bio topic 6
6.1 Absorption
- involves movement of fluids or dissolved substances (i.e nutrients) across a cellular membrane
- absorbed components undergo assimilation within cell in order to become fluid or solid parts of an organism
Membrane transport mechanisms
Secondary active transport
- glucose & aas are co-transported across epithelial membrane with Na+
Facilitated Diffusion
- certain monosaccharides, vitamins and some minerals may be transported by epithelial channel proteins
Simple diffusion
- hydrophobic materials (i.e lipids) are capable of freely diffusing across the epithelial membrane
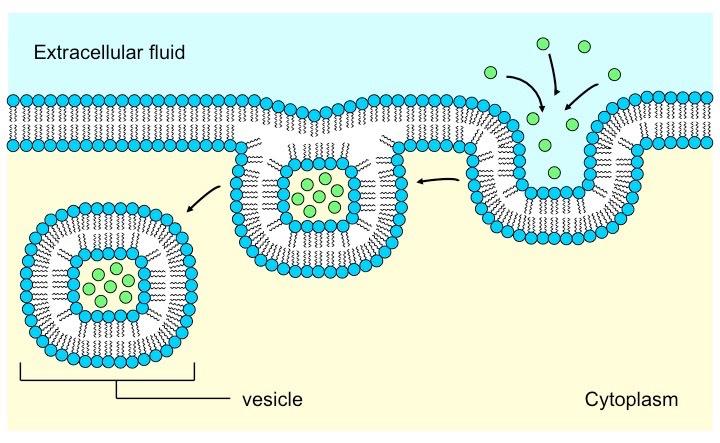
Endocytosis
dissolved materials may be rapidly absorbed en masse via the process of pinocytosis (cell “drinking”)
Villi
- finger-like mucosal projections that increase the SA of epithelium over which absorption is carried out
- key features of villi include:
Microvilli \n Rich blood network \n Single layer epithelium \n Lacteals (absorb lipids) \n Intestinal crypts (exocrine) \n Membrane proteins
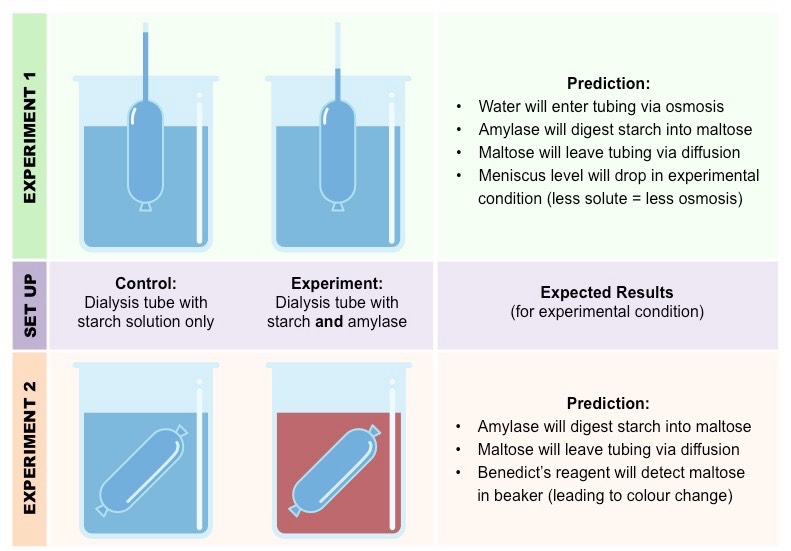
Modelling absorption
dialysis tubing used to model the size-specific permeability of a membrane
large molecules cannot cross (i.e starch)
smaller molecules can cross (i.e glucose)
if larger molecules are digested with enzymes the absorption of the smaller subunits can then be measured in a number of ways:
\
- via change in fluid/meniscus levels
\
- via the presences of specific materials (identified via treatment with a reagent)
6.1 Digestion
- main purpose of the digestive system is to break larger molecules down into smaller subunits due to the fact that:
- \
- large molecules are typically chemically inert & need to be broken down and reassembled into usable products
- \
- large molecules are typically insoluble and cannot be easily absorbed into cells whereas smaller cells are soluble
Digestive system structure
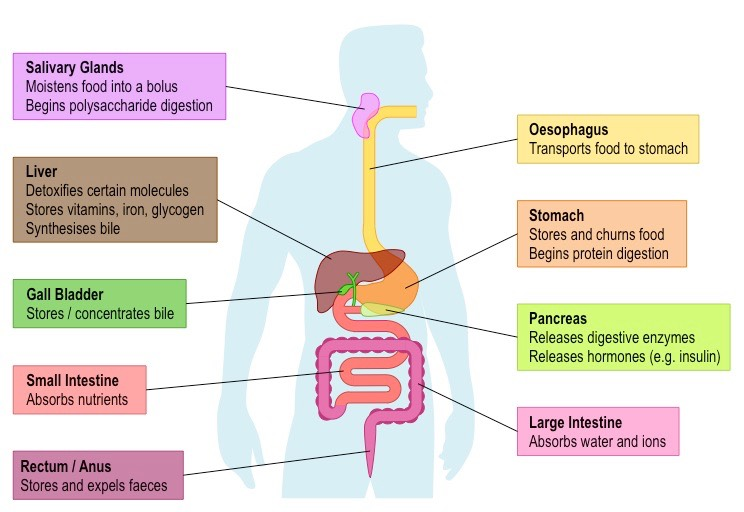
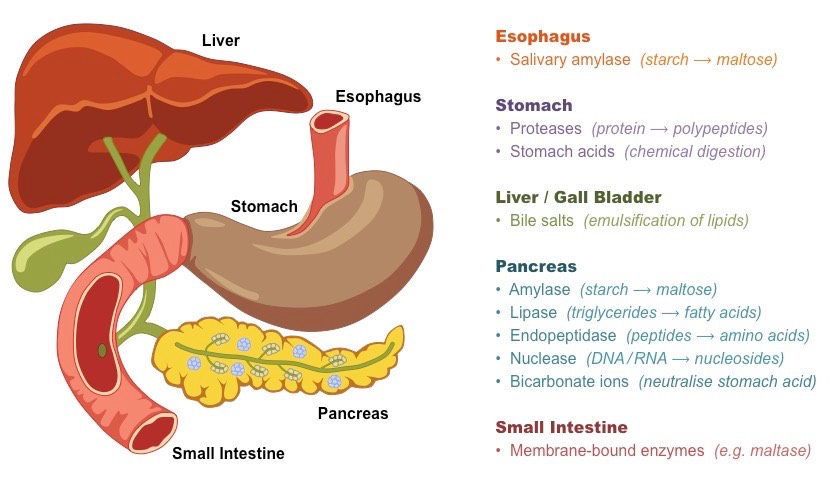
Digestive system componenets
- composed of the alimentary canal and a variety of support accessory organs
Alimentary canal (directly transfers food)
- oesophagus - food tract from mouth to stomach
- stomach - storage tank with low pH (protein digestion)
- small intestine - site of nutrient absorption
- large intestine - absorbs water and dissolved minerals
Accessory organs (supports digestive process)
- salivary glands - moistens food bolus (starch digestion)
- pancreas - secretes key enzymes into small intestine
- liver - metabolizes absorbed nutrients (produces bile)
- gallbladder - stores and secretes bile (emulsifies fats)
Digestive movement
Peristalsis
