5-Management of Complications 2024
Preventing Complications
Review med history
“Never treat a stranger”
Look for gaps or inconsistencies
lots of followup questions/clarifications
Radiographs-current, accurate
Surgical site confimed/documented
diagnosis included
Informed consent explained, questions answered, THEN signed by patient/guardian
Medical History
Unknown medications
“I’m taking something but don’t know name or dosage.”
Update/confirm medical history/meds
EVERY VISIT
Has prescription, but are they taking it?
“Ran out but haven’t gotten refill”
Call MD office, pharmacy if questions
Medical consultation as needed
Radiographs
Current= within ONE YEAR
unchanged visually in mouth!
Properly mounted?→ can be imported backwards or on viewbox backward
scanned films may lack dates
Complications
Nerve injuries
Sinus Perforation
Alveolar osteitis
Bleeding
Infection
Nausea and vomiting
Soft tissue and adjacent osseous tissue injury
Temporomandibular joint injury
Pain and Swelling – to excess
Injuries to adjacent teeth
Displacement of tooth/foreign bodies
Mandible fracture- rare
ALL SHOULD BE IN THE INFORMED CONSENT!!!!!
Nausea and Vomiting Management
Pain meds?
Still bleeding?
New bleeding from vomiting?
Clear liquids
Anti-emetic
PO (oral?); Zofran ODT 4 mg
IM,IV, PR (rectal suppository)
Alveolar Osteitis- “Dry Socket”
Clinical presentation
Increasing pain, usually 3 to 5 days after surgery
Different quality/type of pain
Pain not relieved by previously effective meds
No relief of pain
Get partial relief for short period of time
Radiates to ear
Temporal headache same side
Whole side of jaw hurts
NO CLOT in socket

