Thanatology
Introduction
- Thanatology: The scientific study of death in all its aspects, including its cause and phenomena.
- It also includes bodily changes that accompany death (postmortem changes) and their medico-legal significance.
- Somatic Death: Irreversible cessation of the vital functions of the brain, heart, and lungs.
- Molecular death: Initial changes occur due to metabolic dysfunction and later from structural disintegration.
Brain/Brainstem Death
- Brain death: It is the complete and irreversible cessation of functioning of the brain.
- Brain: It includes all the central nervous system (CNS) structures, except the spinal cord.
- The respiratory center which controls respiration lies within the brainstem. If this area is dead, the person is unable to breath spontaneously or regain consciousness.
- While the integrity of the reticular formation inside the brainstem is important for the appropriate functioning of the cortex, brainstem death may realistically be regarded to be sufficient for brain death.
- The important element in diagnosing brain death is the proof of absence of all brainstem functioning.
Mechanism of Brain Death
- Brain injury has a number of causes, such as traumatic or cerebrovascular injury and generalized hypoxia, all of which produce brain edema.
- Edema: It is accompanied by an increase in intracranial pressure leading to gradual decrease in cerebral circulation to the level of almost cessation, causing aseptic necrosis of the brain.
- Within 3–5 days, there occurs widespread brain destruction or pannecrosis throughout the cerebrum and the brainstem, the brain becomes a liquefied mass, a condition known as ‘respirator brain’.
- Increased intracranial pressure crushes the brain and brainstem, causing complete brain infarction.
Diagnosing Brain Death
- Establishment of cessation of all brain functions
- cerebral and mainly brainstem functions using primarily the clinical criteria and partly by confirmatory paraclinical/ laboratory tests which includes electroencephalogram and somatosensory evoked potentials (SSEP) and tests to measure cerebral blood flow.
- Demonstration that cessation of these functions is irreversible: Irreversibility is established by:
- Determination of the cause of loss of brain function
- Exclusion of reversible conditions
- Demonstration that the cessation of brain functions persists for an appropriate period of observation.
Diagnostic clinical brain death criteria
Prerequisites. Brain death is the absence of clinical brain function when the proximate cause is known and demonstrably irreversible.
- Clinical or neuroimaging evidence of an acute CNS catastrophe that is compatible with the clinical diagnosis of brain death.
- Exclusion of complicating medical conditions that may confound clinical assessment.
- No drug intoxication or poisoning.
- Core temperature > 32°C (90°F).
The three cardinal findings in brain death are coma, absence of brainstem reflexes and apnea.
- Coma or unresponsiveness—No cerebral motor response to pain in all extremities.
- Absence of brainstem reflexes
- Pupils
- Absent pupillary response to bright light.
- Size: Mid position (4 mm) to dilated (9 mm)
- Ocular movement
- No oculocephalic reflex (Doll’s eye phenomenon).
- Absent oculovestibular reflex (Caloric test): No deviation of eyes to irrigation in each ear with 50 ml of cold water.
- Facial sensation and facial motor response
- No corneal reflex to touch with a cotton swab.
- No jaw reflex.
- No grimacing to deep pressure on nail bed, supraorbital ridge, or temporomandibular joint
- Pharyngeal and tracheal reflexes
- No gag reflex: No response after stimulation of the posterior pharynx with tongue blade.
- No cough response to bronchial suction.
- Apnea test: It is based on the fact that loss of brainstem function definitively results in loss of centrally controlled breathing, with resultant apnea.
Exclusion of Reversible Conditions
- Hypothermia.
- Severe electrolyte, acid-base or endocrine abnormalities.
- Drug intoxication: Presence of sedation, neuromuscular blockade, or drugs causing CNS depression.
- Hypoxia, hypotension or shock.
- Other conditions: Brainstem encephalitis, severe hypophosphatemia, encephalopathies associated with hepatic failure, uremia, or hyperosmolar coma of diabetes mellitus.
- Observation period: The duration is still debated. After cardiac resuscitation, neurological testing must wait 30 minutes.
Types of transplants
- Autograft: Tissue transplanted from one part of the body to another in the same individual. It is also called autotransplant or homologous transplantation.
- Allograft: Organ or tissue transplanted from one individual to another of the same species with a different genotype. It is also called allogeneic graft or homograft.
- Isograft: Organs or tissues are transplanted from a donor to a genetically identical recipient (such as an identical twin).