- unidirectional movement of food along alimentary canal
- caused by contraction of sequential longitudinal muscles
Segmentation
- bidirectional mixing of food within the small intestine
- caused by contraction of non-sequential circular muscles
Types of digestion
Mechanical digestion
- breakdown of food via physical actions
- chewing (grinding food using teeth)
- churning (squeezing stomach contents)
- segmentation (intestinal contractions)
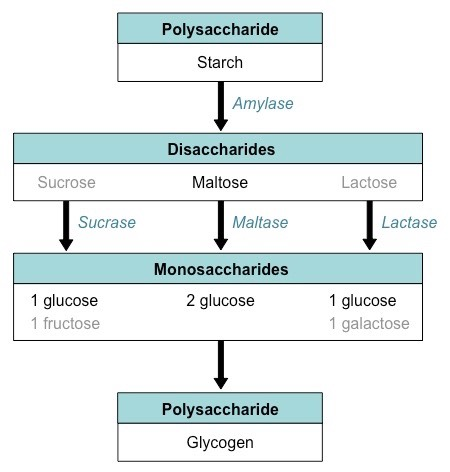
Starch hydrolysis
- starch is composed of glucose monomers
- is linear (amylase) or branched (amylopectin)
Amylase (salivary or pancreatic) digests starch
- it digests amylose into maltose disaccharides
- it digests amylopectin into dextrin chains
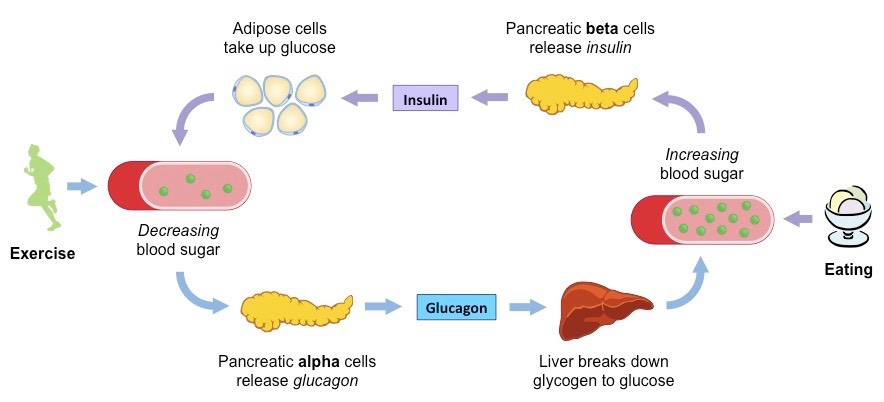
Pancreas regulates uptake of glucose
- insulin increases glucose uptake by cells
- glucagon decreases glucose uptake by cells
Liver is responsible for glucose storage
glucose is stored as glycogen (polysaccharide)
6.2 Blood system
- William Harvey proposed modern understanding of circulatory system
According to Harvey:
- major blood vessels (arteries & veins) are connected by a single network
- blood flow is unidirectional (due to the presence of one-way valves)
- heart is a central pump (arteries = from heart, veins = to heart)
- blood follows continuously and is not consumed by the body
It has further been discovered that:
- arteries and veins are connected by capillaries (via arterioles & venules)
- there is a separate circulation for the lungs (pulmonary versus system)
Blood vessels
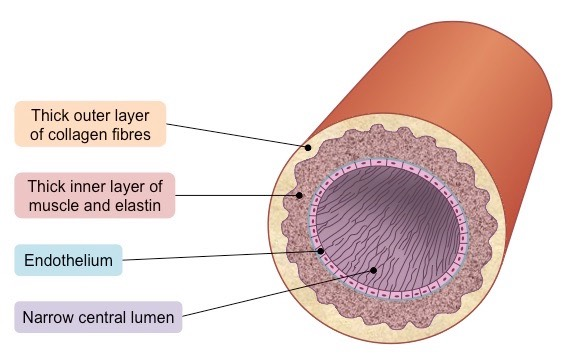
Arteries
transports blood from the heart
blood at high pressure (80-120 mmHg)
walls are thick (muscles and elastin)
walls stretch or contract with pulse
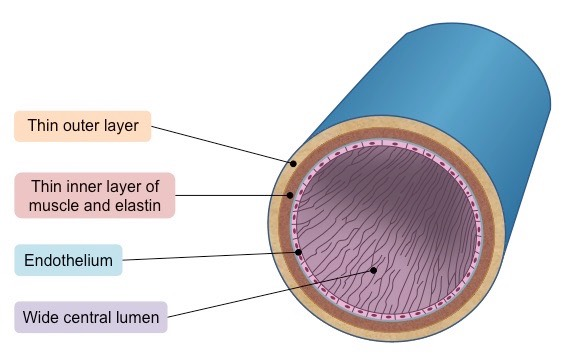
Veins
transport blood to the heart
blood at low pressure (<15 mmHg)
walls are thin (with wider lumen)
have valves to prevent pooling
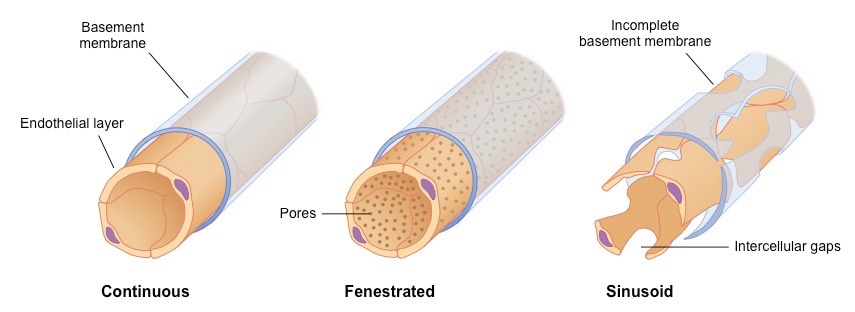
Capillaries
- facilitate material exchange
- blood at low pressure (around 10 mmHg)
- walls are made of single layer of cells
- extremely narrow lumen
Capillaries may be categorized as:
continuous (intact basement membrane)
fenestrated (have endothelial pores)
sinusoidal (discontinuous membrane)
Blood
Blood contains three main elements:
- red blood cells (transport oxygen)
- white blood cells (fight infection)
- platelets (responsible for clotting)
Blood fluid (plasma) transports:
Nutrients (i.e glucose) \n Antibodies \n Carbon dioxide \n Hormones \n Oxygen \n Urea \n Heat
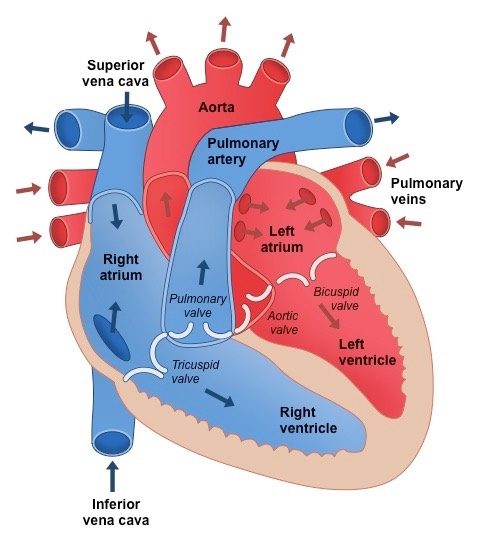
Blood flow
- A heart pumps blood around the body via two distinct circulatory pathways
