Week 9: Female Anatomy, Menstrual Cycle, and Pregnancy Symptoms
Nursing Care of Women, Children & Families (N317)
Learning Outcomes
Identify critical components of:
Conception
Embryonic development
Fetal development
Describe the development of the function of:
Placenta
Amniotic fluid
Understand different methods of contraception and assess client’s desire/preference.
List common causes of infertility.
Describe common methods used to assist fertility.
Discuss the ethical and emotional implications of assisted reproductive therapies.
Quick Anatomy & Physiology Review
Internal Female Reproductive Organs:
Ovary
Fallopian tube
Uterus: pear shaped organ that houses the baby.
Placenta is located inside, provides the baby with blood and nutrients.
Secretes many hormones, such as estrogen and progesterone, which are essential for regulating and maintaining pregnancy.
AVA (2 arteries and 1 veins).
Acts as the lungs, kidney, liver, and gut.
The placenta is expelled from the uterus during the third stage of labor, a process known as afterbirth.
Umbilical cord is born with the baby around their neck.
Most of the time, these cords are harmless and doesn’t choke the baby.
Cervix
This dilates during pregnancy.
Vagina
Urethra
Clitoris
Labia Minora & Majora
Vaginal Orifice
Urinary Bladder
The baby uses this as a pillow, causing frequent urination.
This is normal within the 1st and 3rd trimester.
Not as common in the 2nd trimester, may be a sign of a UTI.
Rectum
4 Months:
Baby’s genitalia starts to form, voice recognition starts.
Later on (around 6 months), movement will start as well, feels like a gassy, bubbling feeling.
Once at full term, the baby will have decreased fetal movement due to the lack of room for the baby to move.
Menstrual Cycle
Phases:
Follicular Phase: Begins on Day 1 through Ovulation (approx. Days 10-14)
Purtirity gland releases FSH.
Ovulation Phase: Occurs typically on Day 14 of a 28-day cycle.
Body releases an egg.
Luteal Phase: Days 15 to 28
Body releases progesterone, which helps prepare the uterine lining for potential implantation of a fertilized egg.
Ovulation Hormonal Surge: Day 14, ovum bursts from ovary.
Surge of hormones that burst through the ovary.
Menstruation
Cycle: Monthly expulsion of the inner uterine lining.
Menarche: Establishment of menstruation.
Roughly starts at age 12.
The age is decreasing with nutrition, greater body fat, increased stress response/traumatic events.
Menopause: Cessation of menstrual cycles.
45-55, can become 8 years before.
Frequency: Varies from 21 to 36 days; average is 28 days.
Menstrual Cycle Breakdown
Days 1-7: Menstruation (3-7 days)
Days 8-11: Thickening of endometrium.
Days 18-25: Corpus luteum fades if fertilization does not occur.
Days 26-28: Uterine lining detaches marking menstruation.
Conception
Definition: Conception occurs when a sperm and egg unite, marking the beginning of pregnancy.
Implantation starts with the egg in the uterus.
Fertilization:
Occurs in the fallopian tubes.
In the amplia of the fallopian tube.
Sperm is viable for 72 hours; ova for 12-24 hours post ovulation.
The single ejaculation contains approximately 200–500 million spermatozoa.
Swim up in the fallopain tubes.
Zygote formation occurs following successful union of sperm and egg.
Stages of Development
Pre-embryonic Stage: First two weeks of prenatal development.
Embryonic Period: Extends from Day 13 to 8 weeks post-conception; critical for fetal development.
Terategens, can cause abnormal fuctions to a developing fetus.
By the end of 8 weeks, external structure and all organ systems are present.
Gestational Age (How Far Along Am I?)
Assessment: Based on last menstrual period (LMP).
Duration of Pregnancy: 280 days (40 weeks).
Trimesters:
First Trimester: Weeks 1-12
Second Trimester: Weeks 13-27
Third Trimester: Weeks 28-delivery
Fractional Weeks Notation: Example - “15 4/7”
Contraception and Fertility Awareness
Contraception: Refers to strategies to reduce risk of fertilization or implantation.
Assessment: Review client’s needs, desires, and preferences related to contraception methods.