- Xenograft: Organs or tissue transplanted from one species to another, e.g. grafting of animal tissue into humans.
- Split transplants: Deceased-donor organ (specifically the liver) may be divided between two recipients, especially an adult and a child.
Cause, Mechanism and Manner of Death
- Cause of death: Any injury or disease producing physiological derangement, briefly or over a prolonged period, and which results in the death of the individual
- E.g. a gunshot wound to the abdomen, a stab wound to the chest, adenocarcinoma of the lung or coronary atherosclerosis.
- Mechanism of death: The physiological derangement produced by the cause of death that results in death
- E.g. haemorrhage, septicemia, metabolic acidosis or alkalosis, ventricular fibrillation or respiratory paralysis.
- A particular mechanism of death can be produced by multiple causes of death and vice versa.
- Manner of death: Explains how the cause of death came about.
- Natural Death: Death resulting from disease
- Homicide: Death resulting from the deliberate action of another
- Suicide: Death intentionally self-inflicted
- Accident: Death as a result of an environmental influence
- Dyadic death: Also known as murder-suicide or homicide-suicide; refers to an incident where a homicide is committed followed by the perpetrator’s suicide almost immediately or soon after the homicide.
- Agonal period: It is the time between a lethal occurrence and death.
Modes of Death (Proximate Causes of Death)
- Mode of death: Refers to an abnormal physiological state that pertained at the time of death
- E.g. coma, congestive cardiac failure, cardio-respiratory failure, cardiac arrest and pulmonary edema.
- Coma: It is a state of profound unconsciousness from which a person cannot be roused, with minimal or no detectable responsiveness to stimuli.
- This is death from failure of the function of the brain.
- Syncope: This is death from failure of the function of the heart resulting in hypoxia and hypoperfusion of the brain.
- Asphyxia: This is death from failure of the function of the lungs.
Anoxia
- Anoxia: Complete lack of oxygen, which ultimately leads to cardiac failure and death.
- Hypoxia: Shortage of oxygen in blood.
- Classification of Anoxia
- Anoxic anoxia: It occurs due to defective oxygenation of blood in the lungs and may be due to:
- Inhaling carbon dioxide, sewage gas, or rarefied air.
- Smothering, hanging, strangulation, throttling, gagging, choking, or drowning.
- Prevention of normal movements of the chest
- Cessation of the respiratory movements, as in paralysis of the respiratory center.
- Anemic anoxia: It occurs due to reduced oxygen carrying capacity of the blood.
- e.g. hemorrhage, poisoning by carbon monoxide or nitrites.
- Histotoxic anoxia: It means inhibition of oxidative processes in the tissue which cannot make use of oxygen in the blood.
- e.g. cyanide poisoning.
- Stagnant/ischemic anoxia: In this type, impaired circulation results in reduced oxygen delivery to the tissues.
- e.g. shock, congestive cardiac failure or heat stroke.
Sudden Death
- Sudden Death: Death occurring instantaneously or within 1 h of the onset of morbid symptoms.
- It is the unexpected death of a healthy individual.
- An external body examination cannot determine the reason of sudden death.
- To rule out foul play, an autopsy is required in all such situations.
- Should the death be ruled a homicide, a doctor who provides a death certificate might be charged with complicity.
- Causes
- Cardiovascular (44–50% of cases)
- Coronary artery disease
- Valvular heart disease
- Congenital heart disease
- Hypertensive heart disease
- Infection, e.g. myocarditis, pericarditis
- Cardiac tamponade
- Cardiomyopathies
- Aortic aneurysm.
- Respiratory system (15–23% of cases)
- Pulmonary embolism
- Lobar/bronchopneumonia
- Massive hemoptysis
- Obstruction by foreign body z Air embolism z Edema of glottis/lungs z Pneumothorax z Neoplasm.
- Central nervous system (10-18% of cases)
- Intracerebral hemorrhage
- Cerebral thrombosis
- Subarachnoid hemorrhage
- Embolism
- Meningitis
- Tumor
- Idiopathic epilepsy
- Abscess.
- Gastrointestinal system (6-8% of cases)
- Hemorrhage from peptic ulcer, esophageal varices or malignancy
- Strangulated hernia
- Rupture of abdominal aneurysm
- Ruptured diseased viscus
- Acute hemorrhagic pancreatitis
- Appendicitis
- Fulminant hepatic failure
- Ruptured liver abscess.