Right side (of heart)
- deoxygenated blood (from tissues) enters right atrium via the vena cava
- blood in the right ventricle is pumped to lungs via the pulmonary artery
- gas exchange at the lungs (capillaries ←→ alveoli) oxygenates the blood
Left side (of heart)
- oxygenated blood (from lungs) enters the left atrium via the pulmonary vein
- blood in the left ventricle is pumped to the body tissues via the aorta
- material exchange occurs at the respiring tissue (deoxygenates the blood)
Valves in veins ensure proper circulation by preventing backflow of blood
- contraction of skeletal muscles may compress veins to aid blood flow
6.2 The heart
Heart structure
Valves:
- tricuspid valve (right)
- bicuspid valve (left)
- pulmonary valve (right)
- aortic valve (left)
Mechanism of the heart beat
- a heart beat is myogenic (contraction initiated by the heart)
- electrical signals are initiated by a sinoatrial (SA) node
- this pacemaker stimulates the atria to contract and also relays signals to an atrioventricular (AV) node)
- AV node sends signals to ventricular Purkinje fibres (via a Bundle of His within the wall of the septum)
- the Purkinje fibres cause the ventricular walls to contracts
SA node maintains a normal sinus rhythm (60-100 BPM)
- pacemaker is regulated by the medulla oblongata
- sympathetic nerves release noradrenaline (heart rate increases)
- parasympathetic nerves release acetylcholine (heart rate decreases)
- heart rate may also be increased via hormonal actions (via the release of adrenaline/epinephrine)
- adrenaline will cause a more sustained elevation in heart rate than that achieved by the action of the brainstem
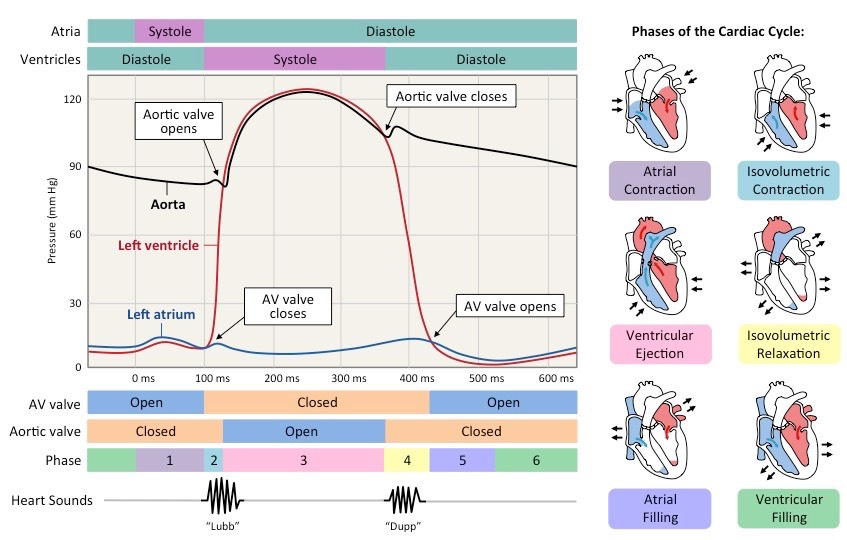
Cardiac cycle
describes events of a heart beat
Systole (contraction)
- as atria contract, atrial pressure exceeds ventricular pressure (AV valves open → blood flows to ventricles)
- as ventricles contract, ventricular pressure exceeds atrial pressure (AV valve closes → 1st heart sound)
- pressure builds (isovolumetric contraction) until the ventricular pressure exceeds the arterial pressure
- semilunar valves opens and blood flows into arteries
Diastole (relaxation)
- as blood flows into arteries, ventricular pressure drops
- backflow closes semilunar valves → 2nd heart sounds
- when ventricular pressure drops below atrial pressure, the AV valves open and cardiac cycle is repeated
Coronary heart disease
- coronary thrombosis is caused by clots within the coronary arteries
- vessels are damaged by cholesterol deposition (atherosclerosis)
- deposits reduce vessel diameter and increase blood pressure
- stress damages arterial walls (and is repaired with fibrous tissue)