Differential Diagnosis
Postoperative pain
Difficult case, just surgical pain→ pain meds and time
Wound Dehiscence or Exposed Bone?
Anesthetize and re-suture?
Postoperative infection
MPD Syndrome (myofascial pain dysfunction)
Dental pain – Now the 2nd chief complaint hurts!
Other source, not related to surgery
Treatment
Anesthetize? (Maybe, but not always)
NS irrigation until clear return
Nu-Gauze; Gelfoam – carriers for medicament
Some carriers need to be removed, some don’t
Many commercial preparations
Eugenol – strong taste of cloves!, but effective; usual ingredient in any preparation
One dressing at a time
Large ext site →1 longer Nu-Gauze strip – best solution ; option→ 2 dressings…make OBVIOUS note of 2 dressings
Insure removal (gauze) → post op infection if not removed
Burning and stinging when socket first packed
Let patient know before packing
B&S goes away in about 20-30 min; so does pain
This lessens the pain but doesn’t go from 10/10 to 0/10, OTC meds generally work well after packing
Packing may need to be changed out every 2-3 days for continued relief – saliva dilutes it
Usually 7-10 days of healing before no packing needed –adequate tissue coverage
Don’t remove pack on start of week-end
Bleeding: Systemic Factors
Medical History
ASA, Anticoagulant, alcohol, chemotherapy
bleeding disorders
Blood Pressure
Intraoral Factors
Intra-operative – KNOW YOUR ANATOMY!!!
Soft tissue
Vessel – steady, pumping?
Muscle ooze
Bone
Nutrient canal
Cancellous bone
Chronic granulation tissue
IA neurovascular bundle
Post-operative
soft tissue
Bone
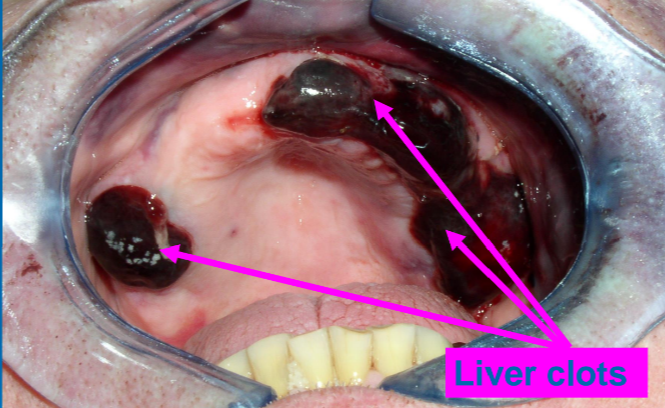
Liver clot-ineffective clotting
Control of Bleeding
Same modalities for intra-op and post-op:
Pressure
local hemostatic agents
ligation
Cautery
Suturing
Local Hemostasis
Gelfoam (Gelatin)
MOA: Helps stabilize clot formation (does not activate coagulation cascade or platelets)
Compressive forces- no
Gelfoam and suture
Gelfoam/topical thrombin/suture
Surgicel (Cellulose)
MOA: Helps stabilize clot formation (does not activate coagulation cascade or platelets)
Delays socket healing – use smallest amt that is effective
Compressive forces - yes
No topical thrombin
CollaPlug (Collagen) $
MOA: Activates platelet aggregation
Bone Wax
Salicylic acid and beeswax
MOA: Mechanical blockage of small bone channels
Topical Thrombin $ (Fibrin Formation)
Epinephrine
Sutures
Pressure
Bleeding: Anti-Fibrinolytic Agents
Systemic Medications
aminocaproic acid (Amicar)
tranexamic acid
In consultation with Hematologist
Von Willebrand, Some Hemophilias
Management of Post-operative Bleeding
If contacted by a patient experiencing prolonged bleeding, review the patient’s medical history and medications. Give the patient explicit instructions to gently remove any “liver clots” and bite down on gauze (OR TEA BAG) with continuous pressure for at least 30 minutes. If the patient complains of continued ACTIVE bleeding, they should be evaluated at the office.
At the office, you apply gauze over the extraction sites and have patient bite with pressure again.
If initial measures do not control the bleeding, surgical intervention is indicated.
The Magic of the Tea Bag
Tea contains “tannic acid” which helps coagulate the blood.
Wet the bag, wring it out, bite on it like a gauze pad
No “herbal” tea
Get all instruments/equipment out you may need while patient is biting on the gauze.
Full surgery tray, suction, irrigation, hemostatic agents, etc.
Inspect the surgical site
Good lighting and suction are essential.
If the use of local anesthetic is required, utilize one that does not contain a vasoconstrictor (this may give you temporary control, but may hinder your ability to determine the source of bleeding).
If sutures are present, they should be removed so the surgical site can be evaluated adequately.
Determine if the bleeding is coming from hard or soft tissues.
Soft tissue bleeding can often be controlled with direct pressure;
if the source of bleeding is granulation tissue, it should be removed
If source is vessel – clamp, suture, electrocautery (except – bleeding from IAN vessels)
Bleeding from bone
If the bleeding is from a pinpoint area the bone can be burnished, or bone wax is used
If the bleeding is more diffuse, a hemostatic adjunct should be packed into the socket and direct pressure applied.
Management of Displaced Teeth and Fragments
Submandibular space:
Thin lingual cortex, thinner to the posterior
If displacement occurs into the submandibular space, immediately place upward external pressure on the lingual cortex to prevent further displacement.
If possible, attempt to manipulate the root fragment back into the extraction site.
If retrieval attempt is unsuccessful, place patient on antibiotics and refer.
Antibiotics are considered mandatory because a fascial space has been violated by the tooth.
Mandibular Canal:
If displacement of root fragment into the mandibular canal is suspected, a periapical and occlusal radiograph should be obtained to verify position. Often the root fragment is not in the mandibular canal, but in a large marrow cavity.
Referral is indicated.
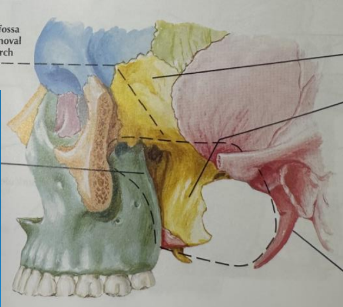
Infratemporal Fossa
Distoangular Maxillary 3rd molar most often
Prevention: After your flap is elevated and the tooth is visualized, a retractor should be placed posterior to the tooth to prevent displacement distally under the flap.
Do not attempt removal unless there is good access, light and visibility
Make only ONE attempt
Multiple attempts push tooth farther away
If unsuccessful, close, antibiotics, refer
Expect 4 - 6 week wait for fibrosis
Patient may elect to leave in place if asymptomatic
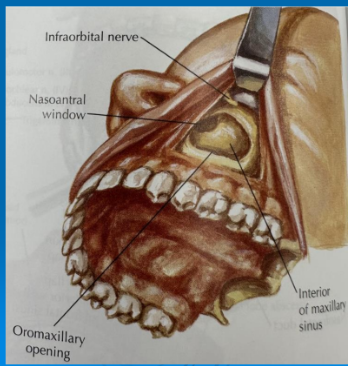
Sinus
Prevention
Avoid excessive apical force when using elevator or root tip pick
2-3 mm without pathology or infection - consider leaving; inform patient; offer referral
Large fragment or whole tooth, small fragment with pathology or infection – remove
Don’t attempt to retrieve through the socket!
For removal of roots with pathology or larger roots, the Caldwell-Luc approach should be used.
Oroantral Communications
Sequelae include
Post-Op Sinusitis
Chronic Oroantral fistula
Management Depends on:
Size
Location (Apex vs Coronal portion)
PREVENTION IS KEY
Section Max Molars
Easy on the irrigation
Careful with apical pressure