- Genitourinary system (3-5%)
- Chronic nephritis
- Tuberculosis of kidney
- Nephrolithiasis
- Tumors of kidney/bladder.
- Reproductive system
- Toxemia of pregnancy
- Rupture of ectopic pregnancy
- Uterine hemorrhage due to fibroids
- Carcinoma of vulva.
- Endocrine
- Adrenal insufficiency or hemorrhage
- Myxedemic coma or crisis
- Diabetic coma
- Parathyroid crisis.
- Iatrogenic
- Abuse of drugs
- Mismatched blood transfusion
- Sudden withdrawal of steroids
- Anesthesia
- Miscellaneous
- Anaphylaxis
- Cerebral malaria
- Alcoholism
- Shock from dread, fright or emotion
- Sickle cell crisis
- Bacteremic shock.
- Special Causes in Children
- Cot deaths or SIDS
- Mongols and others with congenital or mental abnormalities
- Concealed puncture wounds.
Coronary Atherosclerosis
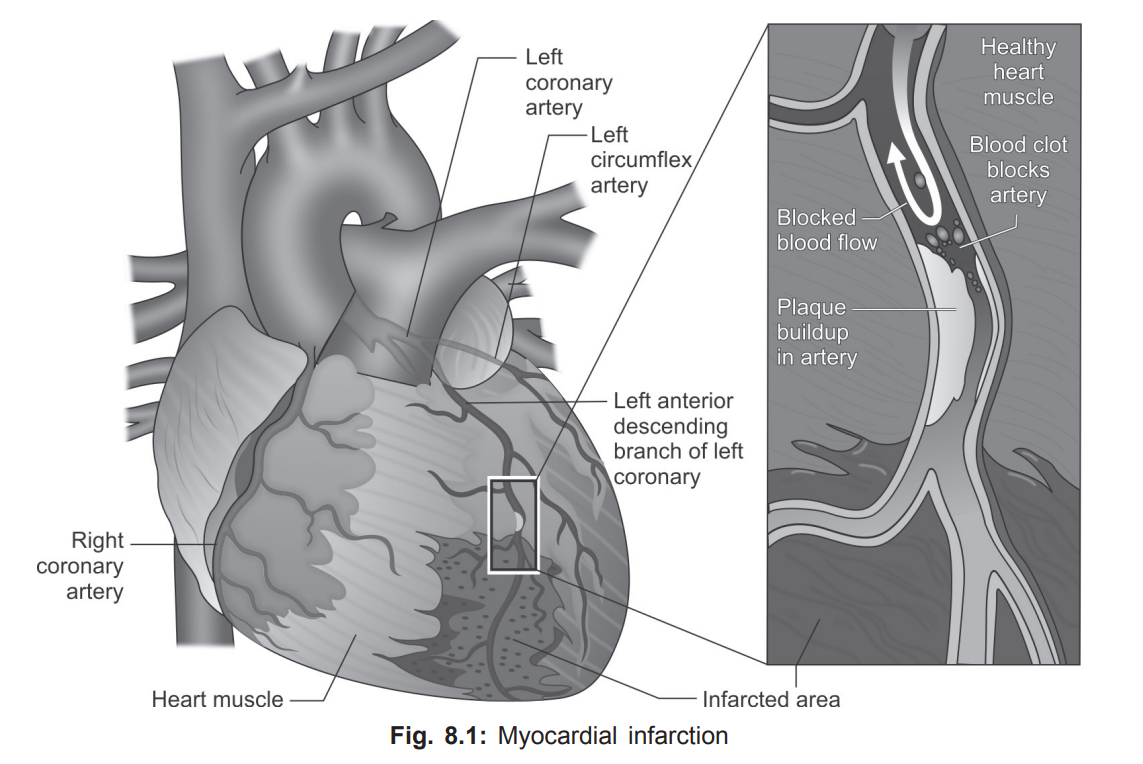
Coronary Atherosclerosis: The most common cause of death from cardiovascular disease.
Acute occlusion of coronary artery may result from thrombosis or hemorrhage within the wall of the artery.
The frequency of occlusion of the coronary arteries is:
- Vascular obstruction and coronary circulation architecture dictate the location of myocardial infarction (MI).
- Most left ventricular anterior wall infarcts occur. Right ventricle involvement is <10%.
- The anterior and apical left ventricle and interventricular septum are infarcted by left anterior descending coronary artery occlusion (anteroapical MI).
- The right coronary artery causes most posterior and basal left ventricular infarcts.