- vessel wall loses elasticity and forms atherosclerotic plaques
- if a plaque ruptures, blood clotting is triggered, forming a thrombus
- if the thrombus blocks blood flow, a myocardial infraction results
- these events are collectively described as CHD
Risk factors
Risk factors for CHD include:
Genetics (i.e hypertension) \n Obesity (overweight = risk) \n Diseases (i.e diabetes) \n Diet (i.e increased consumption of trans fats) \n Exercise (inactivity = risk) \n Smoking (increased blood pressure \n Sex (males = higher risk)
6.3 Adaptive immunity
- adaptive immunity responses share two key characteristics:
- they are specific (i.e they can differentiate between different type of pathogens and respond accordingly)
- they are adaptive (i.e they produce heightened response upon re-exposure – there is immunological memory)
Antigen recognition
- antigens are substances that the body recognises as foreign and that can elicit an immune response
- antigens are presented as lymphocytes via identification markers on the surface of native cells (MHC molecules)
- MHC 1 markers are found on all body cells (except RBCs) and present endogenous antigens (cell-mediated response)
- MHC 2 markers are on innate immune cells (macrophages) and present exogenous antigens (humoral response)
Antibodies
- antibodies are proteins produced by B lymphocytes that are specific to a given antigen (they are also called immunoglobulins)
Role of lymphocytes
Humoral Immunity (targets “non-self”)
- B cells each produce one specific type of antibody
- macrophages or dendritic cells present antigen fragments (via MHC 2 markers) to helper T lymphocytes (TH cells)
- TH cells release cytokines and activate antigen-specific B cells (which rapidly divide to form many plasma cells)
- the plasma cells make antibodies specific to the antigens
- a small proportion of B cell clones differentiate into long-lasting memory B cells (for long-term immunity)
Cell mediated immunity (targets “self”)
- infected cells presents antigens on their MHC 1 markers
- antigens are recognized by cytotoxic T cells (and TH cells)
- cytotoxic T lymphocytes (TC cells) bind to the infected cell and trigger its destruction (via performing enzymes)
- TH cells stimulate the formation of memory TC cells
- TC cells can target virus-infected cells and tumor cells
- suppressor T cells regulate the action of TC cells in order ot prevent sustained T cell activation (i.e autoreactivity)
Immune system disorders
Immunodeficiency
- HIV is a retrovirus that infects helper T cells (TH cells)
- it is usually transmitted via the exchange of bodily fluids (i.e sex, breastfeeding, transfusions, injections, etc.)