Common Methods:
Natural family planning
Highly individualized, involving many preferances.
Medical contraindications.
Desire for children, alongside religious, culutral, and personal beliefs.
Barrier methods
Hormonal methods
Intrauterine devices
Surgical procedures
Unintended Pregnancies
Statistics:
Over 3 million unintended pregnancies annually.
1.3 million due to failure to use contraception.
1 million due to non-adherence to methods.
400,000 due to contraceptive method failure.
Non-Hormonal Methods
Options:
Male condoms
Vaginal barriers:
Diaphragm
Internal condom
Cervical cap
Lactation Amenorrhea Method (LAM)
Abstinence
100% method to prevent pregnancy.
Permanent methods like vasectomy and tubal ligation.
IUD- Copper T
Calendar Method
Evaluation: Track the average cycle length over 6 months.
For a 28-day cycle, know ovulation typically occurs around Day 14.
Most fertile days typically: 12-16 of menstrual cycle.
Education: the client must maintain a steady diet in order to accurately follow this method.
Natural Family Planning (NFP)
Also known as Fertility Awareness.
Requires commitment and daily temperature assessment.
Efficacy:
Perfect use: 98%
Typical use: 76%
Uses a string of color-coded beads to keep track of the days of each cycle.
Designed for women with a regular cycle.
Basal Body Temperature (BBT)
Measure oral temperature each morning.
At the same time and before getting out of bed (at a lying state).
Slight drop before ovulation, followed by a rise of 0.4-0.8 °F post-ovulation.
Slightly increases during ovulation.
Cervical Mucus Assessment
Determines fertility based on cervical mucus characteristics:
Dry/Tacky/Thick: Not Fertile
Creamy/Sticky: Not Fertile
Cloudy/Stretchy: Semi-Fertile
Watery/Stretchy/Egg White: Most Fertile
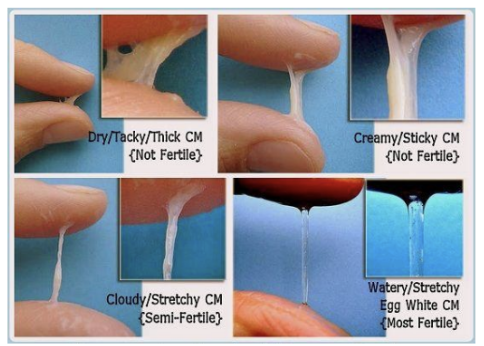
Spinbarkeit refers to the extent to which cervical mucus can stretch between two fingers, indicating peak fertility during ovulation.
Caused by the increase of estrogen.
Lactation Amenorrhea Method (LAM)
This method relies on exclusive breastfeeding.
Most women are not getting their period from breastfeeding and they may not know when they are ovulating.
Requirements: Intervals between feeds must not exceed 4 hours during the day and 6 hours at night.
Barrier Methods
Condoms:
Male and internal condoms; effectiveness varies but typically high when used correctly.
Water-soluble lubricants should be used with condoms.
Condom Application:
Ensure the rolled ring is outside.
Squeeze the tip to avoid air traps.
Pros: Accessible, inexpensive, protect against STId and HIV, prevents pregnancy, and is a non-hormonal method.
Side note (on HIV): well over 100 types, about 40 affect the genitals. Can lead to development of cancers and HPV, get tests and practice safe sex.
Cons: Partner compliance and doesn’t fully provide prevention.
Spermicide
Example: Nonoxynol 9
Typically used with other barrier methods.
Efficacy: Perfect use ~80%, typical use ~70%.
Risks include irritation and increased STI risk if overused.
Makes the vaginal flora become more acidic.
Diaphragm
A dome-shaped soft latex cup used in conjunction with spermicide.
Needs to be fitted.
As similar to the cervical cap that blocks sperm from entering the cervical canal.
Insert the canal at least 30 minutes before sex; can be left in for 48 hours.
Place 2 hours before intercourse and leave in position for at least 6 hours post-intercourse.
Efficacy rates: perfect use 98%, typical use 80% (for cervial cap)
Oral Contraceptives:
Combination
Estrogen contraceptive contraindications:
Hx of thrombophlebitis.
