children)
Bowed legs and other bonds deformities.
Bones ends enlarged and abnormally long.
Osteoporosis:
Condition where bone resorption outpaces deposition, leading to fragile bones and increased fracture risk.
Vertebral and hip fractures commom.