- HIV is integrated into the genome of infected TH cells
- after a prolonged period of inactivity, it becomes active and lyse the TH cells as it begins to spread
- this results in an inability to produce antibodies and a general loss of immunity (disease is called AIDS)
Hypersensitivity
- allergens are substances that trigger an immune response despite not being inherently harmful (i.e peanut allergy)
- when a B cell is activated by an allergen, it makes large quantities of allergen-specific antibodies (IgE)
- these IgE antibodies bind to mast cells and “prime” them
- upon re-exposure to the allergen, the sensitized mast cells release large quantities of histamine (causes inflammation)
- this inflammatory response is called an allergic reaction
6.3 Defense against disease
Pathogens
- disease-causing agents that disrupt the normal physiology of infected organisms (i.e homeostatic imbalance)
- pathogens may be species-specific or cross species barriers
- diseases that can be naturally transmitted are called zoonotic diseases
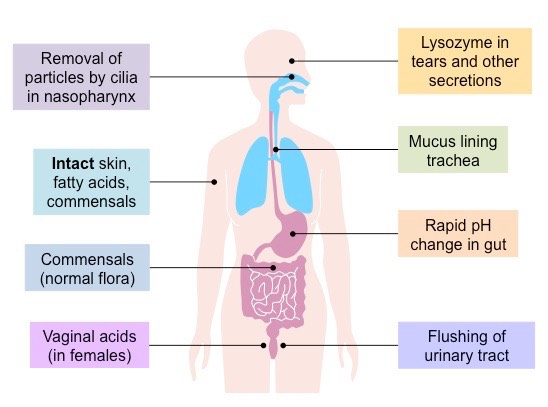
Lines of defense
- 1st line - surface barriers (skin/mucus)
- 2nd line - innate immunity (non-specific)
- 3rd line of defense - adaptive immunity
Antibiotics
- compounds that target prokaryotic features but don’t harm eukaryotic cells (i.e don’t effect host organism)
- may target structures (i.e cell wall) or metabolic processes
- some strains of bacteria have evolved with genes that confer resistance to antibiotics (some even have multiple resistance)
- the first antibiotic identifies was penicillin (Fleming, 1928), its treatment was demonstrated by Florey and Chain
Surface barriers
- first line of defense against infectious disease is the surface barriers that function to prevent pathogenic entry
Skin
- protects external structures (outside the body)
- thick, dry and composed predominantly of dead cells
- glands secrete chemicals to restrict bacterial growth
Mucous membranes
protects internal structures and cavities (inside body)
thin region composed of living cells that secrete fluid (mucus) to trap pathogens (which may then be removed)
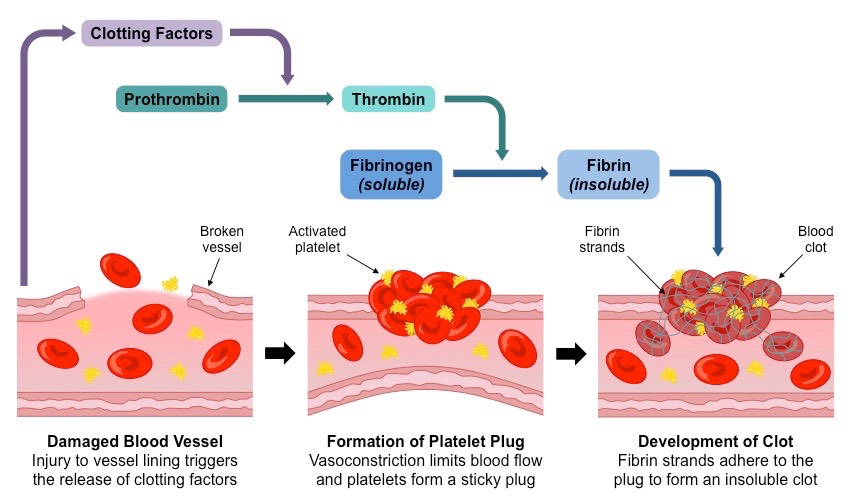
Clotting
Clotting seals damaged vessels to prevents pathogenic entry
injured cells and platelets release clotting factors
these factors convert prothrombin into thrombin
thrombin converts fibrinogen (soluble) into fibrin (insoluble)
fibrin forms mesh of fibers that block the injured site
clotting factors also cause platelets to become sticky and form a solid plug (called a clot) sealing the wound
this process of events is called a coagulation cascade
clot formation in coronary arteries lead to heart attacks
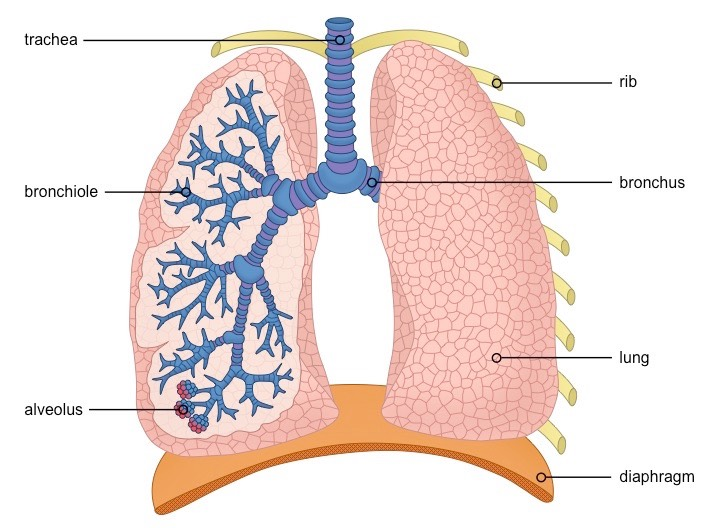
6.4 Gas exchange
Ventilation
- the exchange of gases between the lungs and the atmosphere (achieved by the physical act of breathing)
- these gases are integral to the process of cell respiration
- oxygen is an input, carbon dioxide is a by-product
- ventilation maintains the concentration gradient necessary for passive diffusion (O2 = into lungs, CO2 = out of lungs)
- ventilation rates will change with exercise and can be measured via spirometry (measure amount / rate of air)