- The right vessel or left artery circumflex branch may prevent posterior infarcts.
- Transmural infarcts affect the whole ventricular wall, whereas subendocardial infarcts affect the inner one-third.
- Dark-brown, vessel-attached thrombi are fresh. Aged thrombi are uniform yellowish or gray, solid plugs obstructing vessels.
Significant obstruction of the coronary artery lumen without MI or thrombosis may lead to sudden death.
Hypoxic myocardium is electrically unstable, and liable to arrhythmia and ventricular fibrillation, especially at moments of sudden stress
Postmortem Examination
- No visible change occurs during 12–18 h.
- Age determines a myocardial infarct's appearance.
- For the heart's first detectable alteration to occur, 12–24 h of survival postinfarction is required.
- After coagulation necrosis and inflammation, granulation tissue forms, the necrotic myocardium resorbs, and the granulation tissue forms a collagen-rich scar.
- A particular infarct's gross and microscopic appearance may be used to assess its age because to these events' predictable pattern.
- Immersion of tissue slices in a solution of triphenyl tetrazolium chloride (TTC) produces red color to the healthy part (where dehydrogenase is intact) and pale color to the infarcted portion after 4 h. Results are varied.
- New thrombotic lesion occurs in fewer than 25% of patients.
- Coronary artery spasm may kill angina patients without severe atherosclerosis or congenital abnormalities.
- Arrhythmias and mortality may result from cardiac conducting system defects.
- Despite normal coronary arteries, anybody with a heart above 420 g is at danger of sudden death.
- Enzyme histochemistry: It is the most reliable method of detecting early MI.
- Dehydrogenases—succinic, lactic, malic, hydroxybutyric and cytochrome oxidase are among those used.
- With malate dehydrogenase, normal myocardium stains dark blue-black and infarcted area is devoid of color.
- Periodic Acid-Schiff (PAS) stain: In early infarcts (at least 28 h), damaged myofibers stain a pale purple-blue with PAS, compared with the pink color of healthy fibers.
- Hematoxylin-Eosin (H&E) autofluorescence: Routine formalinfixed H&E sections are examined under UV light.
- Early infarcted fibers show a shift of their secondary emission towards yellow, away from the usual olive-green of healthy fibers.
- Acridine-Orange fluorescent stain: Slides are examined under UV light; normal myocardium is golden-brown/yellowish-brown with damaged fibers showing a shift to green.
Anaphylactic Deaths
- Signs and Symptoms
- Acute respiratory distress or circulatory collapse are common anaphylactic reactions.
- Faintness, skin itching, urticaria, chest tightness, wheezing, respiratory problems, and collapse.
- Symptoms generally appear within 15–20 minutes in anaphylactic fatalities.
- After that period, one would need a well-documented medical history of progressively building symptoms to suggest anaphylactic response.
- Pharyngeal or laryngeal edema may block the upper airway, whereas bronchospasm with lung smooth muscle contraction, vasodilation, and increased capillary permeability can block the lower airway.
- Breathing problems might induce cardiac arrest.
Vagal Inhibition
- Sudden death occurring within seconds or minutes as a result of minor trauma or harmless peripheral stimulation may be caused by vagal inhibition.
- Pressure on the baroreceptors in the carotid sinuses, sheaths, and body (found in the internal carotid artery and around the angle of mandible) raises blood pressure in these sinuses, reducing the heart rate, dilatation of blood vessels, and lowering blood pressure.
- Bradycardia and cardiac arrhythmias, from ventricular to cardiac arrest, may result with carotid sinus stimulation in certain people.
- Mechanisms
- A reflex arc generates afferent (sensory) nerve impulses in the carotid complex of nerve terminals, not the vagal nerve trunk.
- These impulses go by glossopharyngeal nerves to the tenth nucleus in the brainstem and return to the heart and other organs through the vagus (efferent) supply.
- Causes
- Pressure on the carotid sinuses from hanging or strangulation.
- A sudden strike to the larynx, chest, abdomen, or sexual organs.
- Food in the larynx or abrupt fluid inhalation.
- Immersion in cold water.
- The insertion of a device into the bronchus, uterus, bladder, or rectum.
- Pleural puncture causing pneumothorax.
- Sudden expulsion of pathological fluids, such as ascitic tap.
- Brugada syndrome: A disorder characterized by sudden nocturnal death of an apparently healthy young person with no history of any disease/drug abuse, and the findings at autopsy are those of asphyxia.