Management
2mm or less: no treatment necessary
2-6 mm: gently place Gelfoam, suture, sinus cautions no sneezing, nose blowing, antibiotics, decongestants
7 mm or larger: flap procedure (buccal) antibiotics, decongestants
Sinus Precaution
Don’t Blow Your Nose
If You Must Sneeze, LET IT FLY, Do Not Stifle It
No Sucking In or Blowing Out
No Straws, No Smoking, No Blowing Up Balloons, No Trumpet Practice
No Strenuous Workout or Heavy Lifting
We don’t want to get your blood pumping
Avoid Bending Over
sleep with an extra pillow- Head above heart
Fracture of Mandible
Rare, but almost always associated with removal of impacted third molars
Inform patient at pre-op, should be on consent form
Prevention: avoid excessive force, especially with elevators
expect the possibility in deeply impacted teeth, very thin mandible, or large area of pathology
Treatment:
Refer
Thermal Injury to lip/Cheek
Results from…
Heat from friction of rotating shank
Lip numb, patient doesn’t feel it
Handpiece overheating
Mostly important
inadequate retraction
not using bur guard
lack of attention to where handpiece is in mouth
100% PREVENTABLE
ALWAYS use bur guard
Utilize good retraction
Handpiece should NEVER rest against soft tissue
Be aware of where the handpiece and bur are AT ALL TIMES when in use in the mouth
If handpiece is overheating, DO NOT USE – if handpiece feels hot in your hand, burn risk

Soft Tissue Injury
Management:
Frank discussion with the patient since these are usually minor complications
Bacitracin ointment
Clobetasol?
Vaseline?
Wrong Tooth
Prevention:
Confirm surgical site w/patient - “What are we doing today?” Get patient to tell you
Careful pre-op assessment, especially when requested by ortho; confirm w/referring DDS
Count teeth – check once, check twice, place forcep and check again;
Assistant is part of the team – encourage assistant questions
Treatment
If immediately recognized, rinse with saline and replace
If for ortho, consult with orthodontist, they may be able to alter the treatment plan
Do not extract contralateral tooth
Management
Inform patient, patient’s parent(s) if a minor, any other dentist involved in care.
Contact your liability carrier for guidance.
DO NOT TRY TO HIDE IT
TMJ Injury
Prevention: Bite block, support mandible
Treatment
if subluxated or dislocated - reduce
heat, rest, soft diet, NSAIDs
Injury to Adjacent Teeth
Fracture of the crown or existing restoration
Forcep placement
Elevator
TALK ABOUT IN PRE-OP CONSENT!!!
Edema
Prevention
Minimize surgical trauma – good surgical technique
Steroids/NSAIDs
Ice pack – first 24-36 hrs (change sides q20 min)
• Moist heat after 36 hrs
Elevate head- extra pillow
Treatment
Moist heat: 15-20 min, 3-4x/d, reassurance
Elevation – sleep with extra 1-2 pillows
Continue NSAIDs
Ecchymosis
Blood in tissues
Occurs with all surgeries
Some show more than others
May extend down neck – end at clavicles
Inform patient that color will change/fade and could take 1-2 weeks to resolve

Subcutaneous Emphysema
Prevention: avoid traditional high speed handpiece to perform surgery. Special rear exhaust should be used.
Careful when packing for impression and air blast to dry area.
Diagnosis: crackly sound like Rice Krispies
Treatment: time, antibiotics, reassurance

Trismus
Prevention
minimize surgical trauma, bite block, chin support
Treatment- must be aggressive
heat, soft diet, NSAID, opening exercises, muscle relaxant
If not responding:
tongue blade exercise
Physical Therapy referral
r/o infection, especially pterygomandibular space infection if no obvious swelling
Wound Dehiscence
Dehiscence Prevention:
Incisions over sound bone
Avoid suturing under tension
Management
Anesthetize and re-suture
Pain similar to “dry socket” – usually as result of apically positioned flap with exposed bone
Inform patient and instruct in irrigation, oral rinses-NS, Peridex if tissue can’t be repositioned and sutured; most frequently lingual dehiscence
Heal by secondary intention
follow-up appts to assess progress and reassure
Bony Sequestrum
Prevention:
Debridement of surgical
Palpate cortical plates
Not always preventable
Treatment: sequestrectomy
full thickness flap, debride, alveoplasty prn, NS irrigation
Resuture Flap
Specialist Referral?
Severe infection
Nerve injury – MONITOR???
Severe bleeding
Displaced root/tooth
O-A fistula
Mandible fracture
Significant soft tissue injury
IF YOU CAN’T DEAL WITH THE ISSUE, SEND TO SOMEONE WHO CAN
If the issue is highly likely pre-op:
REFER TO BEGIN WITH!!!
Listen to that conscience!