Lung structure
Mechanism of breathing
- Breathing utilises antagonistic sets of respiratory muscles in order to facilitate the passage of air (inhalation / exhalation)
- muscles change lung volume to create negative pressure
- negative pressure is equalised by air from atmosphere
- air flows in / out according to the volume of the thorax
Inhalation
- diaphragm muscles contract (diaphragm flattens)
- external intercostal muscles pull ribs up (outwards)
- this increases the volume of the thoracic cavity
- pressure in lungs decreases below atmospheric pressure
- air flows into the lungs in order to equalise the pressure
Exhalation
- diaphragm muscles relax (diaphragm curves upwards)
- internal intercostal muscles pull the ribs down (inwards)
- abdominal muscles contract to push diaphragm upwards
- this decreases the volume of the thoracic cavity
- pressure in lungs increases above atmospheric pressure
- air flows out of lungs to equalise the pressure
Pneumocytes
- (alveolar cells) line the alveoli and comprise the majority of the inner surface of the lungs
Type 1 pneumocytes
- involved in gas exchange between alveoli and capillaries
- are extremely thin (minimizes gas diffusion distances)
Type 2 pneumocytes
- responsible for the secretion of pulmonary surfactant
- this creates a moist surface that reduces surface tension (prevents sides of alveoli from adhering to each other)
Lung disorders
Lung cancer
- cancer is uncontrolled cell proliferation, leading to tumors
- lungs possess a rich blood supply (for gas exchange), increasing the chances of metastasis (spread of cancer)
There are many factors that contribute to lung cancer:
- intrinsic: genetics, age, certain diseases / infections
- Extrinsic: smoking, asbestos, radiation exposure
Emphysema
- abnormal enlargement of the alveoli
- these form air spaces and lower the overall surface area
- emphysema is most commonly caused by smoking
- chemicals in cigarettes damage the alveoli
- phagocytes release elastase as part of immune response
- elastase destroys elastic fibres in the alveolar walls
- huge air spaces (pulmonary bullac) develop in the lungs
6.5 Neurons & synapses
Nervous system
- central nervous system (CNS) = brain and spinal cord
- peripheral nervous system (PNS) = peripheral nerves
Nervous system is composed of specialized cells called neurons that function to transmit electrical signals
- CNS coordinates sensory & motor signals from the PNS
- sensory neurons send signals to the CNS (afferent pathway)
- motor neurons send signals from the CNS (efferent pathway)
- relay neurons (interneurons) send signals within the CNS
Structure of a motor neuron
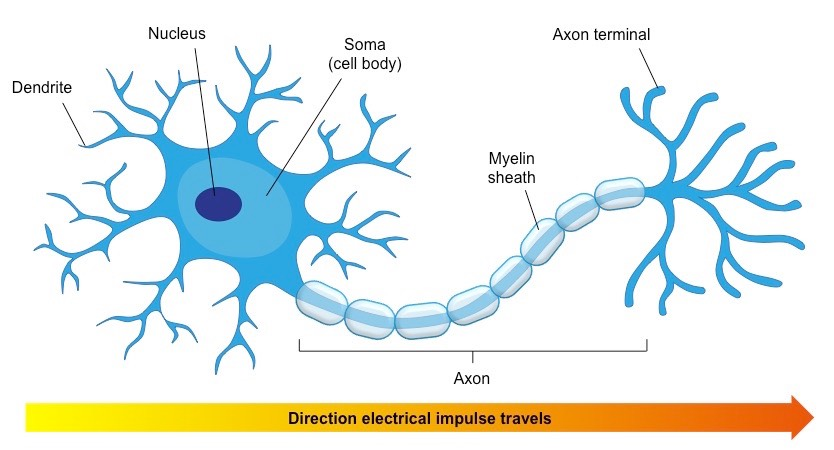
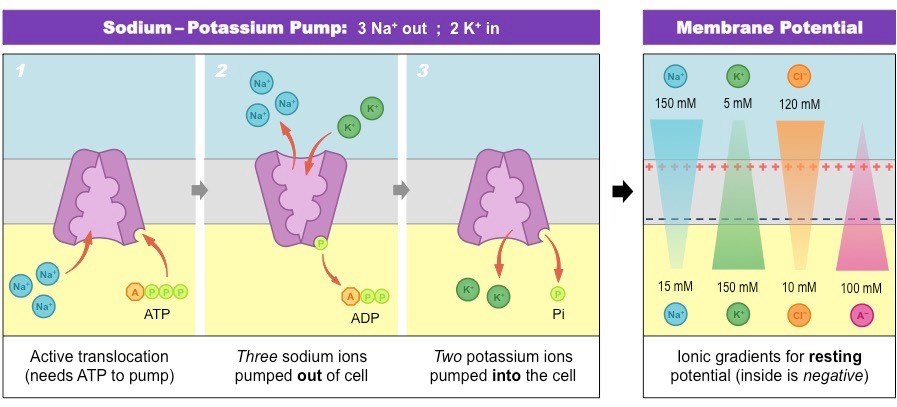
neurons have a difference in charge across their membranes due to the distribution of positively charged ions (Na+/K+)
Electrical signals are created by changing membrane polarity
polarity of a neuron at rest is the resting potential (-70mV)
polarity of a firing neuron is the action potential (+30mV)
Myelination
- nerve impulses are action potentials propagated via axons
- action potentials are “all or none” and are only propagated if a certain threshold potential is reacher (-55mV)