CVA/CV disease
Estrogen-dependent cancer/breast cancer
HTN
Impaired liver function
Heavy smoker
Major surgery requiring prolonged immobilization.
Risk factors:
DVT
Leg pain, warmth on one leg.
Pulmonary embolism
SOB, chest pain.
Stroke/CVA
Transdermal Patch
Sustained release of estrogen and progesterone.
Prevent ovulation, thickens cervical mucus, and alters endo lining.
Placed on the lower abdomen, upper outer arm, upper torso, or buttock.
Progestin-only:
Depo-Provera
An IM ingestion of progestin.
Prevents ovulation for 12 weeks.
Failure rate of 3%.
Side Effects: Irregular menstrual bleeding, weight gain (4 lbs per year), depression, headaches, nervousness, decreased libido, and breast discomfort.
Prolonged use (Black Box warning): decreased bone density in teens, therefore you must stress adequate calcium and vitamin D.
No effects on breast milk and fertility.
Implantable Progestins:
Flexible rods are inserted under the skin of the upper arm.
Effective for a minimum of 3 years.
Side Effects: Irregular menstrual bleeding.
Does not protect against STIs.
Contraindications: Unexplained VB.
Intrauterine Device (IUD)
Most common.
Copper IUD is the only non-hormonal one.
Creates foreign body inflammatory reactions that prevent implantation.
Side effects: Irregular periods, perforation of the uterus at insertion, ectopic pregnancy, and risk of infection.
If pregnancy does occur, spontaneous abortion or preterm birth.
It can be contraindicated with many drugs, antibiotics, antifungals, and more.
Female Sterilization
Process: Commonly performed via abdominal surgery post-birth.
Efficacy: 99.6% with no adherence required, but does not protect against STIs.
Male Sterilization
Procedure: Outpatient vasectomy; effectiveness achieved after 3 months.
Efficacy: 99.8%.
Emergency Contraception
Types:
ParaGard IUD, Ella, Plan B One-Step
Most effective 72 hours after unprotected sex.
Combination of estrogen/progestin or progestin-only forms.
Timing:
Must be initiated within specific periods post-intercourse (Varies by type).
ParaGard & Ella can be used within 5 days.
Common Pregnancy Symptoms
Early Signs:
Morning sickness
Increased appetite or thirst
Food cravings/aversions
Sore breasts
Missed period and many more.
Infertility
Hormonal changes affecting mood and behavior
Increased fatigue and sleep disturbances
Potential emotional responses related to reproductive health
Definition: A lack of conception after 12 months of unprotected intercourse (rule varies with age)
Primary: in a woman who never conceived.
Secondary: conceived in the past, but unable to do so again.
Factors in men:
Abnormality of the sperm (oligospermia (low sperm count)/motility)
Abnormal ejaculations (retrograde: is deposited into the bladder)
Structural or hormonal disorders
Mumps after adolescence
Cancers/tumors
Poor nutrition/obesity
ATIs
Substance use
SSRIs and MAOIs are used
Age (35 and older)
Factors in women
Abnormalities of the Fallopian Tube
Abnormalities of the cervix
Disorders of ovulation
Age (35 and older)
Diagnostic Tests: ovulation prediction, ultrasonography, and post-coital test (cervical mucus/sperm function).
Ovulation Prediction: Detects hormonal changes in urine to determine ovulation timing.
Ultrasonography: Uses sound waves to visualize ovaries, uterus, and follicles for assessing ovulation, ovarian reserve, and early pregnancy.
Post-coital test: Evaluates sperm-cervical mucus interaction to assess sperm motility and mucus quality.
Infertility Therapy
Timing of intercourse
Medications
Ovulation induction
Surgical procedures
Therapeutic insemination
Partner or donor semen
IUI (intrauterine insemination): sperm placed directly into the uterus.
Egg donation
Fewer donors than for sperm donation.
An in-depth screening process where the client takes medications to speed the growth of their egg.
Surrogate Parents
Assisted Reproductive Technology
Conclusion
Understanding the development, methods of contraception, and addressing infertility are crucial aspects of nursing care within the domain of women, children, and families. Further studies and practical applications will ensure proper guidance and support for families in their reproductive health journey.