- in certain neurons, the axon is covered by a myelin sheath
- this enables saltatory conduction (increased transmission speed)
- the action potential “hops” between gaps in the myelin sheath (called nodes of Ranvier) for faster transmission
Nerve impulses
- resting potential is maintained by a Na+/Ka+ pump
- it exchanges sodium ions (3 out) and potassium ions (2 in) so that the membrane potential becomes slightly negative
- an action potential changes the resting membrane potential
- opening of sodium channels causes a sodium influx
- this creates a positives membrane potential (depolarisation)
- opening potassium channels causes a potassium efflux
- this restores a negative membrane potential (repolarisation)
- the ion distribution must be restored to original conditions before a neuron can fire again (this is the refractory periods)
Synaptic transfer
- synapses are the physical junctions between two neurons
- electrical impulses cannot cross the physical gaps
- neurons release neurotransmitters into the synapse cleft
- depolarisation in axon terminals opens Ca2+ channels
- Ca2+ influx causes vesicles containing neurotransmitters to release their contents into the synapse (via exocytosis)
- Neurotransmitters bind receptors on post-synaptic cells and generate graded potentials (excitatory of inhibitory)
- the summation of these graded potentials determines if the post-synaptic neuron (or effector cell) is activated)
Neonicotinoid Pesticides
- acetylcholine is a neurotransmitter used in CNS and PNS
- it is broken down in synapses by acetylcholinesterase
- this prevents the overstimulation of receptors
- neonicotinoid pesticides irreversibly bind to acetylcholine receptors and cannot be digested by acetylcholinesterase
- inserts have higher levels of these types of receptors
- this makes neonicotinoids highly effective pesticides
6.6 Hormones & Homeostasis
Homeostasis
- maintenance of a constant internal environment within physiological tolerance limits
- a disease ensues if a factor deviates from its normal range
- physiological processes are regulated by negative feedback
- an effect is antagonistic (opposite to the stimulus)
- this means the detected change is reversed
Endocrine system
- releases chemical messengers called hormones into the blood to act on distant target cells
- hormones only act on the cells with a specific receptor
- works in tandem with the nervous system to maintain physiological balance (homeostasis)
- hormones initiate slower responses (longer durations)
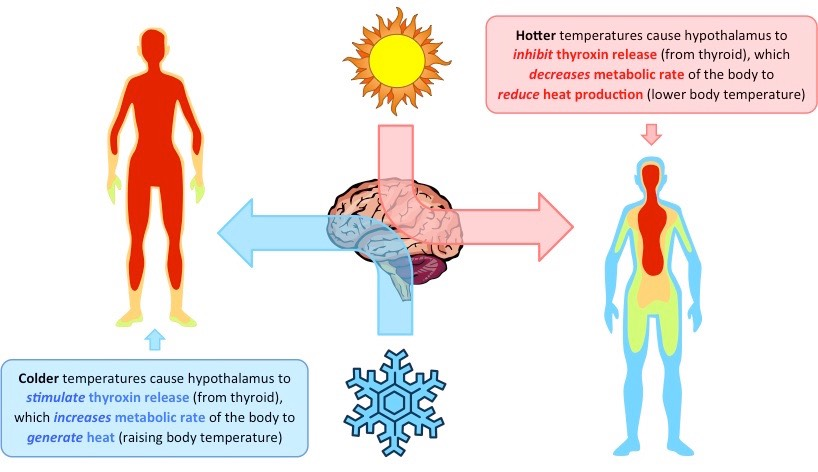
Thermoregulation
body temperature is regulated by the hormone thyroxine
thermoreceptors (skin) send signals to the hypothalamus
thyroxine is released from the thyroid gland when body temperature is low and increases metabolism (generates heat)
thyroxine production requires iodine and a deficiency will result in goitre (enlargement of the thyroid gland)
Circadian rhythms
- regulated by the hormone melatonin
- photoreceptors (eyes) send signals to the hypothalamus
- melatonin is secreted by the pineal gland (in the brain)
- melatonin release is inhibited by light (levels high at night)
- high levels of melatonin promote sleep in diurnal animals
- changing time zones can disrupt melatonin release (jet lag)
- melatonin supplements can recalibrate sleep patterns
Appetite control
- suppression is regulated by the hormone leptin
- adipose cells secrete leptin to suppress appetite (hunger decreases)
- leptin binds to receptors located in the hypothalamus
- over-eating causes more fat cells to be produced (obesity)
- over time, obese people become desensitized to leptin and therefore are more likely to continue to over-eat
- hence, leptin treatments for obese people are ineffective (obesity linked to leptin unresponsiveness - not a deficiency)
Blood glucose regulation
sugar levels are regulated by insulin and glucagon
these hormones are secreted by cells in the pancreas
insulin is secreted by B-cells to lower blood sugar levels
stimulates glucose uptake by the liver and adipose cells
increases the rate of glucose metabolism (respiration increases)
glucagon is secreted by a-cells to raise blood sugar levels
stimulates glycogen breakdown within the liver
decrease rate of glucose metabolism (respiration decreases)
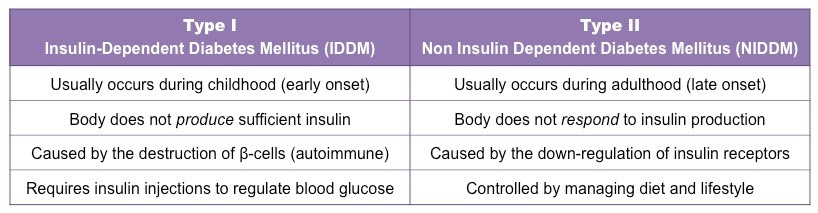
Diabetes
disorder that prevents blood sugar regulation
can be either type 1 or type 2
6.6 Reproductive systems
Human reproductive systems
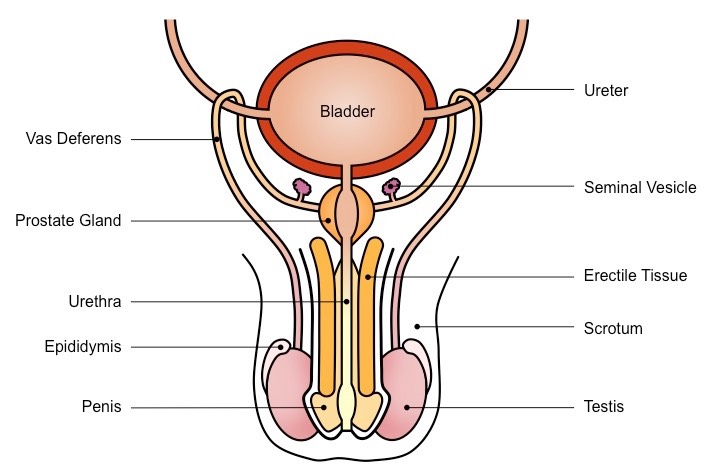
Male system
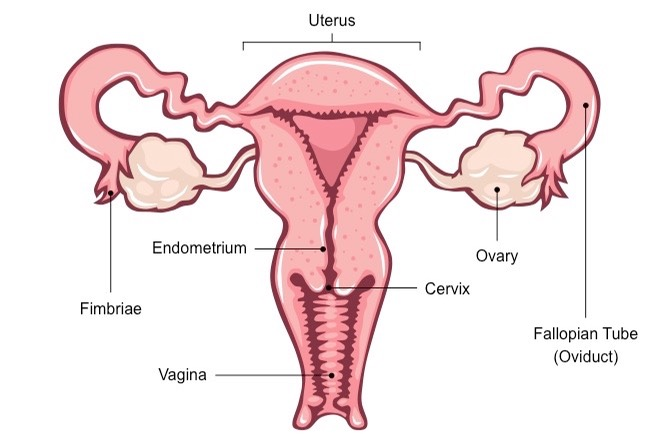
Female system
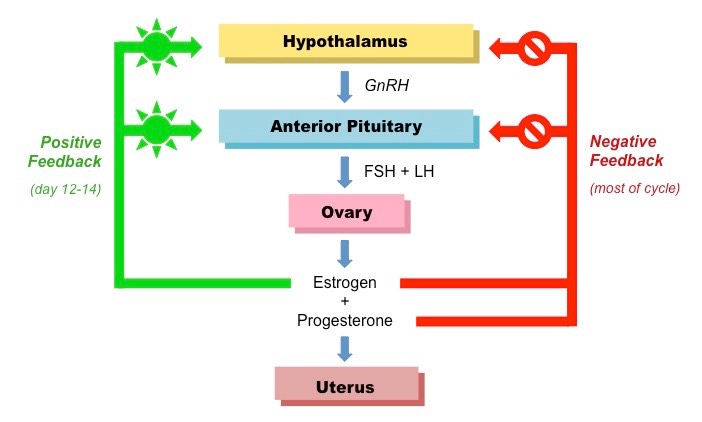
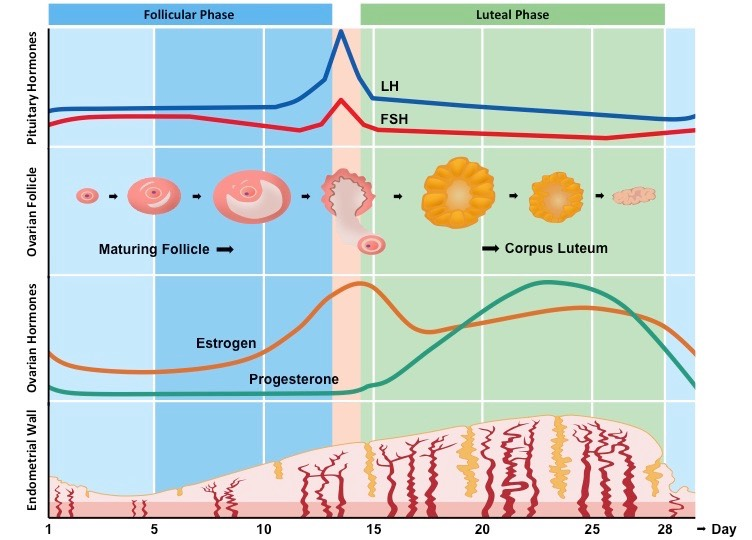
Menstrual cycle
- involves four key hormones and describes the recurring changes that occur to enable pregnancy
Pituitary hormones (FSH and LH):
- stimulates follicular growth within the ovaries
- stimulates estrogen secretion (from the ovarian follicles)
- stimulates progesterone secretion (from corpus luteum)
- a mid-cycle surge in LH triggers ovulation (egg release)
Ovarian hormones (estrogen and progesterone)
promote development / thickening of the endometrium
promote FSH / LH secretion during the follicular phase
inhibit FSH / LH secretion during the luteal phase
Reproductive theories
- “soil and seed” theory proposed by Aristotles
- males provide all the information for life in a “seed”, which forms an egg when mixed with menstrual blood (“soil”)
- William Harvey dissected deer after the mating season and was unable to identify embryos until several months after mating
- he concluded that the “soil and seed” theory was incorrect and that menstrual blood did not contribute to fetal growth
Sex development
- fertilization requires a combination of male and female “seeds”
- male sex is determined by a gene on the Y chromosome which causes gonads to develop as testes and secrete testosterone
- testosterone produces sperm and male characteristics
- female reproductive organs develop in the absence of this gene
- estrogen and progesterone develop female sex characteristics
In vitro fertilization
Stop normal menstrual cycle with drugs \n Hormone treatments to induce ovulation \n Extract multiple eggs from female \n Sperm sample collected from male \n Fertilization occurs externally (in vitro) \n Implantation of embryos into surrogate \n Test for pregnancy to determine success